Abstract
A 43-day-old boy presented with bacteremia after umbilical artery catheterization. Duplex ultrasound examination revealed a 1.1- × 1.6-cm mycotic infrarenal aortic aneurysm and an incidental asymptomatic occluded right common iliac artery. Resection and repair were completed by creating an everted, double-layered internal jugular vein patch. Screening ultrasound examination 10 months postoperatively demonstrated successful repair.
The most common cause of abdominal aortic aneurysm (AAA) in pediatric patients is infection, often in the context of umbilical artery catheterization (UAC).1 We present a case of autologous repair of a mycotic AAA secondary to UAC in a neonate. Consent was obtained from the parents for publication, and Institutional Review Board approval was obtained.
Case report
A 36-week boy was born to a 24-year-old woman. Early life was complicated by hypoglycemia, hyperbilirubinemia, leukopenia, and thrombocytopenia. The patient required UAC for 5 days. By day 10, right knee swelling consistent with a septic knee joint developed. During workup for sepsis, abdominal ultrasound (US) examination revealed nonocclusive thrombus in the infrarenal aorta at the level of the inferior mesenteric artery. Occlusive thrombus was seen in the right common iliac artery. There were no ischemic findings in the right lower extremity, and this was managed by the neonatology and hematology teams without surgical consultation with therapeutic heparin anticoagulation, later switched to enoxaparin, with a planned course of 6 months of anticoagulation. The remaining workup revealed methicillin-sensitive bacteremia, right femur osteomyelitis, and tricuspid valve vegetation. One month later, a surveillance US scan revealed resolution of the thrombus but now a 1.5- × 1-cm AAA at the aortic bifurcation (Fig 1). The healthy portion of the aorta just proximal to the aneurysm measured 3 mm. The vascular surgery service was consulted, and computed tomography angiography (CTA) revealed an AAA extending onto the right common iliac (Fig 2). The patient had palpable pulses bilaterally, including pedal pulses, probably as a result of the formation of collateral circulation. The patient remained bacteremic, and there was concern that the aneurysm was mycotic. The decision was made that he would benefit from the use of autogenous tissue for repair.
Fig 1.
Sagittal view of the aorta and abdominal aortic aneurysm (AAA) at diagnosis.
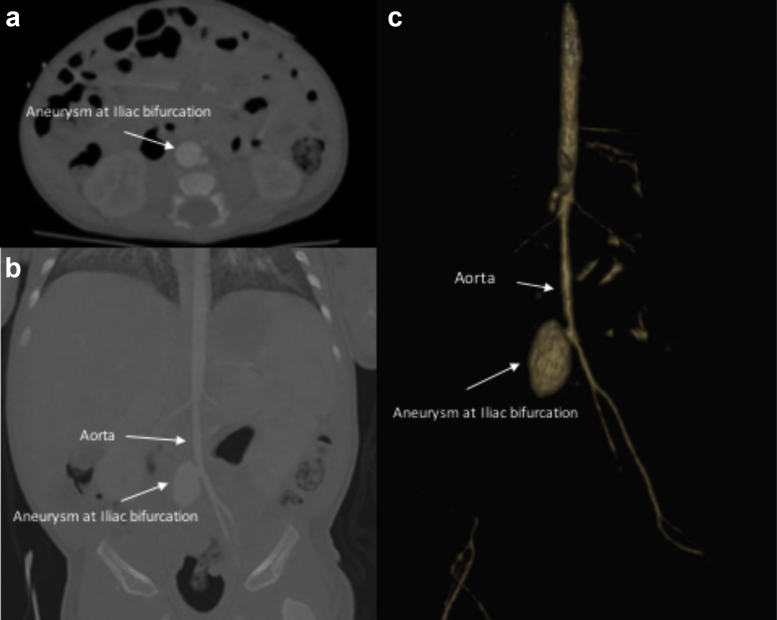
Fig 2.
a, Axial computed tomography angiography (CTA) revealing abdominal aortic aneurysm (AAA). b, Coronal CTA revealing AAA. c, Three-dimensional reconstruction of AAA.
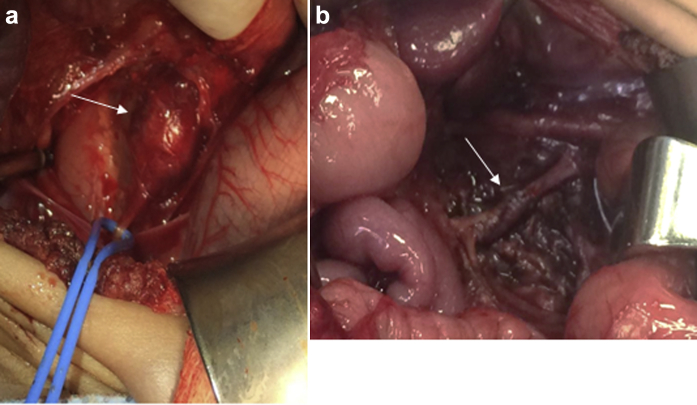
Surgery was performed through an infraumbilical transverse incision. The AAA was at the right common iliac artery-aorta bifurcation (Fig 3). Proximal and distal control were obtained, and the aneurysm was completely resected to normal aorta. The occluded right iliac artery was adherent to the aneurysm, and the decision was made to ligate it as it was thrombosed. The defect was too large for primary repair, so the right internal jugular (IJ) vein was used for patch angioplasty. Harvest of the IJ vein was performed by a pediatric surgeon through a supraclavicular incision. Electrocautery was used to dissect through subcutaneous tissue until the IJ vein was identified. After it was dissected free from surrounding tissue, a 3-cm section of the IJ vein was dissected out between Prolene ties. The vein was then used as a double-sided everted patch so the intima would face the lumen and exterior. This provides a double-layered patch, which was thought to provide additional strength for the patch repair. Femoral artery signals were present immediately after repair; at the first postoperative check, these were palpable with triphasic Doppler signals in both feet. Enoxaparin was restarted on postoperative day (POD) 1. On POD 7, US examination revealed a saccular pseudoaneurysm of the infrarenal aorta at the site of repair. He was taken back to the operating room, and the abdomen was entered through the prior incision. The cause of the pseudoaneurysm was twofold: there was a bleeding vessel coming off the anterior portion of the aorta-common iliac artery bifurcation, and a small part of the superior aspect of the suture line of the patch was leaking. One additional suture was placed at the site of the leak with suture ligation of the anterior bleeding vessel. There was no evidence of infection. Surveillance US on POD 7/14 revealed a normal distal aorta without evidence of aneurysm. Surveillance CTA on POD 20 again revealed no aneurysm. CTA as opposed to US was used for surveillance because the child was additionally being investigated for splenic disease. The patient was prescribed 12 weeks of doxycycline, given the extent of systemic infection. Cultures of the excised aneurysm sac were negative. He completed a 6-month course of enoxaparin per recommendations of the hematologist, and screening US 10 months postoperatively demonstrated successful repair. He will continue to have an annual screening aortic US examination.
Fig 3.
a, Abdominal aortic aneurysm (AAA; arrow pointing to aneurysm, blue vessel loop surrounding right iliac artery). b, Aorta after repair (arrow pointing to jugular vein patch repair of aortic aneurysm).
Discussion
UAC is an option for reliable arterial access in neonates younger than 10 days who need frequent blood pressure monitoring or frequent arterial blood gas samples. An incision is made at the inferior aspect of the umbilical stump, which typically allows identification of one of the two ventral umbilical arteries. The artery can be cannulated with a 3.5F or 5F catheter. Clinically significant aortic thrombus after UAC is 3% to 6% more common in patients with a catheter that extends to L4 or lower. Sepsis results from 2% to 5% of UACs.2 Repair of pediatric mycotic aneurysms after UAC has variable results. Twenty-five years ago, a case series described five infants with methicillin-resistant Staphylococcus aureus mycotic AAAs. Three infants died of sepsis before repair; one infant underwent successful interposition graft but died 6 months later. The fifth infant underwent resection of the aneurysm with primary end-to-end anastomosis and was still alive at the time the case series was published.3 All of the infants in the case series underwent UAC. In another case report, a neonate suffered methicillin-resistant S. aureus bacteremia after UAC and later developed aneurysms of the right innominate artery, the infrarenal aorta, and the left common iliac artery. The infrarenal aneurysm resolved, but the iliac artery aneurysm continued to grow and was resected and repaired with cadaveric vein graft. Nine months postoperatively, the graft remained patent.4 In a final case report, one infant developed an infrarenal AAA and had her aneurysm resected and repaired with cryopreserved vein graft. Repair was patent at 1 year of follow-up.5 Our patient had negative tissue cultures; however, the aneurysm had a gross appearance of infection and may have been sterilized from intravenous antibiotics.
This review highlights the fact that there is no standard operative technique for pediatric aneurysm repair. The decision was made that this child would benefit from an open operation; he had osteomyelitis and persistent bacteremia in the presence of a presumed mycotic aneurysm. Given the presumptive infected field, we opted not to use a prosthetic conduit. The great saphenous vein of a 49-day old infant would be too small. However, the IJ vein of an infant is large enough to serve as an appropriate conduit or patch. There are examples in the literature of everted vein grafts used to increase the strength of carotid artery autologous vein patches.6, 7 Everting the IJ vein and using it as a double-layered patch increase the strength, and the intima on the luminal surface minimizes thrombosis.
We acknowledge that this repair was challenging and not without flaw. Richardson et al8 described a case series of infants diagnosed with aortoiliac thromboses after UAC. In this series, all infants were treated with local infusion of intra-arterial streptokinase for 36 hours to dissolve the clot. Given the bacteremia and aneurysm, we opted for anticoagulation alone and not thrombolysis. We propose that pediatric mycotic AAAs can be safely resected and repaired using everted IJ vein grafts. An annual surveillance US scan will be obtained as there are no published long-term outcome data on repair of neonatal AAAs.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Nathan J.D. Abdominal aortic pathology. In: Ziegler M.M., Azizkhan R.G., Allmen D., Weber T.R., editors. Operative pediatric surgery. 2nd ed. McGraw-Hill Education; New York: 2014. [Google Scholar]
- 2.Hirschl R.B., Moulton S.L., Mulligan J., Convertino V.A., Reiter P.D., Moulton S.L. Pediatric surgical critical care: cardiopulmonary monitoring, advanced hemodynamic monitoring, acute cardiopulmonary resuscitation, pharmacology, respiratory failure, and ECMO*. In: Ziegler M.M., Azizkhan R.G., Allmen D., Weber T.R., editors. Operative pediatric surgery. 2nd ed. McGraw-Hill Education; New York: 2014. [Google Scholar]
- 3.Lobe T.E., Richardson C.J., Boulden T.F., Swischuk L.E., Hayden C.K., Oldham K.T. Mycotic thromboaneurysmal disease of the abdominal aorta in preterm infants: its natural history and its management. J Pediatr Surg. 1992;27:1054–1059. doi: 10.1016/0022-3468(92)90559-p. [DOI] [PubMed] [Google Scholar]
- 4.Monahan D.A., Neville H.L., Saigal G.M., Perez E.A., Sola J.E. Infected common iliac artery aneurysm repaired in an infant with cadaveric vein graft. J Pediatr Surg. 2012;47:606–608. doi: 10.1016/j.jpedsurg.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Benrashid E., McCoy C.C., Rice H.E., Shortell C.K., Cox M.W. Mycotic saccular abdominal aortic aneurysm in an infant after cardiac catheterization: a case report. Ann Vasc Surg. 2015;29:1447.e5–1447.e11. doi: 10.1016/j.avsg.2015.06.061. [DOI] [PubMed] [Google Scholar]
- 6.Abeysekara A.M., Siriwardana H.P., Prabaharan B., Tiwari A., Madipolagedara N., Jacob S. Common facial vein: an alternative patch material in carotid angioplasty. ANZ J Surg. 2008;78:185–188. doi: 10.1111/j.1445-2197.2007.04399.x. [DOI] [PubMed] [Google Scholar]
- 7.Danikas D., Schmeler K.M., Ginalis E.M., Stratoulias C., Shorten S.M., Constantinopoulos G. Double-layer everted saphenous vein patch angioplasty for carotid endarterectomy. Vasc Endovascular Surg. 2001;35:259–261. doi: 10.1177/153857440103500404. [DOI] [PubMed] [Google Scholar]
- 8.Richardson R., Applebaum H., Touran T., Franceschini R.E., Robbie P.A., Wirtschafter D.D. Effective thrombolytic therapy of aortic thrombosis in the small premature infant. J Pediatr Surg. 1988;23:1198–1200. doi: 10.1016/s0022-3468(88)80343-9. [DOI] [PubMed] [Google Scholar]