Abstract
Background
Human immunodeficiency virus (HIV) continues to be a global public health concern, with 2.1 million people newly infected in 2015. Although many high-income countries have noted decreasing rates of HIV, between 2013 and 2015 Canada’s rates had stabilized at 5.8 per 100,000 population.
Objective
To provide a descriptive overview of reported cases of HIV in Canada up until 2016 by geographic location, sex, age group, exposure category and race/ethnicity, with a focus on the most recent data.
Methods
The Public Health Agency of Canada (PHAC) monitors HIV through the national HIV/AIDS Surveillance System (HASS), Immigration, Refugees and Citizenship Canada (IRCC), and the Canadian Perinatal HIV Surveillance Program (CPHSP). HASS is a passive, case-based system that collates non-nominal data voluntarily submitted by all Canadian provinces and territories. Data were also received from the IRCC and the CPHSP. Data were collated, tables and figures were prepared, then descriptive statistics were applied by PHAC and validated by each province and territory.
Results
A total of 2,344 new diagnoses of HIV were reported in 2016 in Canada, with a cumulative total of 84,409 cases since 1985. The national diagnosis rate increased from 5.8 per 100,000 population in 2015 to 6.4 per 100,000 population in 2016. Saskatchewan reported the highest provincial diagnosis rate in 2016 (15.1 per 100,000 population). In 2016, 76.6% of reported HIV cases were among males. Adults aged 30-39 years old accounted for 28.7% of all reported cases. There was a similar age distribution of HIV cases between sexes with notable increases in the proportion of the 50 years and over age group over the past five years. The “men who have sex with men” exposure category continued to represent the largest number and proportion of all reported HIV cases in adults (44.1%). White (40.4%), Black (21.9%) and Indigenous (21.2%) race/ethnicity categories represented the largest proportions of cases.
Conclusion
In 2016, Canada saw a slight increase in the number and rate of reported HIV cases compared with previous years. Although the diagnostic rate was lower than in all years prior to 2012, it is the highest of the past five years. While a number of possibilities exist to explain this increase, further investigation and additional data are needed in order to determine the cause and significance.
Introduction
Human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) are a continuing international epidemic. Though there has been tremendous progress in international efforts to end the HIV/AIDS epidemic over the last 15 years (1), an estimated 2.1 million new (incident) cases were reported in 2015 (2). Despite this, the number of new HIV cases in high-income countries is relatively low with an average diagnostic rate of 6.3 per 100,000 for the Organisation for Economic Co-operation and Development (OECD) countries included in the 2014 HIV and AIDS surveillance report (3). While Canada’s rate of new diagnoses has been lower than the average of OECD countries, it still lags behind other countries such as the Netherlands, Germany, Sweden and Finland.
The Public Health Agency of Canada (PHAC) works in partnership with provincial and territorial governments, other federal departments and non-governmental organizations to address HIV/AIDS in Canada, contribute to the global efforts to eliminate HIV/AIDS, and monitor progress towards Canada’s Federal Initiative to Address HIV/AIDS. The annual publication of HIV surveillance data is part of PHAC’s mandate to collect, analyze and report on surveillance data at the national level (4).
The objective of this report is to provide a descriptive overview of the epidemiology of all reported diagnoses of HIV in Canada up to 2016 by geographic location, sex, age group, exposure category and race/ethnicity, as well as data on the number of infants perinatally exposed to HIV and the proportion of these infants receiving antiretroviral therapy (ART). In the past, HIV data, in combination with AIDS surveillance data, were published annually by PHAC in a stand-alone report entitled HIV and AIDS in Canada—Surveillance Report (3). This is the first iteration of the report to be published under a new title in the Canada Communicable Disease Report (CCDR). Note that a separate surveillance report for 2016 AIDS cases also appears in this issue of CCDR (5). The data in these reports replace all previously published data in the HIV and AIDS surveillance series as they represent the most recent information available. Supplementary information, including data tables and exposure category definitions are available online in a web supplement on the CCDR website (6).
Methods
Data used to prepare this HIV surveillance report came from three different sources: the national HIV/AIDS Surveillance System (HASS) maintained by PHAC, the data collected through immigration medical screening for HIV by Immigration, Refugees and Citizenship Canada (IRCC) and the Canadian Perinatal HIV Surveillance Program (CPHSP).
HIV/AIDS Surveillance System
HASS is a passive, case-based surveillance system that collates non-nominal data on people diagnosed with HIV infection. Details on HASS’s methods, including data collection processes, data management, data quality control, analysis and the classification and categorization of population subgroups have previously been described (3). In short, data, including but not limited to, age, sex, race/ethnicity and risks associated with the transmission of HIV (exposure categories) are voluntarily submitted to PHAC from all provincial and territorial public health authorities. Several limitations are present with regards to race/ethnicity and exposure category data submitted by the provinces. In particular, Quebec does not submit exposure category or race/ethnicity information for HIV cases to PHAC. For Ontario, limited exposure category information was available for reported HIV cases before 2009 and no race/ethnicity data were available for reported HIV cases before 2009. Race/ethnicity data for British Columbia were not submitted for the current reporting year and all historic ethnicity data have been removed at their request pending a review of reporting practices of these data.
Cases reported to PHAC must meet the national case definition (7). Provinces and territories provide data through the National Case Reporting Form (3) or through a secure electronic dataset transmission. All raw data (paper forms and electronic datasets) are retained in compliance with the Directive for the collection, use and dissemination of information relating to public health (PHAC, 2013, unpublished document). Assessment of the quality of data, such as the detection of duplicate entries, is handled by the provinces and territories prior to submission to PHAC. The data presented in this surveillance report represent HIV cases diagnosed on or before December 31, 2016 that were submitted by provincial and territorial surveillance programs to PHAC up to June 7, 2017.
In this surveillance report, the term “cases” or “reported cases” refers to individuals diagnosed by a province or territory in a given year and reported to PHAC. Since surveillance data describe only the diagnosed portion of the epidemic, statistical modelling and additional sources of information are used to produce estimates that describe the overall HIV epidemic in Canada, including people with diagnosed and undiagnosed HIV infection (8).
Immigration medical screening for HIV
All foreign nationals applying for permanent residence and some applying for temporary residence must undergo an immigration medical examination (IME), either in Canada or overseas administered by the IRCC. The IRCC conducts mandatory routine HIV screening on all applicants 15 years of age and older, as well as those under the age of 15 who have certain risk factors (9). The IRCC provides PHAC with non-nominal data collected during the IME, including demographic information as well as the year of testing (for those tested in Canada) or the year the applicant landed in Canada (for those tested overseas). Data relating to HIV diagnosed through an IME were extracted in January 2017; however, due to reporting delays only data up to the end of 2015 were provided.
Canadian Perinatal HIV Surveillance Program
National data on the HIV status of infants exposed perinatally to HIV infection are collected through the CPHSP, an initiative of the Canadian Pediatric AIDS Research Group (CPARG). The CPHSP is a sentinel-based surveillance system that collects data on all identified infants and children in Canada born to mothers who are known to be infected with HIV, including those born outside Canada who are receiving care for HIV infection. Data were obtained through a national, non-nominal, confidential survey of infants known to participating pediatricians in tertiary care centres and specialists in HIV clinics across Canada. Additional information on CPHSP methodology has been described previously (3). The data relating to perinatal surveillance until the end of 2016 presented in this surveillance report were extracted from CPHSP's database in July 2017.
Analysis
Microsoft Excel 2010 and SAS Enterprise Guide (SAS EG) v5.1 software were used for data cleaning and analysis. Standardized data recoding procedures were applied to all submitted provincial and territorial datasets to create a national dataset for analysis. No statistical procedures were used for comparative analysis, nor were any statistical techniques applied to account for missing data. It is worth noting that different HIV reporting requirements and practices exist across the country (10) and that completeness of some epidemiological information varies between provinces and territories; as such, when percentages were calculated, missing data were excluded.
The term “adult” is used throughout the report when examining specific variables such as exposure category. For the purposes of this report, an “adult” is anyone aged 15 years or older.
With the exception of cases where data suppression was requested by the province or territory, data in tables with small cell sizes (n≤5) were not suppressed, since disclosure is not deemed to pose any risk of identifying individual cases. These procedures are in line with PHAC’s Directive for the collection, use and dissemination of information relating to public health. The data were verified by the provinces and territories to ensure accuracy. Key findings are summarised in this manuscript. Additional tables can be found in the web supplement (6).
Results
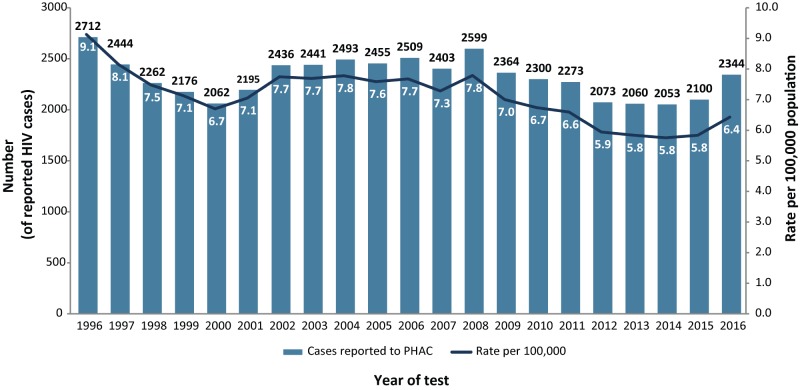
A total of 2,344 new cases of HIV were reported in Canada in 2016, representing an 11.6% increase from the number of cases reported in 2015 (2,100 cases). This is the highest number of annual HIV cases reported since 2009 (2,364 cases) and corresponds to an increase in the national diagnosis rate from 5.8 per 100,000 population in 2015 to 6.4 per 100,000 population (Figure 1).
Figure 1. Number of reported HIV cases, including diagnostic rate, by year of test—Canada, 1996-2016.
Abbreviation: PHAC, Public Health Agency of Canada
Disaggregated data by year are not available before 1995 for some jurisdictions
In Canada, a cumulative total of 84,409 cases of HIV have been reported to PHAC since HIV reporting began in 1985. A steady decrease of reported HIV cases was observed up until the year 2000 (2,062 cases) and then a short rise until a plateau from 2002 to 2008, when the annual number of reported HIV cases fluctuated between 2,403 and 2,599. The number of reported HIV cases then gradually declined from 2008 to 2014, followed by an increase in 2015 and 2016.
Geographic distribution
In 2016, Ontario accounted for the highest number and proportion of reported HIV cases (n=881, 37.6%), followed by Quebec (n=593, 25.3%) and Alberta (n=282, 12.0%).
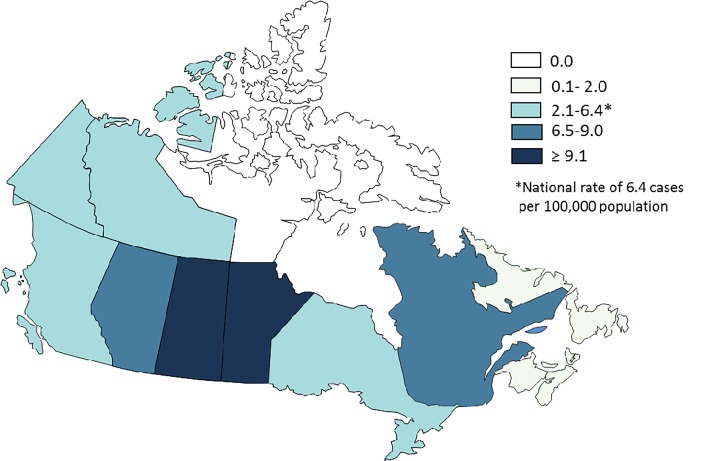
The provincial and territorial HIV diagnosis rates reveal notable variations across the country. In 2016, Saskatchewan, which accounted for 7.4% (n=174) of the total reported new HIV cases, continued to have the highest diagnosis rate of HIV at 15.1 per 100,000 population, more than double that of the overall Canadian rate. Manitoba, representing 5.4% (n=126) of the 2016 HIV cases, accounted for the next highest diagnosis rate of HIV at 9.5 per 100,000 population, followed by Quebec (7.1 per 100,000 population) and Alberta (6.6 per 100,000 population). The diagnosis rates in all other provinces and territories were below the national rate of 6.4 per 100,000 population (Figure 2, Supplementary Table 1, Supplementary Table 2, Supplementary Table 3) (6).
Figure 2. HIV diagnosis rate (per 100,000 population) by province and territory—Canada, 2016.
Population data source: Annual Demographic Statistics, Demography Division, Statistics Canada, October 2016
Age group and sex distribution
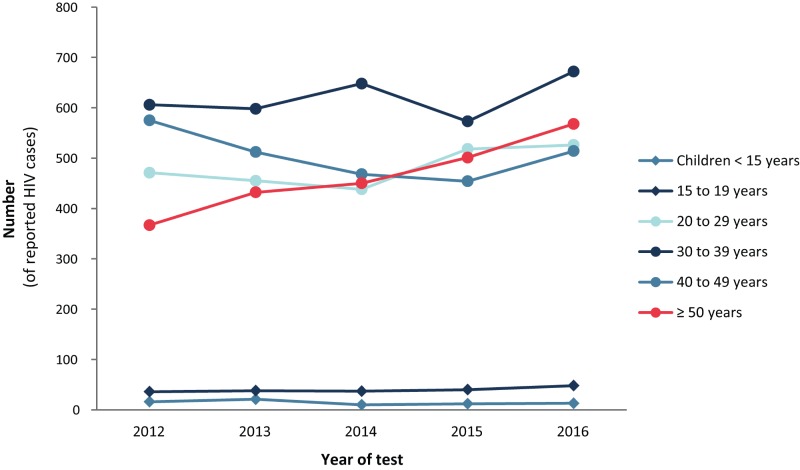
Data on age groups were available for 99.9% of reported HIV cases for 2016. Since 1985 in Canada, 37.2% of reported HIV cases have been diagnosed among people 30–39 years old. In 2016, those 30–39 years old still represented the group with the most new HIV cases (28.7%) but at a lower proportion than previous years. Cases 30–39 years old experienced the highest increase from 2015 to 2016 at 17.3%, followed closely by those 50 years of age or older at 13.4%.
For the past five years, the largest increase with respect to the proportion of HIV cases by age was observed in cases 50 years of age and older, increasing 6.6% from 2012 to 2016 (17.7% to 24.3%). The largest decline was found among those 40–49 years old, decreasing 5.8% from 2012 to 2016 (27.8% to 22.0%). Youth aged 15–19 years old represented 2.1% of cases in 2016. This group has experienced a small but steady increase in the number of HIV cases reported for the past five years, while HIV cases reported in children (<15 years of age) has remained fairly consistent over the same time period when compared with all other age groups (Figure 3, Supplementary Table 3, Table 6) (6).
Figure 3. Proportion of reported HIV cases by age group and year of test—Canada, 2007–2016.
Data on sex were available for 99.6% of reported HIV cases in 2016. In Canada, males have consistently accounted for a larger percentage of reported HIV cases than females. Over the past decade, the annual proportion of reported HIV cases among female adults (≥ 15 years) has remained stable at approximately one quarter of new cases. This trend was also observed in 2016 with females comprising 23.3% of all reported cases (Supplementary Table 2, Supplementary Table 4, Supplementary Table 5, Supplementary Table 6) (6).
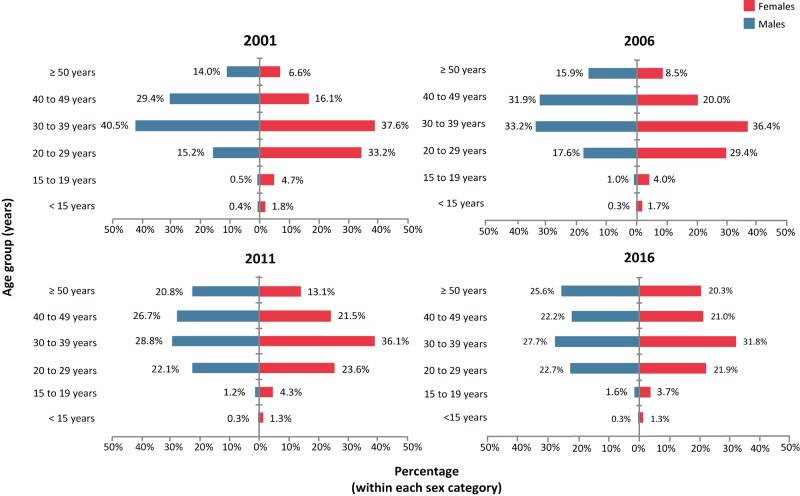
Over the past few years there have been increases in the proportion of HIV cases in the older age groups for both sexes. This trend continued in 2016, with a large proportion of cases aged 50 years and older for both sexes, specifically 25.6% in males and 20.3% in females (Figure 4). There has also been a shift over time in the age distribution for both sexes. While historically, HIV cases have been more frequent in younger age groups for females and older age groups for males, there has been an 11.3% decrease among females aged 20–29 and an increase of 7.5% in the corresponding male age group since 2001. In both sexes, cases aged 30–39 were still the highest proportion of HIV cases accounting for 27.7% and 31.8% of males and females respectively in 2016 (Figure 4).
Figure 4. Age group distribution of reported HIV cases by sex—Canada, 2016 1.
1 Denominators used to calculate percentages exclude "sex not reported/transsexual/transgender" and "age group not reported"
Exposure category distribution
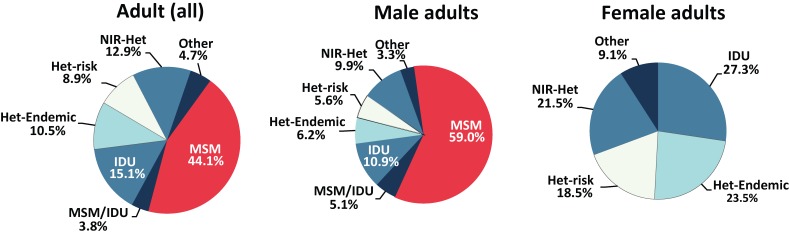
The men who have sex with men (MSM) exposure category continued to represent the largest number and proportion of all reported HIV cases in adults. In 2016, among adults whose exposure category was known (61.6% of all cases), slightly less than half (44.1%) were attributed to the MSM exposure category. The second highest reported exposure category was heterosexual contact (32.3%), with a fairly even distribution of HIV cases attributed to heterosexual contact among people born in a country where HIV is endemic (Het-Endemic, 10.5%), heterosexual contact with a person at-risk (Het-Risk, 8.9%) and heterosexual contact with no identified risk (NIR-Het, 12.9%). The third-most frequently reported exposure category among adults was injection drug use (IDU), accounting for 15.1% of reported HIV cases (Figure 5, Supplementary Table 7) (6). No major changes in the proportions in exposure categories were noted between 2015 and 2016.
Figure 5. Proportion of reported HIV cases among all adults (≥ 15 years old), adult males and adult females by exposure category—Canada, 2016 1,2.
Abbreviations: Het-Endemic, heterosexual contact among people born in a country where HIV in endemic; Het-Risk, heterosexual contact with a person at-risk; HIV, human immunodeficiency virus; IDU, injection drug use; MSM, men who have sex with men; MSM/IDU, men who have sex with men and use injection drugs; NIR-Het, heterosexual contact with no identified risk
1 Percentages are based on the total number of reported cases excluding "NIR" and "not reported" cases. Note that exposure category data were not available for Quebec. Both male and female charts exclude HIV cases where sex was not reported or reported as transsexual or transgender
2 "Other" includes recipient of blood/clotting factor, unspecified exposure routes listed as “other” and Alberta, cases identified as "out of country”
The distribution of HIV cases among adult males and females varied with respect to exposure category. In 2016, the MSM exposure category continued to account for the greatest proportion (59.0%) of reported HIV cases among adult males, followed by any type of heterosexual contact (21.6%) and IDU (10.9%). Among adult females, heterosexual contact accounted for 63.5% of reported cases (23.5% Het-Endemic, 21.5% NIR-Het and 18.5% Het-Risk), followed by IDU (27.3%). With respect to heterosexual contact, there was a substantial difference between males and females in the Het-Endemic exposure category. Het-Endemic cases among males accounted for 6.2% compared with 23.5% among females. The IDU exposure category accounted for slightly over one-quarter of adult female HIV cases (27.3%), compared with 16.0% of adult male HIV cases (10.9% via IDU exposure and up to 5.1% in the MSM/IDU exposure category (Figure 5, Supplementary Table 8, Supplementary Table 9, Supplementary Table 10, Supplementary Table 11) (6).
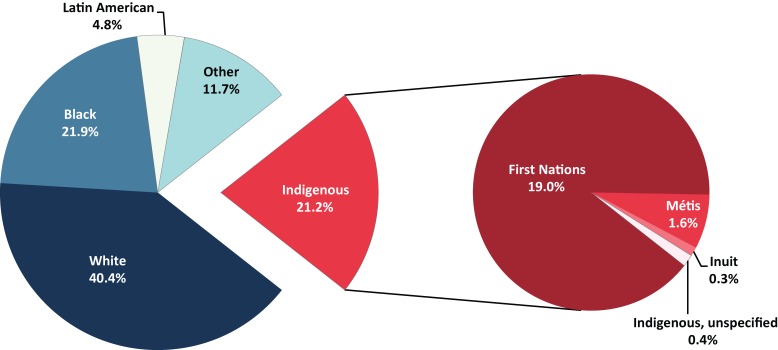
Race/ethnicity distribution
In 2016, information on race/ethnicity was available for nearly half (48.6%) of reported HIV cases. Since 1998, when race/ethnicity data were first collected, the White race/ethnicity has accounted for the largest proportion of new HIV cases in Canada for all ages and sexes (44.4%). In 2016, less than half of the reported HIV cases with a known race/ethnicity were White (40.4%), followed by Black (21.9%) and Indigenous (21.2%). The Indigenous race/ethnicity was further broken down to 19.0% First Nations, 1.6% Métis, 0.4% Indigenous-unspecified and 0.3% Inuit. Between 2015 and 2016 the First Nations race/ethnicity subgroup experienced the largest increase (29.9%) in case counts of all reported races/ethnicities and Indigenous subgroups (Figure 6, Supplementary Table 12) (6).
Figure 6. Proportion of reported HIV cases (all ages) by race/ethnicity (including the Indigenous subgroups)—Canada, 2016 1,2,3,4.
1 Race/ethnicity information was not available for Quebec and British Columbia
2 Excludes cases where race/ethnicity was not reported
3 Latin American includes, for example, Mexican, Central American and South American
4 Other includes, for example, Pakistani, Sri Lankan, Bangladeshi, Armenian, Egyptian, Iranian, Lebanese, Moroccan, Chinese, Japanese, Vietnamese, Cambodian, Indonesian, Laotian, Korean, Filipino, Somali, Haitian and Jamaican
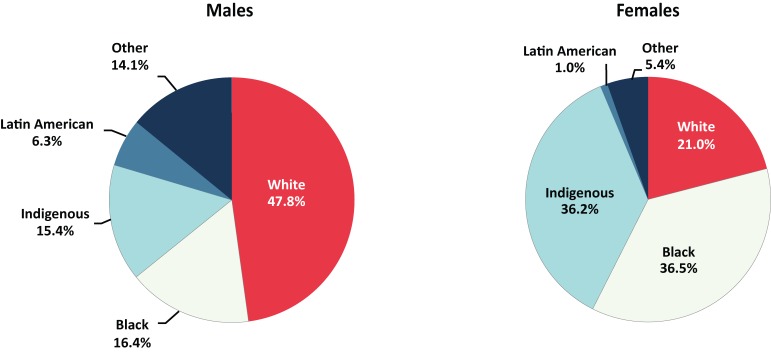
Variations were also observed in the race/ethnicity distribution by sex. In 2016, the majority of reported cases among males were of White race/ethnicity (47.8%), followed by Black (16.4%) and Indigenous (15.4%). By comparison, just over one-third of females were identified as Black (36.5%), followed by Indigenous (36.2%) and White (21.0%) (Figure 7, Supplementary Table 13, Supplementary Table 14) (6).
Figure 7. Proportion of reported HIV cases (all ages) by sex and race/ethnicity—Canada, 2016 1,2,3,4.
1 Race/ethnicity information is not available for Quebec and British Columbia
2 Denominators used to calculate percentages exclude HIV cases where race/ethnicity was "not reported" and HIV cases where sex was "not reported" or “reported” as transsexual or transgender
3 Latin American includes, for example, Mexican, Central American and South American
4 Other includes, for example, Pakistani, Sri Lankan, Bangladeshi, Armenian, Egyptian, Iranian, Lebanese, Moroccan, Chinese, Japanese, Vietnamese, Cambodian, Indonesian, Laotian, Korean, Filipino, Somali, Haitian and Jamaican
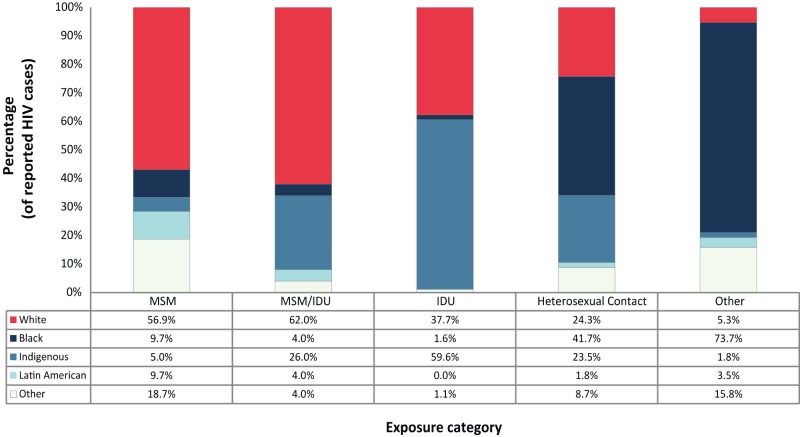
Race/ethnicity and exposure category distribution
Information on both race/ethnicity and exposure category was available for 47.4% of reported cases in 2016. In 2016 the majority of cases were reported as White within the MSM exposure category (56.9%). Of the cases attributed to IDU, almost all of the HIV cases were either Indigenous (59.6%) or White (37.7%). The main racial/ethnic group among reported cases attributed to heterosexual contact was Black (41.7%), 84.3% of whom were reported as Het-Endemic exposure (Figure 8, Supplementary Table 15) (6).
Figure 8. Proportion of reported HIV cases (all ages) by exposure category and race/ethnicity—Canada, 2016 1,2,3,4,5.
Abbreviations: IDU, injection drug use; MSM, men who have sex with men; MSM/IDU, men who have sex with men and use injection drugs
1 Race/ethnicity information is not available for Quebec and British Columbia
2 Excludes HIV cases where race/ethnicity or exposure category was "not reported"
3 Latin American includes, for example, Mexican, Central American and South American
4 Other race/ethnicity includes, for example, Pakistani, Sri Lankan, Bangladeshi, Armenian, Egyptian, Iranian, Lebanese, Moroccan, Chinese, Japanese, Vietnamese, Cambodian, Indonesian, Laotian, Korean, Filipino, Somali, Haitian and Jamaican
5 Other exposure category includes recipient of blood/clotting factor and unspecified exposure routes listed as “other”
Immigration medical screening for HIV
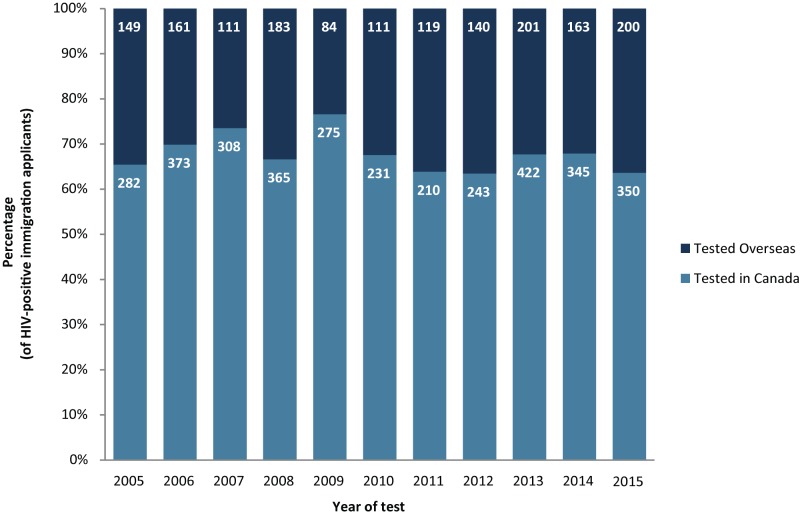
In 2015, there were 550 applicants for Canadian residency who tested positive for HIV. Of the 550, 350 underwent an IME in Canada and 200 underwent an IME overseas. Note that the data do not distinguish between those who eventually established residency in Canada and those who did not (Figure 9, Supplementary Table 16) (6).
Figure 9. Proportion of HIV-positive immigration applicants by testing location and year of test, 2005–2014 1,2.
1 Immigration, Refugees and Citizenship Canada, IRCC HIV Database as of July 2017. Immigration, Refugees and Citizenship Canada, IRCC HB Post-Arrival Health Public Health Liaison Unit Provincial Notifications - Overseas Notifications Database as of July 2017. Reproduced and distributed with the permission of Immigration, Refugees and Citizenship Canada
2 For applicants tested in Canada, the year refers to the year of the test. For applicants tested overseas, the year refers to the year the applicant landed in Canada
Of applicants who underwent an IME in Canada from 2002 to 2015, a total of 4,364 were diagnosed with HIV infection, at an average of 312 diagnoses per year (range: 210 to 422). In total, 57.1% of these HIV-positive applicants were male. The majority of all applicants who tested positive in Canada were either in the 30–39 years old (41.9%) or 40–49 years old (25.0%) age group. The greatest proportion of these HIV-positive applicants were tested in Ontario (54.7%), Quebec (25.2%), British Columbia (8.7%) and Alberta (7.6%) (Supplementary Table 17) (6).
Of applicants screened overseas from 2005 to 2015 who landed in Canada, 1,622 were diagnosed with HIV infection, at an average of 147 per year (range: 84 to 201). Just over half (51.4%) were female. The majority (40.0%) were 30 to 39 years old, followed by those 20 to 29 years old (25.3%). Ontario was the most common intended province of residence (33.4%), followed by Quebec (25.0%), Alberta (14.4%), British Columbia (12.9%) and Manitoba (8.7%). Among these HIV-positive applicants, 72.1% were born in HIV-endemic countries (Supplementary Table 17) (6).
Canadian Perinatal HIV Surveillance Program
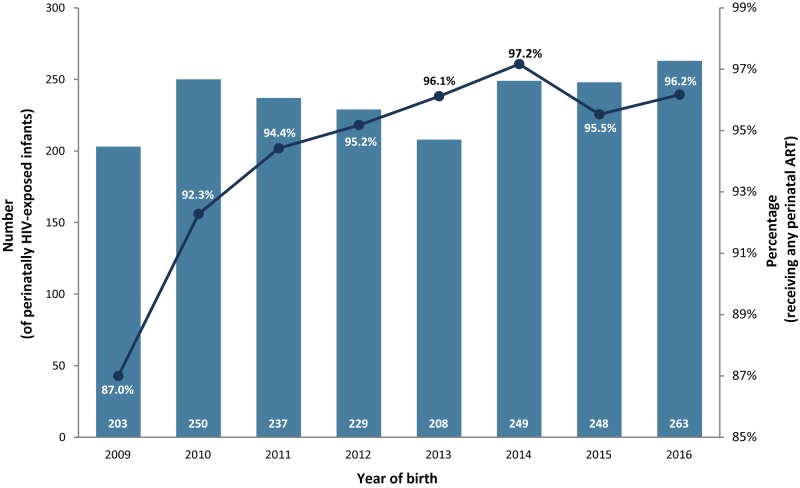
From 1984 to 2016, 4,849 infants in Canada were identified as being perinatally-exposed to HIV. The number of HIV-exposed infants reported per birth year between 2009 and 2016 fluctuated from a low of 203 in 2009 to a high of 263 in 2016 (Figure 10, Supplementary Table 18, Supplementary Table 19, Supplementary Table 20, Supplementary Table 21, Supplementary Table 22) (6).
Figure 10. Number of perinatally HIV-exposed infants and proportion of perinatally HIV-exposed infants receiving perinatal antiretroviral therapy by year of birth—Canada, 2009–2016.
Abbreviation: ART, antiretroviral therapy
Of the 263 perinatally-exposed infants born in 2016, one HIV transmission was confirmed in a mother not receiving any perinatal antiretroviral therapy (ART). The percentage of HIV-positive mothers receiving ART has increased over time and has been fairly stable since 2011, ranging between 94.4% (2011) to 97.2% (2014); in 2016, the percentage was slightly lower than 2014 at 96.2% (Figure 10, Supplementary Table 18) (6).
A review of all perinatally-exposed infants from 1984 to 2016 showed that 73.8% were born to mothers who acquired HIV infection through heterosexual contact (71.0% in 2016) and 22.8% were attributed to IDU exposure (22.3% in 2016) (Supplementary Table 19) (6).
With respect to the race/ethnicity distribution of perinatally-exposed infants from 1984 to 2016, 49.8% were reported as Black, 23.8% as White and 17.8% as Indigenous. In 2016, the Black race/ethnicity remained the most frequently reported race/ethnicity with a proportion (48.7%) similar to that seen in 1984–2016. The proportion of infants of Indigenous race/ethnicity has progressively increased reaching a high of 25.5% in 2016 and the proportion of infants of White race ethnicity has decreased to a low of 11.8% (Supplementary Table 20) (6).
Maternal region of birth for the majority of infants from 1984–2016 was North America (42.4%), Africa (38.2%) or the Caribbean (9.8%) (Supplementary Table 21). For the same time period, the highest proportion of perinatally HIV-exposed infants was reported in Ontario (34.6%), followed by Quebec (25.7%) and Alberta (14.1%) (Supplementary Table 22) (6).
Discussion
In 2016, there was an 11.6% increase in the number of HIV diagnoses compared with 2015 and this represents the highest rate since 2011. A number of possibilities exist to explain this increase in cases including increased testing due to the implementation of provincial testing initiatives (11), (12), (13).
The majority of increases were observed in Quebec, Alberta, Manitoba and Ontario although, overall, Saskatchewan had the highest absolute rate. Across age, sex and race/ethnicity, the greatest increases were observed among those 30–39 years old, the adult male sex and First Nations ethnicity respectively. It is also important to note that for Quebec, the reported increase can in part be explained by a partial shift in 2016 to nominal testing from non-nominal testing as non-nominal cases were not all previously captured for federal reporting.
At the national level, the differences previously observed between the age distribution of males and females have been reduced over the past five years, resulting in a similar age distribution between sexes for 2016. This effect is due to increased proportions diagnosed within older age groups for both sexes. The proportion of HIV diagnoses among Canadians 50 years and older has been increasing gradually since 1985. It is possible that the observed change has been driven by a population with unique risk factors such as higher proportions of widowed and divorced people engaging in new relationships, lower proportions of protected sex due to lack of pregnancy concerns, and a stronger stigma associated with discussion of sexual and drug habits with doctors in this older age group (14).
At the national level, differences continued to be observed between males and females with respect to exposure category and race/ethnicity distribution. Men who have sex with men, the most frequent exposure category in males, was associated with the White race/ethnicity, while heterosexual contact and IDU, the two most predominant exposure categories in females, were associated with people of Black and Indigenous races/ethnicities respectively. Although the White race/ethnicity was the most common racial/ethnic group, both Indigenous and Black people were disproportionately represented as they each make up less than 5% of the population in Canada (15), (16), but account for more than 20% individually of the newly reported HIV cases. Of note, however, ethnicity data were available in only about half of reported cases.
Trends in exposure category have shifted since HIV reporting began in 1985. In the early stages of the epidemic, over 80% of all reported HIV cases with known exposure category were attributed to MSM and although this exposure category is still predominant in Canada, the proportion has decreased over the years. Heterosexual contact and IDU exposure remained the second and third most predominant HIV exposure categories in Canada respectively.
Strengths and limitations
The 2016 HIV in Canada – Surveillance Report is the primary source of national data on reported new HIV cases in Canada. The data contained within this report provide information for policy and program development and assessment, as well as public health action. While details regarding the data limitations of HASS have been previously published (3), several limitations should be highlighted. First, data in this report are deemed provisional and may be subject to change in future HIV surveillance reports, as data are updated. Differences between the data published in this report and the data issued in previous national, provincial and territorial surveillance reports may be due to reporting delays or differences in when the data were extracted from the various surveillance databases. Where such differences are noted, it is recommended that data from the most recent provincial and territorial reports be used.
Second, HASS is a passive, case-based surveillance system that collates data submitted voluntarily to PHAC, on a yearly basis, from all provincial and territorial public health authorities, as opposed to active case solicitation. As a result, it is difficult to ascertain whether all individuals with HIV infection are being identified and reported. The accuracy of the data is partially a function of timely reporting and updates to PHAC from the provinces and territories. Some degree of lag does occur, creating a reporting delay. In addition, reporting of HIV cases for individuals younger than two years of age and those diagnosed prior to immigration also varies among provinces and territories. Occasionally there can be changes to provincial reporting practices which can impact the data.
Third, the identification and removal of duplicate reports of new diagnoses is difficult due to the non-nominal nature of HIV reporting in some jurisdictions. Where possible, provinces and territories review and assess the inclusion of duplicate reports in order to provide as accurate a picture as possible of the number of new individuals who have tested positive for HIV. Some provinces (e.g., Quebec), take a conservative approach to removing potential duplicates, including the exclusion of results from anonymous tests. For jurisdictions that use such an approach, the data presented in this report reflect the minimum number of new HIV diagnoses in that jurisdiction.
Fourth, across the provinces and territories, there is no standardized approach to the handling of HIV cases previously diagnosed out of country or out of province/territory, with some provinces and territories counting them as new cases and others excluding them. Additionally, varying approaches are also applied to HIV diagnoses under the age of two. As a result of both of these, there exists the possibility for small over- or under-reporting of new diagnoses depending on the provincial/territorial rules.
Finally, there are several limitations associated with the reporting of exposure category and race/ethnicity. As noted, little to no exposure category or race/ethnicity information for HIV cases is available from Quebec and Ontario, and no race/ethnicity information is available from British Columbia. Therefore national trends presented in this report may not be fully representative and must be interpreted with caution.
Conclusion
Canada experienced an increased number and rate of reported HIV cases in 2016. Although this diagnostic rate was lower than in all years prior to 2012, it is the highest of the past five years. Further investigation and additional data are needed to determine the significance and cause of this increase. PHAC will continue to collect and report on HIV surveillance data to observe trends and monitor progress toward the goal of reducing the burden of HIV infection in Canada and internationally.
Acknowledgements
PHAC would like to acknowledge the following individuals from the provincial and territorial HIV/AIDS programs for their contribution and participation:
Sumina Fathima, Alberta Health
Rosa Maheden, Alberta Health
Mariam Osman, Alberta Health
Ari Bitnun, Canadian Perinatal HIV Surveillance Program
Laura Sauvé, Canadian Perinatal HIV Surveillance Program
Claire Lafrance, Immigration, Refugees and Citizenship Canada
Jacklyn Quinlan, Immigration, Refugees and Citizenship Canada
Clinical Prevention Service, Surveillance and Epidemiology, BC Centre for Disease Control
Carla Loeppky, Manitoba Health
Rita RaaFat Gad, New Brunswick Department of Health
Shelley Landsburg, New Brunswick Department of Health
Sophie Wertz, New Brunswick Department of Health
Susan Earles, Health and Community Services, Population Health Branch, Newfoundland and Labrador
Jennifer Phillips, Health and Community Services, Population Health Branch, Newfoundland and Labrador
Heather Hannah, Department of Health and Social Services, Northwest Territories
Angela Fitzgerald, Nova Scotia Department of Health and Wellness
Angie Mullen, Nunavut Department of Health
Elaine Randell, Nunavut Department of Health
Abigail Kroch, Ontario Treatment Network
Juan Liu, Public Health Ontario
Alex Marchand-Austin, Public Health Ontario
Doug Sider, Public Health Ontario
Michael Whelan, Public Health Ontario
Marguerite Cameron, Prince Edward Island Department of Health and Wellness
Stacey Burns, Prince Edward Island Department of Health and Wellness
Raphaël Bitera, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Micheline Fauvel, Laboratoire de santé publique du Québec, Institut national de santé publique du Québec
Maureen Hastie, Laboratoire de santé publique du Québec, Institut national de santé publique du Québec
Raymond Parent, Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec
Diane Sylvain, Laboratoire de santé publique du Québec, Institut national de santé publique du Québec
Helen Bangura, Saskatchewan Ministry of Health
John Manalo, Saskatchewan Ministry of Health
Lori Strudwick, Yukon Communicable Disease Control
Rachelle Wallace, Yukon Communicable Disease Control
Sabrina Plitt, Public Health Agency of Canada (Alberta)
Elsie Wong, Public Health Agency of Canada (British Columbia)
Suresh Khatkar, Public Health Agency of Canada (Manitoba)
Marie LaFreniere, Public Health Agency of Canada (Nova Scotia)
Ashleigh Sullivan, Public Health Agency of Canada (Ontario)
Conflict of Interest: None.
Funding: This work was supported by the Public Health Agency of Canada as part of its core mandate.
References
- 1.UNAIDS. Prevention Gap Report, Joint United Nations Programme on HIV/AIDS, Geneva, 2016. http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf
- 2.World Health Organization. World Health Statistics 2017: monitoring health for the SDGs, Sustainable Development Goals, Geneva, 2017. http://www.who.int/gho/publications/world_health_statistics/2017/en/
- 3.Public Health Agency of Canada. HIV and AIDS in Canada: Surveillance Report to December 31, 2014, Minister of Public Works and Government Services Canada, Ottawa, 2015. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-aids-canada-surveillance-report-december-31-2014.html
- 4.Public Health Agency of Canada. Strengthening Federal Action in the Canadian Response to HIV/AIDS, Minister of Public Works and Government Services Canada, 14 August 2012. http://www.phac-aspc.gc.ca/aids-sida/fi-if/fa-if/2-eng.php. [Accessed 31 July 2017].
- 5.Jonah L, Bourgeois AC, Edmunds M, Awan A, Varsaneux O, Siu W. AIDS in Canada—Surveillance Report, 2016. Can Commun Dis Rep 2017;43(12):257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourgeois AC, Edmunds M, Awan A, Jonah L, Varsaneux O, Siu W. HIV in Canada—Supplementary tables, 2016 (Web exclusive). Can Commun Dis Rep 2017;43(12): Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2017-43/ccdr-volume-43-12-december-7-2017/hiv-2016-supplementary-tables.html [DOI] [PMC free article] [PubMed]
- 7.Public Health Agency of Canada. Case definitions for communicable diseases under national surveillance. Can Commun Dis Rep 2009;35 S2:1–121. [PubMed] [Google Scholar]
- 8.Public Health Agency of Canada. Summary: Estimates of HIV incidence, prevalence and proportion undiagnosed in Canada, 2014, Public Health Agency of Canada, Ottawa, 2015. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/summary-estimates-hiv-incidence-prevalence-proportion-undiagnosed-canada-2014.html
- 9.Immigration, Refugees and Citizenship Canada, Immigration Medical Examination Instructions, HIV Screening. 1 November 2013.
- 10.National (Canadian) Collaborating Centre for Infectious Disease. Notifiable Disease Database. http://nddb.ca/diseaseinfo/search/search_disease#search_disease. [Accessed 31 July 2017].
- 11.Region SH, Virus HI. (HIV) - Testing, December 2016. http://www.communityview.ca/pdfs/2016_shr_series5_hiv_testing.pdf. [Accessed 31 July 2017].
- 12.BC Centre for Disease Control. HIV in British Columbia: Annual Surveillance Report 2014, BC Centre for Disease Control, Vancouver, 2015. [Google Scholar]
- 13.Remis RS, Liu J. HIV/AIDS in Ontario: Preliminary Report, 2011, Toronto, August 2013. http://www.ohemu.utoronto.ca/doc/PHERO2011_report_preliminary.pdf
- 14.Public Health Agency of Canada. Questions & Answers: Prevention of sexually transmitted and blood borne infections among older adults. Minister of Public Works and Government Services Canada, Ottawa, 2015. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/reports-publications/questions-answers-adults.html
- 15.Statistics Canada. Aboriginal Peoples Highlight Tables, 2016 Census. http://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/abo-aut/Table.cfm?Lang=Eng&T=101&S=99&O=A
- 16.Statistics Canada. Statistics Canada Catalogue no. 98-400-X2016190, 2016 Census. http://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=0&GK=0&GRP=1&PID=110531&PRID=10&PTYPE=109445&S=0&SHOWALL=0&SUB=0&Temporal=2017&THEME=120&VID=0&VNAMEE=&VNAMEF=