Abstract
Purpose
The purpose of this study was to evaluate the efficacy of Betafoam in terms of wound healing and safety.
Methods
Fifty-four male adult Sprague-Dawley rats (weight, 200–250 g) were used in the study. Full-thickness skin defects were created on the back of each rats. The rats were assigned to 6 groups according to the type of wound dressing used (n = 9 for each group): Betafoam, Allevyn-Ag, Mepilex-Ag, Medifoam silver, Polymem-Ag, and gauze. The wound size, histological findings, and amount of DNA on the changed dressings for each group were analyzed and compared.
Results
All groups showed an effective decrease in wound size. However, the differences between Betafoam and the other dressings were statistically significant on day 14 (P < 0.05). The number of newly generated blood vessels in the Betafoam group was significantly higher than in the gauze, Allevyn-Ag, and Medifoam silver groups (P < 0.001). In the Betafoam group, the proportion of collagen deposition was highest and showed a significantly superior arrangement of collagen fibers compared with the gauze, Allevyn-Ag, Mepilex-Ag, and Medifoam silver groups. The total content of the remaining DNA counts of the exchanged dressings were significantly lower in the Betafoam group than the others.
Conclusion
Betafoam is effective in wound healing and provides the best performance amongst the various types of dressing materials in terms of re-epithelialization, angiogenesis, collagen deposition, and tissue invasion.
Keywords: Polyurethane foam, Wound healing, Povidone-iodine, In vivo
INTRODUCTION
Appropriate wound management is a crucial concern in surgical patients because the failure of wounds to heal is associated with profound morbidity, impaired quality of life, and significant economic costs [1,2]. Therefore, surgeons should become actively involved in wound care to optimize the environment in which a wound can heal. Systematic care, such as the correction of medical comorbidities, improvement of nutritional status, or surgical debridement of infected wounds, should be undertaken in accordance with the proper use of dressings to facilitate optimal healing.
An ideal wound dressing would allow adequate gaseous exchange, maintain a moist environment while preventing maceration, allow drainage and absorption of exudates, protect the wound from trauma and infection, facilitate debridement, minimize scarring, and be nonadherent during dressing changes, thereby minimizing trauma and pain. Other practical considerations include cost, availability, and stability in storage and use [3,4].
Conventional gauze dressings work on the basis of forming a dry, protective barrier that can prevent bacterial contamination and absorb exudate. In the 1950s, a new concept for wound management was introduced that promoted moist wound healing to greatly increase re-epithelialization. This method was aimed at occluding the wound to protect it against bacteria while keeping it moist to supply growth factors and prevent crust formation, which would impede wound healing. Since then, a huge variety of products have been developed and used for all types of wounds. These include semipermeable films, hydrogel, alginate, hydrofiber, hydrocolloid, foam, and nonadherent contact [5,6].
Foam dressings are made of polyurethane or silicone, which enables them to handle large volumes of wound fluid. They are indicated for wounds with moderate to high levels of exudates and across a range of wound characteristics. To be used for complicated, infected, or anticipated infected wounds, local antiseptic treatment should be addressed. Silver, in forms such as silver nitrate and silver sulfadiazine, has been used as a topical antimicrobial agent for controlling colonization. Silver-containing foam dressings are now broadly used because they also have broad-spectrum antimicrobial properties. However, the concern with this type of dressing material is cytotoxicity and resistance to the dressing's antimicrobial properties [7,8].
A newly developed polyurethane foam dressing impregnated with 3% povidone-iodine (PI) (Betafoam, Genewel, Seongnam, Korea) achieves powerful antimicrobial properties while also providing a moist environment. PI is a common antimicrobial agent and has been used as a surgical scrub or a skin cleanser in various forms. Although PI has long been used in its different forms because it has good antimicrobial properties, the efficacy of foam dressings with PI has not been confirmed.
In this study, therefore, we evaluated the efficacy of Betafoam in terms of wound healing and safety by comparison with several silver-containing foam dressings in an animal model.
METHODS
Animal and wound model
Animals
This study was reviewed and approved by the ethical committee of Genewel Institutional Animal Care and Use Committee. All parts of the study were performed in the Experimental Animal Research and Breeding Laboratory, Genewel R&D Center, Seongnam, Korea. Fifty-four male adult Sprague-Dawley rats (weight, 200–250 g) were used in the study. The rats were assigned to 6 groups according to the type of wound dressing used (n = 9 for each group): Betafoam, Allevyn-Ag (Smith & Nephew, Hull, UK), Mepilex-Ag (Mölnlycke Health Care, Gothenburg, Sweden), Medifoam silver (Genewel, Seongnam, Korea), Polymem-Ag (Ferris MFG Corp., Burr Ridge, IL, USA), and gauze. All animals were kept under optimal environmental conditions and none of them died during the study periods. The rats were fed freely with pellet food and water. No prophylactic antibiotic therapy was given.
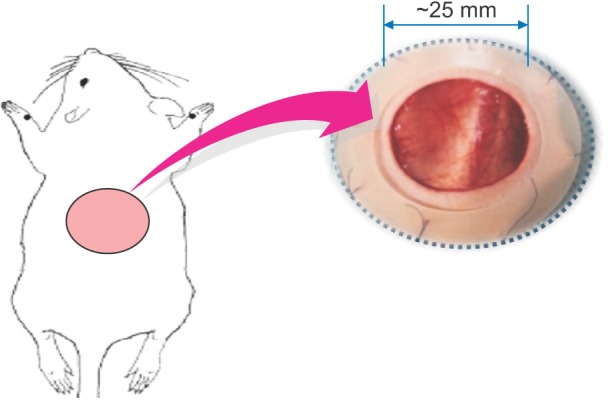
Wound model
After induction of general anesthesia with intramuscular injection of 40- to 50-mg/kg ketamine hydrochloride and 10-mg/kg xylazine hydrochloride, the surgical area was shaved and cleaned with PI solution. Using serrated forceps and iris scissors, a 2.5-cm diameter full-thickness circular piece of tissue was excised from the dorsal skin. Silicone splints were adhered and sutured to the wound perimeter to prevent wound contraction (Fig. 1). The wounds were treated with Betafoam and other control dressings, then covered with a transparent occlusive dressing (Opsite, Smith & Nephew). The dressing was changed every 2 to 3 days and the wound diameter was measured on postwounding days 3, 7, 10, and 14. The wound temperature, humidity, and odor were evaluated on days 3, 7, 10, and 14.
Fig. 1. Full-thickness wound model on the dorsal skin of male adult Sprague-Dawley rats. A 2.5-cm diameter full-thickness circular piece of tissue was excised from the dorsal skin (n = 9 for each group).
Dressing material
The dressings tested in this study were Betafoam, Allevyn-Ag, Mepilex-Ag, Medifoam silver, Polymem-Ag, and gauze. Nine rats per dressing were tested.
Evaluation of wound healing
Wound healing and scar tissue formation
All animals survived and no complications related to the procedure, including infection, were observed. After treatment on days 3, 7, and 14, the wound areas were calculated in cm2. The surface area on the first day after the wounds were prepared was deemed to be 100%, and subsequent changes were compared to that initial area.
Re-epithelialization
On day 7 after wounding, rats from each group were sacrificed and tissue was collected from near the wound site and the wound itself. Tissues were fixed in a 10% formalin solution for hours and prepared for hematoxylin and eosin (H&E) staining to compare the status of re-epithelialization [9]. Re-epithelialization (%) was calculated by sum of each edge's epithelialized area, which was divided by total lengths of wound.
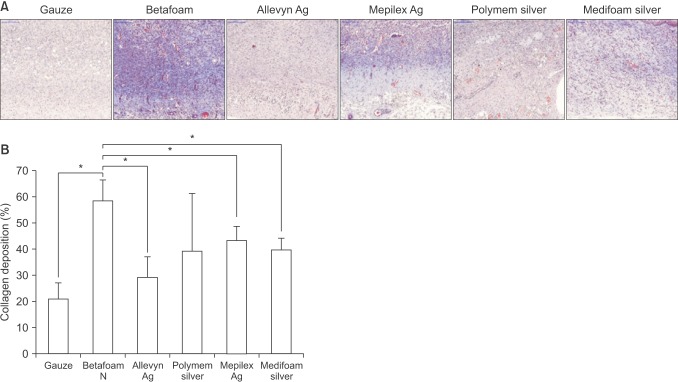
Angiogenesis and collagen deposition
On day 14 after wounding, rats from each group were sacrificed and tissues were collected and stained (H&E stain kit, American MasterTech, Lodi, CA, USA) to assess angiogenesis in the newly forming skin tissue. Collagen deposition over the wound dressing was assessed as the level of inner skin deposition, and the thickness was evaluated by assessment of the full recovery of the impaired skin tissue (Masson's trichrome staining) [9]. Masson's trichome is a 3-color staining protocol used in histology. This method is used for the detection of collagen fibers in tissues such as skin, heart, etc. The collagen fibers will be stained blue and the nuclei will be stained black and the background is stained red. Tissues which stained with Masson's trichrome staining were evaluated its collagen density by using polarized light microscope with the aid of image analyzer software, Image J program (National Institutes of Health, Bethesda, MD, USA).
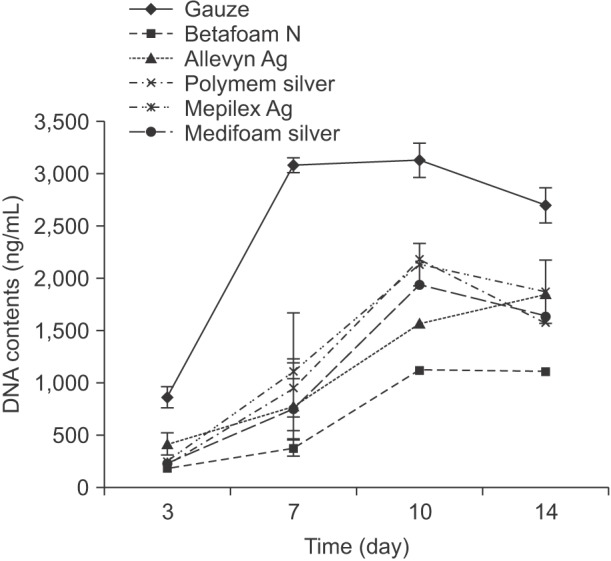
Tissue invasion contents
To evaluate the tissue invasion for exchanged dressings, the amount of residual DNA remaining in the dressings was measured on days 3, 7, 10, and 14. The total DNA was quantified with the CyQuant DNA kit according to the manufacturer's description (Molecular Probes, Eugene, OR, USA) using a fluorescent plate reader (emission, 520 nm; excitation, 480 nm) (Synergy H1, BioTek, Winooski, VT, USA). The standard curve for DNA analysis was generated with λ DNA provided with the CyQuant DNA kit.
Statistical analysis
Values are expressed as the mean ± standard error of the mean with the indicated numbers (n) of experiments. Wound areas were compared at each measurement point using 1-way analysis of variance, an all-pairwise multiple comparisons test (Tukey test), and the Mann-Whitney rank-sum test to determine significant differences. Values of P < 0.05 were considered significant.
RESULTS
Wound healing and scar tissue formation
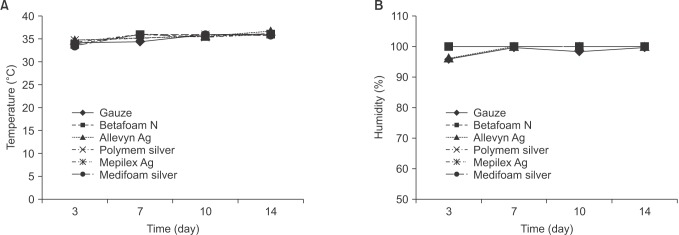
According to measurement of body temperature on wounds at days 3, 7, 10, and 14, no significant difference was observed among the groups (Fig. 2).
Fig. 2. Temperature (A) and humidity (B) for wound healing (n = 9 for each group).
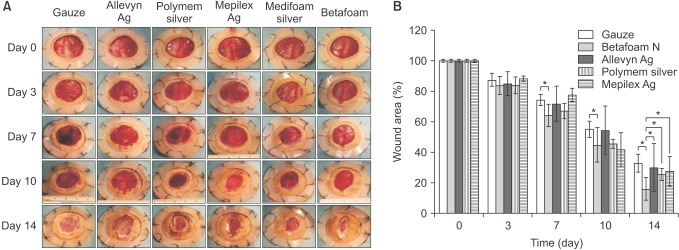
Each group showed decreases in the wound area over time in the following group order: Betafoam, Polymem-Ag, Mepilex-Ag, Allevyn-Ag, Medifoam silver, and gauze (Fig. 3A). According to the numerical comparison of the wound size, all groups showed an effective decrease in the size of the cut wounds. However, the differences between the Betafoam group and the other groups were statistically significant on day 14 (P < 0.05) (Fig. 3B). Additionally, significant differences were found between Betafoam N and gauze groups on days 7 and 10 (P < 0.05) (Fig. 3B).
Fig. 3. Wound areas at each time point. Gross observation (A) and numerical comparison (B) for each group (n = 9 for each group). *P < 0.05.
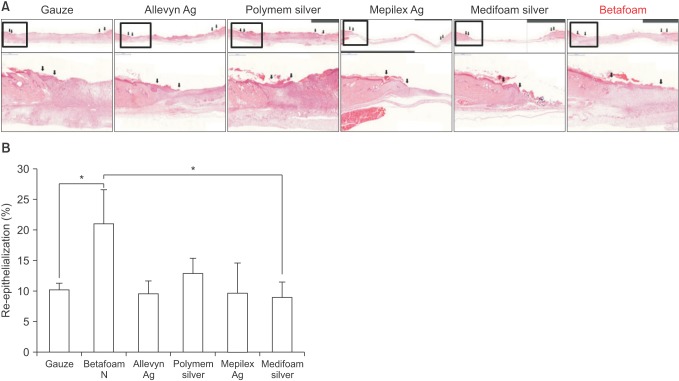
Re-epithelialization
On day 7, all groups were compared according to the area of re-epithelialization. The mean area of re-epithelialization was found to be highest in the Betafoam group (21.0% ± 5.6%) (Fig. 4A), and significant differences were found between the Betafoam group and the gauze group (P = 0.031) (Fig. 4B).
Fig. 4. Histologic analysis of the wound edge and bed. Hematoxylin and eosin staining (×100) (A) and numerical comparison (B) for each group (n = 9 for each group). *P < 0.05.
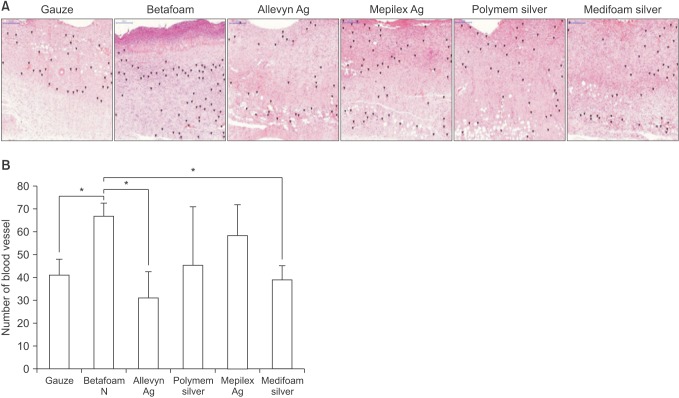
Angiogenesis and collagen deposition
The H&E staining also showed newly generated blood vessels during the experimental analysis (Fig. 5). The results revealed that the mean number of blood vessels in the Betafoam group (n = 67.0 ± 5.6) was significantly higher than in the gauze (n = 41.0 ± 6.9, P < 0.001), Allevyn-Ag (n = 31 ± 11.5, P < 0.001), and Medifoam silver (n = 39.0 ± 6.1, P < 0.001) groups.
Fig. 5. Effects of each dressing material on angiogenesis. Hematoxylin and eosin staining (×200) (A) and numerical comparison (B) for each group (n = 9 for each group). *P < 0.05.
Fig. 6 shows the collagen deposition on the wound bed on postwounding day 14. The order of the mean proportion of collagen deposition was Betafoam (57.4% ± 9.0%), Mepilex-Ag (43.3% ± 5.3%), Medifoam silver (39.7% ± 4.3%), Polymem-Ag (39.2% ± 22.0%), Allevyn-Ag (29.3% ± 7.7%), and gauze (21.0% ± 6.0%). Histologically, the Betafoam group showed a significantly better arrangement of collagen fibers compared with the gauze, Allevyn-Ag, Mepilex-Ag, and Medifoam silver groups (P < 0.001).
Fig. 6. Effects of each dressing material on collagen deposition. Masson's trichrome (×200) (A) staining and numerical comparison (B) for each group (n = 9 for each group). *P < 0.05.
Tissue invasion contents
The effect of each dressing material on tissue separation during dressing changes was investigated. Fig. 7 shows the amount of residual DNA remaining in each exchanged dressing material. The mean total content of the remaining DNA counts of the exchanged Betafoam on days 3, 7, 10, and 14 were 180.4 ± 12.7, 375.8 ± 289.6, 1126.0 ± 119.9, and 1,111.1 ± 277.2 ng/mL, respectively. These levels were determined to be significantly lower than those of the other materials (P < 0.001).
Fig. 7. Amount of residual DNA remaining in each exchanged dressing material (n = 9 for each group).
DISCUSSION
Optimal wound management requires the selection of the most appropriate dressing. The primary focus for wound care is eliminating causative factors such as pressure, shear, moisture, and circulatory impairment; providing systemic support instead of scrubbing wounds; and leaving wounds open to the air [4,8]. Among the various types of dressing materials, foam dressings are most commonly used for good exudate management and shielding from bacterial invasion. Foam in various forms has been widely used for the management of many types of wounds. A large number of clinical results have been published that describe the effectiveness of foam in surgical wounds. Clinical experience from these studies suggests that foam dressings are easy to apply, relatively painless to remove, and therefore preferred by patients and surgeons alike. By their very nature, foam dressings give opportunities to act as carriers for antimicrobial agents, and many kinds of foam dressings that contain silver or other bactericidal agents are available.
Thus far, silver-containing foam dressings have been commonly used for healing wounds, including burns, diabetic ulcers, and surgical wounds. Clinical experience has proved the antibacterial effects of such dressings and, consequently, silver has been used in a variety of dressings in various forms and contents. However, several studies have reported side effects related to silver; in particular, one study demonstrated that silver had cytotoxic effects at the wound site, became deposited in the organs, and inhibited the proliferation of human fibroblasts, thus delaying wound healing [10]. There has also been some concern regarding the use of silver dressings because reactive oxygen species induced by silver are highly reactive and cause oxidative DNA damage and inflammation [11,12,13].
Furthermore, there has been concern that the use of silver dressings may lead to bacterial resistance to antibiotics and silver itself [11]. Therefore, the benefits of the antimicrobial actions of dressing materials need to be carefully balanced against the cytotoxic effects and bacterial resistance that silver can produce.
PI is a commonly used antimicrobial agent. It is a water-soluble complex with elemental iodine bound to a synthetic polymer. It is also a bactericide that can be applied as a paint, spray, or wet soak for various types of wounds including burns, abrasions, lacerations, skin infections, and pressure sores. The basis of its recent development was the premise that the antimicrobial activity of PI was as good as that of current silver-containing foam dressings but was also associated with reduced cost and cytotoxicity. Although the current literature concerning the cytotoxicity of PI is conflicting, some studies have demonstrated improved wound healing through the use of PI [12,13].
The current study showed that Betafoam was the most effective dressing in terms of wound healing and re-epithelialization compared with the various silver-containing foams and the gauze. Wound healing process models including hemostasis, inflammation, proliferation and remodeling, have considerable overlapping phase and re-epithelialization of wounds begins within hours after injury. So we thought that 7 days results would be considerable to evaluate the epithelialization status. Although the wound size generally decreased over time in all groups, the Betafoam group showed the most notable decrease in the size of the cut wound, and the difference between the Betafoam and the other groups was statistically significant on day 14. Also, significant differences were found between Betafoam N and gauze groups on days 7 and 10 (P < 0.05) (Fig. 3B). Levenson et al. [14] demonstrated that the great bulk of collagen formation and gain in tensile strength of healing skin incision is over in the first 2 or 3 weeks, and that the wound reaches its maximal strength at the end of this time. It might be related with fibroplasia, occurring during the first 14 days postoperatively.
After 7 days, re-epithelialization was greater in Betafoam in Fig. 3, however in Fig. 2, wound area was not correlated with the result of re-epithelialization. This discrepancy might come from that re-epithelialization (%) was calculated microscopically, and wound area was analyzed grossly. In terms of re-epithelialization, polyurethane foam dressing has the advantages of stimulating re-epithelialization by enhancing epithelial cell movement and absorbing exudates from the wound [5]. Bennett et al. [13] concluded that PI cream was statistically superior to silver sulfadiazine with regard to the healing of experimental wounds. Consistent with these results, our data demonstrated a significant difference in re-epithelialization between Betafoam and other dressings.
Neovascularization is another important process that takes place during wound healing. The H&E staining also highlighted the capillary network and collagen deposition at the wound edge during the experimental periods. These outcomes demonstrated that the number of blood vessels in the Betafoam group was significantly higher than in the other groups. An in vivo comparison of topical agents on wound repair conducted by Bennett et al. [13] demonstrated that PI cream significantly enhanced angiogenesis compared with other topical agents, including silver. In addition, collagen deposition in the Betafoam group increased to a significantly greater degree than in the other groups. Thus, although the mechanism is still unclear, PI has been proven most effective in collagen deposition while concomitantly increasing angiogenesis.
During dressing changes, minimal mechanical trauma should be inflicted when cleansing wounds because additional trauma to the wound base delays wound healing. Disturbance of the wound base should be minimized not only to avoid additional tissue damage, but also to eliminate unexpected discomfort for the patient and to minimize the spread of microorganisms. To evaluate tissue damage caused during dressing changes, the amount of residual DNA remaining in the dressing materials was measured on days 3, 7, 10, and 14. The results showed that the Betafoam group had less severe tissue separation than any other group.
This study has some limitation. We did not take the inflammatory phase into account in this study. Some may argue that the experimental wound healing model is for the second wound closure, and does not well represent the primary wound repair nor infected wound repair. But we focused basic wound healing characteristics of Betafoam N and further evaluation is needed to evaluated antimicrobial effect for infected wound. We think that partial or full thickness burn wound, pressure sore, diabetic ulcer and chronic venous ulceration could be the best candidate for this material. Also primary surgical wound could benefit from this material for preventing wound infection.
In conclusion, this is the first experimental in vivo study to compare Betafoam and other dressing materials, with a particular focus on full-thickness skin wounds. Our data showed that Betafoam is effective in wound healing and performs best in re-epithelialization, angiogenesis, collagen deposition, and tissue invasion among the various types of dressing materials.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Yuksel EB, Yıldırım AM, Bal A, Kuloglu T. The effect of different topical agents (silver sulfadiazine, povidone-iodine, and sodium chloride 0.9%) on burn injuries in rats. Plast Surg Int. 2014;2014:907082. doi: 10.1155/2014/907082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prestes MA, Ribas CA, Ribas Filho JM, Moreira LB, Boldt AB, Brustolin EV, et al. Wound healing using ionic silver dressing and nanocrystalline silver dressing in rats. Acta Cir Bras. 2012;27:761–767. doi: 10.1590/s0102-86502012001100004. [DOI] [PubMed] [Google Scholar]
- 3.Lin YH, Lin JH, Wang SH, Ko TH, Tseng GC. Evaluation of silver-containing activated carbon fiber for wound healing study: In vitro and in vivo. J Biomed Mater Res B Appl Biomater. 2012;100:2288–2296. doi: 10.1002/jbm.b.32800. [DOI] [PubMed] [Google Scholar]
- 4.Abdelrahman T, Newton H. Wound dressings: principles and practice. Surgery (Oxford) 2011;29:491–495. [Google Scholar]
- 5.Lee JH, Ja Kwak J, Shin HB, Jung HW, Lee YK, Yeo ED, et al. Comparative efficacy of silver-containing dressing materials for treating MRSA-infected wounds in rats with streptozotocin-induced diabetes. Wounds. 2013;25:345–354. [PubMed] [Google Scholar]
- 6.Ge TC, Xing N, Chen J, Zhou JJ, Su GL, Shi JW, et al. Comparison among several foam dressings in the properties of water-absorption, water-locking and air permeability. Zhonghua Shao Shang Za Zhi. 2012;28:349–352. [PubMed] [Google Scholar]
- 7.Ziegler K, Gorl R, Effing J, Ellermann J, Mappes M, Otten S, et al. Reduced cellular toxicity of a new silver-containing antimicrobial dressing and clinical performance in non-healing wounds. Skin Pharmacol Physiol. 2006;19:140–146. doi: 10.1159/000092594. [DOI] [PubMed] [Google Scholar]
- 8.Kramer SA. Effect of povidone-iodine on wound healing: a review. J Vasc Nurs. 1999;17:17–23. doi: 10.1016/s1062-0303(99)90004-3. [DOI] [PubMed] [Google Scholar]
- 9.Losi P, Briganti E, Costa M, Sanguinetti E, Soldani G. Silicone-coated non-woven polyester dressing enhances reepithelialisation in a sheep model of dermal wounds. J Mater Sci Mater Med. 2012;23:2235–2243. doi: 10.1007/s10856-012-4701-8. [DOI] [PubMed] [Google Scholar]
- 10.Zou SB, Yoon WY, Han SK, Jeong SH, Cui ZJ, Kim WK. Cytotoxicity of silver dressings on diabetic fibroblasts. Int Wound J. 2013;10:306–312. doi: 10.1111/j.1742-481X.2012.00977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Percival SL, Bowler PG, Russell D. Bacterial resistance to silver in wound care. J Hosp Infect. 2005;60:1–7. doi: 10.1016/j.jhin.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Kashyap A, Beezhold D, Wiseman J, Beck WC. Effect of povidone iodine dermatologic ointment on wound healing. Am Surg. 1995;61:486–491. [PubMed] [Google Scholar]
- 13.Bennett LL, Rosenblum RS, Perlov C, Davidson JM, Barton RM, Nanney LB. An in vivo comparison of topical agents on wound repair. Plast Reconstr Surg. 2001;108:675–687. doi: 10.1097/00006534-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Levenson SM, Geever EF, Crowley LV, Oates JF, 3rd, Berard CW, Rosen H. The healing of rat skin wounds. Ann Surg. 1965;161:293–308. doi: 10.1097/00000658-196502000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]