Abstract
Objective
Depressive symptoms in middle and later life are associated with an increased risk of greater medical morbidity (i.e., number of chronic health conditions). Yet little is known about mutual influences that may occur within married couples. This study examined the effects of wives' and husbands' depressive symptoms on their own and their partner's number of chronic health conditions over an 8-year period. It was also determined whether these effects varied by gender.
Methods
The U.S. sample included 992 heterosexual couples (M = 63.58 years at baseline) drawn from five waves of the Health and Retirement Study (2006 – 2014). Dyadic growth curve models were estimated to evaluate the effects of own and partner baseline depressive symptoms on medical morbidity across time. Models controlled for baseline marital duration and negative marital quality along with age, education, minority status, health-related self-efficacy, body mass index, disability status, alcohol use, smoking, and moderate and vigorous physical activity.
Results
Husbands' higher baseline depressive symptoms were significantly linked to their own higher number of chronic conditions. When wives had higher depressive symptoms at baseline, husbands showed significantly greater increases in their number of chronic conditions over time. Own and partner depressive symptoms were not significantly associated with baseline levels or changes in wives' number of chronic conditions.
Conclusions
This study demonstrates that depressive symptoms within middle-aged and older couples may have long-term associations with medical morbidity. Findings underscore the value of considering the implications of depressive symptoms for chronic health conditions among individuals and couples.
Keywords: chronic illness, couples, depressive symptoms, marriage, multimorbidity
The prevention, treatment, and management of multimorbidity, or multiple chronic conditions, is the largest burden on our modern healthcare system (Fabbri et al., 2015; World Health Organization, 2013). Multimorbidity is particularly relevant for middle-aged and older adults because the prevalence and incidence of chronic health conditions increases with age (Violan et al. 2014). Indeed, multimorbidity impacts nearly one in five U.S. adults aged 45 to 64 and up to 80% of people aged 65 and older (DuGoff, Canudas-Romo, Buttorff, Leff, & Anderson, 2014; Freid, Bernstein, & Bush, 2012). A robust body of literature has positioned depression as a risk factor for incident chronic health conditions, such as type 2 diabetes mellitus (Rotella & Mannucci, 2013), acute cardiovascular disease (Nicholson, Kuper, & Hemingway, 2006), stroke (Dong, Zhang, Tong, & Qin, 2012), and overall multimorbidity (Barnett et al., 2012; Violan et al., 2014). Aging adults with elevated depressive symptoms and multimorbidity likely require more comprehensive and complex healthcare, and so a better understanding of the relationship between these conditions is necessary to align services with this growing public health concern.
The present study builds upon this literature by moving beyond the within-person links between depressive symptoms and medical morbidity to evaluate the reciprocal associations that may occur between spouses. Scholars have long recognized the marital relationship as a critical social context to study health in midlife and later life. Spouses commonly share environmental and behavioral risk factors for poor physical and psychological well-being (Hoppmann & Gerstorf, 2009). Moreover, spouses affect one another's thoughts, feelings, and behaviors in ways that mutually shape each partner's health trajectories (Hoppmann, Gerstorf, & Hibbert, 2011). Spousal associations have been observed across a host of indicators, such as sleep, alcohol use, and physical activity (e.g., Birditt, Cranford, Manalel, & Antonucci, 2016; Monin, Chen, & Stahl, 2016; Revenson, Marín-Chollom, Rundle, Wisnivesky, & Neugut, 2016). Prior work has considered how chronic health conditions are associated with depressive symptoms within couples both concurrently (Ayotte, Yang, & Jones, 2010) and over time (Thomeer, 2016; Valle, Weeks, Taylor, & Eberstein, 2013). Yet much less is known about the role of spouses' depressive symptoms in shaping levels and change in medical morbidity.
Depressive symptoms reported by partners may influence medical morbidity for at least four reasons. First, elevated depressive symptoms in one's partner may result in the couple's reduced social activity engagement, which may negatively impact the health and well-being of both spouses (Hoppmann, Gerstorf, & Luszcz, 2008). Second, partners' greater depressive symptoms may have adverse implications for engagement in health-maintenance behaviors including physical activity and sleep (Monin et al., 2016; Revenson et al., 2016). Third, spouses with higher depressive symptoms may lack the energy needed to provide adequate social support to their partners, thereby contributing to worsening health problems (Benazon & Coyne, 2000). Finally, greater depressive symptoms experienced by one or both spouses may generate stress within the marriage (Kouros & Cummings, 2011) that ultimately manifests as physical illness (Umberson, Williams, Powers, Liu, & Needham, 2006). Hence, elevated depressive symptoms reported by one's partner may be linked to greater medical morbidity, over and above the effects of one's own depressive symptoms.
Emotional and physical health problems, as well as marital dynamics, often vary by gender (e.g., Abad-Díez et al., 2014; Kiecolt-Glaser & Newton, 2001). As a consequence, within-couple effects of depressive symptoms on medical morbidity may differ between wives and husbands. With regard to the health effects of one's own depressive symptoms, wives may be more adversely impacted than husbands. Compared with their male counterparts, middle-aged and older women are less inclined to take care of themselves when ill (Thomeer et al., 2015) and receive less spousal and family support in managing their health problems (Rosland et al., 2010; Thomeer, Umberson, & Pudrovska, 2013; Thomeer et al., 2015). Furthermore, relative to men, women provide more caregiving in response to illness along with more frequent everyday support (e.g., emotional aid) to partners and other relatives (Antonucci, 2001; Monin & Clark, 2011; Thomeer, Reczek, & Umberson, 2015). Perhaps as a result, women perceive more family barriers to self-care and sustaining their own health than do men (Rosland, Heisler, Choi, Silveira, & Piette, 2010). Hence, wives may be more likely to experience increased medical morbidity as a consequence of their own depressive symptoms.
Regarding the effects of partners' depressive symptoms on medical morbidity, however, husbands may be more negatively affected than wives. The literature consistently shows that men derive more health benefits from marriage than women (Kiecolt-Glaser & Newton, 2001; Monin & Clark, 2011). This may be partly attributed to men's greater reliance on their partner as a source of social support (Antonucci, 2001). In addition, relative to women, men receive more social control from partners to encourage health-promoting behavior such as eating a healthy diet and taking prescription medication (August & Sorkin, 2010; Umberson, 1992). Wives with elevated depressive symptoms may be less able to meet their partner's emotional support needs or to effectively guide their partner's healthy behavior. Consequently, husbands may develop greater medical morbidity over time when wives have higher depressive symptoms.
Study Aims and Hypotheses
Utilizing a U.S. sample of middle-aged and older married couples, the effects of own and partner depressive symptoms on medical morbidity (i.e., self-reported number of major chronic health conditions including arthritis, diabetes, heart disease, hypertension, lung disease, and stroke) were evaluated across an 8-year period. Chronic conditions were selected based on their prevalence and strong associations with depression, disability, and mortality among aging adults (Hayward, 2002; Thomeer et al., 2016). The following hypotheses were examined:
Wives' and husbands' own higher baseline depressive symptoms are linked to their own higher levels and greater increases in medical morbidity over time.
For wives and husbands, their partner's higher baseline depressive symptoms are linked to their own higher levels and greater increases in medical morbidity over time.
Potential gender differences were considered with two additional hypotheses:
-
3
The associations between one's own depressive symptoms at baseline and one's own medical morbidity are stronger for wives than for husbands.
-
4
The associations between one's partner's depressive symptoms at baseline and one's own medical morbidity are stronger for husbands than for wives.
Methods
Participants and Sample
This study used a retrospective cohort design based on a U.S. sample of 992 heterosexual married couples drawn from five waves (2006 – 2014) of the Health and Retirement Study (HRS). The HRS has collected data biennially since 1992, with a response rate of over 80% at each wave. All participants are read a confidentiality statement when first contacted, and provide oral or implied consent by agreeing to be interviewed. Participants are also given a written informed consent document for each interview. In accord with the University of Michigan's policies, ethical approval for the current analysis was not required because publicly available secondary data with no individual identifiers were used.
In 2006, phone interviews were conducted with 18,469 participants, of whom 11,273 (61%) were married. Of the married participants, 11,027 (98%) had spouses who also completed an interview in 2006. Since 2006, an enhanced face-to-face interview has been conducted biennially from 50% of the panel participants followed by a self-administered psychosocial questionnaire (SAQ) with questions including the assessment of marital quality. Participants are asked to complete and mail the SAQ to the main field office at the University of Michigan. A total of 5,686 respondents (2,843 heterosexual couples) from unique households reported that they were married to the same spouse from 2006 to 2014 and participated in each wave.
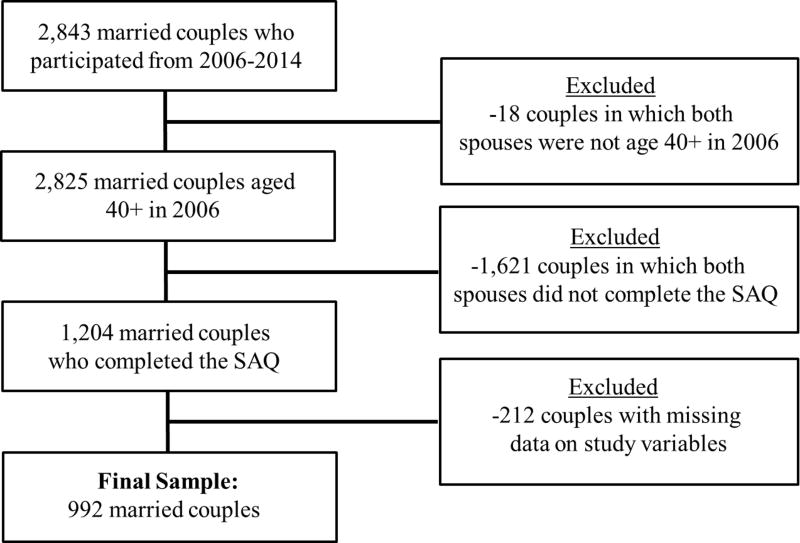
Sample selection for the current study is depicted in Figure 1. The present interest was in examining how own and partner depressive symptoms are associated with medical morbidity in midlife and later life, and so 2,825 couples were selected in which both spouses were aged 40 or older at baseline (2006). Marital quality and health-related self-efficacy were considered as key covariates on the basis of their associations with health outcomes (Marks, Allegrante, & Lorig, 2005; Robles, Slatcher, Trombello, & McGinn, 2014). As such, 1,621 couples in which one or both spouses did not complete the SAQ (which included marital quality and health-related self-efficacy measures) in 2006 were removed. Of the remaining 1,204 couples, 212 were removed due to missing data on study variables. Thus, the analysis focused on 992 consistently married wives (M = 61.93 years, SD = 8.46, range = 41 – 84) and husbands (65.23 years, SD = 8.11, range = 41 – 89). Compared with the total of 1,851 couples who were removed from the initial sample of 2,843 couples, the 992 couples in this study had more years of education (t(4,785.25) = 7.04, p < .001), reported fewer baseline depressive symptoms (t(4,676.88) = -4.61, p < .001), and were less likely to be racial or ethnic minorities (χ2 (1, N = 5,685) = 39.46, p < .001). There was no significant difference in their baseline number of chronic health conditions. On average, the 992 couples had been married for 34.85 years (SD = 13.97, range = 0.20 – 65.20) at baseline. Most wives (71.2%) and husbands (68.8%) were in their first marriage (see Table 1 for baseline characteristics and scores for key variables).
Figure 1.
Sample selection for the present study. SAQ refers to the self-administered psychosocial questionnaire conducted in 2006.
Table 1. Baseline Characteristics and Scores on Key Variables for Wives and Husbands.
| Wives | Husbands | |||
|---|---|---|---|---|
|
|
|
|||
| Characteristic | M | SD | M | SD |
| Age | 61.93 | 8.46 | 65.23 | 8.11 |
| Education in years | 13.37 | 2.47 | 13.55 | 2.84 |
| Depressive symptomsa | 1.01 | 1.59 | 0.80 | 1.36 |
| Medical morbidityb | 1.45 | 1.10 | 1.51 | 1.15 |
| Health-related self-efficacyc | 7.66 | 2.07 | 7.46 | 2.02 |
| Body mass index | 28.28 | 6.18 | 28.65 | 4.79 |
| Drinks per week | 1.77 | 3.82 | 3.75 | 7.01 |
| Moderate physical activityd | 3.37 | 1.22 | 3.57 | 1.06 |
| Vigorous physical activitye | 2.09 | 1.36 | 2.40 | 1.38 |
| Negative marital qualityf | 1.95 | 0.63 | 1.89 | 0.58 |
| Number of living children | 3.16 | 1.92 | 3.16 | 1.92 |
| Proportions | ||||
|
|
||||
| Minority statusg | .10 | .10 | ||
| Works for pay | .48 | .52 | ||
| Smoking statush | .09 | .09 | ||
| Disability statusi | .07 | .07 | ||
| Number of chronic conditions | ||||
| None | .21 | .21 | ||
| One | .34 | .32 | ||
| Two | .29 | .28 | ||
| Three | .12 | .14 | ||
| Four | .03 | .04 | ||
| Five | .004 | .01 | ||
| Six | .002 | .000 | ||
Note.
Sum of eight symptoms.
Self-reported number of six chronic health conditions.
One item assessing control over one's health from 0 (no control at all) to 10 (very much control).
Frequency of activities (e.g., brisk walking) from 0 (hardly ever or never) to 4 (more than once a week).
Frequency of activities (e.g., running) from 0 (hardly ever or never) to 4 (more than once a week).
Mean of four items (critical, demanding, lets you down, gets on your nerves).
1 = racial/ethnic minority, -1 = non-Hispanic White.
1 = currently smokes, -1 = does not currently smoke.
1 = has difficulty with one or more ADLs, -1 = does not have difficulty with ADLs.
N = 992 married couples.
Measures
Depressive symptoms
Depressive symptoms were assessed at each wave from 2006 to 2014 with the 8-item version of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), which has been found to show high reliability and validity in older adult populations (Karim, Weisz, Bibi, & Rehman, 2015). The present study focused on participants' reports at baseline (2006) for the main analysis but considered time-varying depressive symptoms in post hoc tests. Participants reported whether they experienced the following symptoms much of the time in the past week (1 = yes, 0 = no): felt everything was an effort, had restless sleep, could not get going, felt depressed, felt lonely, felt sad, was happy, enjoyed life. Ratings for the two positive items were reverse coded. Items were summed to create a total score, with higher scores indicating greater symptoms (α = .74).
Medical morbidity
Consistent with previous research (e.g., Fabbri et al., 2015; Thomeer, 2016), medical morbidity was assessed as the total number of six self-reported chronic health conditions. At each wave from 2006 to 2014, participants reported whether they had received a diagnosis of the following conditions: arthritis, diabetes, heart disease, hypertension, lung disease, and stroke (1 = has condition, 0 = does not have condition). Although the HRS includes cancer as a chronic health condition, it was not considered in the present analyses given the limited evidence for a causal connection between depressive symptoms and incident cancer (Gross, Gallo, & Eaton, 2010). Items were summed to determine a total score, with higher scores reflecting greater medical morbidity.
Covariates
Models controlled for baseline sociodemographic and health characteristics that are linked to medical morbidity in middle and later life (Autenrieth et al., 2013; Marengoni et al., 2011; Marks et al., 2005; Nagel et al., 2008): age, education in years, minority status (1 = racial/ethnic minority, -1 = non-Hispanic White), body mass index (BMI), health-related self-efficacy, smoking status (1 = currently smokes, -1 = does not currently smoke), frequency of alcoholic drinks per week, and frequency of vigorous and moderate physical activity. Health-related self-efficacy was measured with a single item assessing the degree of perceived control over one's own health from 0 (no control at all) to 10 (very much control). Drinks per week were calculated by multiplying participants' reports of their usual number of drinks on drinking days by their usual number of drinking days per week in the last three months. Participants separately reported how often they engaged in vigorous physical activities (e.g., running, cycling, aerobics) and moderate physical activities (e.g., gardening, stretching, brisk walking). Responses for both measures ranged from 0 (hardly ever or never) to 4 (more than once a week). Disability status was determined from self-reported difficulty with at least one activity of daily living (ADL): bathing, dressing, eating, toileting, getting in or out of bed, and walking (1 = has difficulty with one or more ADLs, -1 = does not have difficulty with ADLs).
Models also controlled for two marital characteristics related to health: marital duration in years and negative marital quality. Prospective studies show that longer marital duration is associated with a lower incidence of chronic health conditions and reduced risk of mortality (Dupre, Beck, & Meadows, 2009; Dupre & Meadows, 2007). Four brief but commonly used items assessed negative marital quality (Schuster, Kessler, & Aseltine, 1990; Walen & Lachman, 2000). Participants reported how often their spouse (a) makes too many demands on them; (b) criticizes them; (c) lets them down when counted upon; and (d) gets on their nerves from 1 (a lot) to 4 (not at all). Items were reverse coded and averaged so that higher scores represented more negative qualities (α = .76). These items have shown high reliability and construct validity (Bertera, 2005; Schuster et al., 1990; Walen & Lachman, 2000), along with links to objective health indicators (e.g., blood pressure, waist circumference) among aging couples over time (Birditt, Newton, Cranford, & Ryan, 2016; Birditt, Newton, Cranford, & Webster, 2016).
Statistical Analysis
Dyadic growth curve models were estimated using the MIXED procedure in SPSS Version 24. This multilevel approach is a version of the actor-partner interdependence model (APIM; Kenny, Kashy, & Cook, 2006) that facilitates the modeling of own and partner influence within couples over time. Models included the recommended two levels for longitudinal dyadic data, whereby the lower level represents variability due to within-person repeated measures for wives and husbands and the upper level represents between-couple variability across wives and husbands (Kenny et al., 2006). The intercept and slope of time were allowed to vary both between and within couples. Models also permitted correlated errors between wives and husbands in a given wave using a heterogeneous compound symmetry error structure (CSH). Thus, models accounted for nonindependence of observations within couples and over time.
In this study, actor effects represent the effects of wives' and husbands' depressive symptoms on their own medical morbidity (e.g., the link between wives' depressive symptoms and their own chronic health conditions). Partner effects represent the effects of one's partner's depressive symptoms on one's own medical morbidity (e.g., the link between wives' depressive symptoms and husbands' chronic health conditions). Associations between baseline depressive symptoms and reports of baseline levels and change in medical morbidity across waves were examined, controlling for baseline age, education, minority status, health-related self-efficacy, BMI, smoking, alcohol use, physical activity, marital duration, and negative marital quality. Waves represented time, which was centered at baseline. Predictors included own and partner depressive symptoms, time, and two interaction terms (Actor Depressive Symptoms X Time; Partner Depressive Symptoms X Time) to determine whether baseline depressive symptoms were linked to significantly greater increases in medical morbidity within couples.
Separate intercepts and slopes for wives and husbands were estimated using spouse gender (1 = wife, -1 = husband) as a distinguishing variable (Kenny et al., 2006). TEST statements in the SPSS syntax were used to evaluate whether there were significant gender differences between spouses for each tested association. Continuous predictors and covariates were grand mean centered (Kenny et al., 2006) and binary variables were effect coded (i.e., 1, -1) so that parameter estimates specify the deviation of each level of the variable from the grand mean of the outcome. We assessed whether there was a significant difference between the fit of the full model (with predictors and covariates) relative to a covariate-only model by subtracting their −2 log likelihood estimations and examining differences on a chi-square distribution with degrees of freedom equaling the change in number of parameters (Singer & Willett, 2003).
Results
Paired t tests were performed in preliminary analyses to examine differences between wives and husbands in major variables at baseline. Wives reported more depressive symptoms (t(991) = 3.38, p = .001) than husbands but there was no significant gender difference in number of chronic health conditions. Spouses' reports were positively correlated for depressive symptoms (r = .15, p < .001) and number of chronic health conditions (r = .21, p < .001).
Table 2 presents the prevalence of chronic health conditions for wives and husbands across waves. Significant gender differences in wives' and husbands' reports of each condition were examined using McNemar tests, which are appropriate for paired binary data (Kenny et al., 2006). Notably, although wives were more likely than husbands to develop arthritis by the final wave (2014), husbands were more likely than wives to develop diabetes, heart disease, hypertension, lung disease, and stroke over the duration of the study.
Table 2. Prevalence of Chronic Health Conditions for Wives and Husbands Across Study Waves (2006-2014).
| Wives | Husbands | |||
|---|---|---|---|---|
|
|
|
|||
| Baseline assessment (2006) | n | % | n | % |
| Arthritis | 571* | 57.6 | 486 | 49.0 |
| Diabetes | 140*** | 14.1 | 186 | 18.8 |
| Heart disease | 135*** | 13.6 | 226 | 22.8 |
| Hypertension | 499 | 50.3 | 504 | 50.8 |
| Lung disease | 67*** | 6.8 | 58 | 5.8 |
| Stroke | 23*** | 2.3 | 37 | 3.7 |
| Final wave assessment (2014) | ||||
|
| ||||
| Arthritis | 687*** | 69.3 | 608 | 61.3 |
| Diabetes | 202*** | 20.4 | 272 | 27.4 |
| Heart disease | 215*** | 21.7 | 356 | 35.9 |
| Hypertension | 606*** | 61.1 | 643 | 64.8 |
| Lung disease | 85*** | 8.6 | 89 | 9.0 |
| Stroke | 49*** | 4.9 | 80 | 8.1 |
Note. Significant differences between wives and husbands were examined using McNemar tests.
N = 992 married couples.
Indicates significant difference between wives and husbands at p ≤ .05.
Indicates significant difference between wives and husbands at p ≤ .001.
Dyadic growth curve model parameters are shown in Table 3. Medical morbidity showed a linear increase over time for wives (B = .05, p < .001, 95% CI [.05, .06]) and husbands (B = .07, p < .001, 95% CI [.06, .08]) on average. The rate of change, however, was steeper for husbands (B = -.02, p < .001, 95% CI [-.03, -.01]) (not shown in Table 3). The fit of the full model was significantly better than the covariate-only model (χ2 (4) = 30.63, p < .001), demonstrating that own and partner depressive symptoms accounted for a significantly greater amount of variance in medical morbidity over and above that explained by the covariates.
Table 3. Dyadic Growth Curve Model Examining the Effects of Own and Partner Depressive Symptoms on Medical Morbidity for Wives and Husbands.
| Wives' Medical Morbidity |
Husbands' Medical Morbidity |
|||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Parameter | B | SE | β | B | SE | β |
| Intercept | 1.78*** | .09 | 1.60*** | .09 | ||
| Time | .05*** | .003 | .13 | .07*** | .003 | .18 |
| Actor Depressive symptoms | .03 | .02 | .04 | .11*** | .03 | .14 |
| Partner Depressive symptoms | .01 | .02 | .01 | -.02 | .02 | -.03 |
| Actor Depressive symptoms X Time | .001 | .002 | .01 | -.0002 | .003 | -.001 |
| Partner Depressive symptoms X Time | .003 | .002 | .02 | .01** | .002 | .06 |
| Δ -2 Log Likelihood | 30.63*** | |||||
| Covariates | ||||||
| Age | .04*** | .01 | .30 | .05*** | .01 | .37 |
| Minority status | .07 | .05 | .04 | -.04 | .05 | -.02 |
| Education in years | -.03* | .01 | -.07 | -.02 | .01 | -.05 |
| Marital duration in years | -.001 | .003 | -.01 | -.002 | .003 | -.03 |
| Negative marital quality | .03 | .05 | .02 | .06 | .06 | .03 |
| Health-related self-efficacy | -.07*** | .02 | -.13 | -.04** | .02 | -.07 |
| Body mass index | .05*** | .01 | .25 | .07*** | .01 | .34 |
| Disability status | .20*** | .06 | .09 | .17** | .07 | .07 |
| Smoking status | -.01 | .05 | -.01 | .03 | .06 | .02 |
| Drinks per week | .01 | .01 | .05 | .001 | .01 | .01 |
| Moderate physical activity | -.06* | .03 | -.06 | -.07* | .03 | -.07 |
| Vigorous physical activity | -.01 | .02 | -.01 | .01 | .02 | .01 |
Note. Depressive symptoms and covariates were assessed at baseline, whereas medical morbidity was assessed biennially from 2006 to 2014. Change in -2 log likelihood for the full model (16,573.94) is based on comparison with a covariate-only model (16,604.57). Estimates are presented from the full model.
N = 992 married couples.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Dyadic Effects of Wives' and Husbands' Depressive Symptoms on Medical Morbidity
Wives' medical morbidity
As presented in Table 3 and counter to prediction, neither wives' nor husbands' higher baseline depressive symptoms were significantly linked to wives' higher baseline levels or greater increases in their number of chronic health conditions over time.
Husbands' medical morbidity
Husbands' greater baseline depressive symptoms were significantly associated with their own higher levels of medical morbidity at baseline (B = .11, p < .001, 95% CI [.06, .16]), showing that husbands with elevated depressive symptoms reported a higher number of chronic health conditions (Table 3). Contrary to prediction, the link between one's own greater baseline depressive symptoms and higher baseline levels of medical morbidity was significantly stronger for husbands than for wives (B = -.08, p = .02, 95% CI [-.15, -.02]) (not shown in Table 3). Husbands' baseline depressive symptoms were not significantly linked to the rate of change in their own medical morbidity over time.
In line with prediction, wives' higher baseline depressive symptoms were significantly linked to greater increases in husbands' medical morbidity over time (B = .01, p = .01, 95% CI [.001, .01]). Thus, when wives had higher depressive symptoms, husbands reported a steeper rate of change in their number of chronic health conditions across waves. Wives' higher depressive symptoms were not significantly associated with husbands' number of chronic conditions at baseline.
Post Hoc Tests
The stability of findings was considered in a series of post hoc tests. The potential moderating effects of baseline negative marital quality, health-related self-efficacy, and moderate and vigorous physical activity were evaluated in separate models. Interaction terms were used to examine these effects on baseline levels (e.g., Actor/Partner Depressive Symptoms X Negative Marital Quality) and change (e.g., Actor/Partner Depressive Symptoms X Negative Marital Quality X Time) in medical morbidity, including the effect of each potential moderator over time (e.g., Negative Marital Quality X Time). None of these variables significantly moderated the findings, confirming their stability.
Bidirectional associations were explored in a model examining how own and partner reports of baseline number of chronic health conditions are linked to changes in depressive symptoms. The model controlled for all covariates from the main analysis. For husbands, their own higher baseline number of chronic health conditions was associated with their own higher levels of depressive symptoms at baseline (B = .12, p < .001, 95% CI [.06, .19]); but this link was not found for wives. There were no significant partner effects and number of baseline chronic health conditions was not linked to changes in depressive symptoms across waves. Hence, depressive symptoms within couples may have greater long-term effects on medical morbidity for aging husbands than the reverse associations.
Discussion
This study expands prior research on depression, marriage, and health by identifying wives' depressive symptoms as a key factor that may contribute to the accelerated development of medical morbidity among aging husbands. Multimorbidity is associated with a range of detrimental outcomes for middle-aged and older adults including greater healthcare expenditures and higher rates of hospitalization, adverse drug events, disability, and mortality (Fabbri et al., 2015). The present findings therefore have public health significance and reveal depressive symptoms within couples to be one potentially modifiable factor that may magnify the risk of multimorbidity among men in middle and later life. Considering that most individuals are married by midlife (U.S. Census Bureau, 2013), this study has critical implications for policymakers and clinicians working with people who may be susceptible to negative health consequences related to their own or their partner's depressive symptoms.
Associations Between Own Depressive Symptoms and Own Medical Morbidity
For husbands, their own elevated depressive symptoms at baseline were associated with their own higher number of chronic health conditions at baseline; but this association was not present for wives. Thus, while it was hypothesized that the links between one's own depressive symptoms and medical morbidity would be stronger for wives than for husbands, the opposite pattern emerged. One plausible explanation is that men have less effective coping resources than women in managing their depressive symptoms and concomitant physical health conditions (Ito & Matsushima, 2016). This may be due in part to several factors. Whereas women generally have larger and more varied social networks, men often have weaker social ties and tend to exchange social support less frequently (Antonucci, 2001; Monin & Clark, 2011). Furthermore, relative to women, men with elevated depressive symptoms are less likely to seek social support from family and friends, and are less likely to be referred to or enter mental health treatment (Vogel, Wester, Hammer, & Downing-Matibag, 2014). As a consequence, men utilize fewer resources that may attenuate the impact of depressive symptoms on their physical well-being. Men also have a greater tendency than women to use maladaptive strategies to cope with depressive symptoms that could be hazardous to their health, such as binge drinking and risk-taking (Addis, 2008; Martin, Neighbors, & Griffith, 2013).
Associations Between Partner Depressive Symptoms and Own Medical Morbidity
In line with the hypothesis, wives' higher baseline depressive symptoms were associated with husbands' increased number of chronic health conditions over time; however, contrary to prediction, there were no partner effects for wives. Interestingly, wives' depressive symptoms were not associated with husbands' levels of medical morbidity at baseline, indicating that partner influence for husbands unfolds over time. The enduring adverse consequences of wives' elevated depressive symptoms could be especially detrimental to husbands' health because wives typically maintain the couple's social ties that benefit the well-being of both partners (Antonucci, 2001; Polenick, Fredman, Birditt, & Zarit, 2016). Wives' emotional challenges may also render them less able to meet their partner's support needs themselves, perhaps making husbands more vulnerable to physical illness as they age.
Furthermore, wives' elevated depressive symptoms may lead to or intensify problems within the marriage that reverberate negatively on husbands' physical health. Qualitative research has found that couples in which wives have higher levels of depressive symptoms report greater marital dysfunction, hostility, and perceived isolation (Thomeer et al., 2013). That is, conflict and negative emotions may arise partly as a result of divergent spousal expectations of wives' depressive symptoms (e.g., when a wife desires mental health treatment but her husband thinks she just needs to “snap out of it”) along with husbands' inability or unwillingness to provide emotional support to their partner. Given the links between marital strain and health (e.g., Kiecolt-Glaser & Newton, 2001; Robles et al., 2014; Umberson et al., 2006), such marital processes may eventually take a toll on husbands' mental and physical well-being.
Finally, husbands were more likely than wives to develop five of the six conditions assessed in this study and demonstrated steeper increases in their overall number of chronic conditions across waves. It is therefore plausible that husbands' partner effect over time was easier to detect. Future studies should consider how depressive symptoms within couples are associated with a broader array of chronic health conditions, including those that are more common among aging women such as osteoporosis (Cawthon, 2011).
Strengths, Limitations, and Future Directions
Strengths of this study include a bidirectional examination of the long-term associations between own and partner depressive symptoms and medical morbidity, data from both spouses, and the selection of couples from a large, nationally representative sample. Utilizing dyads as the unit of analysis permitted the simultaneous modeling of own and partner influences over time. Models controlled for marital duration and quality, along with known sociodemographic and behavioral correlates of health status. Moreover, the associations in this study did not vary by baseline marital quality, health-related self-efficacy, or physical activity. Also of note, each partner's number of chronic health conditions at baseline was not associated with changes in depressive symptoms over time. Although the relationship between depression and chronic disease is likely bidirectional in the shorter term (e.g., Renn, Feliciano, & Segal, 2011), this suggests that depressive symptoms may have greater long-term effects on medical morbidity for aging husbands than vice versa. Hence, the findings add to a burgeoning literature showing robust spousal associations in a variety of health indicators (e.g., Birditt, Cranford, et al., 2016; Hoppmann et al., 2011; Thomeer, 2016) by demonstrating that own and partner depressive symptoms are independently linked to medical morbidity among men in middle and later life.
The study has several limitations. First, although self-reports of chronic health conditions are commonly used in population-based research, this approach could be an underrepresentation of illness prevalence (Hayward, 2002). There was also a restricted range and somewhat low levels of medical morbidity in the present sample. Second, the assessment of medical morbidity as the total number of chronic conditions does not account for all aspects of disease burden such as illness severity and complexity of self-management. There is currently no consensus, however, on the optimal measurement of multimorbidity (Fabbri et al., 2015). Furthermore, models in this study controlled for functional disability, helping to alleviate concerns about the differential impact of various types and combinations of conditions. Third, the findings are specific to consistently married heterosexual couples and may not generalize to other types of couples, such as those who eventually divorce, cohabiting partners, or same-sex couples. Fourth, most couples were non-Hispanic White, limiting generalizability to more ethnically diverse couples. Nonetheless, the current findings provide valuable insights into the long-term health ramifications of depressive symptoms as couples move through middle and later life, a highly vulnerable time for developing serious and disabling chronic conditions (Barnett et al., 2012).
An important area for future research is to determine the more proximal (e.g., daily level) mechanisms through which depressive symptoms are linked to medical morbidity within aging couples. Spouses with higher depressive symptoms may, for instance, exert negative influences on their partner's health behaviors that accumulate to heighten the risk of chronic illness. There may be short-term bidirectional effects as well such that poor health increases or maintains high levels of depressive symptoms within the couple (e.g., Ayotte et al., 2010; Hoppmann et al., 2011; Thomeer, 2016; Valle et al., 2013). Additionally, levels of depressive symptoms and medical morbidity may show concurrent links within couples across different time frames. The determination of individual and couple factors that may buffer or exacerbate these processes would be informative. Research shows, for example, that positive dyadic coping in young married couples is associated with lower levels of systemic inflammation, a potential mechanism that may explain the link between depression and onset of chronic health conditions (Gouin, Scarcello, da Estrela, Paquin, & Barker, 2016). Pinpointing such dyadic characteristics and mechanistic pathways may help to identify men and women who are more or less susceptible to the detrimental health effects of depressive symptoms within their marriage.
Lastly, given the increased attention to screening for and treating depression in primary care and other medical settings, understanding the potential risk of depressive symptoms in incident medical morbidity is a key direction for subsequent research. The present findings lay groundwork for future studies to explore whether mental health treatment yields long-term benefits for couples' physical health. Prior work has shown, for example, that couple-based interventions tend to improve marital functioning (Baucom, Belus, Adelman, Fischer, & Paprocki, 2014), which could help to protect each partner's health (Robles et al., 2014).
In sum, this study demonstrates that elevated depressive symptoms within middle-aged and older married couples are associated with husbands' greater medical morbidity. Findings highlight the importance of considering the detrimental health consequences of depressive symptoms in later life from both individual and couple perspectives.
Acknowledgments
This work was supported by training grant T32 MH 073553-11 from the National Institute of Mental Health (Stephen J. Bartels, Principal Investigator). The Health and Retirement Study is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan.
Contributor Information
Courtney A. Polenick, Department of Psychiatry, University of Michigan
Brenna N. Renn, Department of Psychiatry and Behavioral Sciences, University of Washington
Kira S. Birditt, Institute for Social Research, University of Michigan
References
- Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, Poblador-Plou B, Calderón-Meza JM, Sicras-Mainar A, Prados-Torres A. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatrics. 2014;14:35. doi: 10.1186/1471-2318-14-75. http://dx.doi.org/10.1186/1471-2318-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addis ME. Gender and depression in men. Clinical Psychology: Science and Practice. 2008;15(3):153–168. http://dx.doi.org/10.1111/j.1468-2850.2008.00125.x. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, London: Sage Publications; 1991. [Google Scholar]
- Antonucci TC. Social relations: An examination of social networks, social support and sense of control. In: Birren JE, Schaie KW, Abeles RP, editors. Handbook of the psychology of aging. San Diego, CA: Academic Press; 2001. pp. 427–453. [Google Scholar]
- August KJ, Sorkin DH. Marital status and gender differences in managing a chronic illness: The function of health-related social control. Social Science and Medicine. 2010;71(10):1831–1838. doi: 10.1016/j.socscimed.2010.08.022. http://dx.doi.org/10.1016/j.socscimed.2010.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autenrieth CS, Kirchberger I, Heier M, Zimmermann AK, Peters A, Doring A, Thorand B. Physical activity is inversely associated with multimorbidity in elderly men: Results from the KORA-Age Augsburg Study. Preventive Medicine. 2013;57(1):17–19. doi: 10.1016/j.ypmed.2013.02.014. http://dx.doi.org/10.1016/j.ypmed.2013.02.014. [DOI] [PubMed] [Google Scholar]
- Ayotte BJ, Yang FM, Jones RN. Physical health and depression: A dyadic study of chronic health conditions and depressive symptomatology in older adult couples. The Journal of Gerontology, Series B: Psychological Sciences. 2010;65(4):438–448. doi: 10.1093/geronb/gbq033. http://doi.org/10.1093/geronb/gbq033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. The Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. http://dx.doi.org/10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- Baucom DH, Belus JM, Adelman CB, Fischer MS, Paprocki C. Couple-based interventions for psychopathology: A renewed direction for the field. Family Process. 2014;53:445–461. doi: 10.1111/famp.12075. http://dx.doi.org/10.1111/famp.12075. [DOI] [PubMed] [Google Scholar]
- Benazon NR, Coyne JC. Living with a depressed spouse. Journal of Family Psychology. 2000;14:71–79. http://doi.org/10.1037/0893-3200.14.1.71. [PubMed] [Google Scholar]
- Bertera EM. Mental health in U.S. adults: The role of positive social support and social negativity in personal relationships. Journal of Social and Personal Relationships. 2005;22(1):33–48. http://doi.org/10.1177/0265407505049320. [Google Scholar]
- Birditt KS, Cranford JA, Manalel JA, Antonucci TC. Drinking patterns among older couples: Longitudinal associations with negative marital quality. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2016 doi: 10.1093/geronb/gbw073. Advance online publication. https://doi.org/10.1093/geronb/gbw073. [DOI] [PMC free article] [PubMed]
- Birditt KS, Newton NJ, Cranford JA, Ryan LH. Stress and negative relationship quality among older couples: Implications for blood pressure. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2016;71(5):775–787. doi: 10.1093/geronb/gbv023. https://doi.org/10.1093/geronb/gbv023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Newton NJ, Cranford JA, Webster NJ. Chronic stress and negative marital quality among older couples: Associations with waist circumference. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2016 doi: 10.1093/geronb/gbw112. Advance online publication. https://doi.org/10.1093/geronb/gbw112. [DOI] [PMC free article] [PubMed]
- Cawthon PM. Gender differences in osteoporosis and fractures. Clinical Orthopaedics and Related Research. 2011;469(7):1900–1905. doi: 10.1007/s11999-011-1780-7. https://doi.org/10.1007/s11999-011-1780-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong JY, Zhang YH, Tong J, Qin LQ. Depression and risk of stroke: A meta analysis of prospective studies. Stroke. 2012;43(1):32–37. doi: 10.1161/STROKEAHA.111.630871. http://dx.doi.org/10.1161/Strokeaha.111.630871. [DOI] [PubMed] [Google Scholar]
- DuGoff EH, Canudas-Romo V, Buttorff C, Leff B, Anderson GF. Multiple chronic conditions and life expectancy: A life table analysis. Medical Care. 2014;52(8):688–694. doi: 10.1097/MLR.0000000000000166. http://dx.doi.org/10.1097/MLR.0000000000000166. [DOI] [PubMed] [Google Scholar]
- Dupre ME, Beck AN, Meadows SO. Marital trajectories and mortality among U.S. adults. American Journal of Epidemiology. 2009;170(5):546–555. doi: 10.1093/aje/kwp194. http://dx.doi.org/10.1093/aje/kwp194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre ME, Meadows SO. Disaggregating the effects of marital trajectories on health. Journal of Family Issues. 2007;28(5):623–652. http://dx.doi.org/10.1177/0192513X06296296. [Google Scholar]
- Fabbri E, Zoli M, Ginzalez-Freire M, Salive ME, Studenski SA, Ferrucci L. Aging and multimorbidity: New tasks, priorities, and frontiers for integrated gerontological and clinical research. Journal of the American Medical Directors Association. 2015;16(8):640–647. doi: 10.1016/j.jamda.2015.03.013. http://dx.doi.org/10.1016/j.jamda.2015.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. Hyattsville, MD: National Center for Health Statistics; 2012. NCHS data brief, no 100. [PubMed] [Google Scholar]
- Gouin JP, Scarcello S, da Estrela C, Paquin C, Barker ET. Dyadic coping and inflammation in the context of chronic stress. Health Psychology. 2016;35(10):1081–1084. doi: 10.1037/hea0000395. http://dx.doi.org/10.1037/hea0000395. [DOI] [PubMed] [Google Scholar]
- Gross AL, Gallo JJ, Eaton WW. Depression and cancer risk: 24 years of follow-up of the Baltimore Epidemiologic Catchment Area sample. Cancer Causes Control. 2010;21(2):191–199. doi: 10.1007/s10552-009-9449-1. http://dx.doi.org/10.1007/s10552-009-9449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M. Using the Health and Retirement Survey to investigate health disparities. 2002 Retrieved from http://hrsonline.isr.umich.edu/sitedocs/dmc/hrs_healthdisparities_hayward.pdf.
- Hoppmann C, Gerstorf D. Spousal interrelations in old age—A mini-review. Gerontology. 2009;55:449–459. doi: 10.1159/000211948. http://doi.org/10.1159/000211948. [DOI] [PubMed] [Google Scholar]
- Hoppmann C, Gerstorf D, Hibbert A. Spousal associations between functional limitations and depressive symptom trajectories: Longitudinal findings from the Study of Asset and Health Dynamics among the Oldest Old (AHEAD) Health Psychology. 2011;30:153–162. doi: 10.1037/a0022094. http://doi.org/10.1037/a0022094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D, Luszcz M. Spousal social activity trajectories in the Australian Longitudinal Study of Ageing in the context of cognitive, physical, and affective resources. The Journal of Gerontology, Series B: Psychological Sciences. 2008;63:41–50. doi: 10.1093/geronb/63.1.p41. http://dx.doi.org/10.1093/geronb/63.1.P41. [DOI] [PubMed] [Google Scholar]
- Ito M, Matsushima E. Presentation of coping strategies associated with physical and mental health during health check-ups. Community Mental Health Journal. 2016 doi: 10.1007/s10597-016-0048-9. Advance online publication. http://dx.doi.org/10.1007/s10597-016-0048-9. [DOI] [PMC free article] [PubMed]
- Karim J, Weisz R, Bibi Z, Rehman S. Validation of the eight-item Center for Epidemiologic Studies Depression Scale (CES-D) among older adults. Current Psychology. 2015;34(4):681–692. http://dx.doi.org/10.1007/s12144-014-9281-y. [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: The Guilford Press; 2006. [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. http://dx.doi.org/10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kouros CD, Cummings EM. Transactional relations between marital functioning and depressive symptoms. American Journal of Orthopsychiatry. 2011;81(1):128–138. doi: 10.1111/j.1939-0025.2010.01080.x. http://dx.doi.org/10.1111/j.1939-0025.2010.01080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Fratiglioni L. Aging with multimorbidity: A systematic review of the literature. Ageing Research Reviews. 2011;10(4):430–439. doi: 10.1016/j.arr.2011.03.003. http://dx.doi.org/10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part I) Health Promotion Practice. 2005;6(1):37–43. doi: 10.1177/1524839904266790. https://doi.org/10.1177/1524839904266790. [DOI] [PubMed] [Google Scholar]
- Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry. 2013;70(10):1100–1106. doi: 10.1001/jamapsychiatry.2013.1985. http://dx.doi.org/10.1001/jamapsychiatry.2013.1985. [DOI] [PubMed] [Google Scholar]
- Monin JK, Chen B, Stahl ST. Dyadic associations between physical activity and depressive symptoms in older adults with musculoskeletal conditions and their spouses. Stress and Health. 2016;32:244–252. doi: 10.1002/smi.2603. http://dx.doi.org/10.1002/smi.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Clark MS. Why do men benefit more from marriage than do women? Thinking more broadly about interpersonal processes that occur within and outside of marriage. Sex Roles. 2011;65:320–326. http://doi.org/10.1007/s11199-011-0008-3. [Google Scholar]
- Nagel G, Peter R, Braig S, Hermann S, Rohrmann S, Linseisen J. The impact of education on risk factors and the occurrence of multimorbidity in the EPIC-Heidelberg cohort. BMC Public Health. 2008;8:384. doi: 10.1186/1471-2458-8-384. http://dx.doi.org/10.1186/1471-2458-8-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146 538 participants in 54 observational studies. European Heart Journal. 2006;27(23):2763–2774. doi: 10.1093/eurheartj/ehl338. http://dx.doi.org/10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- Polenick CA, Fredman SJ, Birditt KS, Zarit SH. Relationship quality with parents: Implications for own and partner well-being in middle-aged couples. Family Process. 2016 doi: 10.1111/famp.12275. Advance online publication. http://doi.org/10.1111/famp.12275. [DOI] [PMC free article] [PubMed]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurements. 1977;3:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Renn BN, Feliciano L, Segal DL. The bidirectional relationship of depression and diabetes: A systematic review. Clinical Psychology Review. 2011;31(8):1239–1246. doi: 10.1016/j.cpr.2011.08.001. http://dx.doi.org/10.1016/j.cpr.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Revenson TA, Marín-Chollom AM, Rundle AG, Wisnivesky J, Neugut AI. Hey Mr. Sandman: Dyadic effects of anxiety, depressive symptoms and sleep among married couples. Journal of Behavioral Medicine. 2016;39:225–232. doi: 10.1007/s10865-015-9693-7. http://doi.org/10.1007/s10865-015-9693-7. [DOI] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. Psychological Bulletin. 2014;140:140–187. doi: 10.1037/a0031859. http://dx.doi.org/10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosland A, Heisler M, Choi H, Silveira MJ, Piette JD. Family influences on self-management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help? Chronic Illness. 2010;6(1):22–33. doi: 10.1177/1742395309354608. http://dx.doi.org/10.1177/1742395309354608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotella F, Mannucci E. Depression as a risk factor for diabetes: A meta-analysis of longitudinal studies. The Journal of Clinical Psychiatry. 2013;74(1):31–37. doi: 10.4088/JCP.12r07922. http://dx.doi.org/10.4088/JCP.12r07922. [DOI] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology. 1990;18(3):423–438. doi: 10.1007/BF00938116. http://dx.doi.org/10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford, UK: Oxford University Press; 2003. [Google Scholar]
- Thomeer MB. Multiple chronic conditions, spouse's depressive symptoms, and gender within marriage. Journal of Health and Social Behavior. 2016;57(1):59–76. doi: 10.1177/0022146516628179. http://doi.org/10.1177/0022146516628179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer MB, Reczek C, Umberson D. Gendered emotion work around physical health problems in mid- and later-life marriages. Journal of Aging Studies. 2015;32:12–22. doi: 10.1016/j.jaging.2014.12.001. http://dx.doi.org/10.1016/j.jaging.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer MB, Umberson D, Pudrovska T. Marital processes around depression: A gendered and relational perspective. Society and Mental Health. 2013;3(3):151–169. doi: 10.1177/2156869313487224. http://dx.doi.org/10.1177/2156869313487224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D. Gender, marital status and the social control of health behavior. Social Science and Medicine. 1992;34(8):907–917. doi: 10.1016/0277-9536(92)90259-s. http://dx.doi.org/10.1016/0277-9536(92)90259-S. [DOI] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. http://doi.org/10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. America's families and living arrangements. 2013 Retrieved from http://www.census.gov/hhes/families/data/cps2013A.html.
- Valle G, Weeks JA, Taylor MG, Eberstein IW. Mental and physical health consequences of spousal health shocks among older adults. Journal of Aging and Health. 2013;25(7):1121–1142. doi: 10.1177/0898264313494800. http://doi.org/10.1177/0898264313494800. [DOI] [PubMed] [Google Scholar]
- Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, Valderas JM. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS One. 2014;9(7):e102149. doi: 10.1371/journal.pone.0102149. http://dx.doi.org/10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel DL, Wester SR, Hammer JH, Downing-Matibag TM. Referring men to seek help: The influence of gender role conflict and stigma. Psychology of Men and Masculinity. 2014;15(1):60–67. http://dx.doi.org/10.1037/a0031761. [Google Scholar]
- Walen HR, Lachman ME. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships. 2000;17:5–30. http://doi.org/10.1177/0265407500171001. [Google Scholar]
- World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013 Retrieved from http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf.