Abstract
Background
Emergency department (ED) acuity is the general level of patient illness, urgency for clinical intervention, and intensity of resource use in an ED environment. The relative strength of commonly used measures of ED acuity is not well understood.
Methods
We performed a retrospective cross-sectional analysis of ED-level data to evaluate the relative strength of association between commonly used proxy measures with a full spectrum measure of ED acuity. Common measures included the percentage of patients with Emergency Severity Index (ESI) scores of 1 or 2, case mix index (CMI), academic status, annual ED volume, inpatient admission rate, percentage of Medicare patients, and patients-seen-per-attending-hour. Our reference standard for acuity is the percentage of high acuity charts (PHAC) coded and billed according to the Centers for Medicare and Medicaid Service’s Ambulatory Payment Classification (APC) system. High acuity charts included those APC 4, 5 or critical care. PHAC was represented as a fractional response variable. We examined the strength of associations between common acuity measures and PHAC using Spearman’s rank correlation coefficients (rs) and regression models including a quasi-binomial generalized linear model and linear regression.
Results
In our univariate analysis, the percentage of patients ESI 1 or 2, CMI, academic status and annual ED volume had statistically significant associations with PHAC. None explained more than 16% of PHAC variation. For regression models including all common acuity measures, academic status was the only variable significantly associated with PHAC.
Conclusion
ESI had the strongest association with PHAC followed by CMI and annual ED volume. Academic status captures variability outside of that explained by ESI, CMI, annual ED volume, percentage Medicare patients, or patients-per-attending-per-hour. All measures combined only explained only 42.6% of PHAC variation.
INTRODUCTION
Emergency department (ED) acuity may be defined as the general level of patient illness, urgency for clinical intervention, and the intensity of resource use within an ED’s clinical care environment. In this context it is a characteristic encompassing the intensity of medical need and services delivered. Validated measures to compare ED acuity, as a cross-institutional measure, are limited despite it being an important metric to guide clinical resource allocation.
Here we explore acuity as a quality of the ED care environment for which comparisons can be made across facilities with 2 specific phenomena in mind. First, is the growing number of metrics making performance comparisons across a diversity of facilities all described as EDs. The function and performance of an ED may be different based on whether it is a relatively lower or higher acuity facility. Being able to identify these differences relies on comprehensively assessing acuity. EDs also range from 5,000 visit per year critical access centers to 250,000 visits per year facilities with care sub-units. Measures need to go beyond size and volume differences to include the diversity of patient care needs, resources available and applied to provide care, and the urgency with which ED care is needed or delivered (i.e. – the balance of primary/urgent care to emergency acute care requiring early involvement of specialist services such as stroke, emergency abdominal surgery, ST-segment elevation myocardial infarction, and impending labor). Second, is the drive to adopt practice innovations (e.g. - split flow, team triage, physician-in-triage, ED physician cath lab activation, chest pain protocols) from one ED to another. Doing so relies on being able to assess the transferability of a practice or policy between EDs. One important consideration is whether the intervention’s performance was tested in an ED of similar overall patient illness, urgent need for clinical intervention, and intensity of resources used for acute care. As a result, it is critical to understand the reliability of measures used to differentiate EDs by their acuity.
Common proxies for ED acuity include: the aggregated Emergency Severity Index (ESI) score, case mix index (CMI),1,2 annual ED volume,3,4,5 academic status,6 and inpatient admission rate (the percentage of ED patients admitted to the hospital with the intensity of care meeting “inpatient” as opposed to intense “observation” level admissions).6,7 In addition, many national benchmarking organizations within emergency medicine use percentage of higher risk ED populations and resource-to-patient ratios. Examples include the percentage of Medicare patients and patients-per-attending-hour.8,9,10
Despite the frequent use of these metrics, each has significant limitations in capturing the level of acuity for the full spectrum of an ED’s clinical environment. In this study we assess how commonly used proxies are related to the full spectrum of ED acuity as measured by the percentage of high acuity charts (PHAC). To our knowledge, a study of this kind has not been done in emergency medicine, because obtaining these measures for cross-institutional comparison is challenging. The ED Operations Study Group (EDOSG) is a non-profit research consortium dedicated to advancing research informing evidence-based clinical operations. The organization’s research network has the ability to obtain these measures for a sample of EDs, while representing the diversity of clinical practice in the United States (US). Despite this innovation and opportunity to explore ED acuity, we acknowledge there is no true reference standard. As a result, our analyses should be considered more suggestive than conclusive.
METHODS
Study Design
This was a retrospective cross-sectional study using ED-level EDOSG data collected via survey as reported by each member ED. The objective was to determine the strength of association between common proxies for ED acuity with a rationalized reference standard, PHAC. Independent variables included seven established proxies for ED acuity including the percentage of patients with an Emergency Severity Index (ESI) score of 1 or 2, CMI,1,2 annual ED volume,3,4,5 academic status,6 inpatient admission rate (the percentage of ED patients admitted to the hospital with the intensity of anticipated care designated as “inpatient” as opposed to “observation”), the percentage of Medicare patients, and patients-seen-per-attending-hour per day.
Study Population
With the ED as the unit of analysis, our study population included 62 facility members of the EDOSG summarizing the care delivered during 3,323,071 ED visits in 2014. The group represents the diversity of US EDs in terms of US geographic regions, infrastructure, patient acuity, patient volume, academic intensity, and clinical staffing differences. (Table 1)
Table 1.
Characteristics of Emergency Departments with and without Complete Data1
| N | Complete Data N=27 |
Incomplete Data N=27 |
Full Study Sample N=54 |
P-value | |
|---|---|---|---|---|---|
| Percentage high acuity charts | 54 | 0.54 0.66 0.73 (0.65±0.15) | 0.46 0.64 0.71 (0.58±0.21) | 0.52 0.64 0.72 (0.61±0.19) | 0.363 |
| Percentage of ESI2 1 or 2 | 41 | 0.08 0.18 0.25 (0.17±0.11) | 0.05 0.10 0.15 (0.12±0.089) | 0.07 0.13 0.25 (0.16±0.11) | 0.153 |
| Case Mix Index | 40 | 1.40 1.68 1.80 (1.63±0.28) | 1.45 1.56 1.80 (1.71±0.49) | 1.40 1.64 1.80 (1.65±0.35) | 0.993 |
| Annual ED Volume (per 10,000) | 54 | 3.7 5.3 6.6 (5.6±2.6) | 2.1 5.2 7.0 (5.6±4.6) | 3.5 5.3 6.8 (5.6±3.7) | 0.583 |
| Academic Status | 54 | 0.204 | |||
| Non-academic | 19% 5/27 | 41% 11/27 | 30% 16/54 | ||
| AMC affiliated5 | 44% 12/27 | 33% 9/27 | 39% 21/54 | ||
| Primary AMC ED | 37% 10/27 | 26% 7/27 | 31% 17/54 | ||
| Percentage Medicare Patients | 45 | 20.4 23.7 28.0 (23.1±7.9) | 22.8 28.0 30.0 (27.2±7.7) | 20.9 26.1 29.0 (25.1±8.0) | 0.093 |
| Inpatient Admission Rate | 53 | 15 18 24 (23±17) | 13 19 23 (19±10) | 14 18 24 (22±15) | 0.893 |
| Patients Per Attending hr/day | 54 | 2.15 2.40 2.90 (2.62±0.78) | 1.92 2.50 3.18 (2.45±0.83) | 2.10 2.50 3.0 (2.54±0.8) | 0.713 |
| Region | 0.144 | ||||
| Midwest | 7% 2/27 | 26% 7/27 | 17% 9/54 | ||
| Northeast | 56% 15/27 | 41% 11/27 | 48% 24/54 | ||
| South | 30% 8/27 | 33% 9/27 | 31% 17/54 | ||
| West | 7% 2/27 | 0% 0/27 | 4% 2/54 |
a b c represent the lower quartile a, the median b, and the upper quartile c for continuous variables x ± s represents X ± 1 SD.
Complete Cases were those EDs without missing data. Yes: indicates no missing data. No: indicated any missing data.
ESI is the emergency severity index. Tests used:
Wilcoxon Rank Sum test;
Pearson Chi Square test.
AMC is an academic medical center.
Data Collection
We asked each site to provide demographic information for their facility, percentage of patients with ESI 1 or 2, CMI1,2 annual ED volume,3,4,5 academic status,6 inpatient admission rate,6,7 percent of patient admitted under observation status, percentage of Medicare patients, patients-seen-per-attending-hour per day, and the aggregated percentage of billed charts falling into each ambulatory payment classification (APC) coding level category.8,9,10 Each site PI agreed to accurate data collection and reporting to the EDOSG. Most frequently site-PIs are medical or clinical operations directors. The group, however, includes directors of research, nurse administrators, and research faculty with clinical operations interests. All were individuals with roles permitting data access. The data for this study were collected simultaneously with the EDOSG’s 2015 ED metric collection reflecting 2014 clinical care.
Primary Outcome
Our primary outcome was the PHAC coded and billed within each ED according to the Center for Medicare and Medicaid Service’s APC system as our measure of the acuity within each EDs care environment. Most ED visits are captured in a chart documenting patient symptoms, clinician observations, and medical care provided. The majority are then coded using the APC system. APC coding is a federal scaling system developed to guide Medicare and Medicaid reimbursements according to a hierarchy of patient illness and resources applied for ambulatory care.9 It consists of a scale of 1–5 where 5 represents a high level of care intensity and patient acuity.11 Two levels of critical care can replace a level 5 chart if intensive-care unit level services are provided. Higher coding levels result in higher reimbursements for physician evaluation and management professional fees. Charts scored as levels 4, 5, or with associated critical care represent the highest acuity patients. Other payers have since adopted this system for reimbursement.
The US Office of the Inspector General (OIG) monitors fraud and abuse of this classification system, and is empowered to conduct audits when inappropriate billing is suspected. Periodic analyses of national trends are performed to monitor coding shift. Penalties can be applied to the institution for verified misconduct.11 The APC system was not designed to measure ED acuity. However, the ability of the percentage of high acuity charts to retrospectively account for resource intensity and patient level of illness, and the wide spread use of the standardized and federally monitored APC system, makes it our rationalized reference standard.
We asked each ED to report the percent distribution of their coded and billed charts for 6 ranked categories: levels 1 through 5, and critical care. We then calculated the percentage of high patient acuity charts – levels 4, 5 and critical care – to obtain the PHAC for each ED. EDs with missing PHAC were excluded from the analysis. All unbilled patient charts were excluded, yet represented less than 5% of all ED visits.
Statistical Analysis
We reported data as aggregated counts, means, and percentages for measures of resource utilization, process, and performance. We used descriptive statistics to report summaries as percentages and medians with interquartile ranges (IQR). This is the standard for measuring clinical performance within emergency medicine.14 However, we simultaneously calculated means with one standard deviation (SD) to identify skewness that would otherwise be masked.
We evaluated associations between common proxies of acuity and PHAC in three ways: rank-based analyses, graphical assessment and regression analyses. First, we examined the strength of association between PHAC and common acuity measures using Spearman’s rho rank correlation coefficients for continuous acuity measures and the Kruskal-Wallis rank sum test for categorical acuity measures. Those rank-based methods avoid distributional assumptions and thus are less influenced by outliers. Second, we used scatterplots with loess smoothed lines or box plots to visualize the relationship of each common acuity measure with PHAC. Lastly, we conducted regression analysis to relate traditional acuity measures separately and combined with PHAC. PHAC ranges between 0 and 1 and represents a proportional quantity represented as a fractional response varable. In addition, we were concerned relationships with PHAC may not be linear. As a result we used a quasi-binomial generalized linear regression models (GLM) with logit link as our primary regression approach. We then repeated the univariate and multivariate analyses using a linear model to compare and assess whether assuming linearity in the measures relationship with PHAC was reasonable. Within both models, the univariate analyses quantified the relationship between each individual common acuity measure and PHAC and the multivariate analyses tested the degree to which the common measures could jointly predict PHAC.
Multiple imputation was used to handle missing common acuity measures to prevent a statistical power reduction and avoid potentially biased results from only including EDs with complete cases.12 Specifically, missing data for independent variables were imputed 10 times using additive imputation models allowing for nonlinear transformations on the data to make optimal use of partial information recorded for each ED. We then summarize the regression results from all 10 multiple imputations.
Traditional likelihood based goodness of fit statistics such as the Akaike information criterion (AIC) do not apply to quasi-likelihood based GLM. Therefore, R-squared (R2) was used as a goodness-of-fit statistic for model comparisons. For models assessing combined effects of all seven acuity measures (full model), we tested a series of nested models and compared each with the full model using R2 to avoid over-fit. The nested models excluded 1 or 2 variables explaining the least variance of PHAC. We observed minimal differences in R2, the strength of associations or significance of remaining variables, so the full model is reported. We evaluated linearity in the GLM using residual plots based on standardized deviance residuals plotted against PHAC on the logit scale. We calculated variance inflation factors for each independent variable to ensure there is no collinearity problem among the common acuity measures.
We set significance a-priori at p<0.05, and present results as odds ratios (OR) with 95% confidence intervals (CI). Statistical analyses were performed by biostatisticians in R, version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria, 2015, https://www.R-project.org).
RESULTS
From the rank-based analyses, we found notable associations with PHAC for the following 5 common measures: percentage of patients with ESI 1 or 2, CMI, academic status, annual ED volume, and inpatient admission rate. We did not find statistically significant associations with the percentage of Medicare patients or patients-seen-per-attending-per-hour (Table 2).
Table 2.
Rank-Based Analyses: Strength of Association with the Proportion of High Acuity Charts in an Emergency Department1, 2
| (Spearman Correlation) | |||
|---|---|---|---|
|
| |||
| Correlation with PHAC3 | CI | P-value | |
| Percentage of ESI 1 or 24 | 0.466 | (0.187, 0.676) | 0.000 |
| Case Mix Index | 0.383 | (0.101, 0.607) | 0.006 |
| Academic Status – Non-Academic5 | - | - | |
| Academic Status – Primary AMC6 | - | - | 0.0297 |
| Academic Status – AMC Affiliated | - | - | |
| Annual ED Volume | 0.378 | (0.123, 0.586) | 0.005 |
| Inpatient Admission Rate | 0.360 | (−0.113, 0.420) | 0.015 |
| Percentage of Medicare Patients | 0.171 | (−0.031, 0.560) | 0.226 |
| Patient per Attending hr/day | 0.127 | (−0.142, 0.387) | 0.366 |
Imputed complete outcome cohort (N= 54).
High acuity chart as determined by Center for Medicare and Medicaid Services’ (CMS) Ambulatory Payment Classification (APC) System.
Spearman correlation coefficient.
ESI is the emergency severity index
Reference for comparison
AMC is an academic medical center.
Kruskal-Wallis rank sum test was used for this categorical variable.
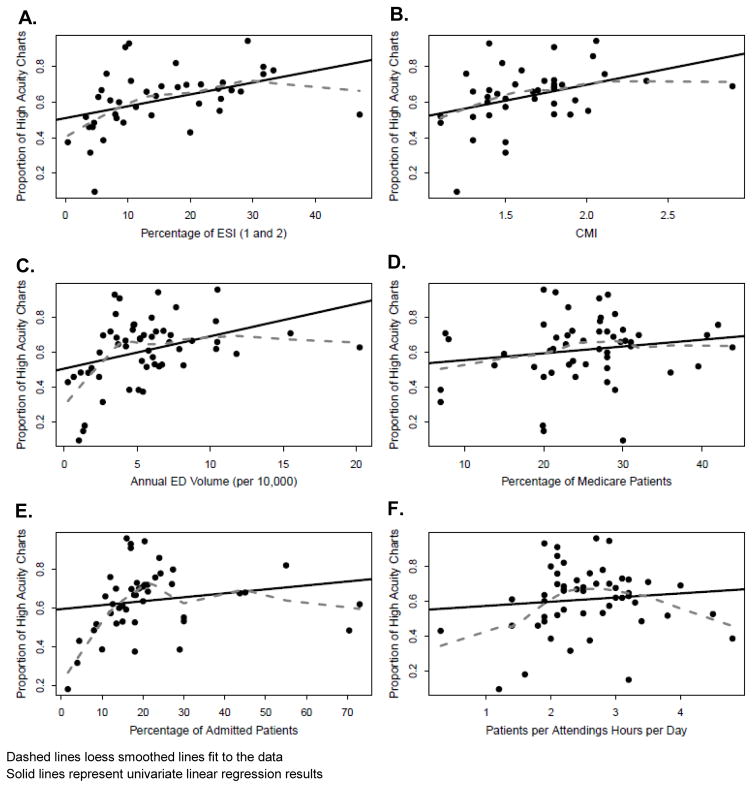
Scatterplots suggest the percentage of patients with ESI 1 or 2, CMI and the percentage of Medicare patients are linearly related with PHAC. Bell-shaped loess smooth curves from the scatterplots for annual ED volume, inpatient admission rates and patients-per-attending-hour suggest potential non-linear relationships with PHAC (Figure 2a–f).
Figure 2.
Scatterplots for the Associations between Common Acuity Measures (Continuous Variables) with the Proportion of High Acuity Charts
Results from univariate analyses using quasi-binomial GLM are consistent with findings from rank-based analyses. We found similar notable associations between the following 5 acuity measures and PHAC: percentage of patients with ESI 1 or 2, CMI, academic status, annual ED volume and inpatient admission rate (Table 3). When all acuity measures are included in one model, only academic status demonstrated a statistically significant association with PHAC, and annual ED volume is borderline (p=0.052). The R2 from this full model accounts for less than half of the PHAC variability. No systematic patterns against randomness around 0 were observed from residual plots of each acuity measure from the full model. Results using linear regression are similar to quasi-binomial GLM, but with lower R2 for both univariate analyses and multiple linear regression, which indicates quasi-binomial GLM is a more appropriate modeling approach.
Table 3.
Regression Analyses: Relationship between Common Measures of ED1 Patient Population Acuity and the Proportion of High Acuity Charts (PHAC)2
| 3a – Generalized Linear Model3 | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Univariate Analysis4 (N=54) | Multiple Regression (N=54) | |||||||
|
|
|
|||||||
| OR | CI | P-value | R2 | OR | CI | P-value | R2 | |
| Percent ESI 1 or 26 | 1.03 | (1.01, 1.05) | 0.015 | 0.16 | 1.01 | (0.99, 1.04) | 0.263 | |
| Case Mix Index | 2.21 | (1.15, 4.25) | 0.020 | 0.14 | 1.58 | (0.79, 3.16) | 0.204 | |
| Academic Status – Non-Academic | 1.00 | - | - | - | - | - | 0.426 | |
| Academic Status – Primary AMC7 | 1.09 | (1.03, 1.16) | 0.007 | 0.15 | 1.07 | (1.00, 1.14) | 0.052 | |
| Academic Status – AMC Affiliated | 1.73 | (1.08, 2.79) | 0.027 | 1.84 | (1.15, 2.93) | 0.014 | ||
| Annual ED Volume | 2.04 | (1.23, 3.38) | 0.008 | 0.16 | 1.49 | (0.79, 2.81) | 0.228 | |
| %Medicare Patients | 1.02 | (0.99, 1.04) | 0.242 | 0.03 | 1.02 | (0.99, 1.05) | 0.193 | |
| Inpatient Admission Rate | 1.01 | (1.00, 1.02) | 0.170 | 0.04 | 1.00 | (0.99, 1.02) | 0.615 | |
| Patient per Attending hr/day | 1.11 | (0.58, 1.45) | 0.435 | 0.01 | 0.96 | (0.73, 1.27) | 0.777 | |
| 3b – Linear Regression Results3 | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Univariate Analysis4 (N=54) | Multiple Regression5 (N=54) | |||||||
|
|
|
|||||||
| Beta | CI | P-value | R2 | Beta | CI | P-value | R2 | |
| Percent ESI 1 or 26 | 0.006 | (0.001, 0.011) | 0.013 | 0.13 | 0.003 | (−0.003, 0.009) | 0.27 | |
| Case Mix Index | 0.178 | (0.019, 0.336) | 0.021 | 0.11 | 0.101 | (−0.090, 0.929) | 0.21 | |
| Academic Status – Non-Academic | - | - | - | - | - | - | - | |
| Academic Status – Primary AMC7 | 0.019 | (0.005, 0.032) | 0.007 | 0.13 | 0.016 | (0.001, 0.031) | 0.04 | |
| Academic Status – AMC Affiliated | 0.134 | (0.02, 0.25) | 0.025 | 0.15 | 0.142 | (0.029, 0.256) | 0.01 | 0.385 |
| Annual ED Volume | 0.170 | (0.05, 0.292) | 0.008 | 0.15 | 0.098 | (−0.067, 0.264) | 0.19 | |
| %Medicare Patients | 0.004 | (−0.003, 0.01) | 0.242 | 0.03 | 0.004 | (−0.002, 0.011) | 0.20 | |
| Inpatient Admission Rate | 0.002 | (−0.002, 0.006) | 0.174 | 0.03 | 0.001 | (−0.003, 0.005) | 0.62 | |
| Patient per Attending hr/day | 0.025 | (−0.038, 0.089) | 0.435 | 0.01 | −0.001 | (−0.079, 0.058) | 0.75 | |
Emergency department (ED).
High acuity chart as determined by Center for Medicare and Medicaid Services’ (CMS) Ambulatory Payment Classification (APC) System.
Imputed complete outcome cohort (N= 54).
The univariate analysis test each common measure for its individual association with PHAC.
The multivariate analysis combines all measures to test their collective ability to explain variation in PHAC.
ESI is the emergency severity index
AMC is an academic medical center.
Through univariate quasi-binomial GLM, we quantified the change in PHAC associated with a unit of change in each measure. Specifically, PHAC increases by 3% with a 1% increase of patients categorized as ESI 1 or 2, increases by 8% for each 0.1 unit increase in CMI, and increases by 9% for each 10,000 patient increase in annual ED volume. The ratio of AMC affiliated ED and primary AMC ED PHAC to non-academic EDs was 1.73 and 2.04 respectively.
DISCUSSION
We found the percentage of patients with ESI 1 or 2 had the strongest association with PHAC followed by CMI and annual ED volume. Academic status captures variability outside of that explained by ESI, CMI, annual ED volume, percentage Medicare patients, or patients-seen-per-attending-per-hour as evidenced by retaining its significant association in the multiple regression analysis. We found no significant relationships between PHAC and the percentage of Medicare patients, inpatient admission rate, or patients-seen-per-attending-per-hour.
Emergency Severity Index (ESI) Scoring
The percentage of patients with an ESI score of 1 or 2 had the strongest, albeit moderate, correlation with PHAC. These are patients anticipated to need immediate attention for a potentially life or limb threatening condition. ESI is a prospectively applied score that considers illness urgency and intensity of anticipated services. It is calculated for the majority of individual ED patients shortly after arrival and prospectively estimates acuity using vital sign instability, signs of distress, symptoms associated with urgent medical needs, and the clinical judgement of emergency medical service personnel and triage providers. The ESI’s inclusion of objective findings, clinical judgement, predetermined symptoms of concern, and the majority of ED patients likely impart a significant advantage over the other measures which primarily rely on retrospectively assessed administrative data. Given these characteristics, we anticipated a stronger association in our regression analysis, and a more positive slope in Figure 2f. We found a more moderate correlation than we anticipated. This may be due to limitations of the measure as it scores anticipated needs and does not account for the actual illness level determined or resources used during the ED visit.
Case Mix Index (CMI)
CMI also had a moderate correlation coefficient. It is a complex measure designed to capture the intensity of in-hospital care provided to admitted Medicare or Medicaid patients. The adjusted association, however, was not statistically significant. Our loess curves of the relationship with PHAC (Figure 2a) showed a slope of nearly 1, but it appears to be significantly influenced by two outliers. The linear model demonstrates a more positive slope that may plateau in higher CMI facilities, thus reducing the strength of the association overall. However, this is unclear given there are few EDs with CMI >2.3. CMI’s major limitation is it excludes the majority of patients, those who are discharged from the ED or admitted to observation. The ability of CMI to stratify acuity within the admitted patient subgroup likely accounts for its discrimination of PHAC across EDs.
Annual Emergency Department (ED) Patient Volume
Annual ED volume had a moderate correlation with PHAC. This may be because, although it accounts for the full ED patient spectrum, it provides no information on services or illness level for individual patients. Nonetheless, prior work has demonstrated an ED will function differently and require an increase in the intensity of resources to meet care demand with every 20,000 patient increase in annual ED volume,2–4 This increase in acuity with rising volume is seen in our data (Figure 2b). The relationship demonstrates a sharp rise until EDs reach 60,000 patients per year, then the trend levels off. A more linear trend in the higher volume EDs may be difficult to detect in this study due to there being only 7 EDs with annual volume >100,000 visits. Greater representation of larger volume EDs may demonstrate a stronger association.
Academic Status
There was a clear distinction in acuity between the academically-connected EDs and non-academic community practice sites illustrated by the medians of the academic groups being not only higher than non-academic EDs, but also falling outside of the non-academic ED interquartile range. In Figure 3, however, we did not observe a significant distinction in the distribution of acuity between primary academic medical center (AMC) EDs and academically-affiliated EDs. AMCs serve as teaching centers partly because they provide a mix of patient acuity adequate for trainee education. As a result, they tend to be urban, tertiary care referral centers, with high acuity patient populations. It is, however, possible that resident and attending physician documentation may comparatively increase the care captured in patient charts and augment the resultant APC coding. Academic-affiliated sites are typically the community practice experience locations for trainees, thus a step away from the tertiary care hub function of many primary academic centers. As a result, we anticipated a significant difference from primary AMC sites. It may be that academic-affiliated sites benefit from added resident staffing in a practice environment were attending physicians document for the majority of patients. This increased documentation may augment coding. This is in contrast to primary AMC EDs where attendings more typically review resident documentation for most patients and may be more engaged in bedside teaching for a larger proportion of trainees than charting.
Figure 3.
Histogram for the Association of Academic Status with the Proportion of High Acuity Charts
Inpatient Admission Rate
We found a moderate correlation coefficient and a no significant regression associations between inpatient admission rate and PHAC. It seems intuitive that a higher percentage of patients admitted under inpatient status would indicate a sicker patient population. Hospitals, however, have varied thresholds for admission and varied ED resources. In some cases, more intense ED care may obviate inpatient admission. This makes it difficult to compare one ED’s admission rate to another. In addition, this measure reveals little about the care provided during the ED stay, and does not represent the majority: those discharged or admitted to observation. The mean inpatient admission rate have been previously reported as 17.5%.16 This is similar to the 18% observed in our study. The scatterplot demonstrates a sharp rise until inpatient admissions reach approximately 18–20% with an IQR of 14–24% (Figure 2d). We anticipated this variability, within the interval with the steepest slope, would reliably discriminate acuity across EDs, as is often assumed in practice. However, the moderate correlation observed suggests other factors may contribute to the admission decision. Some EDs may provide more extensive diagnostic testing or treatment permitting discharge that, if deferred, could qualify a patient for inpatient admission. (i.g., cardioversion for atrial fibrillation with a rapid ventricular response;17,18 or young patients with suspected infection who present with hemodynamically unstable vital signs, improve with resuscitation, and are discharged with home care). This may be due to most EDs lying within the plateau area of the loess curve in the scatter plot (Figure 2e). Additionally, this metric is vulnerable to variable leveling as inpatient versus observation status across institutions. This may create artificial differences between similar patient populations. For example, a 2013 OIG report found significant variation across hospitals in the relative mix of long outpatient stays and short inpatient stays.17 This may explain why the OR for inpatient admission rate were 1.0 in both our univariate and multivariate regression analyses.
Percentage of Medicare Patients
We found a weak association with PHAC and the percentage of Medicare patients. A larger percentage of ED Medicare beneficiaries would seem to introduce a larger patient cohort with higher risk for severe illness due to increased age, number of comorbidities, and frequency of healthcare utilization. This group, however, is generally a minority subset of the larger ED population and thus this measure does not account for the service or illness for the majority of patients. We observed a slight, but non-statistically significant, trend towards an increasing percentage of high acuity charts with an increasing Medicare population (Figure 2c). The lack of association in our correlation or regression analyses suggests any association with acuity is indirect.
Patients Seen Per Attending Hours Per Day
A high patient to attending physician ratio, measured as patients-per-attending-hour, is assumed to correlate with a lower acuity ED. The rationale is if one physician can see many patients, the intensity of care and level of illness of the broader patient population is likely low. We observed an initial rise in the association of patients-per-attending-hour, an inflection around 3 patients per hour, then a downturn (Figure 2e). The progression from 1–3 patients per hour may be reflective of higher acuity with ≥3 patients per hour is consistent with a low acuity environment. Nursing, resident, and physician extender staffing levels, in addition to facility design and other variables such as the use of scribes may impact the productivity of an attending physician. This efficiency effect is a difficult confounder to quantify.20 Alternatively, physicians seeing ≥3 patients per hour may not have the time to provide the same attention to documentation details thus resulting in a lower billing acuity. This parabolic association, however, did not demonstrate significant influence in our study. Further investigation into the dynamics responsible for inflection at ~3 patients per hour warrants further investigation.
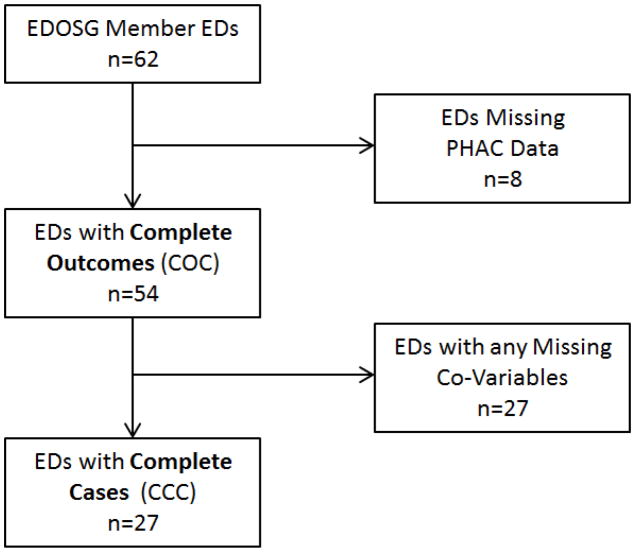
LIMITATIONS
There is no established reference standard for retrospectively measuring ED patient population acuity. As a result, we present our study as a thought provoking analysis exploring the validity of several traditional acuity measures for cross-facility comparisons. Participating EDs are members of a voluntary reporting organization motivated to share these metrics for the purpose of research. This likely introduces selection bias into the sample. To reduce this bias, the EDOSG strategically recruits EDs from all regions of the US with attention to the diversity of ED types (size, population served, urbanicity, and academic status) as is reflected in Table 1. The study uses an administrative data set, however, the data were collected with the intent of informing this specific study. The sample size is small with 27 of the 54 EDs sending complete data. However, 88% of the data requested was received, and we applied multiple imputations to our Complete Outcome Cohort (54) to reduce the bias introduced by a small data set (Figure 1).
Figure 1.
ED Inclusion/Exclusion Diagram
The objective of our modeling was to quantify each common acuity measure’s association with PHAC using this sample, rather than generating probabilities for unobserved EDs. As a result these findings should be considered suggestive given the limitations described above. Many multi-center studies of this type are limited to focal regions of the US or a particular type of ED. In addition, they often include academic centers with an interest and an incentive to perform research. This data set includes representation of the geographic and demographic diversity of EDs in the US including sites not typically involved in clinical research. There is less representation of the West and Midwest; however the proportional regional representation mirrors the population distribution of the US.
Our outcome variable is a percentage (or fraction) rather than a continuous variable, which involves loss of information on the acuity of individual patients within each ED. However, our primary objective was to capture the presence of a subset of truly acute patients within each ED. In addition, a fractional response outcome permits the use of a quasi-binomial linear model with a logit link allowing us to include variables into the analysis without major transformations that risk over-fitting the model to the idiosyncrasies of our sample. Despite our concerns over assuming linearity, our linear regression results mirrored that of the GLM. PHAC’s dependent on the translation of medical record data to acuity scoring for billing reimbursement may introduce information bias and selection bias. In a study examining the accuracy of coding-based billing compared to coding from direct observation, they found agreement amongst different coders in only 55% of patient visits.21 Other studies have documented similar agreement level with the use of similar methods.22,23 However, under and over estimating the intensity of services provided was equivalent suggesting that aggregate summary measures of patient visits over time may be valid. In addition, much of this prior research was done at a time when our current coding and reimbursement system was being introduced to medicine. Contemporary provider practices have likely adjusted. However, longitudinal research using billing data should account for this confounder. Transitioning electronic medical record systems has been known to impact the quality of documentation and the accuracy of billing. However, none of the EDs in this sample were involved in an EMR system change during the study period.
Our unit of analysis is the ED, and PHAC is an aggregated measure for individual EDs. As a result we have not weighted the PHAC for number of patients included at each hospital. This was handled in our analysis with the use of the logit link. The use of a fractional response outcome prevents one from using our model to estimate the acuity for an ED that was not included in our sample. Even if we had weighted our outcome variable, the low odds ratios obtained would not yield reliable estimates of PHAC.20 This was a study performed on an available dataset, and the sample size did not permit traditional internal validation procedures. However, we boot strapped our confidence intervals to validate the associations of acuity. As a result of this discrepancy, our analysis should be repeated in a larger sample to assure external validity before widespread adoption of our results.
CONCLUSION
The percentage of ESI 1 or 2 patients had the strongest association with PHAC followed by CMI and annual ED volume. Academic status captures variability outside of that explained by ESI, CMI, annual ED volume, percentage Medicare patients or patients-seen-per-attending-per-hour. The relative strengths of association observed in our study suggest a hierarchy of quality as measure for ED acuity, but should be examined in a larger data sample. All measures combined only explained 42.6% of PHAC variation so the validity of their common use as proxies for ED acuity should be further investigated.
Acknowledgments
GRANTS: Dr. Yiadom is supported by the National Heart Lung and Blood Institute (NHLBI) award numbers 5K12HL109019 and 1K23HL133477, and the National Center for Advancing Translational Sciences/NIH UL1 TR000445. Funding from this grant supported her effort on this project, data collection, biostatistical analysis, and manuscript development. Dr. Storrow is supported by NHLBI 5K12HL109019, NHLBI RO1HL111033, National Center for Advancing Translational Sciences/NIH UL1 TR000445, and PCORI FC14-1409-21656. He has received grant support from Abbott Diagnostics and Roche Diagnostics. He is a consultant for Roche Diagnostics, Novartis Pharmaceuticals Corp, Alere Diagnostics, Trevena, Beckman Coulter, and Siemens. Dr. Barrett has received research support as site principal investigator from Janssen Pharmaceuticals, Raritan, NJ and Alere, San Diego, CA. He is a consultant for Red Bull GmbH, Fuschl am See, Salzburg and Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield, Connecticut. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CONFLICTS OF INTEREST Dr. Yiadom is the founding director of the ED Operations Study Group
AUTHOR CONTRIBUTIONS:
MYY contributed to the study and served as project lead. MYY and the ED Operations Study Group 2015 site-primary investigators collected the study data. XL and VT contributed to the analysis plan. DL, CMS, CB, TB, TV and SR contributed to results interpretation and the discussion. AS provided scientific content guidance. DL served as the lead biostatistician for data analysis and refined the final study analysis.
References
- 1.Harris T, McDonald K. Is the case-mix of patients who self-present to EDs similar to general practice and other acute-care facilities? Emerg Med J. 2014;31(12):970–974. doi: 10.1136/emermed-2013-202845. [DOI] [PubMed] [Google Scholar]
- 2.Weissman J, Epstein AM. Case mix and resource utilization by uninsured hospital patients in the Boston metropolitan area. JAMA. 1989 Jun 23;261(24):3572–6. [PubMed] [Google Scholar]
- 3.Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone-Griffith S. Emergency department performance measures updates: proceedings of the 2014 Emergency Department Benchmarking Alliance Consensus Summit. Academic Emergency Medicine. 2015 May 1;22(5):542–53. doi: 10.1111/acem.12654. [DOI] [PubMed] [Google Scholar]
- 4.Emergency Department Size Determines the Demographics of Emergency Department Patients. Michalke JA, Patel SG, Siler Fisher A, Hoxhaj S, Augustine J, Davidson SJ, O’Connor RE, Reese CL., IV Annals of Emergency Medicine. 2005 Sep;46(3 Supplement):39. [Google Scholar]
- 5.Patients Per Day and Admission Rate Predict Average Length of Stay in the Emergency Department. Moseley MG, Patel SG, Coletti CM, Augustine J, Davidson SJ, Fisher AS, Hoxhaj S, O’Connor RE, Reese CL., IV EDBA Acad Emerg Med. 2005 [Google Scholar]
- 6.Vieth TL, Rhodes KV. The effect of crowding on access and quality in an academic ED. The American journal of emergency medicine. 2006 Nov 30;24(7):787–94. doi: 10.1016/j.ajem.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 7.Pitts SR, Pines JM, Handrigan MT, Kellermann AL. National trends in emergency department occupancy, 2001 to 2008: effect of inpatient admissions versus emergency department practice intensity. Annals of emergency medicine. 2012 Dec 31;60(6):679–86. doi: 10.1016/j.annemergmed.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Yiadom MY, Schuelen J, McWade C, Augustine JJ. Implementing Data Definition Consistency for ED Operations Benchmarking and Research. Academic Emergency Medicine. 2016;23(7):796–802. doi: 10.1111/acem.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mark BA, Harless DW. Adjusting for patient acuity in measurement of nurse staffing: Two approaches. Nursing research. 2011 Mar 1;60(2):107–14. doi: 10.1097/NNR.0b013e31820bb0c6. [DOI] [PubMed] [Google Scholar]
- 10.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical care. 2007 Dec 1;45(12):1195–204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 11.Center for Medicaid and Medicare Services, Department of Health and Human Services. 42 CFR Parts 410, 411, 412, 413, 414, 416, 419, 482, and 485. Medicare and Medicaid Programs; Interim and Final Rule Federal Register. Rules and Regulations. 2007;72(227):66580–66934. [Google Scholar]
- 12.Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2. Springer; New York: 2015. [Google Scholar]
- 13.Smith LR, Harrell FE, Muhlbaier . Problems and potentials in modeling survival. In: Grady ML, Schwartz HA, editors. Medical Effectiveness Data Methods (Summary Report) US Depart. Of Health and Human Services, Agency for Health Care Policy and Research; Rockville, MD: 1992. pp. 151–159.pp. 72 AHCPR, Pub No 92–0056. [Google Scholar]
- 14.Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone-Griffith S. Emergency department performance measures updates: proceedings of the 2014 Emergency Department Benchmarking Alliance Consensus Summit. Acad Emerg Med. 2015 May 1;22(5):542–53. doi: 10.1111/acem.12654. [DOI] [PubMed] [Google Scholar]
- 15.Hammer GP, du Prel JB, Blettner M. Avoiding bias in observational studies. Dtsch Arzteblatt Int. 2009;9(106):664–8. doi: 10.3238/arztebl.2009.0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pines JM, Mutter RL, Zocchi MS. Variation in emergency department admission rates across the United States. Med Care Res Rev. 2013;70(2):218–231. doi: 10.1177/1077558712470565. [DOI] [PubMed] [Google Scholar]
- 17.Wright S. Evaluation and Inspection. Office of the Inspector General; Washington DC: Jul 29, 2013. [Accessed: September 9, 2016]. Memorandum Report: Hospitals’ Use of Observational Stay and Short Inpatient Stays for Medicare Beneficiaries OEI -02-12-00040; pp. 1–20. Available at: https://oig.hhs.gov/oei/reports/oei-02-12-00040.pdf. [Google Scholar]
- 18.Barrett TW, Storrow AB, Jenkins CA, Abraham RL, Liu D, Miller KF, Moser KM, Russ S, Roden DM, Harrell FE, Darbar D. The AFFORD clinical decision aid to identify emergency department patients with atrial fibrillation at low risk for 30-day adverse events. Am J Cardiol. 2015;115(6):763–70. doi: 10.1016/j.amjcard.2014.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papke LE, Wooldridge JM. Econometric methods for fractional response variables with an application to 401K plan participation rates. [Accessed August 15, 2016];Journal of Applied Econometrics. 1996 11:619–632. Available at: http://faculty.smu.edu/millimet/classes/eco6375/papers/papke%20wooldridge%201996.pdf. [Google Scholar]
- 20.Anderson D, Pimentel L, Golden B, Wasil E, Hirshon JM. Drivers of ED efficiency: a statistical and cluster analysis of volume, staffing, and operations. The American journal of emergency medicine. 2016 Feb 29;34(2):155–61. doi: 10.1016/j.ajem.2015.09.034. [DOI] [PubMed] [Google Scholar]
- 21.Chao Jason, et al. Billing for physician services: a comparison of actual billing with CPT codes assigned by direct observation. Journal of Family Practice. 1998 Jul;:28. Academic OneFile. Web. 21 July 2016. [PubMed] [Google Scholar]
- 22.King MS, Lipsky MS, Sharp L. Expert agreement in Current Procedural Terminology evaluation and management coding. Archives of internal medicine. 2002 Feb 11;162(3):316–20. doi: 10.1001/archinte.162.3.316. [DOI] [PubMed] [Google Scholar]
- 23.Zuber TJ, Rhody CE, Muday TA, et al. Variability in code selection using the 1995 and 1998 HCFA documentation guidelines for office services. J Fam Pract. 2000:49642–645. [PubMed] [Google Scholar]