Abstract
Objective
To determine if 1) patients have distinct affective reaction patterns to medication information, and 2) whether there is an association between affective reaction patterns and willingness to take medication.
Methods
We measured affect in real time as subjects listened to a description of benefits and side effects (SEs) for a hypothetical new medication. Subjects moved a dial on a handheld response system to indicate how they were feeling from “Very Good” to “Very Bad”. Patterns of reactions were identified using a cluster-analytic statistical approach for multiple time series. Subjects subsequently rated their willingness to take the medication on a 7-point Likert scale. Associations between subjects’ willingness ratings and affect patterns were analyzed. Additional analyses were performed to explore the role of race/ethnicity regarding these associations.
Results
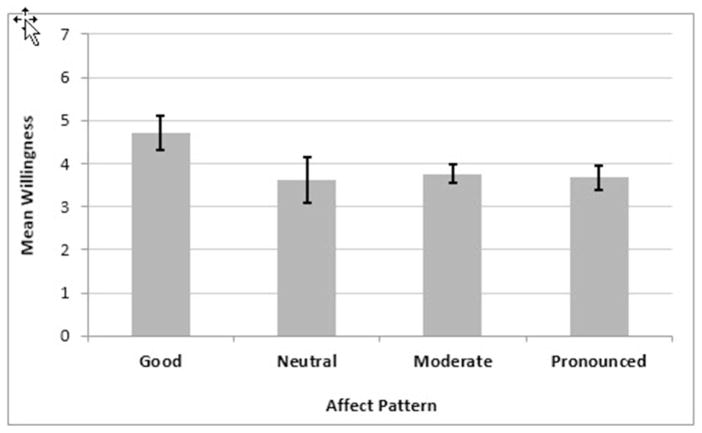
Clusters of affective reactions emerged that could be classified into four patterns: “Moderate” positive reactions to benefits and negative reactions to SEs (n= 186), “Pronounced” positive reactions to benefits and negative reactions to SEs (n= 110), feeling consistently “Good” (n= 58), and feeling consistently close to “Neutral” (n= 33). Mean (standard error) willingness to take the medication was greater among subjects feeling consistently Good 4.72 (0.20) compared to those in the Moderate 3.76 (0.11), Pronounced 3.68 (0.14), and Neutral 3.62 (0.26) groups. Black subjects with a Pronounced pattern were less willing to take the medication compared to both Hispanic (p= 0.0270) and White subjects (p= 0.0001) with a Pronounced pattern.
Conclusion
Patients’ affective reactions to information clustered into specific patterns. Reactions varied by race/ethnicity and were associated with treatment willingness. Ultimately, a better understanding of how patients react to information may help providers develop improved methods of communication.
Patient reluctance to take medications that have proven benefit is widespread and an important barrier to implementing clinical practice guidelines across many different conditions. Thus, understanding the factors which underlie patients’ decisions are critical to improving uptake and adherence to medical therapies. Although patients’ decision making is complex and influenced by a myriad of factors (e.g., patient-physician relationships, patients’ beliefs and/or values, risk tolerance, mood, as well as social/contextual factors such as insurance), numerous studies have documented the influence of affect on decision making.1,2
In 2002, Slovic et al.3 proposed a theoretical framework which described the significant influence of affect on judgment and decision making. In this context, affect (integral feelings about a stimulus that are experienced as one considers a stimulus) was defined as being based in experienced feelings of goodness and badness.4 Such emotional valence has been defined and measured with various similar terms including positive/negative.4
Affective reactions have been shown to have a strong influence on judgments5 and on people’s tendency to neglect probabilities. For example, society is willing to pay far more to remove a chemical that might cause cancer (a dreaded risk which evokes strong negative feelings) than to develop programs to prevent cardiovascular disease (an objectively greater hazard that does not, however, evoke strong feelings of fear or dread).6 In a recent study, Waters et al.7 found that, of four components underlying side effect (SE) perceptions associated with a necessary medication (negative affect, negative impact on social or physical function, and familiarity), affect was the strongest predictor of SE aversiveness.
There are several mechanisms by which affect may influence decision making. First, it may act as an important source of information.1 When presented with new information, patients react with feelings towards presented facts. Those feelings rather than the facts themselves are then thought to act as information in further judgments. In particular, feeling positive about the information leads to positive judgments, whereas the opposite is true for negative feelings.2,3,8 Affect can also influence decision making by refocusing attention on information consistent with the affective reaction. For example, good feelings about a medication may lead a patient to focus their attention on the medication’s benefits. In addition, affect can act as a common metric by enabling patients to compare treatment options based on how they feel about them as opposed to how they appraise their specific risks and benefits.1
Recent studies have extended our knowledge of how affect may influence decision making. In a replication and extension of earlier findings with respect to probability neglect in affect-rich scenarios,9 Suter et al.10 found that subjects draw upon different cognitive mechanisms when evaluating affect-rich versus affect-poor scenarios. Specifically, they found that affect-rich choices were less sensitive to probabilities and triggered activation in brain regions involved in processing emotions and memories. Affect-poor choices, on the other hand, were more sensitive to probabilities and activated brain regions known to be involved in cognitive and number processing.
Despite the influence of immediate affective responses in decision making, patients’ reactions to medication information in real time have not been previously measured. Moreover, the clear majority of studies have examined patients’ reactions to written materials, which may not be representative of reactions to spoken words in a clinical setting. Given the importance of understanding variability in affective responses to information communicated to patients in clinical practice and its impact on decision making, the objective of this study was to examine whether patients’ affective reactions to audible information influenced their willingness to take a newly described prescription medication.
In addition, because some studies have demonstrated differences in treatment preferences by race, we sought to explore whether race/ethnicity might moderate the relationship between affect and willingness. Kwoh et al.11, for example, found that minority patients were less willing to undergo total joint replacement than their Caucasian counterparts despite having comparable or greater levels of pain and disability. Similarly, Constantinescu et al.12 found that African American patients with active rheumatoid arthritis were less likely to choose to escalate their care compared to White patients, after adjusting for relevant sociodemographic factors. These results were due to a relative overweighting of rare complications and underweighting of benefits.13
To capture affective reactions in real time, subjects used a dial to continuously indicate how they felt as they listened to a physician describing a new medication for pain. We examined whether 1) affective reactions would vary, 2) subjects could be clustered by their patterns of affective reactions, and 3) specific affective reaction patterns would be associated with willingness to take medication.
Methods
Subjects
The study population was the same as described in a recent companion paper.14 Briefly, subjects were English-speaking persons with a diagnosed chronic systemic inflammatory disease, under the care of a rheumatologist. Subjects were compensated $25 at the end of a single face-to-face interview conducted by a trained research assistant.
Procedure
Subjects were randomized to listen to one of five versions of a hypothetical scenario describing a new medication. The versions varied in the amount and the order of risk benefit information. Actors were audiotaped as they read each of the five scripts. All versions began with the same introduction, after which the content included a brief or extended amount of information describing benefits and SEs. The five versions were created in order to examine the impact of varying risk communication strategies and have been published in a separate manuscript.14 Because of the possible effects of the audiotaped physicians’ ethnicity and gender on subjects’ affective reactions and risk perceptions,15–17 we asked each subject to select the physician from whom they would prefer to hear about a new medication by choosing one of six faces displayed on a computer screen (i.e. male or female physician of Black, White, or Hispanic race/ethnicity; images available upon request). We measured subjects’ affect in real time as they listened to the description of the risks and benefits of a new medication.
Reactions were measured using the Perception Analyzer (Dialsmith ®), a wireless handheld response system which uses a dial and runs on a Windows platform. Data are recorded at one second intervals based on the position of the dial. Ratings, mapped to the specific content of the presentation, are treated as continuous variables. Subjects were instructed to: “Please use the dial to show your feelings about what the doctor is saying as you watch the video.” Extreme ranges of the dial were 100= Very good on the left and 0= Very bad on the right, with the middle position 50 being neutral.18 This conceptualization of affect is similar to that used in studies of the affect heuristic.19 The recorded subject-generated data reflect the valence of subjects’ affect. All subjects practiced using the dial while listening to a weather forecast prior to engaging in the study task.
After hearing the presentation, subjects rated their willingness to take the described medication on a 7-point Likert rating scale (0= Not willing at all, 6= Extremely willing). Self-reported data on subject demographic and clinical characteristics were also collected. Subjective numeracy (perceived numerical aptitude and preference for numbers) was measured using the 8-item Subjective Numeracy Scale.20 A measure of numeracy was included because of previous published research documenting increased risk aversion in patients with lower levels of numeracy.21–23 We measured subjective numeracy because of the resistance we have previously encountered in our patient population to using objective numeracy measures which ask subjects to solve mathematical problems.
Statistical Methods
The five scenarios coupled with the different speakers (based on the selected physician) varied in length of time and number of time points. Valid cluster analysis within each scenario, independent of the chosen speaker’s presentation, required rescaling the data streams within scenarios to a common standardized timeline consisting of 100 affect response values (1=start, 100=end). Linear interpolation was used to rescale all signals to a standard time series of 100 equally spaced measurement times. Then, separately for each scenario, groups of similar longitudinal patterns of affect reactions were identified using a cluster-analytic statistical approach developed for classifying independent univariate time series obtained from multiple subjects. Specifically, we used a Euclidean dissimilarity approximation based on area between two series to generate a dissimilarity matrix between subjects’ series, followed by ‘partitioning-around-medoids’ (pam) for generating cluster solutions consisting of a specified number (k) of clusters. Then, for each specific k-cluster solution, ‘silhouette plots’ were examined and a summary measure, ‘average silhouette width’ (asw), was calculated. Visual comparison of silhouette plots and the asw indicate whether there is a good structure to the k-cluster solution, i.e., whether most observations seem to belong to the cluster to which they are assigned. This heuristic approach was used to select a ‘best’ choice for the number of clusters to be retained separately for each scenario. R packages TSdist24, fpc25, and cluster26 were used to perform the calculations and to produce the plots for each of the five scenarios. The emergent clusters were observed to have affect patterns that could be similarly labeled across the scenarios. For parsimony and ease of interpretability and analysis, we settled on four affect patterns (Moderate, Pronounced, Neutral, and Good).
We used multivariate linear regression modeling to examine the association between affect patterns and willingness to take medication. Affect was treated as a nominal 4-level categorical variable. We adjusted for variables having the potential to influence the association between affect pattern and willingness to take medication: ethnicity (three nominal levels: Hispanic, Black, White), age, subjective numeracy, patient global assessment of disease activity, and a binary indicator of current use of a disease modifying medication (traditional disease modifying anti-rheumatic drug, biologic, cyclosporine, azathioprine, mycophenylate mofetil, or cyclophosphamide).12,13,21,27,28 We adjusted p-values for multiple comparisons with an adaptive linear step-up adjustment to control false discovery rate at α=0.05 using the SAS® v 9.4 MULTTEST procedure.29
Additionally, we modeled the interaction of ethnicity with affect pattern effects by including a 3-level main effect term for ethnicity, a 4-level main effect term for affect pattern, and a 3 X 4 cross-product term for modification of the affect effect by ethnicity. The adjusted estimates of the coefficients for the interactions were used to calculate least squares means and their pairwise differences. An omnibus Type 3 sum of squares test was used to assess global statistical significance of the effect modification heterogeneity.
A single-imputation method, ‘predicted means’, was used so that five subjects having missing values for age could be included in the statistical analyses. Imputed values were predicted using an ordinary least-squares multiple regression algorithm to impute the most likely value. The imputation model for age consisted of the variables subjective numeracy, use of disease modifying drugs, ethnicity, and global score. The imputation was performed using SOLAS v4.02 ©2011, Statistical Solutions, Ltd. (http://www.statsols.com/products/solas-for-missing-data/).
Results
Of the 432 subjects contacted, 395 agreed to participate in the study (91%). Of these, two were excluded because of hearing impairments, one was excluded because of a language barrier, and five were excluded because the computer malfunctioned.
Subject Characteristics
The mean (SD) age of the analytic sample (N= 387) was 55 (14) years, 75% were female; 59% identified themselves as Non-Hispanic White (hereafter referred as White), 23% as Non-Hispanic Black (hereafter referred as Black), and 18% as Hispanic; participants could not choose more than one primary racial/ethnic identity. The three most commonly reported systemic inflammatory diagnoses were rheumatoid arthritis (53%), systemic lupus (20%), and psoriatic arthritis (16%). Thirty-three percent reported having very good or excellent health, and the majority of subjects (82%) were currently taking a disease modifying drug.
Affect Patterns
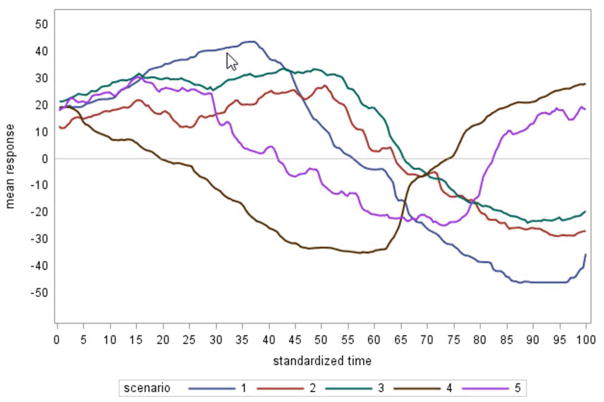
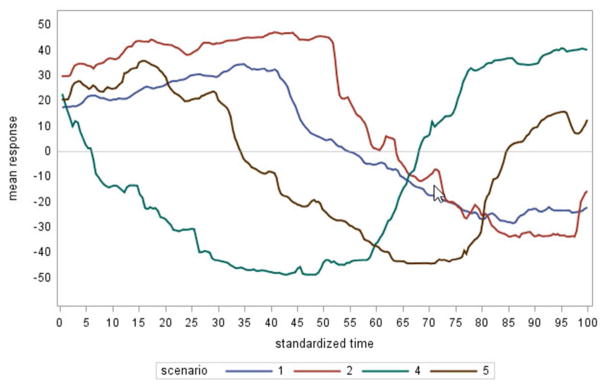
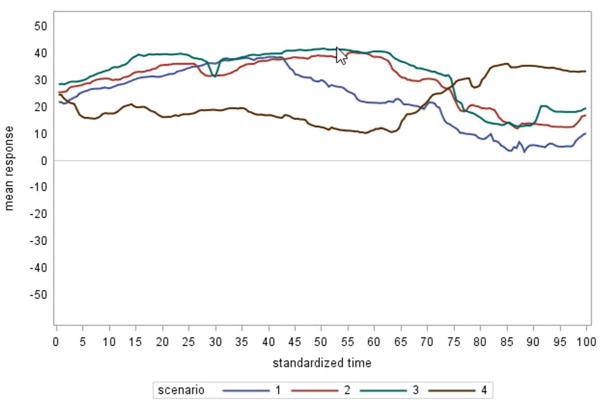
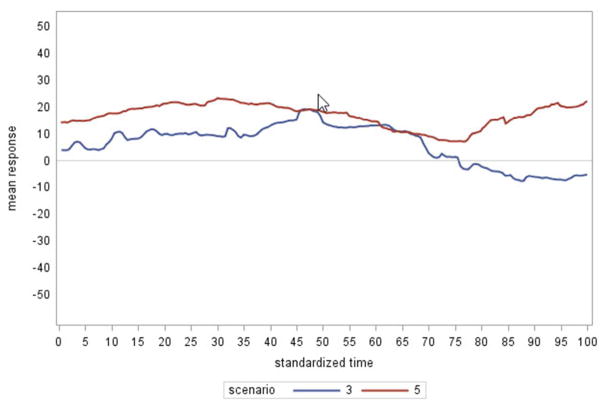
Affective reactions varied and were classified into four patterns. The largest group (n= 186) felt “Moderate” and had positive scores while listening to benefits and negative scores while listening to risks (Figure 1). The next largest group (n= 110) also indicated feeling good and bad while listening to the benefits and risks respectively, but had more “Pronounced” reactions than did the Moderate group (Figure 2). A third group (n= 58) felt consistently “Good” while listening to the medication description (Figure 3). These subjects’ scores were more positive while listening to the benefits than to the risks, but scores remained positive throughout the scenarios. The smallest group (n= 33) exhibited little reaction and remained fairly “Neutral” throughout the scenarios (Figure 4). Two subjects were excluded from the analyses because they did not fit within one of the four affect patterns.
Figure 1.
Moderate reaction to benefits and side effects (n = 186)
Scenario #1: Brief benefits followed by extended side effects
Figure 2.
Pronounced reaction to benefits and side effects (n = 110)
Scenario #2: Extended benefits followed by extended side effects
Figure 3.
Consistently Good reaction to benefits and side effects (n = 58)
Scenario #3: Extended benefits followed by brief side effects
Figure 4.
Consistently Neutral reaction to benefits and side effects (n = 33)
Scenario #4: Extended side effects followed by brief benefits
Subjects’ clinical and demographic characteristics by affect pattern are shown in Table 1. Of the variables measured, only ethnicity was significantly associated with affect pattern. Post hoc analyses revealed that the only significant difference was a higher than expected number of White subjects and a lower than expected number of Hispanic subjects in the Good affect pattern.
Table 1.
Descriptive Summary Statistics for Clinical and Demographic Patient Characteristics by Affect Type
| Characteristics | All N= 387 |
Moderate n= 186 (48%) |
Pronounced n= 110 (28%) |
Good n= 58 (15%) |
Neutral n= 33 (9%) |
p-value |
|---|---|---|---|---|---|---|
| Age (yrs), mean (SD) | 54.8 (14.1) | 55.5 (13.7) | 54.6 (14.3) | 54.0 (13.5) | 52.7 (16.7) | 0.0890 a |
| Numeracy, mean (SD) | 3.83 (1.23) | 3.80 (1.23) | 3.72 (1.25) | 4.22 (1.13) | 3.73 (1.22) | 0.0729 a |
| Patient global, mean (SD) | 4.55 (2.62) | 4.82 (2.59) | 4.55 (2.69) | 4.10 (2.46) | 3.79 (2.61) | 0.7008 a |
| Duration (yrs), mean (SD) | 10.8 (8.5) | 10.8 (8.2) | 11.0 (7.7) | 10.2 (8.3) | 11.1 (12.3) | 0.9491 a |
| Female, n (%) | 289 (75) | 137 (47) | 85 (29) | 43 (15) | 24 (8) | 0.8994 b |
| Ethnicity, n (%) | ||||||
| Hispanic | 71 (18) | 38 (54) | 21 (30) | 3 (4) | 9 (12) | 0.0446 b |
| Black | 89 (23) | 43 (48) | 28 (32) | 11 (12) | 7 (8) | |
| White | 227 (59) | 105 (46) | 61 (27) | 44 (19) | 17 (7) | |
| Current disease modifying drug, n (%) | 318 (82) | 156 (49) | 91 (29) | 41 (13) | 30 (9) | 0.0791 b |
| Some college, n (%) | 242 (63) | 118 (49) | 65 (27) | 42 (17) | 17 (7) | 0.1882 b |
| Married, n (%) | 169 (44) | 70 (41) | 53 (31) | 32 (19) | 14 (8) | 0.0770 b |
| Employed, n (%) | 150 (39) | 78 (52) | 39 (26) | 25 (17) | 8 (5) | 0.1965 b |
| Willingness, mean (SD) | 3.77 (1.47) | 3.67 (1.72) | 4.71 (1.18) | 3.61 (1.97) | 0.0001c | |
| Hispanic | 4.17 (1.18) | 4.24 (1.17) | 4.05 (1.40) | 5.00 (1.73) | 3.89 (1.62) | 0.7047f |
| Non-Hispanic Black | 3.36 (1.63) | 3.63 (1.40) | 2.75 (1.60) | 4.36 (1.50) | 2.57 (2.30) | 0.0065f |
| Non-Hispanic White | 3.97 (1.61) | 3.67 (1.57) | 3.97 (1.74) | 4.77 (1.08) | 3.88 (1.96) | 0.0011f |
| 0.0011d | 0.1111g | 0.0011g | 0.6872g | 0.1305g | 0.1648e |
Association test p-values:
1-way Global Type 3 test of linear model fixed effects, F(3,383)
Fisher’s Exact Test
2-way ANOVA affect main effect, F(3,375)
2-way Global Type 3 test of linear model fixed effects ethnicity main effect, F(2,375)
2-way ANOVA affect*ethnicity interaction, F(6,375)
2-way Global Type 3 test of linear model fixed effects, ethnicity simple effects F(3,375)
2-way Global Type 3 test of linear model fixed effects, simple effects F(2,375)
Association between Affect and Willingness to Take the Medication
Mean willingness ratings by affect and ethnicity group are presented in Table 1. After adjusting for age, subjective numeracy, current use of a disease modifying medication, and patient global assessment of disease activity, least squares mean (standard error) willingness to take the medication was greater among subjects feeling consistently Good [4.72 (0.20)] compared to those who felt Moderate 3.76 (0.11), Pronounced 3.68 (0.14) and Neutral 3.62 (0.26), respectively (Figure 5).
Figure 5.
Mean* willlingness to take medication per affect pattern
*LS Means adjusted for age, subjective numeracy, current use of a disease modifying drug, and patient global disease activity. Bars indicate 95% confidence intervals.
Scenario #5: Benefits followed by extended side effects followed by benefits
Given the association between affect pattern and ethnicity, we further explored the relationships between affect pattern, ethnicity, and willingness to take the medication. With few exceptions, willingness was similar across ethnic groups and affect pattern. However, estimated differences of adjusted least squares means (p-values corrected for multiplicity) demonstrated that Black subjects with a Pronounced affect pattern were less willing to take the medication compared to both Hispanic (t= 2.80, p= 0.0270) and White subjects (t= 4.13, p= 0.0001) with a Pronounced pattern. In addition, both Black and White subjects who felt consistently Good were more willing to take the medication compared to Black (t= 2.92, p= 0.0259) and White (t= 2.71, p= 0.0327) subjects with a Pronounced affect pattern. White subjects feeling consistently Good were also more willing to take the medication compared to White subjects with a Moderate affect pattern (t= 4.21, p= 0.0001). We found no association between affect pattern and willingness among Hispanic subjects. All estimated differences between ethnic groups within each affect pattern and between affect patterns within each ethnic group are included in Tables 2a and 2b. Because subjects each listened to one of five versions of the scenario, we considered version as a confounder and as an effect modifier. It did not, however, play any role in the associations between affect pattern, ethnicity, and willingness to take the medication (all significance tests > 0.05).
Table 2a.
Estimated Difference of Least Squares Means for Willingness to Take the Medication between Ethnic Subgroups (within each Affect Pattern)
| Affect Pattern | Comparison | Estimate | SE | DF | t Value | P > |t| | Adjusteda p-value | |
|---|---|---|---|---|---|---|---|---|
| Moderate (n= 186) | Hispanic | Black | 0.52 | 0.33 | 371 | 1.57 | 0.1162 | 0.2324 |
| Hispanic | White | 0.28 | 0.30 | 371 | 0.95 | 0.3448 | 0.4499 | |
| Black | White | −0.24 | 0.28 | 371 | −0.86 | 0.3913 | 0.4499 | |
| Pronounced (n= 110) | Hispanic | Black | 1.19 | 0.43 | 371 | 2.80 | 0.0054 | 0.0270 |
| Hispanic | White | −0.24 | 0.38 | 371 | −0.63 | 0.5320 | 0.5320 | |
| Black | White | −1.43 | 0.34 | 371 | −4.13 | <.0001 | 0.0001 | |
| Good (n= 58) | Hispanic | Black | 0.80 | 0.95 | 371 | 0.83 | 0.4049 | 0.4499 |
| Hispanic | White | 0.11 | 0.88 | 371 | 0.13 | 0.8994 | 0.8994 | |
| Black | White | −0.68 | 0.51 | 371 | −1.35 | 0.1766 | 0.2943 | |
| Neutral (n= 33) | Hispanic | Black | 1.16 | 0.74 | 371 | 1.57 | 0.1162 | 0.2324 |
| Hispanic | White | −0.10 | 0.61 | 371 | −0.17 | 0.8681 | 0.8681 | |
| Black | White | −1.26 | 0.66 | 371 | −1.91 | 0.0575 | 0.1917 | |
LS means adjusted for age, subjective numeracy, current use of a disease modifying medication, and patient global assessment of disease activity; p-values are corrected for multiplicity.
Discussion
Affect is known to have a significant influence on decision making across domains; people make both important and trivial decisions based on their emotions.1,2,8,30 Despite the importance of affect, relatively few studies have quantified emotional reactions to medical information in real time, and, to the best of our knowledge, none have examined affective responses to audible information in real time.
In this study, most subjects had a Moderate affect pattern, i.e., they felt good when listening to a description of benefits and bad when listening to a description of SEs, but generally avoided the extreme ranges of the scale. The second largest group reported feeling the same pattern of affect, but with greater intensity. A small group of subjects reported more muted responses with little variability in affect; other subjects varied in the affect they reported, but kept the dial in the positive range throughout the presentation. Notably, the latter reported being significantly more willing to take the medication compared to the other three groups. Interestingly, subjects in the consistently Good pattern reacted similarly to other groups when hearing about the benefits of the medication, but did not react as negatively to the risks. Thus, it appears that willingness to take medication is driven primarily by differences in subjects’ reactions to risk, as opposed to benefit, information. This finding is consistent with Fried et al.’s31 study in which older persons’ willingness to take medication for primary cardiovascular prevention was also more strongly influenced by risks than benefits. Less clear from the present data is whether affect was used as information to guide willingness to take the medication or whether negative affect towards the medication caused subjects to attend more to negative SE-related information and less to positive information describing benefits.9
Consistent with previous literature demonstrating that Black subjects may be less willing to accept risky treatment or to undergo elective surgery,12,32,33 Black subjects in the present study were less willing to take the medication compared to their White and Hispanic counterparts. The paired comparisons revealed that this lower willingness among Black subjects was strongest among those with a Pronounced affect pattern. These results suggest that disparities in treatment preferences may be influenced by differences in the influence of affect on judgement. The limited studies that have compared treatment preferences in Hispanic versus Non-Hispanic patients in the U.S. demonstrate mixed results. Cooper et al.34 found that Hispanics had weaker preferences for antidepressant medications compared to White patients. Hispanic patients have also been shown to be more likely to prefer life prolonging care compared to White patients.35 In the present study, we found no differences in willingness to take the medication in Hispanic versus Non-Hispanic subjects. Despite underutilization of treatment in rheumatoid arthritis36 and total joint replacement37 among Hispanic patients, few studies describing their treatment preferences in rheumatic conditions have been published. However, consistent with our findings, both Souchek et al.38 and Byrne et al.39 found no differences between Hispanic and White subjects’ valuations for arthritis-related health states.
Limitations of the study include the use of a hypothetical scenario, which enabled us to use an experimental design, but cannot replicate communication between patients and their physicians. Moreover, although we adjusted for perception of disease activity and current use of medications, treatment decisions are likely also influenced by numerous other factors such as patient-physician relationships, patients’ beliefs and/or values, risk tolerance, mood, as well as social/contextual factors such as insurance. Whether these factors moderate affective reactions would be important to examine in future studies. One might expect, for example, that having negative attitudes towards medication might drive more pronounced affect reactions whereas having had positive personal experiences might drive moderate reactions.
In addition, our primary objective was to examine whether affective reactions varied among subjects and whether these affective reactions could be clustered in meaningful ways. Thus, unlike some other studies investigating the role of affect in decision making, we did not manipulate affect. As interviews were conducted in a convenient place chosen by the subject (usually their homes), objective measurements of arousal were not performed because we did not have the required equipment. We also did not include baseline measures of mood (e.g., the PANAS) in our model. Given the impact of mood on risk perceptions5, future research should examine whether current mood modifies affective reactions to health-related information. In addition, the number of subjects in specific subgroups may have limited our ability to achieve statistical significance of associations between affect and willingness to take medication among minority subjects. Moreover, we recruited a convenience sample of subjects which limits the generalizability of our results. Lastly, although used in other fields, the software used in this study has not been validated in previous health-related studies.
In summary, affective reactions to information heard about a potential new medication can be clustered into distinct patterns. Subjects who did not react negatively to risk information were more willing to take a new medication compared to those feeling bad when hearing about SEs. Moreover, Black subjects with Pronounced affect patterns were less willing than Hispanic or White subjects. Ultimately, a better understanding of how patients react to information may help providers develop improved methods of communication. For example, inquiring how patients feel after hearing about SEs and further tailoring risk information to those who feel bad may prove to support decision making more effectively than trying to convince patients about the benefits of a recommended treatment. Providing these same patients with information on how best to decrease their risk and/or cope with SEs, may also enable them to be more open to considering treatment. However, future research is needed to examine whether and how best to tailor communication based on explicit inquiry of affective reactions to risk.
Table 2b.
Estimated Difference of Least Squares Means for Willingness to Take the Medication between Affect Patterns (within Ethnic Subgroups)
| Ethnic Group | Comparison | Estimate | SE | DF | T Value | Pr > |t| | Adjusteda p-value | |
|---|---|---|---|---|---|---|---|---|
| Hispanic (n= 71) | Moderate | Pronounced | 0.19 | 0.40 | 371 | 0.48 | 0.6295 | 0.6295 |
| Moderate | Good | −0.94 | 0.89 | 371 | −1.06 | 0.2899 | 0.3382 | |
| Moderate | Neutral | 0.24 | 0.54 | 371 | 0.44 | 0.6604 | 0.6604 | |
| Pronounced | Good | −1.14 | 0.91 | 371 | −1.25 | 0.2128 | 0.2929 | |
| Pronounced | Neutral | 0.04 | 0.58 | 371 | 0.08 | 0.9387 | 0.9387 | |
| Good | Neutral | 1.18 | 0.98 | 371 | 1.20 | 0.2301 | 0.2929 | |
| Black (n= 89) | Moderate | Pronounced | 0.87 | 0.36 | 371 | 2.42 | 0.0158 | 0.0553 |
| Moderate | Good | −0.66 | 0.50 | 371 | −1.34 | 0.1820 | 0.2831 | |
| Moderate | Neutral | 0.88 | 0.60 | 371 | 1.47 | 0.1416 | 0.2831 | |
| Pronounced | Good | −1.52 | 0.52 | 371 | −2.92 | 0.0037 | 0.0259 | |
| Pronounced | Neutral | 0.01 | 0.62 | 371 | 0.02 | 0.9816 | 0.9816 | |
| Good | Neutral | 1.54 | 0.71 | 371 | 2.17 | 0.0306 | 0.0714 | |
| White (n= 227) | Moderate | Pronounced | −0.32 | 0.24 | 371 | −1.37 | 0.1711 | 0.2831 |
| Moderate | Good | −1.11 | 0.26 | 371 | −4.21 | <.0001 | 0.0001 | |
| Moderate | Neutral | −0.14 | 0.38 | 371 | −0.38 | 0.7069 | 0.7069 | |
| Pronounced | Good | −0.79 | 0.29 | 371 | −2.71 | 0.0070 | 0.0327 | |
| Pronounced | Neutral | 0.18 | 0.40 | 371 | 0.45 | 0.6553 | 0.6553 | |
| Good | Neutral | 0.97 | 0.42 | 371 | 2.31 | 0.0214 | 0.0599 | |
LS means adjusted for age, subjective numeracy, current use of a disease modifying medication, and patient global assessment of disease activity; p-values are corrected for multiplicity.
Acknowledgments
This clinical research study was made possible by a grant from the Arthritis Foundation. Research reported in this publication was also supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, part of the National Institutes of Health, under Award Number AR060231-01 (Fraenkel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Peters is supported by National Science Foundation Grants SES-1155924 and 1558230. Dr. Street is supported by the Houston VA Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413).
The authors do not have any financial interests that would be considered a conflict of interest. Each of the co-authors listed has had a substantial role in the creation of this manuscript and the work reported herein.
Appendix
Each version started with the same introduction:
Hello, my name is Dr - and I know we have never met before – but for the next few minutes – try and pretend that I am your regular doctor. In this video I am going to be telling you about a new medication. Ok let’s start:
There is a medication that I would like to recommend for you. Before we get into details, it is important that you know that the medication is completely covered by your insurance. It is a small pill taken once a day and it does not interfere with any of your other medications. This medication works by targeting specific cells of the immune system that in your case are overactive and cause inflammation. It tends to start working quickly, so you may feel the benefits within 2 to 4 weeks. So let’s talk about the benefits of this medication:
To facilitate comparisons, comparable content are presented in the same font across brief and extended benefits. The description of sleep is unique to the extended benefits scenario (ALL CAPITALIZED). The same applies to the brief and extended adverse event descriptions.
Brief Benefits
First, it is very effective for relieving pain and fatigue. About half (or 50%) of the people taking this medication have mild to moderate pain every now and then and very little fatigue. And about one quarter (or 25%) will improve to the point where they are almost completely pain free and have as much energy as they did before they got sick. Because patients taking this medication have less pain and fatigue, they are able to be more active, work (either in or outside of the home) with less difficulty, and participate in more social and recreational activities outside of the house. What is really important is that this medication doesn’t just treat your symptoms. It is aimed at targeting the actual cause of your illness, and so it decreases the chance of flare ups and the progression of your disease. Because the medication controls the underlying disease it also decreases your risk of future complications that are caused by years of inflammation such as heart attacks.
Extended Benefits
First, it is very effective for relieving pain. About half (or 50%) of the people taking this medication will have their pain reduced to the point where they only have mild to moderate pain every now and then which doesn’t prevent them from doing the activities they want to do. And about one quarter (or 25%) of people will improve to the point where they are almost completely pain free. THIS MEDICATION CAN ALSO IMPROVE THE QUALITY OF YOUR SLEEP. THIS IS IMPORTANT BECAUSE PATIENTS WITH YOUR ILLNESS OFTEN HAVE TROUBLE SLEEPING. AND THEY HAVE DISRUPTED SLEEP PATTERNS WHEN MEASURED IN A SPECIALIZED SLEEP LABORATORY. MANY PATIENTS, EVEN THOSE WHO SLEEP WELL – OFTEN FEEL VERY FATIGUED OR TIRED. THE FATIGUE IS CAUSED BY AN INCREASED LEVEL OF SPECIFIC CHEMICALS IN YOUR BLOOD. THE MEDICATION DECREASES THE LEVELS OF THESE CHEMICALS AND THAT’S WHY PATIENTS FEEL LESS FATIGUED AND MORE ENERGETIC. Because patients feel better, they are able to be more active, work with less difficulty, (regardless of whether you work at home or outside of the home) and have an easier time enjoying social, leisure, and recreational activities outside of the house. What is really important is that this medication doesn’t just treat your symptoms. It is aimed at targeting the actual cause of your illness, and so it decreases the chance of flare ups and it decreases the progression of your disease. Controlling the underlying disease also decreases your risk of future complications. Patients who have illnesses that cause inflammation are at higher risk for heart disease. Taking this medication and controlling inflammation now, may lower your risk of having a heart attack in the future.
Brief Adverse Events
The medication is very well tolerated in almost all patients who take it – but there are some side effects that you need to be aware of. About 10% of people taking the medication have some stomach discomfort or headaches from the medication. Patients taking this medication are at increased risk of infections such as bronchitis. Bronchitis happens in about 10% to 15% of patients and can be easily treated with antibiotics. Pneumonia which happens more rarely – in about 3% of people – needs to be treated in the hospital with intravenous antibiotics. Sepsis is a very serious condition that can decrease blood flow to your heart, lungs and kidneys. It happens in about 1 in 1000 people taking this medication. Sepsis is always treated in the intensive care unit and can rarely be life threatening. When this medication came on the market doctors worried that it might weaken the immune system’s ability to recognize early cancer cells. While we are still not certain whether or not these drugs increase the risk of cancer, large studies have not shown any significant increased risk in adults taking this medication compared to adults taking other medications.
Extended Adverse Events
The medication is very well tolerated in almost all patients who take it – but there are some side effects that you need to be aware of. About 10% of people taking the medication have some stomach upset or a queasy feeling that comes and goes. About the same number of patients, about 10%, develop a headache and some dizziness or lightheadedness from the medication. If needed the headaches can be treated with Tylenol. Patients taking this medication are at increased risk of infections. About 10 to 15% of patients develop bronchitis. This is when you feel like you have a cold and have a cough and you may have a fever. This type of bronchitis gets better in about a week with antibiotics that you take by mouth. About 3% of people develop pneumonia that needs to be treated in a hospital with intravenous (or IV) antibiotics for about a week. People who have had pneumonia say that it takes a good 3 weeks to start feeling like yourself again. About 1 in 1,000 people develop a serious infection called “sepsis”. Sepsis can decrease blood flow to the kidneys, liver, and lungs and is always treated in the intensive care unit with intravenous (or IV) medications. In rare cases, sepsis can be life threatening. When this medication came on the market, doctors worried that it might increase the risk of cancer. One of the jobs of the immune system is to find early cancer cells and destroy them. Doctors worried that this medication might weaken the immune system’s ability to recognize these early cancer cells. While we are still not certain whether or not this medication increases the risk of cancer, several large studies done over the past 10 years, have not shown any increased risk of cancer in adults taking this medication.
References
- 1.Peters E, Lipkus I, Diefenbach MA. The functions of affect in health communications and in the construction of health preferences. J Commun. 2006;56:S140–S62. [Google Scholar]
- 2.Slovic P, Peters E, Finucane ML, Macgregor DG. Affect, risk, and decision making. Health Psychol. 2005;24:S35–40. doi: 10.1037/0278-6133.24.4.S35. [DOI] [PubMed] [Google Scholar]
- 3.Slovic P, Finucane M, Peters E, MacGregor DG. The affect heuristic. In: Gilovich T, Griffin D, Kahneman D, editors. Heuristics and biases: The psychology of intuitive judgment. Cambridge, UK: Cambridge University Pres; 2002. pp. 397–420. [Google Scholar]
- 4.Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24:311–22. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson EJ, Tversky A. Affect, generalization, and the perception of risk. J Pers Soc Psychol. 1983;45:20–31. [Google Scholar]
- 6.Reynolds T. News headlines feed on fear of cancer risk, experts say. J Natl Canc Inst. 2001;93:9–11. doi: 10.1093/jnci/93.1.9. [DOI] [PubMed] [Google Scholar]
- 7.Waters EA, Pachur T, Colditz GA. Side effect perceptions and their impact on treatment decisions in women. Med Decis Making. 2017;37:193–203. doi: 10.1177/0272989X16650664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters EM, Burraston B, Mertz CK. An emotion-based model of risk perception and stigma susceptibility: Cognitive appraisals of emotion, affective reactivity, worldviews, and risk perceptions in the generation of technological stigma. Risk Anal. 2004;24:1349–67. doi: 10.1111/j.0272-4332.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 9.Rottenstreich Y, Hsee CK. Money, kisses and electric shocks: On the affective psychology of risk. Psychol Sci. 2001;12:185–90. doi: 10.1111/1467-9280.00334. [DOI] [PubMed] [Google Scholar]
- 10.Suter RS, Pachur T, Hertwig R, Endestad T, Biele G. The neural basis of risky choice with affective outcomes. PLoS One. 2015;10:e0122475. doi: 10.1371/journal.pone.0122475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwoh CK, Vina ER, Cloonan YK, Hannon MJ, Boudreau RM, Ibrahim SA. Determinants of patient preferences for total knee replacement: African-Americans and whites. Arthritis Res Ther. 2015;17:348. doi: 10.1186/s13075-015-0864-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Constantinescu F, Goucher S, Weinstein A, Fraenkel L. Racial disparities in treatment preferences for rheumatoid arthritis. Med Care. 2009;47:350–55. doi: 10.1097/MLR.0b013e31818af829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Constantinescu F, Goucher S, Weinstein A, Smith W, Fraenkel L. Understanding why rheumatoid arthritis patient treatment preferences differ by race. Arthritis Rheum. 2009;61:413–8. doi: 10.1002/art.24338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fraenkel L, Stolar M, Swift S, Richard L, Street J, Chowdhary H, Peters E. Subjective numeracy and the influence of order and amount of audible information on perceived medication value. Med Decis Making. 2017;37:230–8. doi: 10.1177/0272989X16650665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 17.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 18.Carpenter S, Peters E, Isen AM, Vastfjall D. Positive feelings facilitate working memory and complex decision making among older adults. Cogn Emot. 2013;27:184–92. doi: 10.1080/02699931.2012.698251. [DOI] [PubMed] [Google Scholar]
- 19.Peters E, Slovic P. Affective asynchrony and the measurement of the affective attitude component. Cogn Emot. 2007;21:300–29. [Google Scholar]
- 20.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: Development of the Subjective Numeracy Scale (SNS) Med Decis Making. 2007;27:672–80. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 21.Fraenkel L, Cunningham M, Peters E. Subjective numeracy and preference to stay with the status quo. Med Decis Making. 2015;35:6–11. doi: 10.1177/0272989X14532531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peters E. Beyond comprehension: The role of numeracy in judgments and decisions. Curr Dir Psychol Sci. 2012;21:31–5. [Google Scholar]
- 23.Peters E, Västfjäll D, Slovic P, Mertz CK, Mazzocco K, Dickert S. Numeracy and decision making. Psychol Sci. 2006;17:407–13. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- 24.TSdist: Distance Measures for Time Series Data. at https://cran.r-project.org/web/packages/TSdist/index.html.
- 25.fpc: Flexible Procedures for Clustering. at https://cran.r-project.org/web/packages/fpc/index.html.
- 26.cluster: “Finding Groups in Data”: Cluster Analysis Extended. at https://cran.r-project.org/web/packages/cluster/index.html.
- 27.Peters E. Numeracy and the perception and communication of risk. Ann NY Acad Sci. 2008;1128:1–7. doi: 10.1196/annals.1399.001. [DOI] [PubMed] [Google Scholar]
- 28.Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychological Bulletin. 2009;135:943–73. doi: 10.1037/a0017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benjamini Y, Krieger AM, Yekutieli D. Adaptive linear step-up procedures that control the false discovery rate. Biometrika. 2006;93:491–507. [Google Scholar]
- 30.Pachur T, Hertwig R, Wolkewitz R. The affect gap in risky choice: Affect-rich outcomes attenuate attention to probability information. Decision. 2014;1:64–78. [Google Scholar]
- 31.Fried TR, Tinetti ME, Towle V, O’Leary JR, Iannone L. Effects of benefits and harms on older persons’ willingness to take medication for primary cardiovascular prevention. Arch Intern Med. 2011;171:923–8. doi: 10.1001/archinternmed.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kwoh CK, Vina ER, Cloonan YK, Hannon MJ, Boudreau RM, Ibrahim SA. Determinants of patient preferences for total knee replacement: African-Americans and whites. Arthritis Res Ther. 2015;17:348. doi: 10.1186/s13075-015-0864-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vina ER, Masi CM, Green SL, Utset TO. A study of racial/ethnic differences in treatment preferences among lupus patients. Rheumatology (Oxford, England) 2012;51:1697–706. doi: 10.1093/rheumatology/kes128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003;41:479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 35.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: Impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26:4131–7. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chu LH, Portugal C, Kawatkar AA, Stohl W, Nichol MB. Racial/ethnic differences in the use of biologic disease-modifying antirheumatic drugs among California Medicaid rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 2013;65:299–303. doi: 10.1002/acr.21798. [DOI] [PubMed] [Google Scholar]
- 37.Escalante A, Espinosa-Morales R, del Rincon I, Arroyo RA, Older SA. Recipients of hip replacement for arthritis are less likely to be Hispanic, independent of access to health care and socioeconomic status. Arthritis Rheum. 2000;43:390–9. doi: 10.1002/1529-0131(200002)43:2<390::AID-ANR20>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 38.Souchek J, Byrne MM, Kelly PA, et al. Valuation of arthritis health states across ethnic groups and between patients and community members. Med Care. 2005;43:921–8. doi: 10.1097/01.mlr.0000173600.53788.13. [DOI] [PubMed] [Google Scholar]
- 39.Byrne MM, O’Malley KJ, Suarez-Almazor ME. Ethnic differences in health preferences: analysis using willingness-to-pay. J Rheumatol. 2004;31:1811–8. [PubMed] [Google Scholar]