Abstract
Background:
Surgical treatment of cervical myelopathy is common, and the impact of perioperative malnutrition in these patients is unclear; yet, malnutrition pre- and postoperatively has been associated with higher rates of wound infection in spine patients. We evaluated the association of low prealbumin level, a marker for poor nutrition, with length of hospitalization and complication rates after surgery for cervical myelopathy.
Methods:
We retrospectively identified patients with cervical myelopathy who underwent anterior cervical discectomy and fusion, anterior cervical corpectomy and fusion, or posterior cervical decompression and fusion over a 5-year period. Patients’ prealbumin levels were measured within 4 days of surgery; they were divided into low and normal groups (threshold 15 mg/dL). Demographic, clinical, operative, and postoperative parameters were correlated with prealbumin levels by utilizing univariate and multivariable analyses.
Results:
Eighteen patients were in the “low prealbumin” group and 37 were in the “normal prealbumin” group. Patients with low prealbumin were significantly more likely to have an extended length of hospitalization/stay (LOS) (median 6 days, interquartile range 7.5 days vs. median 3 days, interquartile range 2 days, P < 0.001) and more postoperative complications (33% versus 0%, P < 0.001). Multivariable analysis revealed that only the low prealbumin category (P < 0.001) was associated with a prolonged LOS.
Conclusions:
Low prealbumin levels were associated with prolonged LOS after surgery for cervical myelopathy. We need to better define the effects of malnutrition in patients with cervical myelopathy in the future.
Keywords: Cervical myelopathy, complications, length of stay, malnutrition, prealbumin
INTRODUCTION
Malnutrition is relatively common among patients undergoing cervical spinal surgery for myelopathy,[4] and low preoperative prealbumin levels likely contribute to higher rates of wound infections. Here, we assessed the relationship between perioperative malnutrition, as measured by serum prealbumin levels, with the length of stay (LOS) and outcomes/complications in patients undergoing three types of cervical surgery for myelopathy.
MATERIALS AND METHODS
Hypothesis
We hypothesized that patients with cervical myelopathy who have perioperative malnutrition, as indicated by low serum prealbumin levels, have worse clinical outcomes compared with patients with normal prealbumin levels.
Study population
Approvals from the Institutional Review Board were obtained for all patients. We retrospectively evaluated patients 18 years or older with cervical myelopathy who underwent anterior cervical discectomy and fusion, anterior cervical corpectomy and fusion, or posterior cervical decompression and fusion. Those who had prealbumin levels available for analysis were included in the study. Patients who had multiple procedures in a staged manner (e.g., an anterior cervical discectomy and fusion followed by a posterior spinal fusion) were excluded from the analysis. All surgical procedures were performed by experienced spine surgeons at a single institution.
Data collection
Prealbumin levels were obtained within 4 days of surgery for all patients; the median time between surgery and prealbumin assessment was 1 day, with an interquartile range of 1 day. Serum prealbumin levels were dichotomized into “low” and “normal” groups using a threshold value of 15 mg/dL based on previously published normal values.[1]
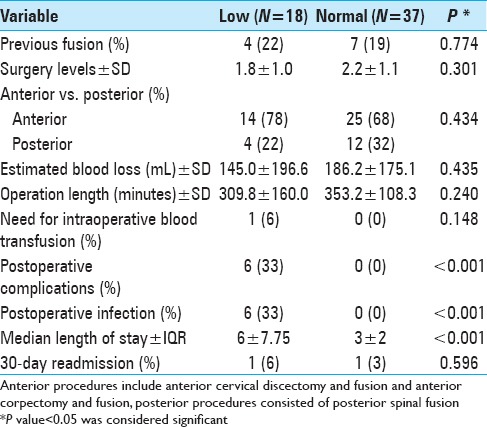
Fifty-five patients met the inclusion criteria for our study; 18 patients (33%) were in the “low prealbumin” category and 37 patients (67%) were in the “normal prealbumin” category. Demographic, clinical, intraoperative, and postoperative data were collected for all patients [Tables 1 and 2]. Postoperative complications evaluated for each patient were defined as follows; those requiring medical intervention (e.g., antibiotics for infection) and/or those requiring surgical/procedural intervention (e.g., feeding tube placement, return to surgery for wound debridement).
Table 1.
Univariate analysis for low versus normal prealbumin groups

Table 2.
Univariate analysis of surgical variables for low versus normal prealbumin groups
Statistical analysis
Continuous variables were analyzed utilizing the unpaired Student's t-test and the Mann–Whitney U test. Categorical variables were analyzed with Chi-square analysis. Univariate and multivariate analyses were performed. In all cases, P < 0.05 was considered statistically significant. All statistical analysis was performed using SPSS V20.0 (IBM Corporation, Armonk NY).
RESULTS
Patient population
In our univariate analysis, patients in the low prealbumin group had significantly longer hospital stays vs. the normal prealbumin group; the former had median LOS of 6 days (interquartile range of 7.75 days) and the latter had median LOS of 3 days (interquartile range of 2 days, U = 90.5, P < 0.001). The low prealbumin group also had more postoperative complications (33% vs. 0%, P < 0.001) and postoperative infections (33% vs. 0%, P < 0.001) [Tables 2 and 3].
Table 3.
Postoperative complications

Greater length of stay only statistically significant difference for patients with low prealbumin levels
There were no statistically significant differences in the two groups regarding demographic or preoperative variables. The surgical approaches, number of levels fused, number of prior cervical fusions, surgical times, blood loss, and transfusion requirements were not significantly different between the two groups. Although the LOS and complications reached statistical significance in this analysis, our low complication rate did not allow for robust multivariable modeling.
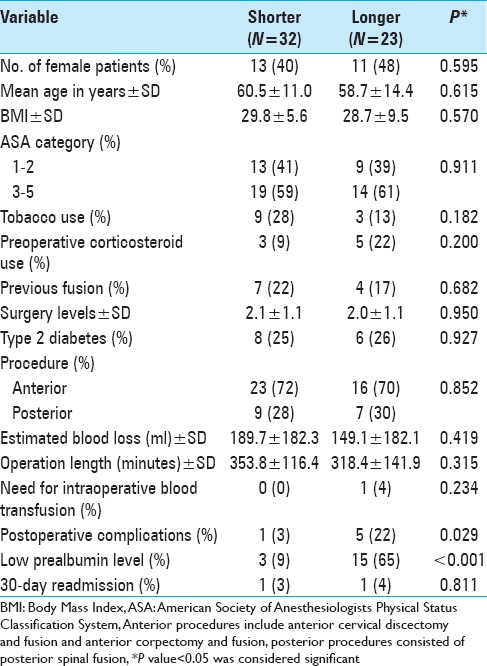
“Shorter” (32 patients) and “longer” (23 patients) LOS groups were based on the median LOS of 4 days [Table 4]. Although demographic and intraoperative factors were similar for the two groups, those with the longer LOS were more likely to have low prealbumin levels (65% vs. 9%, P < 0.001) and to experience more postoperative complication (22% vs. 3%, P = 0.029).
Table 4.
Univariate analysis for shorter versus longer length-of-stay groups
The increased number of postoperative complication resulted in increased hospitalization time/LOS.[3] Three factors—tobacco use, prealbumin levels (high/low), and surgical approaches—were included in the final model, but only the low prealbumin category remained significantly associated with prolonged hospitalization (with a standardized beta coefficient of -0.544 for patients in the high prealbumin group 95% CI − 8.311 to − 3.245, P < 0.001).
DISCUSSION
Our study demonstrated an association between low perioperative prealbumin level and prolonged hospitalization/increased LOS after surgery for cervical myelopathy. The LOS was previously shown to be significantly associated with greater complication rates and increased healthcare costs in patients undergoing spine surgery.[2] Furthermore, those with cervical myelopathy requiring operative intervention were substantially impacted by malnutrition.
In our univariate analysis, low prealbumin levels correlated with significantly higher rates of postoperative complications (e.g., half of all patients with prealbumin levels <15 mg/dL had one or more events vs. none in the normal group). Our complication rate was 6/55 (10.9%). This was comparable with those of previously published series,[5] however, the low absolute number of patients with adverse events prevented robust multivariable modeling.
Despite limitations associated with the retrospective nature of the study and the small patient cohort, this study preliminarily investigated the effect of low prealbumin levels on patients undergoing cervical surgery for myelopathy. In the future, spinal surgeons should consider nutritional/protein supplementation prior to and/or immediately after cervical spine and other spinal surgeries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Jian Guan, Email: jian.guan@hsc.utah.edu.
Christopher M. Holland, Email: Christopher.holland@cnsa.com.
Vijay M. Ravindra, Email: Vijay.ravindra@hsc.utah.edu.
Erica F. Bisson, Email: erica.bisson@hsc.utah.edu.
REFERENCES
- 1.Beck FK, Rosenthal TC. Prealbumin: A marker for nutritional evaluation. Am Fam Physician. 2002;65:1575–8. [PubMed] [Google Scholar]
- 2.Glennie RA, Ailon T, Yang K, Batke J, Fisher CG, Dvorak MF, et al. Incidence, impact, and risk factors of adverse events in thoracic and lumbar spine fractures: An ambispective cohort analysis of 390 patients. Spine J. 2015;15:629–37. doi: 10.1016/j.spinee.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Gruskay JA, Fu M, Bohl DD, Webb ML, Grauer JN. Factors affecting length of stay after elective posterior lumbar spine surgery: A multivariate analysis. Spine J. 2015;15:1188–95. doi: 10.1016/j.spinee.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Spiekerman AM. Nutritional assessment (protein nutriture) Anal Chem. 1995;67:429R–36R. doi: 10.1021/ac00108a026. [DOI] [PubMed] [Google Scholar]
- 5.Tetreault L, Tan G, Kopjar B, Cote P, Arnold P, Nugaeva N, et al. Clinical and surgical predictors of complications following surgery for the treatment of cervical spondylotic myelopathy: Results from the multicenter, prospective AOSpine International Study of 479 patients. Neurosurgery. 2016;79:33–44. doi: 10.1227/NEU.0000000000001151. [DOI] [PubMed] [Google Scholar]


