Abstract
Background
Social influences on tobacco use have been reported but not well quantified.
Objectives
We aimed to detect and quantify social influences on tobacco use by gender and form of tobacco use.
Materials and Methods
The International Tobacco Control Project (TCP), India surveyed individuals ≥15 years in four areas of India about their tobacco use and that of their close associates, using stratified multistage cluster sampling. Odds ratios for tobacco use for each type of close associate were calculated using logistic regression.
Results
Among the 9,780 respondents, tobacco use was significantly associated with its use in the same form by close associates. Women smokers were 9 times likelier to have a mother who ever smoked. Men smokers were 5 times likelier to have a mother who ever smoked and 7 times likelier to have close friends who smoked. Both men and women SLT users were 5 times likelier to have friends who used SLT and 4 times likelier to have a spouse who used SLT.
Conclusions
Social influence on tobacco use in families, communities, workplaces, etc., needs to be addressed in India while working to control tobacco use.
Keywords: Tobacco Use, Smoking, Tobacco, smokeless, Social environment
INTRODUCTION
Knowing the social context of tobacco use is important for interventions promoting its cessation.1,2 Community surveys and interventions in India have shown that tobacco use is often learned from parents, other elders, and peers.3,4 Studies at workplaces and in educational institutions have reported similar findings.5–8 The rationale for this study was that the pattern of influence of close social contacts using tobacco has not yet been well quantified or studied by gender in India and that this information might be useful when designing effective interventions. It was expected that the pattern of social influence on women’s tobacco use, which is mainly smokeless tobacco,9 would differ from that for men. The purpose of this study was to quantify the associations of tobacco use with its use by close social contacts, gender-wise, in a large general population across different states. Since tobacco use is implicated in cancer, cardiovascular disease, stroke and chronic lung diseases, higher mortality and adverse reproductive effects, it is important to understand in detail the transmission of this disease causing factor.10
MATERIAL AND METHODS
The International Tobacco Control Policy Evaluation Project (the ITC Project), which in India is called the Tobacco Control Project (TCP), to avoid associations with the India Tobacco Company, conducted its baseline survey between August 2010 and December 2011. This provided an opportunity to study how strongly tobacco use (in smoked and smokeless forms) and specific product choices may be influenced by other users in the close social context. All study materials and procedures used in the TCP India Survey were reviewed and cleared for ethics by the Office of Research Ethics at the University of Waterloo, Canada and by the Institutional Review Board at the Healis-Sekhsaria Institute for Public Health, Navi Mumbai, India.
Sampling method and data collection
A stratified, multistage cluster sampling design was used to collect samples of adults (defined as persons aged 15 years and older), tobacco users and non-users, in four major cities of four states (Mumbai, Maharashtra; Indore, Madhya Pradesh; Patna, Bihar; Kolkata, West Bengal), and near-by rural areas (within 50 km from city centers).11 The sampling procedure aimed at recruiting at least 2,000 adult tobacco users and 600 non-users in each state. Eligible persons included those living in private homes and belonging to one of four categories: smokers, smokeless tobacco users and non-users; for the present study, users of both smoked and smokeless forms of tobacco were excluded. Up to 4 tobacco-using household members were interviewed and if there were more in a household, 4 were selected with the role of a die. One adult non-user was selected from every third household enumerated.12 In each city, 10 wards were selected with probability proportional to their size. From each ward, 10 census enumeration blocks were selected to provide a total of 150 households. In each chosen rural district, two or three sub-districts were identified, from which four villages, each with at least 1,000 households were selected. In each village, 125 households were enumerated. In all, from the selected areas, 9,699 households were enumerated for data collection. Up to four individuals in the household who were tobacco users were selected for interview and up to one non-user from every third enumerated household was randomly selected.11 Structured questionnaires were used to collect information in face-to face interviews with each respondent in Hindi, Marathi, Bengali, or English by trained interviewers after an information letter was provided and consent obtained.
Definitions
Current use of any tobacco by respondents was defined as use at least once in the past 30 days by self-report. Tobacco users were categorized according to the form of tobacco they used: smoked, smokeless or mixed use (smoked and smokeless). For this study, all 805 mixed users in the original sample11 were excluded in order to study the relationship between respondent’s smoking or SLT use with similar tobacco use by close associates. The concept ‘close associate’ in this paper includes father, mother, spouse, and the five closest friends. Respondents were asked about current smoking and smokeless tobacco (SLT) use by their spouse (if married) and five closest friends, as well as about ‘ever’ smoking and ‘ever’ use of SLT by each parent (a parent could have died or quit tobacco before the survey).
Products
Smoked tobacco products comprised cigarettes, bidis (tobacco flakes wrapped in a tendu or temburni leaf), pipes, including the hookah (water pipe), other pipes (including the hookli and others), chuttas, cigars, and other products.13,14 SLT products included: 1) those for chewing or holding in the mouth, e.g., plain chewing tobacco, generally sold loose; zarda, which is scented, branded chewing tobacco; khaini, consisting of finely cut tobacco mixed with slaked lime, either by the user or in packaged form, which is placed between the lips and gums; 2) areca nut and tobacco mixtures for chewing: gutka, of which there are many brands sold all over India and contains crushed areca nut with tobacco and slaked lime; betel quid, which is areca nut, tobacco, slaked lime and condiments, wrapped in a fresh betel leaf, prepared by vendors or at home; 3) products commonly used for application to teeth and gums and as dentifrice, such as dry snuff (also called tapkir), gudhaku (a paste of tobacco and unrefined sugar, mainly used in West Bengal and Bihar), pyrolized products (gul and mishri, the latter mostly used in Maharashtra), and lal dantmanjan (red toothpowder). Laldantmanjan, of which there are several brands, although not claiming to contain tobacco, nor legally permitted to, has been found to contain nicotine in some analyses.15–17
Data analysis
Binary logistic regression was used to calculate separate odds ratios (ORs) for 1) current exclusive smoking and 2) current exclusive SLT use and its use by close associates, using Statistical Package for Social Studies (SPSS) Licensed Version 20 ®. All ORs were adjusted for age (in 10 year groups), residence (urban or rural), state and three levels of monthly household income (Low = < Rs. 5,000; Moderate = Rs. 5,001–15,000; High = ≥ Rs. 15,001). These variables were used for adjustment because tobacco use prevalence has been found to vary by socio-economic characteristics and state of residence, to be higher in older age groups and persons living in rural areas.9 ORs for smoking and for SLT use were also separately calculated for the number of closest friends who used tobacco of the same type (smoked or smokeless). ORs were also calculated for any one, any two, any three and any four types of close associates who also smoked or used SLT. The chi square test for linear trend was performed using Epi Info. Sampling weights were applied to the data for all logistic regression calculations to ensure better representativeness of the data.
RESULTS
The sample consisted of 9,780 respondents aged 15 and above (56.6% male or 5,536), whose demographics are shown in Table 1. Most were married (71.7%) and urban (73.0%). Some 1,255 were exclusive smokers (97% men), while 5,991 exclusively used SLT and 2534 were non-users. Tobacco users were more concentrated in higher age groups compared to non-users. Smokers had a higher proportion of married respondents, tended to be older and a higher proportion of smokers were rural compared to SLT users and non-users. West Bengal had the highest proportion of smokers; Maharashtra and Bihar had higher proportions of SLT users compared to the other states.
Table 1.
Sample characteristics by tobacco use status in TCP India Wave 1 Survey in 2010–11 [N=9,780 (4,244 women; 5,536 men)].
| Category | Non-tobacco Users | Smoked Tobacco Users | Smokeless Tobacco (SLT) Users | ||||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | ||
| Totals | All | 2534 | (100) | 1255 | (100) | 5991 | (100) |
| Sex | Men | 879 | (34.7) | 1218 | (97.0) | 3439 | (57.4) |
| Women | 1655 | (65.3) | 37 | (3.0) | 2552 | (42.6) | |
| Age Group (years) | 15–24 | 740 | (21.3) | 104 | (8.3) | 883 | (14.7) |
| 25–39 | 947 | (37.4) | 379 | (30.2) | 1996 | (33.3) | |
| 40–54 | 523 | (20.6) | 442 | (35.2) | 1703 | (28.4) | |
| 55+ | 324 | (12.8) | 330 | (26.3) | 1409 | (23.5) | |
| Residence | Urban | 1890 | (74.6) | 852 | (67.9) | 4398 | (73.4) |
| Rural | 644 | (25.4) | 403 | (32.1) | 1593 | (26.6) | |
| State | Bihar | 600 | (23.7) | 117 | (9.3) | 1696 | (28.3) |
| West Bengal | 625 | (24.7) | 631 | (50.3) | 1077 | (18.0) | |
| Madhya Pradesh | 621 | (24.5) | 327 | (26.1) | 1459 | (24.4) | |
| Maharashtra | 688 | (27.2) | 180 | (14.3) | 1759 | (29.4) | |
| HH Income | Low | 591 | (24.2) | 398 | (32.5) | 1570 | (27.0) |
| Medium | 1376 | (56.4) | 621 | (50.7) | 3482 | (59.8) | |
| High | 474 | (19.4) | 205 | (16.7) | 773 | (13.3) | |
| Marital Status | Married | 1671 | (65.9) | 1023 | (81.5) | 4321 | (72.2) |
| Single | 715 | (28.2) | 181 | (14.4) | 923 | (15.4) | |
| Other | 148 | (5.9) | 51 | (4.1) | 739 | (12.4) | |
Note: Unweighted data.
Smoking by a spouse was apparently less common among smokers (0.8%) than among SLT users (17.2%) and non-users (23.4%), however, high proportions of married respondents were either unaware or unwilling to say whether their spouse smoked (16.9% of men smokers and 11.7% of male non-users; 66.6% of women smokers and 34.6% of female non-users). A substantial portion of women also did not answer about their husband’s use of SLT (13.7% of women SLT users and 16.2% of female non-users), but only about 2% of men did not answer about their wife’s use of SLT. Lack of knowledge or reluctance to answer questions about parental or friend’s tobacco use in any form varied only from zero to 4.1%.
Smokers had the highest proportion of fathers who ever smoked (63.9%), while SLT users had the highest proportions of fathers (51.1%) or mothers (37.9%) who ever used SLT. Smokers were most likely to say they had any close friend who smoked (86.1%) while SLT users were most likely to have any close friend who used SLT (76.5%) (not shown in the tables). In view of this pattern, further analysis concentrated on the associations between users of the same form of tobacco.
Among the 1,218 men who smoked, about two fifths smoked only cigarettes (40.6%), about one third smoked only bidis (34.3%) and about one fourth smoked both cigarettes and bidis (22.5%). The remaining men smoked other products, such as the hookah, other pipes, chuttas, cigars, etc., mostly in combinations. Of the 37 women who smoked, nearly half smoked exclusively bidis (48.6%) and over a third smoked only the hookah (37.8%).
Exclusive SLT users included 3439 men and 2552 women. The largest group of SLT using men used combinations (29.9%), followed by exclusive use of gutka (21.1%), khaini (17.8%) or plain chewing tobacco (17.2%). Among women SLT users, about one sixth used combinations (17.9%) and all others used a single product exclusively, most commonly lal dantmanjan (25.4%), followed by mishri (16.1%), plain chewing tobacco (8.0%%), and gutka (6.3%).
Tables 2 and 3 show that almost all of the odds ratios (ORs) for tobacco users having close associates who used tobacco in the same form were elevated and most were highly significant, showing strong associations. In Table 2, the ORs for association with smoking by either parent were especially strong for women smokers (7-and 9-fold for father and mother smoking respectively), while for men having close friends who smoked was strongest (7-fold). Product-wise, for men, the highest associations with close associates were for the combination of cigarettes and bidis, while for women, for exclusive bidi smoking. ORs for spouse smoking could not be calculated.
Table 2.
Odds ratios of association between tobacco use (exclusive smoking) by respondent and use by close associates, among men and women in the TCP India Wave 1 Survey.
| SMOKING | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| USER CATEGORY | Sex | Father Ever Smoked | Mother Ever Smoked | Close Friend Smokes | Spouse Smokes | ||||
| OR (Adj)* 95% CI | OR (Adj)*95% CI | OR (Adj)* 95% CI | OR (Adj)* 95% CI | ||||||
| Smoking (Exclusive) | Men | 2.4 | 2.0–3.0 | 5.4 | 2.1–14.1 | 7.2 | 5.6–9.3 | –† | – |
| Women | 7.3 | 3.1–17.5 | 9.0 | 3.3–24.7 | 3.5 | 1.5–7.9 | –† | – | |
| Cigarettes | Men | 2.2 | 1.7–2.9 | 5.3 | 2.0–14.4 | 7.1 | 5.2–9.7 | –† | – |
| Bidis | Men | 2.6 | 1.9–3.6 | 15.1 | 3.3–69.2 | 5.7 | 3.8–8.5 | –† | – |
| Women | 7.9 | 2.4–26.1 | 14.9 | 4.3–51.3 | 4.7 | 1.6–13.3 | –† | – | |
| Cigarettes & Bidis | Men | 4.0 | 2.8–5.7 | 4.0 | 0.7–22.2 | 9.5 | 5.6–15.9 | –† | – |
| Other smoking | Men‡ | 2.6 | 1.1–5.9 | –† | – | –† | – | –† | – |
| Women§ | 8.6 | 2.2–33.9 | 6.7 | 1.0–47.2 | –† | – | –† | – | |
Adjusted for age group (with first two groups combined as reference category [ref. cat.]=first), urban/rural residence (urban as ref. cat.), state (Maharashtra as ref. cat.), and income level (with highest category as ref. cat.). CI=Confidence interval.
For cells with frequency < 5 cases ORs were not calculated.
For men, “Other smoking” includes other products used exclusively and smoking combinations.
For women, “Other smoking” is only exclusive hookah smoking as there were no other categories.
Notes: Weighted data used. Lal dantmanjan may not necessarily contain tobacco.
Table 3.
Odds ratios of association between tobacco use (smokeless tobacco [SLT] use) by respondent and use by close associates, among men and women in the TCP India Wave 1 Survey.
| SLT USE | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| USER CATEGORY | Sex | Father Ever Used SLT | Mother Ever Used SLT | Close Friend Uses SLT | Spouse Uses SLT | ||||
| OR (Adj)* 95% CI | OR (Adj)* 95% CI | OR (Adj)* 95% CI | OR (Adj)* 95% CI | ||||||
| SLT use (Exclusive) | Men | 2.3 | 1.9–2.7 | 2.1 | 1.7–2.5 | 5.3 | 4.4–6.3 | 4.1 | 3.0–5.8 |
| Women | 2.1 | 1.8–2.4 | 4.0 | 3.3–4.7 | 5.0 | 4.3–5.9 | 4.3 | 3.6–5.3 | |
| Gutka | Men | 1.8 | 1.4–2.2 | 1.9 | 1.5–2.4 | 5.7 | 4.3–7.5 | 2.2 | 1.4–3.4 |
| Women | 2.4 | 1.6–3.4 | 4.2 | 2.8–6.1 | 10.3 | 6.4–16.5 | 7.8 | 4.5–13.7 | |
| Khaini | Men | 2.7 | 2.1–3.6 | 2.2 | 1.6–3.1 | 7.7 | 5.4–11.1 | 5.1 | 3.1–8.5 |
| Women | 2.8 | 1.2–6.3 | 2.7 | 1.2–6.2 | 9.0 | 3.3–25.0 | 6.5 | 1.3–31.5 | |
| Plain Chewing Tobacco | Men | 1.7 | 1.3–2.3 | 1.4 | 1.0–1.8 | 3.4 | 2.6–4.6 | 2.3 | 1.4–3.6 |
| Women | 1.6 | 1.0–2.3 | 3.2 | 2.1–4.8 | 6.7 | 4.3–10.3 | 7.5 | 4.1–13.3 | |
| Zarda | Men | 2.3 | 1.5–3.4 | 2.5 | 1.6–3.8 | 11.3 | 5.9–21.6 | 7.1 | 3.7–13.7 |
| Women | 1.6 | 1.0–2.7 | 4.5 | 2.7–7.4 | 6.3 | 3.7–10.6 | 4.3 | 2.3–8.0 | |
| Betel Quid with Tobacco | Men | 2.3 | 1.4–3.7 | 1.8 | 1.0–3.0 | 2.8 | 1.7–4.6 | 2.2 | 1.2–4.3 |
| Women | 1.5 | 0.9–2.4 | 3.3 | 2.1–5.2 | 4.9 | 3.1–7.8 | 2.4 | 1.3–4.3 | |
| Lal Dantmanjan | Men | 2.4 | 1.4–4.2 | 9.7 | 5.3–17.8 | 4.4 | 2.2–9.0 | 18.2 | 7.3–45.6 |
| Women | 1.5 | 1.1–2.0 | 2.5 | 1.8–3.6 | 3.8 | 2.8–5.1 | 2.7 | 1.9–3.9 | |
| Mishri | Men | 1.7 | 0.8–3.6 | 1.6 | 0.8–3.3 | 1.1 | 0.5–2.3 | 18.2 | 6.7–49.4 |
| Women | 2.0 | 1.4–2.8 | 2.7 | 2.0–3.8 | 3.8 | 2.6–5.4 | 5.3 | 3.6–7.9 | |
| Gul | Men | 2.9 | 1.2–6.8 | 1.7 | 0.6–4.6 | 2.9 | 1.1–7.6 | 6.9 | 1.9–25.1 |
| Women | 3.3 | 2.1–5.2 | 3.3 | 2.0–5.5 | 4.0 | 2.5–6.5 | 3.3 | 1.8–6.0 | |
| Snuff | Men | 1.9 | 0.8–4.7 | 1.7 | 0.7–4.1 | 1.2 | 0.5–2.9 | 6.5 | 2.1–20.1 |
| Women | 2.9 | 1.8–4.8 | 4.3 | 2.6–7.1 | 2.8 | 1.7–4.7 | 10.8 | 4.8–24.3 | |
| Gudhaku | Men | 5.2 | 1.8–15.5 | 4.7 | 1.8–13.0 | 3.1 | 1.1–9.0 | 17.6 | 3.8–81.5 |
| Women | 2.4 | 1.5–3.8 | 5.4 | 3.5–8.5 | 5.9 | 3.8–9.2 | 4.8 | 2.7–8.7 | |
| Other SLT Use | Men | 4.1 | 1.6–10.0 | 3.5 | 1.4–8.9 | 5.1 | 1.5–17.1 | 17.0 | 4.2–68.3 |
| Women | 2.4 | 1.2–5.0 | 4.3 | 2.0–8.9 | 2.5 | 1.2–5.3 | 6.7 | 1.5–28.8 | |
| SLT Combinations | Men | 3.0 | 2.5–3.7 | 2.3 | 1.8–2.9 | 5.3 | 4.2–6.8 | 5.6 | 3.9–8.1 |
| Women | 2.2 | 1.7–2.8 | 5.3 | 4.0–6.9 | 5.3 | 4.1–7.0 | 4.5 | 3.2–6.4 | |
Adjusted for age group (with first two groups combined as reference category [ref. cat.]=first), urban/rural residence (urban as ref. cat.), state (Maharashtra as ref. cat.), and income level (with highest category as ref. cat.). CI= confidence interval. SLT=smokeless tobacco.
For cells with frequency < 5 cases ORs were not calculated.
Notes: Weighted data used. Lal dantmanjan may not necessarily contain tobacco.
The influence of SLT use by parents appeared strong for both men and women (Table 3), significantly more so for mothers on daughters (OR=4.0), than for mothers on sons (OR=2.1). For women, for father ever use of SLT, ORs for use of khaini, gul and snuff were highest and close to 3; for mother ever SLT use, ORs ranged from 2.5 to 5.4 for all SLT products. For men, ORs for use of specific SLT products for father’s ever SLT use were highest for gudhaku, gul, and “other SLT”, but ORs for mother’s ever SLT use were higher for lal dantmanjan and gudhaku.
The association of SLT use with having any close friends who also used SLT was five-fold higher compared to non-tobacco users, for both men and women. For men who used zarda, khaini, gutka or plain chewing tobacco, the odds ratios for close friends’ SLT use were significantly higher than those for father’s or mother’s SLT use (no overlap of confidence intervals=CI). For women, the same was true only for gutka. The highest odds ratio for betel quid use was for women whose close friends used smokeless tobacco.
ORs for SLT users whose spouse used SLT were generally intermediate between ORs for parents and friends using SLT. Women’s use of SLT was strongly associated with SLT use by the spouse, especially gutka, khaini, plain chewing tobacco, zarda, snuff and mishri. For men, lal dantmanjan use was highly associated with spouse (wife’s) SLT use as well as mother’s SLT use. ORs for use of products applied to teeth and gums and used as dentifrice were elevated for all close associates using SLT, but tended to be highest for spouse SLT use, for both men and women.
Figure 1 shows that the ORs for the number of five closest friends using the same form of tobacco as the respondents tended to go up with increasing numbers of friends using tobacco in the same form, for both men and women (even though for women who smoked, being few in number, the first three elevated ORs did not reach significance). Chi squares for linear trend for all four sets of values were highly significant (p<0.0001).
Figure 1.
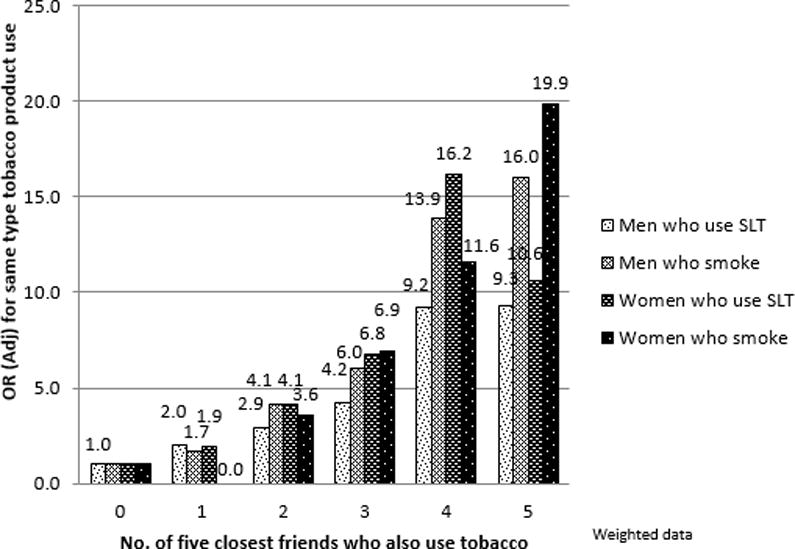
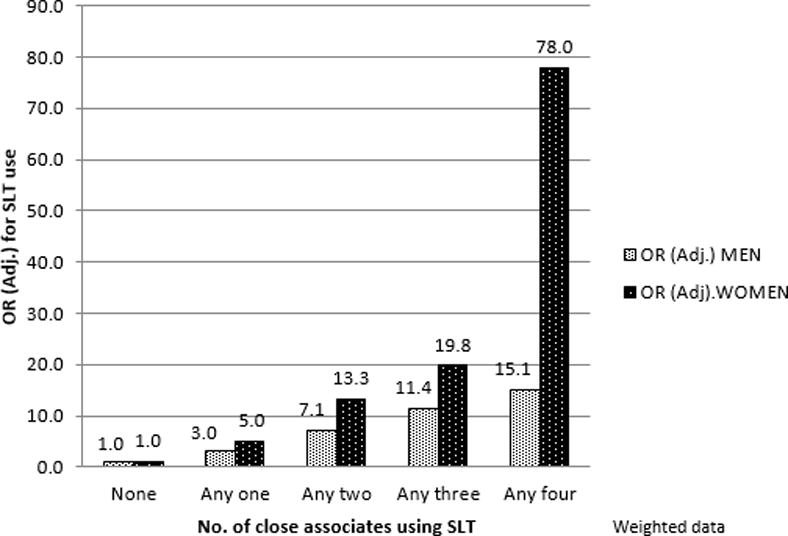
Figure 2 shows that the ORs for SLT use rose with increasing numbers of associates who used SLT (any one, any two, any three, or all four among father, mother, close friends, and spouse) in a highly significant manner (p<0.0001). ORs for smoking for any close associates who smoked increased only up to two close associates because few women smoked and so is not shown.
Figure 2.
DISCUSSION
This study shows that use of tobacco by close social contacts is very likely to influence or reinforce tobacco use among adults in India. Friends appear to strongly influence both men and women to use SLT. Friends appear to strongly influence men more than parents for smoking, while the reverse is true for women. The influence of mothers on daughters to use tobacco appears especially strong. Among married SLT users, the spouse is also likely to be a user and in particular wives seem to influence their husbands to use tobacco based dentifrices. Individuals are increasingly likely to use tobacco in any form as more of their close social contacts use it. The implications of this survey, conducted in both urban and rural areas of four states may well be generalizable to the whole of India.
Considering that our sampling criteria (persons aged 15 and above) included a large part of the adolescent age group, it seems relevant that a previous study of adolescents in Noida city, Uttar Pradesh found a similar order of association: among 4,786 students aged 11–19 years in classes VII to XII, tobacco users were more than 8 times more likely to have friends or classmates who also use tobacco (OR=8.6 (CI 6.3–12.0), seven times more likely if their mother used it (OR=7.2 [CI 4.2–12.1]) and three times more likely to have a father who used it (OR=3.0[CI 2.2–4.1]).7
Four earlier studies from India quantified associations of tobacco use by individuals with that by friends or peers. In a study among 1,587 male students (aged 16–23 years) at eleven colleges in southern Karnataka, smokers were 5 times more likely to have friends who smoked compared to nonsmokers.8 A community study among 500 youth 15–24 years old in urban and rural Chandigarh found that youth were much more likely to smoke if their friends smoked (OR=40 (95% CI: 11.4- 142.8).4 In a study of smokeless tobacco use among 336 office workers in Mumbai, 61% lower level workers and 83% of male clerks reported peer pressure to be an influence on their use of SLT, especially gutka.9 In a small intervention study of 104 factory workers in Ratnagiri district of Maharashtra, peer influence for tobacco use on and off the job was found to be important (but not quantified), mainly for SLT in that population.6
Studies available from other countries also report social influence on tobacco use by friends and/or parents.18–21 For example, in a study in Italy on 7,469 persons 15 years old and above, 61% reported smoking due to the influence of friends; men were more likely to report the influence of friends, but women more frequently reported the influence of parents or partner.19
The present study shows that mothers’ influence in India is especially strong on women’s smoking. Although not studied previously in India, a similar phenomenon has been reported in a 20-year literature review of 51 studies published during 1989–2009 on mothers’ smoking and adolescent smoking included studies from North America, Europe, Oceanea and Asia. Forty-three studies (86%) found a positive association between the mother’s smoking and that of the adolexcent offspring; among these, 21 found the mother’s tobacco smoking more strongly associated with girls’ own smoking than that of boys.22
The phenomenon of parental and peer influence on smoking has sometimes been explained with the help of social learning theory, according to which individuals imitate behaviours modelled by individuals with whom they identify closely, such as parents, elder siblings and peers/friends.23,24 While initiation to tobacco use may occur in adolescence or earlier, and may be partly influenced by parents and friends, role modelling by significant others may remain important for continuation of tobacco use into adulthood, aided by addiction to nicotine.
Our study also showed that SLT use is highly associated with the spouse’s use of SLT, and these associations were intermediate in value between those for parents and close friends. In particular, use of SLT products as a dentifrice by men appears strongly associated with their use by the wife.
The significance of having friends who smoke may extend to quitting intention and behaviour. A qualitative study among 60 disadvantaged women smokeless tobacco users in Delhi, participants expressed that seeing others around them chewing tobacco would pose a challenge to quitting.25 On the other hand, the ITC Four Country Survey found that smokers who lost touch with smoking friends between two waves of the survey were significantly more likely to have attempted to quit (OR= 1.5; p< 0.0001) and to have quit successfully (OR= 1.6; p< 0.01) than those who did not lose any smoking friends during the period.26
One limitation of our study was that substantial proportions of married respondents did not want to disclose the use of tobacco by the spouse. Due to this, results on smoking in association with spouse smoking could not be calculated. Also, since many women were unaware or were unwilling to discuss their husband’s use of SLT, results on husband’s use of SLT might be somewhat biased. Investigation of the reasons for non disclosures on spousal tobacco use could shed light on underlying views on the acceptability tobacco use. A second limitation was that specific products used by close associates were not recorded. A third limitation was that study did not look at the gender-wise direction of friends’ influence.
Our findings suggest that tobacco control interventions might be more effective if they distinctly addressed social influences on tobacco use generally and on specific products. Better enforcement of laws against tobacco in dentifrices could also greatly help reduce their use, since these products are used by whole families. The influence of any form of advertising (including point of sale or surrogate) on an individual is potentially amplified by the influence of that person’s tobacco use on close social contacts. Thus, enforcement of rules banning tobacco advertising can potentially prevent tobacco use even by those not exposed to the ads. Future research could design and analyse interventions that address social networks for tobacco use cessation.
CONCLUSION
In India, adult tobacco use is strongly associated with having one or more close social contacts using tobacco in the same form. Interventions for tobacco cessation are likely to be more effective if they address the influence of family and friends on tobacco use to reduce its social acceptability.
Acknowledgments
We thank the project managers at U. Waterloo, Canada and those at Healis Sekhsaria Institute for Public Health in India, the state collaborators, all the interviewers and respondents. We also thank Mr. Sameer N. Narake, Healis, for technical support for data analysis and checking of results; we acknowledge Ms. Jooi Vasa, Healis, for editorial comments.
Funding: The TCP India Project was supported by grants from the US National Cancer Institute (P01-CA138389), Canadian Institute of Health Research (57897, 79551, and 115016) and Ontario Institute for Cancer Research Senior Investigator Award. GTF was supported by a Senior Investigator Award from the Ontario Institute for Cancer Research and by a Prevention Scientist Award from the Canadian Cancer Society Research Institute.
Footnotes
Contributions: CSR developed the initial concept for this paper; CSR developed and undertook the data analysis with guidance and support from MSP, PCG. MSP and PCG; CSR wrote the first drafts of the manuscript. MSP and PCG further developed the arguments and structure of for the paper; MBT, ACKQ and GTF contributed to the writing of the manuscript and agree with its results and conclusions. All the authors made critical revisions and approved the final version for publication. The survey was part of the larger ITC project, originally conceived by GTF.
Disclosures and ethics: All study materials and procedures used in the TCP India Survey were reviewed and cleared for ethics by the Office of Research Ethics at the University of Waterloo, Canada and by the Institutional Review Board at the Healis-Sekhsaria Institute for Public Health, Navi Mumbai, India. Written consent was obtained from the particpants for publication of this study. Authors declare no competing interests.
As a requirement of publication authors have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and protection of human research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
References
- 1.Kyaing NN, Islam MA, Sinha DN, Rinchen S. Social, economic and legal dimensions of tobacco and its control in South-East Asia region. Indian J Public Health. 2011;55:161–8. doi: 10.4103/0019-557X.89944. [DOI] [PubMed] [Google Scholar]
- 2.Poland B, Frohlich K, Haines RJ, Mykhalovskiy E, Rock M, Sparks R. The social context of smoking: the next frontier in tobacco control? Tobacco Control. 2006;15:59–63. doi: 10.1136/tc.2004.009886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta PC, Aghi MB, Bhonsle RB, Murti PR, Mehta FS. An intervention study of tobacco chewing and smoking habits for primary prevention of oral cancer among 12,212 Indian villagers. IARC SciPubl. 1986:307–18. [PubMed] [Google Scholar]
- 4.Thakur JS, Lenka SR, Bhardwaj S, Kumar R. Why youth smoke? An exploratory community-based study from Chandigarh Union Territory of Northern India. Indian J Cancer. 2010;47(Suppl 1):S59–S62. doi: 10.4103/0019-509X.63871. [DOI] [PubMed] [Google Scholar]
- 5.Bansode NN. An exploratory study on gutkha and smokeless tobacco consumption. Nurs J India. 2002;93:127–8. [PubMed] [Google Scholar]
- 6.Mishra GA, Shastri SS, Uplap PA, Majumdar PV, Rane PS, Gupta SD. Establishing a model workplace tobacco cessation program in India. Indian J Occup Environ Med. 2009;13:97–103. doi: 10.4103/0019-5278.55129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narain R, Sardana S, Gupta S, Sehgal A. Risk factors associated with tobacco habits among adolescents: a cross-sectional school-based study. Natl Med J India. 2013;26:197–202. [PubMed] [Google Scholar]
- 8.Nichter M, Nichter M, Sickle DV. Popular perceptions of tobacco products and patterns of use among male college students in India. Social Science and Medicine. 2004;59:415–31. doi: 10.1016/j.socscimed.2003.10.032. [DOI] [PubMed] [Google Scholar]
- 9.International Institute for Population Sciences, Ministry of Health and Family Welfare, Government of India. Global Adult Tobacco Survey India (GATS India), 2009–10. New Delhi: Ministry of Health and Family Welfare; Mumbai: International Institute for Population Sciences; 2010. Available from: http://mohfw.nic.in/WriteReadData/l892s/1455618937GATS%20India.pdf Accessed Jun 9 2014. [Google Scholar]
- 10.Alwan A, editor. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization; 2011. Available from: http://www.who.int/nmh/publications/ncd_report_full_en.pdf. [Google Scholar]
- 11.ITC Project. Findings from the Wave 1 Survey 34 (2010–2011) University of Waterloo; Waterloo, Ontario, Canada: Healis-35 Sekhsaria Institute for Public Health; Navi Mumbai, India: Sep, 2013. TCP India National Report. Available from: http://www.itcproject.org/files/TCP_IndiaNR-ENG-Sept25v-web.pdf Accessed Nov 29 2014. [Google Scholar]
- 12.ITC Project. TCP India Survey. Wave I Technical Report. 2013 Jul; Available from: http://www.itcproject.org/files/IN1-TR-July_2013-revised-v3-FINAL.pdf Accessed Nov 29 2014.
- 13.Bhonsle RB, Murti PR, Gupta PC. Tobacco Habits in India. In: Gupta PC, Hamner JE III, Murti PR, editors. Control of Tobacco-related Cancers and Other Diseases; Proceedings of an International Symposium, TIFR; Bombay. January 15–19, 1990; Bombay: Oxford University Press; 1992. pp. 25–46. [Google Scholar]
- 14.Reddy SK, Gupta PC, editors. Tobacco Control in India. New Delhi: Ministry of Health and Family Welfare, Government of India; 2004. Sociocultural aspects of tobacco use; Tobacco use practices; pp. 33–48. Available from: http://mohfw.nic.in/WriteReadData/l892s/4898484716Report%20on%20Tobacco%20Control%20in%20India.pdf [[Last accessed on 2014 Nov 29] [Google Scholar]
- 15.Sinha DN, Gupta PC, Pednekar MS. Use of tobacco products as dentifrice among adolescents in India: questionnaire study. BMJ. 2004;328:323–4. doi: 10.1136/bmj.328.7435.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agrawal SS, Ray RS. Nicotine Contents in Some Commonly Used Toothpastes and Toothpowders: A Present Scenario. J Toxicol. 2012:237506. doi: 10.1155/2012/237506. [published online: 12 Jan.2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Agency for Research on Cancer (IARC) Smokeless Tobacco and Some Tobacco-specific N-Nitrosamines. Lyon, France: IARC; 2007. Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans, Vol. 89; pp. 47–54. [PMC free article] [PubMed] [Google Scholar]
- 18.Rostila M, Almquist YB, Östberg V, Edling C, Rydgren J. Social network characteristics and daily smoking among young adults in Sweden. Int J Environ Res Public Health. 2013;10:6517–33. doi: 10.3390/ijerph10126517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muttarak R, Gallus S, Franchi M, Faggiano F, Pacifici R, Colombo P, et al. Why do smokers start? Eur J Cancer Prev. 2013;22:181–6. doi: 10.1097/CEJ.0b013e32835645fa. [DOI] [PubMed] [Google Scholar]
- 20.Nugent KL, Million-Mrkva A, Backman J, Stephens SH, Reed RM, Kochunov P, et al. Familial Aggregation of Tobacco Use Behaviors in Amish Men. Nicotine Tob Res. 2014;16:923–30. doi: 10.1093/ntr/ntu006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Amin Sel-T, Nwaru BI, Ginawi I, Pisani P, Hakama M. The role of parents, friends and teachers in adolescents’ cigarette smoking and tombak dipping in Sudan. Tob Control. 2011;20:94–9. doi: 10.1136/tc.2010.038091. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan KM, Bottorff J, Reid C. Does Mother’s Smoking Influence Girls’ Smoking More Than Boys’ Smoking? A 20-Year Review of the Literature Using a Sex- and Gender-Based Analysis. Substance Use & Misuse. 2011;46:656–668. doi: 10.3109/10826084.2010.528122. [DOI] [PubMed] [Google Scholar]
- 23.Flay BR, Hu FB, Siddiqui O, Day LE, Hedeker D, Petraitis J, et al. Differential influence of parental smoking and friends’ smoking on adolescent initiation and escalation of smoking. J Health Soc Behav. 1994;35:248–65. [PubMed] [Google Scholar]
- 24.Bandura A. Social cognitive theory. In: Vasta R, editor. Annals of child development. Vol 6 Six theories of child development. Greenwich, CT: JAI Press; 1989. pp. 1–60. [Google Scholar]
- 25.Stoebner-Delbarre A, Aghi MB. A comparative study of perceptions on tobacco in vulnerable populations between India and France. Global Health Promotion. 2013;20(Supp 4):82–9. doi: 10.1177/1757975913501209. [DOI] [PubMed] [Google Scholar]
- 26.Hitchman SC, Fong GT, Zanna MP, Thrasher JF, Laux FL. Socioeconomic status and smokers’ number of smoking friends: findings from the International Tobacco Control (ITC) Four Country Survey. Drug Alcohol Depend. 2014;143:158–66. doi: 10.1016/j.drugalcdep.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]


