Abstract
Objectives
Breastfeeding has short- and long-term health benefits for children and mothers, but US breastfeeding rates are suboptimal. Exposure to violence may contribute to these low rates, which vary by race/ethnicity. We studied: (1) whether patterns of violence exposure differ by race/ethnicity and (2) whether these patterns are associated with breastfeeding outcomes.
Methods
We conducted a secondary analysis of data drawn from self-report surveys completed by a convenience sample of low-income postpartum women (n=760) in upstate New York. Latent class analysis was used to identify groups of women with similar responses to seven violence measures, including childhood physical and/or sexual violence, experience of partner violence during or just after pregnancy (physical, emotional, verbal), and neighborhood violence (perceived or by ZIP code). Logistic regression and survival analysis were utilized to determine if classes were associated with breastfeeding initiation, duration, and exclusivity, controlling for demographics.
Results
Exposure to at least one form of violence was high in this sample (87%). We identified 4 classes defined by violence exposure (combining current and historical exposures). Violence exposure patterns differed between racial/ethnic groups, but patterns were inconsistently associated with breastfeeding plans or outcomes. For White women, history of violence exposure increased the likelihood of earlier breastfeeding cessation. By contrast, among Black women, history of violence exposure increased the likelihood of having a breastfeeding plan and initiating breastfeeding.
Conclusions for Practice
Some differences between violence exposure classes are likely due to the correlation between race/ethnicity and socioeconomic status in the community studied. Additional studies are warranted to better understand how exposure to violence is related to breastfeeding and how best to support women making decisions about intention, initiation, and duration of breastfeeding.
Keywords: Breastfeeding, exposure to violence, latent class analysis, domestic violence, neighborhood, vulnerable populations
Objectives
Breastfeeding has important, well-established short and long-term health benefits to the infant and mother (Eidelman et al., 2012; Ip et al., 2007; Office on Women’s Health, 2016). Numerous psychosocial factors are acknowledged to interfere with breastfeeding outcomes (initiation, duration, exclusive breastfeeding) and prenatal intention (plan) to breastfeed (Singh, Kogan, & Dee, 2007). There is a growing body of literature on women’s experiences of violence across the lifespan and its impact on birth outcomes, including breastfeeding (Sharps, Laughon, & Giangrande, 2007; Silverman, Decker, Reed, & Raj, 2006). In the United States (US), nearly 36% of women report lifetime physical abuse, rape, and/or stalking by intimate partners (Black et al., 2011). Significantly more Black non-Hispanic women (44%) and multiracial non-Hispanic women (54%) report lifetime experience of rape, physical violence, or stalking by an intimate partner compared to White non-Hispanic women (35%) (Black et al., 2011). Pregnancy is not protective against abuse. Four to eight percent of pregnant women in the US report experience intimate partner violence (IPV) (Sharps, Laughon, & Giangrande, 2007). Also, approximately 32% of US women report a history of childhood sexual abuse (CSA) and 19.5% report childhood physical abuse (Briere & Elliot, 2003).
The relationship between breastfeeding and IPV, prior to, during, and after pregnancy, has been a subject of several studies that show mixed results. Bair-Merritt and colleagues examined breastfeeding as one of several physical health outcomes of childhood exposure to IPV (Bair-Merritt, Blackstone, & Feudtner, 2006). Identifying only one study for inclusion in their review, they concluded that there was insufficient evidence of a relationship between the two (Bair-Merritt et al., 2006). A later study, using data from over 100,000 women, found lower rates of breastfeeding initiation and higher rates of early breastfeeding termination among women with IPV during pregnancy (Silverman et al., 2006). However, this relationship was not maintained in multivariable models. A study by Bullock et al. (2001) of 150 women showed no relationship between IPV and breastfeeding initiation or duration among low-income women. A more recent study of 6,410 mothers of infants showed similar results; there was no significant difference in the rate of breastfeeding by sexually assault experience, either in childhood or adulthood (Kendall-Tackett, Cong, & Hale, 2013).
Ogbo et al., (2017) examined exclusive breastfeeding (EBF) in the first month after birth among 17,564 live births in Australia; their findings show an early cessation of EBF among abused women compared to non-abused women. A large prospective cohort of 53,934 women reported that both past childhood abuse and recent IPV were associated with early cessation of breastfeeding (Sørbø, Lukasse, Brantsæter, & Grimstad, 2015). A study conducted in Brazil (N=564) identified a relationship between women’s exposure to severe IPV and early termination of exclusive breastfeeding (Hasselmann, Lindsay, Surkan, Vianna, & Werneck, 2016). Suboptimal breastfeeding (initiation and exclusivity) was associated with maternal lifetime IPV among African women (Misch & Yount, 2014). A study of feeding practices among Indian women demonstrated a relationship with IPV exposure and lower rates of exclusivity, but not initiation (Zureick-Brown, Lavilla, & Yount, 2015). Findings from a cluster randomized controlled trial with 2,111 Australian women and a cross-sectional study with 731 women from Sweden showed no difference in breastfeeding rates and EBF by IPV experiences (James et al., 2014; Finnbogadóttir & Thies-Lagergren, 2017). While several samples mentioned above had experiences of childhood and adult victimization, none of these studies included exposure to neighborhood violence in their analyses.
Similar to studies on the relationship between IPV and breastfeeding, studies of women survivors of CSA present mixed results on the association between experiencing CSA and breastfeeding intention and initiation. Kendall-Tackett (2007) reviewed the limited literature regarding sexual abuse and breastfeeding and concluded that women with a history of CSA, when compared with non-abused women, are more likely to intend to and initiate breastfeeding. A study of 78 Mexican American young adults did not show a significant association between CSA history and feeding choice (Bowman, Ryberg, & Becker, 2008). Coles et al. (2016) analyzed data from nearly 4,000 Australian women demonstrating no difference in rates of breastfeeding at six months by CSA experience.
When describing the pathways connecting women’s experiences of IPV and breastfeeding, Kendall-Tackett (2007) highlighted that some barriers related to breastfeeding are more prevalent in women in abusive relationships. These factors include smoking, shorter postpartum hospital stays, preterm deliveries, low birth weight, and non-supportive partners. Further, IPV- and childhood abuse-related trauma might impact cortisol levels in the mother, leading to a delayed milk supply post delivery. This delay might influence the women to quit breastfeeding as they might think that they are producing inadequate amount of breastmilk.
There is a scant body of literature on neighborhood context and its relationship to breastfeeding. Data from the National Survey of Children’s Health show that women from perceived safe neighborhoods had slightly higher rates of breastfeeding initiation (73.4% vs 68.0%). This difference shrank to less than 3% at 6 months postpartum for breastfeeding duration (38.1% vs. 35.3%). Neighborhood safety was not found to be significant in multivariable models (Singh et al., 2007). A study among a sample of predominately unmarried urban women (N=4228) found neighborhood socioeconomic context was associated with higher odds of initiating and sustaining breastfeeding (Burdette, 2013).
In sum, studies to date related to breastfeeding and violence exposure across the lifespan are limited. No studies were found that combined both early life and current, and interpersonal and community, exposure to violence. This preliminary study seeks to fill this gap by creating exposure patterns combining prior and current interpersonal with neighborhood exposure to violence. Latent class analysis (LCA) is a method to identify distinct groups of observations (called classes) that have common features, and combine a variety of measures to a smaller number of classes, which may represent common patterns of experience. LCA has been used in a variety of social and behavioral science areas, including violence exposure and association with mental health (Cavanaugh et al., 2012; Lambert, Nylund-Gibson, Copeland-Linder, & Ialongo, 2010). Here we examine classes of maternal violence exposure by race and ethnicity. This analysis may help us understand the relationship between these patterns of experience and an outcome such as breastfeeding behavior. Our research questions were: (1) do patterns of violence exposure differ by race and ethnicity and (2) are these patterns associated with breastfeeding outcomes, including initiation, duration, and exclusivity?
Methods
Secondary data analysis was conducted on data drawn from self-report surveillance surveys completed by a convenience sample of postpartum women (n=760) in upstate New York (2009–2011). As described in Dozier et al. (2012), this surveillance survey was distributed to all women with infants between 5–7 months old who received well-baby care at 4 low-income serving practices (4 pediatric; 1 family medicine). Mailings occurred at approximately 5–7 months postpartum and included items about the pre-pregnancy, prenatal, and postpartum periods. A second mailing was sent 3 weeks later. Other follow-up (e.g., by telephone) was not possible because only addresses were provided by the participating practices. The response rate was 21%. The over 80 survey items were primarily based on US Centers for Disease Control’s Pregnancy Risk Assessment Monitoring System (version 6) (CDC, 2016). Only women who answered all questions pertaining to violence in their past and present were included in the analysis (n=499). Of these 499 women, 49 were excluded: 40 answered “Mixed or Other Race” and 9 did not answer the race question.
The outcome, breastfeeding, was based on maternal self-report, and included initiation (ever breastfed), duration (did breastfeeding continue through 4 weeks and through 13 weeks), and exclusivity (was breastfeeding the only source of nutrition for the infant at 4 weeks and at 13 weeks).
The primary independent variables were exposure to violence, including past and current violence exposure in several domains. Specific survey items are footnoted in Table 1. [TABLE 1] Questions regarding arguments with husband or partner and emotional cruelty by husband or partner were based on the Stressful Life Events Questionnaire originally developed by Barnett et al (1993) and adapted by O’Connor (2013). Women rated how safe they felt during the day and during the night in their neighborhood on 4-level scales from very safe to not safe, which we dichotomized to very safe during both the day and the night vs. usually, somewhat, or not safe either during the day or at night. Nine ZIP codes in the service area surveyed are known for substantially higher poverty and violence rates. These geographically-contiguous ZIP codes were coded as inner city, and the remaining ZIP codes were not inner city. Demographic information gathered are listed in Table 1 and used as covariates.
Table 1.
Sample description
| White (n=133) |
Black (n=197) |
Hispanic (n=120) |
Total (n=450) |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| English speaking | 10 6 |
80 | 179 | 91 | 44 | 37 | 329 | 73 |
| Age (years) | ||||||||
| <20 | 5 | 4 | 16 | 8 | 16 | 13 | 37 | 8 |
| 20–29 | 86 | 65 | 118 | 60 | 72 | 60 | 276 | 61 |
| 30–49 | 39 | 29 | 53 | 27 | 22 | 18 | 114 | 25 |
| Body Mass Index | ||||||||
| Underweight | 9 | 7 | 8 | 4 | 4 | 3 | 21 | 5 |
| Healthy weight | 64 | 48 | 71 | 36 | 48 | 40 | 183 | 41 |
| Overweight | 29 | 22 | 55 | 28 | 40 | 33 | 124 | 28 |
| Obese | 31 | 23 | 63 | 32 | 26 | 22 | 120 | 27 |
| Depressed | 35 | 26 | 51 | 26 | 35 | 29 | 121 | 27 |
| Had a breastfeeding plan | 61 | 46 | 75 | 38 | 49 | 41 | 185 | 41 |
| Smoker | ||||||||
| Never | 49 | 37 | 99 | 50 | 50 | 42 | 198 | 44 |
| Current | 49 | 37 | 51 | 26 | 41 | 34 | 141 | 31 |
| Former smoker | 35 | 26 | 49 | 25 | 29 | 24 | 113 | 25 |
| Alcohol consumption | ||||||||
| Never | 29 | 22 | 73 | 37 | 50 | 42 | 152 | 34 |
| Current | 73 | 55 | 97 | 46 | 53 | 44 | 223 | 50 |
| Former drinker | 31 | 23 | 32 | 16 | 17 | 14 | 80 | 18 |
| Work & school attendance | ||||||||
| Neither | 73 | 55 | 79 | 40 | 58 | 48 | 210 | 47 |
| Work | 45 | 34 | 73 | 37 | 34 | 28 | 152 | 34 |
| School | 15 | 11 | 22 | 11 | 22 | 18 | 59 | 13 |
| Work and School | 0 | 0 | 18 | 9 | 8 | 7 | 26 | 6 |
| Completed high school | 10 9 |
82 | 152 | 77 | 82 | 68 | 343 | 76 |
| Any prior birth | 59 | 44 | 67 | 34 | 54 | 45 | 180 | 40 |
| Violence exposure | ||||||||
| Sexually abused as a childa | 29 | 22 | 47 | 24 | 32 | 27 | 108 | 24 |
| Physical abuse (when younger) b | 47 | 35 | 43 | 22 | 41 | 34 | 131 | 29 |
| Physical abuse (during pregnancy) b | 16 | 12 | 30 | 15 | 12 | 10 | 58 | 13 |
| Argue with husband or partner c | 65 | 49 | 91 | 46 | 53 | 44 | 209 | 46 |
| Emotional cruelty of husband or partner d | 24 | 18 | 47 | 24 | 22 | 18 | 93 | 21 |
| Perceived unsafe neighborhood safety e | 73 | 55 | 79 | 40 | 54 | 45 | 206 | 46 |
| Inner city zip codef | 55 | 41 | 160 | 81 | 96 | 80 | 311 | 69 |
| History of Violenceg | ||||||||
| Yes | 57 | 13 | 69 | 15 | 49 | 11 | 175 | 39 |
| No | 76 | 17 | 128 | 28 | 71 | 16 | 275 | 61 |
Have you ever been sexually abused? (as a child) (Yes)
Did anyone close to you hit, slap, kick, choke or physically abuse you in any other way? Check all that apply: Never, when I was younger; In the year before my pregnancy; during pregnancy, since baby’s birth
I had a serious argument with my husband or partner
My husband or partner was emotionally cruel to me (Yes, affected me a lot and Yes affected me a little)
Calculated variable combining responses from How safe do you feel during the day in the neighborhood you live in now? and How safe do you feel at night in the neighborhood you live in now?; response option of Very safe, usually safe, somewhat safe; not safe. Dichotomized to very safe during both the day and the night vs. all other responses
Nine geographically contiguous zipcodes with a concentration of poverty and violence
Calculated combining answering “yes” to either sexual abuse as a child or physical abuse when younger
LCA was used to identify groups of women with similar responses to the seven violence measures described above. The number of classes for each group was based on several model fit statistics (Akaike information criterion [AIC] and adjusted Bayesian information criterion [BIC]) and interpretability of classes. In addition, we tested for measurement invariance by race and ethnicity. The PROC LCA macro for SAS was used for LCA (Collins & Lanza, 2010) and SAS was used for all other analyses. We also explored using the violence measures that differentiated the classes most strongly associated with breastfeeding outcomes to predict these outcomes directly.
Logistic regression was utilized to determine if classes were associated with breastfeeding initiation. Survival analysis was conducted for breastfeeding duration and exclusivity outcomes. For all models, the covariates (dichotomous, except as noted) included: English spoken, age (3 categories), smoking history, alcohol history, high school completion, self-reported depression (pre- or postnatal), school and work status, body mass index (BMI; 3 categories; underweight omitted due to small sample size), and prior births. We controlled for BMI in these models, because BMI is negatively correlated with initiation of breastfeeding (Krause, Lovelady, & Ostbye, 2011). Because having a breastfeeding plan was a strong predictor of breastfeeding outcomes, models were run with and without this variable.
Results
Most of the women in this study were between 20 and 29 years old. See Table 1 for demographic information by race and ethnicity. The most common forms of violence exposure were inner city ZIP code (69%), perceived neighborhood safety (46%), and arguing with husband or partner (46%). The least commonly reported exposure was physical abuse during pregnancy (13%). Overall, 87% of the sample reported at least one exposure to violence (not in table). The same proportion of Black and Hispanic women reported at least one exposure to violence (92%), while fewer White women reported at least one exposure (74%; P<.001).
We started with a constrained model that used the same class structure for all race/ethnicity groups. In this model, AIC suggested 5 classes, BIC suggested 3 classes, and the adjusted-BIC suggested 4 classes as the best fit for this model (Online Resource 1). After reviewing the interpretability of the classes for each race/ethnicity, we chose the 4-class model, because the fourth class was meaningfully different from the first three, but the fifth class did not improve interpretation. We then considered an unconstrained model to test measurement invariance by race/ethnicity; measurement invariance is an assumption that the classes are the same for each group. Measurement invariance was not rejected in the three- and four-class models (P<.08), but was rejected in the five-class model (P<0.007), based on the difference in G2 between constrained and unconstrained models. Due to the moderate sample size and low p-value for the final 4-class model, we chose the conservative approach of stratifying all subsequent analyses using non-Hispanic Black, non-Hispanic White, and Hispanic categories.
To finalize the number of classes, we conducted a bootstrapped likelihood ratio test, comparing the model fit of each model to the model with one less class. Based on this and the AIC, we found that 3 classes were supported for Black and Hispanic women, but 4 for White women. The adjusted-BIC also supported 3 classes for Black and Hispanic women, but supported 5 classes for White women. For consistency between racial/ethnic groups, and because the fourth class was meaningfully different, we used 4 classes for the remainder of our analyses. These 4 classes have slightly different meanings for the different racial/ethnic groups, as described below. We therefore used these race/ethnic group-specific classes for all subsequent analyses.
Figure 1 shows the violence exposure items that correspond to each class. [FIGURE 1] Class A is characterized by history of violence exposure and current partner arguments. Class AW White women were also likely to report living in unsafe neighborhoods, Class AB Black women were likely to report physical abuse during pregnancy, and Class AH Hispanic women were likely to report living in unsafe neighborhoods and the inner city. Class B women had elevated likelihood of having history of violence exposure, some likelihood of current partner arguments, and living in bad neighborhoods. Class C women had elevated levels on all measure of violence, including current violence exposure, history of exposure, and neighborhood exposure. Class D women overall had lower violence exposure, but Black Class DB and Hispanic Class DH women were likely to live in the inner city.
Figure 1.
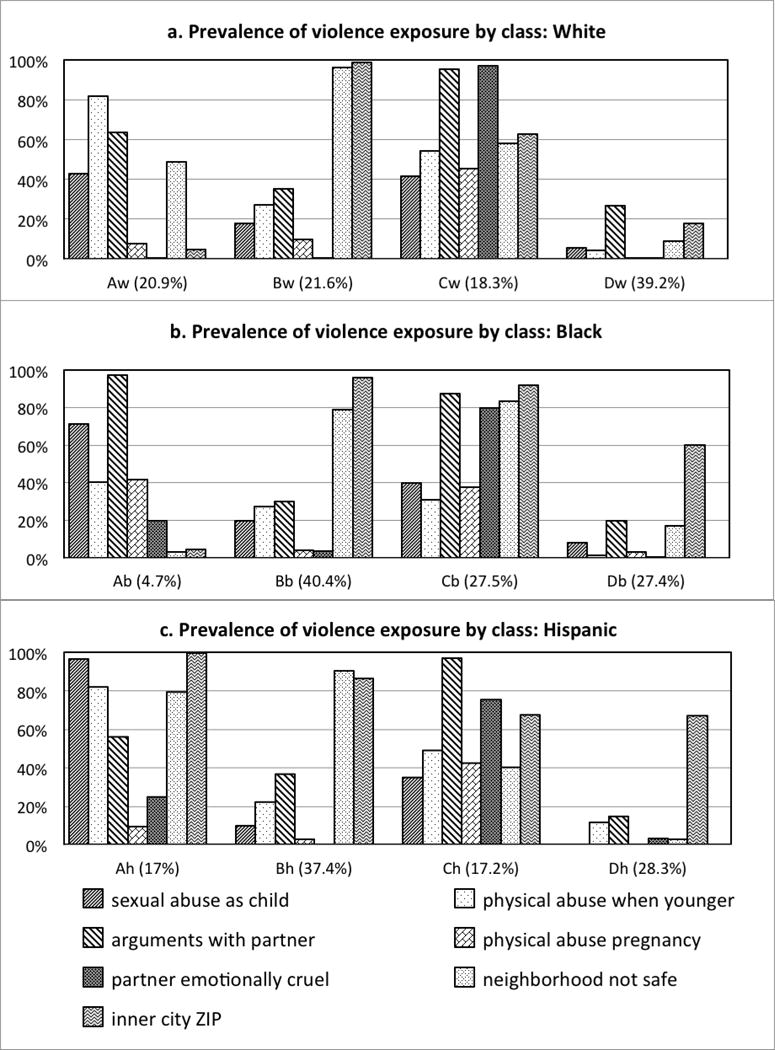
Violence history for each class by race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic). Within each race/ethnicity, four classes were identified (A, B, C, D), but these classes are not the same between race/ethnicity (White Class A [AW} is similar, but not identical, to Black Class A [AB]). For each class, the percentage of the racial/ethnic group in that class is indicated parenthetically (e.g., 20.9% of White women were in Class AW).
In bivariate models, White women in Class BW were more likely to initiate breastfeeding than White women in Class DW (P<0.045) and White women in Class AW were less likely to continue breastfeeding for 4 weeks (P<0.038) and 13 weeks (P<0.002), breastfeed exclusively for 4 weeks (P<0.031) and 13 weeks (P<0.019) than White women in Class DW. Hispanic women in Class BH were less likely to continue breastfeeding (P<0.03) or breastfeed exclusively (P<0.04) for 13 weeks than Hispanic women in Class DH. No other statistically significant bivariate associations were found.
In multivariable models including violence exposure classes, Hispanic women in Class BH were more likely to initiate breastfeeding when controlling for breastfeeding plan, but more likely to stop before 13 weeks when not controlling for breastfeeding plan, than Hispanic women in Class DH (Table 2). [TABLE 2] White women in Class AW were less likely to continue breastfeeding to 13 weeks than those in Class DW, controlling for breastfeeding plan. There were no other associations between violence exposure classes and breastfeeding behaviors.
Table 2.
Models predicting breastfeeding initiation and probability of stopping, including violence exposure classes as predictors.a Violence exposure classes are labeled A through D, with subscripts indicating the race/ethnicity because the class structures vary by race/ethnicity.b Model 1 includes classes, breastfeeding plan, and covariates, while Model 2 includes only classes and covariates
| Predictors | BF initiation
|
BF duration: 4 weeks
|
BF duration: 13 weeks
|
BF exclusivity: 4 weeks
|
BF exclusivity: 13 weeks
|
|---|---|---|---|---|---|
| Odds Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
|
| White | |||||
| Model 1 | |||||
| Class AW vs. DW | 2.37 (0.46, 12.1) | 2.57 (0.70, 10.70) | 2.86 (1.01, 8.53)* | 1.89 (0.90, 3.95) | 1.74 (0.87, 3.43) |
| Class BW vs. DW | 0.38 (0.08, 1.73) | 1.40 (0.26, 6.91) | 2.11 (0.54, 7.94) | 1.52 (0.64, 3.46) | 1.30 (0.59, 2.76) |
| Class CW vs. DW | 0.88 (0.18, 4.36) | 0.63 (0.07, 3.99) | 1.19 (0.29, 4.68) | 1.08 (0.38, 2.67) | 1.26 (0.53, 2.77) |
| Breastfeeding plan | -c | 0.45 (0.15, 1.30) | 0.23 (0.09, 0.53)** | 0.72 (0.39, 1.32) | 0.65 (0.38, 1.13) |
| Model 2: | |||||
| Class AW vs. DW | 3.39 (0.75, 15.29) | 1.97 (0.56, 7.30) | 2.21 (0.80, 6.35) | 1.79 (0.87, 3.68) | 1.61 (0.82, 3.13) |
| Class BW vs. DW | 0.44 (0.14, 1.41) | 1.06 (0.20, 4.76) | 1.18 (0.32, 4.14) | 1.40 (0.60, 3.09) | 1.18 (0.54, 2.43) |
| Class CW vs. DW | 0.74 (0.20, 2.74) | 0.49 (0.06, 2.68) | 1.19 (0.31, 4.35) | 1.10 (0.39, 2.65) | 1.21 (0.52, 2.65) |
| Black | |||||
| Model 1 | |||||
| Class AB vs. DB | 2.50 (0.24, 25.85) | 0.96 (0.05, 5.70) | 1.24 (0.35, 3.54) | 0.67 (0.16, 1.92) | 0.66 (0.22, 1.58) |
| Class BB vs. DB | 1.26 (0.57, 2.81) | 1.21 (0.46, 3.43) | 1.05 (0.57, 1.96) | 1.23 (0.75, 2.05) | 1.42 (0.91, 2.25) |
| Class CB vs. DB | 1.70 (0.66, 4.37) | 0.75 (0.23, 2.40) | 0.76 (0.38, 1.54) | 1.15 (0.67, 2.00) | 1.40 (0.85, 2.34) |
| Breastfeeding plan | 9.40 (3.51, 25.21)** | 0.37 (0.14, 0.89)* | 0.29 (0.16, 0.48)** | 0.56 (0.37, 0.85)** | -d |
| Model 2: | |||||
| Class AB vs. DB | 4.50 (0.52, 39.30) | 1.40 (0.21, 5.93) | 0.95 (0.31, 2.42) | 0.69 (0.20, 1.79) | 0.66 (0.25, 1.47) |
| Class BB vs. DB | 1.28 (0.61, 2.69) | 1.09 (0.41, 3.05) | 0.88 (0.48, 1.65) | 1.24 (0.76, 2.07) | 1.41 (0.90, 2.23) |
| Class CB vs. DB | 1.98 (0.82, 4.75) | 0.67 (0.21, 2.10) | 0.64 (0.32, 1.28) | 1.11 (0.64, 1.92) | 1.31 (0.79, 2.18) |
| Hispanic | |||||
| Model 1 | |||||
| Class AH vs. DH | 0.25 (0.025, 2.40) | 1.70 (0.45, 6.08) | 2.16 (0.80, 5.74) | 1.02 (0.45, 2.14) | 1.07 (0.51, 2.14) |
| Class BH vs. DH | 0.13 (0.02, 0.83)* | 1.26 (0.41, 3.88) | 2.06 (0.92, 4.76) | 1.61 (0.89, 2.95) | 1.68 (0.94, 3.06) |
| Class CH vs. DH | 0.17 (0.01, 2.00) | 1.37 (0.26, 6.15) | 2.42 (0.84, 7.10) | 0.57 (0.19, 1.44) | 1.12 (0.51, 2.31) |
| Breastfeeding plan | - c | 0.40 (0.16, 0.99)* | 0.40 (0.21, 0.74)** | 0.75 (0.45, 1.24) | - d |
| Model 2: | |||||
| Class AH vs. DH | 0.60 (0.12, 2.88) | 1.30 (0.35, 4.54) | 1.66 (0.63, 4.23) | 0.96 (0.43, 2.00) | 0.95 (0.45, 1.88) |
| Class BH vs. DH | 0.29 (0.07, 1.11) | 1.22 (0.39, 3.80) | 2.30 (1.06, 5.18)* | 1.65 (0.92, 3.00) | 1.72 (0.96, 3.11) |
| Class CH vs. DH | 0.33 (0.07, 1.67) | 1.00 (0.19, 4.30) | 2.22 (0.8, 6.08) | 0.55 (0.18, 1.38) | 1.05 (0.48, 2.15) |
P<0.05
P<0.001
The following variables were included as covariates if they were significantly associated with the given outcome in bivariate tests: language (English vs. other), age, smoking history, alcohol history, education, depression, reasons for stopping breastfeeding (went back to school, went back to work, went back to both school and work, or neither), BMI, parity (no prior births vs. prior births).
Joint tests of class contribution to each model were run; results are not presented because they were >0.05 in all cases.
Not reported, because fewer than 3 individuals who had a breastfeeding plan did not initiate breastfeeding, leading to unreasonable standard error estimates.
Not reported, because fewer than 3 individuals who had no breastfeeding plan continued exclusively breastfeeding through 13 weeks, leading to unreasonable standard error estimates.
Breastfeeding intention was the most consistent predictor of breastfeeding outcomes. Current smoking was associated with increased breastfeeding in some cases. Working and going to school had mixed impacts on breastfeeding outcomes, with White women generally breastfeeding more if they had less than a high school education and were in school, but others breastfeeding less if they were in school or worked. Age also had mixed results, with older Hispanic and younger White women breastfeeding more. Depression was associated with less breastfeeding in a few models, as was non-primarily English speaking for White women. Having a previous child increased breastfeeding for Black and Hispanic women in some models.
Because of the limited associations found between violence exposure classes and breastfeeding outcomes, we explored associations between specific aspects of violence exposure and breastfeeding. We focused on history of violence exposure because that appeared to be a defining characteristic of the classes that were associated with breastfeeding outcomes. We defined a new variable (history of violence exposure) as reporting sexual abuse as a child or physical abuse when younger. For White women, a history of violence exposure was associated with ending breastfeeding earlier at both 4 and 13 weeks postpartum (Table 3). [TABLE 3] The association for White women holds when breastfeeding intention is removed as a covariate (Supplemental Table S2). When breastfeeding intention was removed from the model, an association between history of violence exposure and breastfeeding initiation is apparent for Black women.
Table 3.
Models predicting breastfeeding initiation and probability of stopping, including history of violence exposure as a predictor. These models includes history of violence exposure, breastfeeding plan, and covariates.
| Predictors | BF initiation
|
BF duration: 4 weeks
|
BF duration: 13 weeks
|
BF exclusivity: 4 weeks
|
BF exclusivity: 13 weeks
|
|
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
Hazard Ratio (95% CI) |
||
| White | ||||||
| History of Violence Exposure | 2.30 (0.70, 7.20) | 5.92 (1.72, 27.98)* | 3.33 (1.46, 8.00)** | 1.73 (0.97, 3.11) | 1.65 (0.95, 2.86) | |
| Breastfeeding plan | b | 0.52 (0.17, 1.47) | 0.28 (0.13, 0.59)** | 0.76 (0.43, 1.39) | 0.66 (0.39, 1.13) | |
| Black | ||||||
| History of Violence Exposure | 1.80 (0.90, 3.90) | 0.66 (0.25, 1.59) | 0.93 (0.54, 1.58) | 0.95 (0.63, 1.43) | 0.97 (0.67, 1.39) | |
| Breastfeeding plan | 9.20 (3.40, 24.8) | 0.39 (0.15, 0.93)* | 0.29 (0.17, 0.50)** | 0.55 (0.36, 0.84)** | c | |
| Hispanic | ||||||
| History of Violence Exposure | 0.90 (0.20, 3.80) | 0.68 (0.25, 1.72) | 0.87 (0.44, 1.68) | 0.71 (0.41, 1.19) | 0.83 (0.50, 1.35) | |
| Breastfeeding plan | b | 0.46 (0.18, 1.11) | 0.42 (0.23, 0.78)** | 0.73 (0.44, 1.22) | c |
P<0.05
P<0.001
The following variables were included as covariates if they were significantly associated with the given outcome in bivariate tests: language (English vs. other), age, smoking history, alcohol history, education, depression, reasons for stopping breastfeeding (went back to school, went back to work, went back to both school and work, or neither), BMI, parity (no prior births vs. prior births).
Not reported, because fewer than 3 individuals who had a breastfeeding plan did not initiate breastfeeding, leading to unreasonable standard error estimates.
Not reported, because fewer than 3 individuals who had no breastfeeding plan continued exclusively breastfeeding through 13 weeks, leading to unreasonable standard error estimates.
Because breastfeeding plan was a consistent predictor of breastfeeding initiation and longer breastfeeding duration, we explored the associations between these factors. We found significant (P<.05) bivariate associations between breastfeeding plan and each breastfeeding outcome, except for duration at 4 weeks for White and Hispanic women (not shown in tables). In addition, we explored multivariable models using breastfeeding plan as an outcome, testing both the exposure of classes and history of violence as predictors, and including the same covariates as our other models. The only multivariable model that was significant was for Black women, with these women being more likely to have a breastfeeding plan if they had a history of violence (p=0.04) or prior pregnancies (p=0.04).
Conclusions for Practice
Our latent class analysis of surveillance data from a convenience sample of low-income women resulted in identification of meaningful classes defined by violence exposure, combining current and history of exposure. Results show that this group of women had very high levels of violence exposure with 87% of the sample reporting childhood, recent/current, and/or neighborhood exposure to violence. Further, we found that violence exposure patterns were different between racial and ethnic groups, but similar to other studies (Black et al., 2011; Kendall-Tackett, 2007) with Black and Hispanic women reporting higher levels of violence in their lives (92%) compared to White women (74%). These patterns of violence were inconsistently associated with breastfeeding plans or outcomes.
Based on our class analysis, we conducted additional analyses using only history of violence as the exposure. For White women, a history of violence exposure increased the likelihood of earlier breastfeeding cessation. This finding suggests that White women with a history of violence who begin breastfeeding may need additional support to continue breastfeeding. Because we do not know the reasons why they stopped breastfeeding, additional research is needed to determine the appropriate form of support. By contrast, for Black women, a history of violence exposure increased the likelihood that they would have a breastfeeding plan. This contrary finding may suggest an opportunity to support the intention to breastfeed.
The majority of our findings are consistent with the trend of violence exposure being associated with decreased breastfeeding behaviors. The one exception was Black women with a history of violence being more likely to have a plan to breastfeed. The literature also showed an exception with women who had a history of childhood sexual abuse, which is one of the two measures our history of violence exposures variable was based on. Therefore, it appears that there may be a difference in impact of recent vs. previous exposure.
The strong association between having a breastfeeding plan and other breastfeeding outcomes was not surprising, but the differences by race and ethnicity have not been previously reported, to our knowledge. Some differences between violence exposure classes are likely due to the correlation between race and socioeconomic status in the community studied. The majority of the Hispanic (80%) and Black women (81%) lived in the inner city, while a minority of the White women did (41%). This difference is reflected in the class characteristics. All of the Hispanic classes and all but one of the Black classes were characterized as having many inner city residents. The Black class with a low percentage of inner city residents accounted for only a small portion of the Black sample (4.7%). In contrast, only two of the White classes had a high percentage of inner city residents and these classes accounted for a minority of the White sample (39.9%). Because of these differences between inner city residence by race and the use of inner city residence to create the classes, it follows that White classes were characterized differently than Black or Hispanic classes. We note that living in the inner city was not correlated with perceived neighborhood safety by race. From these data, we do not know if the neighborhoods were substantially different, or if the perceptions were different.
These data are limited by being primarily self-report and collected postpartum, which may introduce recall bias and bias towards denying violence exposure. The data are also a convenience sample of moderate size, which may have reduced our ability to detect associations with small effect sizes. However, the availability of multiple types of violence exposure linked with collection of breastfeeding outcomes in the time period of breastfeeding provided a novel opportunity to explore these associations. Unlike other studies that have relied on breastfeeding recall after a longer time period, in this study breastfeeding was reported within 5–7 months postpartum. Another strength of this analysis was the use of LCA to distinguish violence exposure classes between race and ethnicity.
While our methodology demonstrated that violence exposure was associated with poorer breastfeeding outcomes, as noted by Cerruli et al. (2010), additional studies are warranted to improve our understanding of the relationship between violence exposure and breastfeeding outcomes among low- and non-low-income populations. Additional research is also needed on how to utilize information on exposure to violence to modify interventions that support prenatal decision making about breastfeeding intention, initiation of breastfeeding and sustaining breastfeeding, and how to take race into account when determining which women would benefit most from a targeted intervention.
Because of the life-long benefits of breastfeeding, identifying women who would benefit from interventions to improve breastfeeding outcomes should be a public health priority. Our findings add to the existing literature that violence exposure may reduce breastfeeding or limit breastfeeding duration, and present a new finding that there may be differences in patterns of violence exposure by race.
Supplementary Material
Significance.
What is known?
Some specific types of violence have been associated with breastfeeding patterns, but findings are inconsistent.
What this article adds?
We include a variety of violence measures, including childhood physical and/or sexual violence, experience of partner violence during or just after pregnancy, and neighborhood measures, combining them using latent class analysis, and allowed for differences by racial and ethnic backgrounds. Having a history of violence exposure impacted White and Black women differently, and was a stronger predictor of breastfeeding behaviors than exposure to violence during pregnancy.
Contributor Information
Margaret L. Holland, Yale University School of Nursing, 400 West Campus Drive, Orange, CT 06477, (203) 737-4929.
Kelly Thevenent-Morrison, University of Rochester, Department of Public Health Sciences, 265 Crittenden Blvd, Rochester, NY, 14642, (585) 275-1817.
Mona Mittal, University of Maryland, School of Public Health, Department of Family Science 255 Valley Drive College Park, MD 20742, (301) 405-7937.
Alice Nelson, 8348 SE Rhone St, Portland, OR 97266, (541) 600-0062.
Ann M. Dozier, University of Rochester, Department of Public Health Sciences, 265 Crittenden Blvd, Rochester, NY, 14642, (585) 276-3998.
References
- Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: A systematic review. Pediatrics. 2006;117(2):e278–e290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- Barnett BE, Hanna B, Parker G. Life event scales for obstetric groups. Journal of Psychosomatic Research. 1983;27(4):313–320. doi: 10.1016/0022-3999(83)90054-5. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens MR. The National Intimate Partner and Sexual Violence Survey: 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Bowman KG, Ryberg JW, Becker H. Examining the relationship between a childhood history of sexual abuse and later dissociation, breast-feeding practices, and parenting anxiety. Journal of Interpersonal Violence. 2009;24(8):1304–17. doi: 10.1177/0886260508322196. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse & Neglect. 2003;27(10):1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Bullock LF, Libbus MK, Sable MR. Battering and Breastfeeding in a WIC Population. Can J Nurs Res. 2001;32(4):43–56. [PubMed] [Google Scholar]
- Cavanaugh CE, Messing JT, Petras H, Fowler B, La Flair L, Kub J, Campbell JC. Patterns of violence against women: A latent class analysis. Psychological Trauma-Theory Research Practice and Policy. 2012;4(2):169–176. doi: 10.1037/a0023314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. CDC-Pregnancy Risk Assessment Monitoring System-Reproductive Health. 2016 Retrieved December 1, 2016, from www.cdc.gov/prams.
- Cerulli C, Chin N, Talbot N, Chaudron L. Exploring the Impact of Intimate Partner Violence on Breastfeeding Initiation: Does It Matter? Breastfeed Med. 2010;5(5):225–226. doi: 10.1089/bfm.2010.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles J, Anderson A, Loxton D. Breastfeeding duration after childhood sexual abuse: An Australian cohort study. Journal of Human Lactation. 2016;32(3):Np28–Np35. doi: 10.1177/0890334415590782. [DOI] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. New York: Wiley; 2010. [Google Scholar]
- Dozier AM, Nelson A, Brownell E. The relationship between life stress and breastfeeding outcomes among low-income mothers. Advances in Preventive Medicine. 2012;2012:902487. doi: 10.1155/2012/902487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eidelman AI, Schanler RJ, Johnston M, Landers S, Noble L, Szucs K, Breastfeeding S. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):E827–E841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Finnbogadóttir H, Thies-Lagergren L. Breastfeeding in the context of domestic violence-a cross-sectional study. Journal of Advanced Nursing. 2017 doi: 10.1111/jan.13339. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Hasselmann MH, Lindsay AC, Surkan PJ, Vianna GVdB, Werneck GL. Intimate partner violence and early interruption of exclusive breastfeeding in the first three months of life. Cadernos de Saúde Pública. 2016;32(10) doi: 10.1590/0102-311X00017816. [DOI] [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Lau J. evidence report/technology assessment No 153 (Prepared by Tufts-New England Medical Center Evidence-Based Practice Center, under Contract No 290-02-0022) Rockville, MD: Agency for Healthcare Research and Quality; 2007. Breastfeeding and maternal and infant health outcomes in developed countries. (Ahrq Publication No. 07-E007). [PMC free article] [PubMed] [Google Scholar]
- James J, Taft A, Amir L, Agius P. Does intimate partner violence impact on women’s initiation and duration of breastfeeding? Breastfeeding Review. 2014;22(2):11–19. [PubMed] [Google Scholar]
- Kendall-Tackett KA. Violence against women and the perinatal period - the impact of lifetime violence and abuse on pregnancy, postpartum, and Breastfeeding. Trauma, Violence, & Abuse. 2007;8(3):344–353. doi: 10.1177/1524838007304406. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K, Cong Z, Hale TW. Depression, sleep quality, and maternal well-being in postpartum women with a history of sexual assault: A comparison of breastfeeding, mixed-feeding, and formula-feeding mothers. Breastfeeding Medicine. 2013;8(1):16–22. doi: 10.1089/bfm.2012.0024. [DOI] [PubMed] [Google Scholar]
- Krause K, Lovelady C, Ostbye T. Predictors of breastfeeding in overweight and obese women: Data from Active Mothers Postpartum (AMP) Maternal and Child Health Journal. 2011;15:367–75. doi: 10.1007/s10995-010-0667-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Nylund-Gibson K, Copeland-Linder N, Ialongo NS. Patterns of community violence exposure during adolescence. American Journal of Community Psychology. 2010;46(3–4):289–302. doi: 10.1007/s10464-010-9344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misch ES, Yount KM. Intimate partner violence and breastfeeding in Africa. Maternal and Child Health Journal. 2014;18(3):688–697. doi: 10.1007/s10995-013-1294-x. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Bergman K, Sarkar P, Glover V. Prenatal cortisol exposure predicts infant cortisol response to acute stress. Developmental Psychobiology. 2013 Mar;55(2):145–55. doi: 10.1002/dev.21007. Epub 2012 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office on Women’s Health. Breastfeeding. 2016 Retrieved November 26, 2016, 2016, from https://www.womenshealth.gov/breastfeeding/breastfeeding-benefits.html.
- Ogbo FA, Eastwood J, Page A, Arora A, McKenzie A, Jalaludin B, The Early Years Research Group Prevalence and determinants of cessation of exclusive breastfeeding in the early postnatal period in Sydney, Australia. International Breastfeeding Journal. 2017;12(16):1–10. doi: 10.1186/s13006-017-0110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharps PW, Laughon K, Giangrande SK. Intimate partner violence and the childbearing year: Maternal and infant health consequences. Trauma, Violence, & Abuse. 2007;8(2):105–16. doi: 10.1177/1524838007302594. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence around the time of pregnancy: Association with breastfeeding behavior. Journal of Womens Health. 2006;15(8):934–940. doi: 10.1089/jwh.2006.15.934. [DOI] [PubMed] [Google Scholar]
- Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and Duration in the United States, 2003. Pediatrics. 2007;119:S38–S46. doi: 10.1542/peds.2006-0289G. [DOI] [PubMed] [Google Scholar]
- Sørbø MF, Lukasse M, Brantsæter AL, Grimstad H. Past and recent abuse is associated with early cessation of breast feeding: Results from a large prospective cohort in Norway. BMJ Open. 2015;5(12) doi: 10.1136/bmjopen-2015-009240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zureick-Brown S, Lavilla K, Yount KM. Intimate partner violence and infant feeding practices in India: A cross-sectional study. Maternal and Child Nutrition. 2015;11(4):792–802. doi: 10.1111/mcn.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


