Abstract
Objectives
To measure the size and timing of changes in utilization and costs for employees and dependents who had major access barriers to primary care removed, across an 8‐year period (2007 to 2014).
Study design and methods
Retrospective observational study examining patterns of utilization and costs before and after the implementation of a worksite medical office in 2010. The worksite office offered convenient primary care services with no travel from work, essentially guaranteed same day access, and no co‐pay. Trends in visit rates and costs were compared for an intervention fixed cohort group (employees and dependents) at the employer (n = 1211) with a control fixed cohort group (n = 542 162) for 6 types of visits (primary, urgent, emergency, inpatient, specialty, and other outpatient). Difference‐in‐differences methods assessed the significance of between‐group changes in utilization and costs.
Results
The worksite medical office intervention group had an increase in primary care visits relative to the control group (+43% vs +4%, P < 0.001). This was accompanied by a reduction in urgent care visits by the intervention group compared with the control group (−43% vs −5%, P < 0.001). There were no differences in the other types of visits, and the total visit costs for the intervention group increased 5.7% versus 2.7% for the control group (P = 0.008).
A sub‐group analysis of the intervention group (comparing dependents to employees) found that that the dependents achieved a reduction in costs of 2.7% (P < 0.001) across the study period.
Conclusions
The potential for long‐term reduction in utilization and costs with better access to primary care is significant, but not easily nor automatically achieved.
Keywords: access, costs, primary care access, primary care shortage, utilization, worksite medical office
1. INTRODUCTION
What happens when access to primary care is improved? There is a large body of literature that posits that many problems in the US health care system would be greatly ameliorated if primary care were more readily available to patients.1, 2 The belief is that utilization,3, 4 costs,4, 5, 6 quality,7, 8, 9, 10, 11 and patient satisfaction12 would all improve if better access to primary care could be provided. The process by which these positive outcomes would be achieved is widely accepted. Essentially, ready access to primary care would appropriately shift care away from more intensive and expensive care provided in urgent care, emergency departments, specialty departments, and inpatient settings.
Much of the literature on the primary care shortage is focused on the size of the problem (ie, how many additional primary care physicians are required to meet patient needs for primary care),13 the effects of a primary care shortage (eg, higher rates of emergency department use; higher rates of preventable hospitalizations; higher costs),14, 15 the barriers to change,16, 17 and suggestions about changes that might help remedy the problem.18, 19, 20, 21 However, there is much less information about what would happen if ready access to primary care suddenly occurred.22, 23, 24 There is little evidence about how quickly and how much utilization would shift and costs change if ready access to primary care were provided.
This research is intended to help address this gap by examining the impact of an unusual pilot project in which major barriers to accessing primary care were removed. We examine how utilization and costs varied in an employed and insured population after a worksite primary care medical office was built at the workplace of a large employer.
This research provides insight into several fundamental issues. At the policy level, it offers some insight into the size and timing of the shifts in utilization and costs that might be expected if primary care services were more readily available in the United States. At a tactical level, it examines a path—the worksite—to providing convenient full primary care services in which there is immediate, substantial opportunity for employers (78% of large employers in the United States currently do not offer worksite primary care service).25 In the realm of patient‐centred care, this study provides a window into how seriously one should take patient declarations that they would have gone to see their primary care physician “if only I could get in.” Finally, this study offers some sobering lessons about any easy assumption that “all good things go together”—that ready access to primary care will lead to decreased utilization and reduced costs in lockstep fashion.
2. STUDY DATA AND METHODS
2.1. Study population
California Steel Industries, Inc. (CSI) is a steel company with approximately 1000 employees located in Fontana, California. These employees and their dependents receive health coverage from CSI. This study examines the annual utilization and costs of employees of CSI and their dependents who were insured by Kaiser Permanente (KP) from 2007 to 2014 (approximately 60% of all the employees and dependents at CSI). Across this 8‐year period, we followed a fixed cohort of KP members covered by CSI (our intervention group), beginning with 1211 members in 2007, with an annualized turnover rate of 5.4% per year (see Appendix Exhibit 1).
As a control group, we examined all the visits of a fixed cohort of KP members, ages 0 to 64, in the “Inland Empire” area (the larger geographic area around CSI in which most CSI employees live) across this same time period, starting with 542 162 members in 2007. We used propensity weighting to reweight this control group to match the intervention group on gender, age, ethnic composition, and BMI (Table 1). This control group receives their care at the same Kaiser medical centres in the Inland Empire where CSI KP members received their care prior to the opening of the worksite medical office.
Table 1.
Demographic comparison of intervention and control group, 2007
| Intervention group (CSI) % (n = 1211) | Control group (Inland Empire) % (n = 542 162) un‐weighted | Control group (Inland Empire) % (n = 424 892) propensity score weighted | |
|---|---|---|---|
| Gender | |||
| Female | 45 | 51 | 45 |
| Male | 55 | 49 | 55 |
| Age | |||
| 0–17 | 32 | 33 | 31 |
| 18–29 | 14 | 15 | 14 |
| 30–49 | 29 | 21 | 33 |
| 50–64 | 25 | 21 | 23 |
| Ethnicity | |||
| Hispanic | 44 | 38 | 44 |
| Non‐Hispanic White | 44 | 34 | 44 |
| Non‐Hispanic Black | 4 | 10 | 4 |
| Others/unknown | 8 | 19 | 8 |
| Body mass index | |||
| <25 | 20 | 28 | 20 |
| 25–29 | 17 | 20 | 17 |
| 30–34 | 14 | 13 | 14 |
| 35–39 | 8 | 6 | 8 |
| 40+ | 4 | 4 | 4 |
| Unknown | 36 | 29 | 36 |
Finally, we included in both the intervention and control groups only those who were continuously insured by KP from 2007 to 2014. We excluded from both groups anyone 65 years old or older, as there were almost no employees at California Steel Industries in this age category.
2.2. Intervention
In January, 2010, the worksite medical office (the “Family Health Center”) was opened at CSI. This Center was created as a joint effort between California Steel and KP. The Family Health Center is a small 2 exam room medical office located on the 430 acre campus of the steel mill. It is staffed by 2 half‐time family medicine doctors, a nurse, and a receptionist, open Monday through Friday from 7:30 am to 4:30 pm. Employees rotate among shifts across the year so that all have equal access to the clinic. We compare the utilization and visit costs at CSI before and after the opening of the Family Health Center at the worksite.
Three major barriers to primary care were minimized for this population. First, travel time from work to the doctor's office was eliminated, and primary care was readily available to employees where they were already going to be on work days. Second, the supply of physician services at the worksite clinic was such that same day, timely access to primary care was essentially guaranteed (reflected in an average of only 12 doctor visits per day in 2013 and an extremely high average patient satisfaction score for wait time for an appointment of 9.5 on a 10 point scale). Third, employees and their dependents paid no co‐pay for a doctor visit at the worksite medical office. In short, the opening of the worksite clinic provided convenient and free primary care services.
2.3. Measuring utilization
Utilization was measured by in‐person visits per member per year. The visits are captured in the electronic medical record system used by KP. The 6 categories of visits measured were as follows: (1) primary care; (2) urgent care; (3) emergency care; (4) inpatient; (5) specialty; and (6) other outpatient visits.
For cost purposes, inpatient visits were further analysed by the length‐of‐stay in the hospital and whether or not the stay involved surgery.
2.4. Measuring the costs of care
The costs of care per visit were obtained from the 2009 Medical Expenditure Panel Survey (MEPS) and are based on national figures.26 These MEPS costs include payments for a visit from all sources (including private insurance, out‐of‐pocket, government insurance, etc) and include prescription medications. These 2009 costs are imputed to all KP visits, thus giving a true sense of cost trends, and inherently avoiding the impact of medical inflation. The costs per visit used were as follows: $152 for primary care; $960 for emergency care; $260 for specialty care; $218 for “other outpatient” visits. The cost for an urgent care visit was $156, based on the most authoritative study of costs in that setting.27 KP operates in a capitated structure rather than a fee‐for‐service model, so we are using visit costs from MEPS because it makes our findings more generalizable.
Inpatient cost estimates are also imputed based on a 2010 Medical Expenditure Panel report, with a cost of $7566 per day for surgical stays and $2560 per day for non‐surgical stays, applied to the actual length of stay (capped at 4 days or more).28
2.5. Statistical analyses
Using the full dataset of intervention and control cases, logistic regression was employed to estimate the propensity of subjects being in the CSI intervention.29 Predictor variables were age, sex, race ethnicity, and BMI. Propensity score weights were calculated using the average treatment effect for the treated (ATT) method. These weights reweight the control group to look like the intervention group. This method estimates the average effect of intervention on those subjects in the intervention. Thus, the distribution of the measured baseline covariates is similar between the intervention and control subjects after weighting. Next, a propensity score‐weighted logistic regression model was fitted to compare the outcomes. After weighting, the standardized differences were calculated for all baseline covariates.30 The largest standardized difference was 0.11% for primary care visits count (see Appendix Exhibit 4).
The difference‐in‐differences model was estimated as a Poisson regression with an intervention indicator, a post period indicator, and an intervention by post period interaction term. The coefficient of the interaction term is the D‐I‐D estimate of the intervention effect. ATT weights were used, and a person level random effect was incorporated to adjust standard errors for the clustering of observations within subject.
Cost factors were not modelled directly. Rather, we modelled utilization using a Poisson regression, and then the standard cost factors were applied to the results of the Poisson model.
To explore the possible effects of over dispersion, we fit an alternative negative binomial model. The results were similar, and no significant treatment effects lost their significance.
We used SAS Version 9.3 to conduct the analyses. The Institutional Review Board of Kaiser Southern California approved this study.
3. RESULTS
3.1. Trend in visit rates: Intervention vs control group
The visits rates (per person per year) of the intervention group (California Steel KP members) and the control group (Inland Empire KP members) significantly diverge from each other on 3 measures following the implementation of the worksite medical office in 2010 (Table 2). The worksite medical office intervention group had an increase in primary care visits of 43% compared with only a 4% increase for the control group. The intervention group simultaneously had a decrease of the use of urgent care of 43%, while the urgent care utilization only dropped by 5% for the control group. These shifts would seem to be associated and suggest there was some substitution of one (primary care) for the other (urgent care). Finally, there is an increase in the total number of visits of the intervention group (18%) relative to the control group (6%). It should be noted that there was a rapid adoption of using the Family Health Center for primary care in the intervention group, with 47% of their primary care visits taking place there in the first year and then levelling at approximately 60% of all primary care visits in the following years (data not shown).
Table 2.
Percentage change in visits/person/year, post (2010–2014) vs pre (2007–2009). Comparison between intervention and control groups
| Intervention group | Control group | Difference in differences P value | |||||
|---|---|---|---|---|---|---|---|
| Pre avg. visit rate (2007–2009) | Post avg. visit rate (2010–2014) | % change post vs pre | Pre avg. visit rate (2007–2009) | Post avg. visit rate (2010–2014) | % change post vs pre | ||
| Primary care | 1.90 | 2.72 | +43% | 1.90 | 1.97 | +4% | <0.001 |
| Urgent care | 0.47 | 0.27 | −43% | 0.44 | 0.41 | −5% | <0.001 |
| Emergency dept. | 0.17 | 0.17 | −4% | 0.17 | 0.19 | +8% | 0.245 |
| Inpatient | 0.08 | 0.06 | −24% | 0.08 | 0.07 | −19% | 0.781 |
| Specialty | 1.36 | 1.60 | +18% | 1.40 | 1.66 | +19% | 0.986 |
| Other outpatient | 1.32 | 1.44 | +8% | 1.58 | 1.68 | +6% | 0.309 |
| Total | 5.30 | 6.27 | +18% | 5.57 | 5.97 | +6% | 0.008 |
| Avg. N | 1094 | 853 | 364 485 | 249 417 | |||
Source: See online Appendix Exhibit 2A and 2B for detailed trend results and P values for % change of post vs pre intervention results. For those interested in the regression coefficients, see online Appendix Exhibit 4.
In terms of the other types of visits, there were no significant differences between the intervention and control groups. Among these non‐significant visits, the one which comes closest to significance is emergency care. While the changes in emergency care are not statistically significant, the trends are in the direction one might expect with the intervention group dropping 4% while the control group rose 8%.
In summary, comparing the intervention group to the control group, primary care visits increased quite a bit more in the intervention group with a concomitant greater decrease in utilization of urgent care, and an insignificant but noteworthy decrease in emergency room care.
3.2. Trend in visit rates within the intervention group: California Steel KP employees vs California Steel KP dependents
We conducted a simple stratification of the intervention group, examining differences in the trends between CSI KP employees and CSI KP dependents. The rationale for this stratified analysis was to explore he impact of the more limited improvement in primary care access for dependents. Dependents, of course, did not have the reduced travel time from work to the medical office of employees. They did, though, experience the timely access of nearly guaranteed same day appointments to primary care and no‐copay of employees.
The trend in the visit rates of CSI employees and CSI dependents were strikingly different in several areas (Table 3). While the primary care visit rate increased for the CSI employees by 96% from the pre to post intervention period, it only increased by 15% for the CSI dependents. This would seem to reflect the relative geographic convenience of the Family Health Center for employees travelling to work 5 days each week compared with the dependents who are not normally or regularly in the vicinity of California Steel and the Family Health Center. Mirroring that difference, the total number of visits increased by 44% for the employees, while it increased only 3% for dependents. The 2 groups also had a significant difference in the trend of emergency care—with dependent emergency use rising 11% while employees' emergency use fell by 30%. Despite these differences, however, both employees and dependents exhibited strong decreases in the utilization of urgent care.
Table 3.
Percentage change in visits/person/year, post (2010–2014) vs pre (2007–2009). Comparison between employees vs dependents in the intervention group
| Intervention group | |||||||
|---|---|---|---|---|---|---|---|
| Employees | Dependents | Difference in differences P value | |||||
| Pre avg. visit rate (2007–2009) | Post avg. visit rate (2010–2014) | % change post vs pre | Pre avg. visit rate (2007–2009) | Post avg. visit rate (2010–2014) | % change post vs pre | ||
| Primary care | 1.69 | 3.33 | +96% | 2.03 | 2.33 | +15% | <.001 |
| Urgent care | 0.36 | 0.19 | −46% | 0.54 | 0.31 | −42% | 0.673 |
| Emergency dept. | 0.17 | 0.12 | −30% | 0.18 | 0.20 | +11% | 0.017 |
| Inpatient | 0.07 | 0.06 | −14% | 0.09 | 0.06 | −29% | 0.761 |
| Specialty | 1.37 | 1.88 | +37% | 1.35 | 1.43 | +6% | 0.163 |
| Other outpatient | 1.40 | 1.69 | +21% | 1.28 | 1.28 | +1% | 0.151 |
| Total | 5.06 | 7.27 | +44% | 5.47 | 5.61 | +3% | <.001 |
| Avg. N | 435 | 338 | 659 | 515 | |||
Source: See online Appendix Exhibit 3A and 3B for detailed trend results and P values for % change of post vs pre intervention results.
3.3. Trend in costs
The average costs for all visits for the intervention group increased by 5.7% from the pre to the post intervention period (Figure 1). The average costs for all visits for the control group increased by 2.7% over this same time period. In summary, the intervention group averaged 3% more on costs than the control group in the 5 years of the post‐intervention period.
Figure 1.
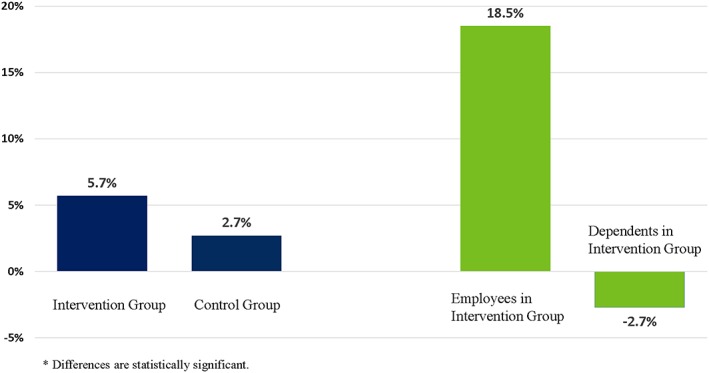
% change in average annual cost*: Post (2010–2014) vs pre intervention (2007–2009)
The 2 subgroups of the intervention group (employees and dependents) show quite different cost trends (Figure 1). While employees' costs rose 18.5%, those of dependents decreased by 2.7%. These different cost trends seem in keeping with the different trends in visit rates shown in Table 3.
The yearly trends behind these averages show a very steady level of costs for the control group (Figure 2). However, the intervention group has a much more uneven pattern of ups and downs. The dependents in the intervention group consistently had the lowest costs after the implementation of the worksite clinic.
Figure 2.
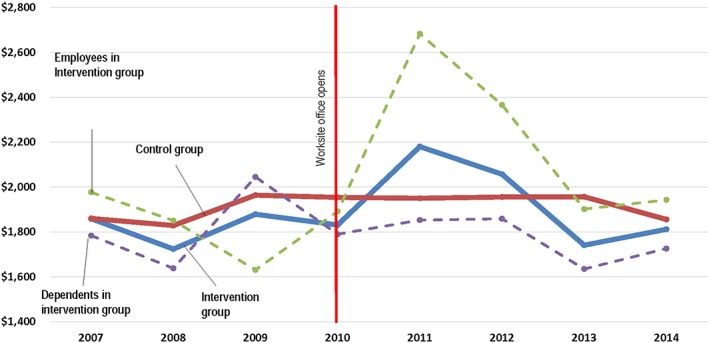
Trend of medical costs from 2007 to 2014 (costs per member per year)
4. DISCUSSION
There is a substantial evidence that improved or better access to primary care is associated with decreased utilization of the emergency department, decreased inpatient admissions, decreased surgeries, and lower costs.1, 4, 31 Based on these previous findings, it seemed reasonable to expect that the implementation of a worksite medical office at a large employer would produce similar results. At first glance, the results would seem to meet this expectation with decreases in utilization for the CSI KP members in urgent care (−43%), emergency care (−4%), and inpatient admissions (−24%), accompanied by a large increase in (43%) in the use of primary care—a counter balance to the utilization decreases that is sometimes not thoroughly discussed or explored. However, taking into account the changes in the control group, the results from this study did not match these expectations in many ways.
Despite the large increase in primary care utilization that has continued in the years after the opening of the worksite medical office, emergency room utilization did not change significantly from that of the control group. The trend in emergency room utilization is in the expected direction (that is, it decreased)—but it did not achieve statistical significance. Similarly, hospital admissions trended in the expected direction but also did not reach the level of statistical significance compared with the control group. The only significant shift in the expected direction was for urgent care.
A second and related surprise was the trend in costs. Cost savings are often assumed in discussions concerning increased primary care access (with the more specific questions of how much and how soon often not addressed).6, 32, 33, 34 However, this study found that taking all visits into account, costs increased more in the intervention group (+5.7%) than in the control group (+2.7%). There were no cost savings. The increases in primary care utilization were large enough that they swamped any potential savings from decreased utilization in other types of visits. This suggests that there can be a point at which more primary care access and visits are not substituting for other more expensive types of visits but rather adding utilization for a population. It appears that the CSI worksite clinic may have crossed that boundary.
A closer look at the results reveals 2 reasons for some optimism about the potential long‐term cost results of a worksite clinic. First, the results for dependents suggest that it is possible to achieve a more balanced shift in utilization in which a relatively modest increase in primary care access can have a large effect. The Kaiser employees at CSI increased their primary care visits by 96%. However, the Kaiser dependents increased their primary care visits by only 15%, yet also experienced decreases in urgent care (−42%) and inpatient visits (−29%). Dependent costs, as a result, declined 2.7% compared with a 2.7% increase for the control group—implying a 5.4% annual savings. An annual savings of this magnitude is a noteworthy outcome for both employers and employees, given that the family coverage premiums in the United States have increased at an annual average rate of 4.7% across the last 10 years (2007–2016).35 The compounded effect of achieving such savings over multiple years would be of great consequence. In short, access to primary care may be structured in ways that make it too easy or too difficult, but there seems to be a point at which the access is “just right”—achieving the beneficial results without a huge uptick in primary care utilization.36
Second, the increased costs for the intervention group as a whole are largely driven by the large increases in costs in 2 years (20% in 2011 and 13% in 2012, Figure 2). In 2011, a larger number of cases with longer lengths of stay in the hospital (even with a cap of 4 days to limit outliers) drove the increases in overall visit costs (data not shown). This type of risk is no doubt more pronounced for any employer with 1000 employees, which is at the lower end of the “large” employer category. If one averages only the costs for 2010, 2013, and 2014, the post intervention costs for the intervention group are instead a decrease of 1.4%.
Will the future costs at California Steel look more like 2010, 2013, and 2014, when costs were flat or down, or more like 2011 and 2012 when costs were up? We don't know. It is impossible to predict if or how often adverse events that drove overall costs are likely to recur. We will track and report on these trends in future years as California Steel has contracted to continue the worksite clinic for at least another 5 years.
These results suggest that additional worksite pilots with employers with substantially larger populations than 1000 employees (perhaps in the 5000+ employee range) could be helpful. It may be that these larger employers will be less vulnerable to and better able to smooth out the inevitable ups and downs in health risk. These larger employee populations will allow finer tuned measurement of the trends in emergency and inpatient utilization. Finally, a larger employer may also be able to structure and adjust their primary care access to better mirror the results found here for dependents.
4.1. Strengths and weaknesses
Certain limitations of this study should be considered. First, this study does not conduct a comprehensive ROI analysis of all costs and savings associated with the creation of the worksite clinic. There is no agreed upon ROI approach to evaluating worksite clinics.21 However, this study focuses on costs based on the MEPS estimates, which capture all the major cost factors that are likely to drive long‐term cost trends.
Second, this study does not control for changes in co‐payments and deductibles. We have detailed knowledge of the changes that occurred at CSI in these areas across the study period. The copayment for a visit to the on‐site clinic was implemented and remained at $0 per visit during the intervention years. Other copayments increased somewhat over time. For example, an off‐site primary care visit went from $15 in 2008 to $30 in 2014 (reflecting the desire of CSI to encourage the use of the on‐site clinic). CSI never implemented any plans with deductibles. However, it is not possible to compare and control for these changes in the control group. Copayments and deductibles are determined in the United States by an employer for their employees and dependents. Our control group consists of hundreds of thousands of individuals who work for thousands of different employers, who each made decisions year by year about the copayments and deductibles for their employees and dependents. There was no practical way to adjust for these changes among these thousands of employers.
Third, by design, this study does not look at quality and clinical outcomes. These may be the subject of future research for us. There are several studies showing that increased primary care utilization and/or decreased spending does not imply a decrease in quality.5, 7, 8, 9, 37
Fourth, there were some differences in attrition in the fixed cohorts between the CSI and control populations. Gender, Hispanic ethnicity, and unknown BMI were differential predictors of attrition.
There are 6 strengths in this study which should be highlighted and contribute to the literature on the impacts of improved primary care access. It involves a more generalizable population than many studies (examining the employed, insured population rather than much narrower populations such as the uninsured or those in Medicaid or Medicare)3, 38, 39, 40, 41; employs a longitudinal33 rather than a cross‐sectional approach3, 4, 32, 42 (providing a stronger case for causality, and examining longer term effects than just a year or two); includes a large control group; is more comprehensive than many studies (looking at all types of visits, not just ED visits or hospital visits)43, 44, 45, 46, 47, 48; focuses on 3 clear tangible independent variables that are core components of access (travel time, wait time for appointments, and co‐payments)3, 36 rather than difficult factors to change like doctor communication styles49; and, gives some sense of the timing and trends of change.
5. CONCLUSIONS
Our study demonstrates that improving access to primary care for an employed, insured population through the provision of a worksite clinic does not automatically guarantee a shift from more expensive types of visits, such as emergency room visits or inpatient admissions, to primary care. Moreover, the cost impact of this worksite clinic after 5 years involved swings up and down making the long‐term cost impact uncertain. While longer term cost savings seem possible, the path to such savings can involve a bumpy ride. Additional worksite pilots with the largest possible employers would help ascertain the benefits and challenges associated with improved access to primary care.
Supporting information
Appendix S1. Trend in fixed cohorts by year*
Appendix S2A. Comparison of trend in # of visits/person/year between CSI Kaiser members vs Inland Empire Kaiser members.
Appendix S2B. Comparison of trend in # of visits/person/year between CSI Kaiser members vs Inland Empire Kaiser members
Appendix S3A. Comparison between CSI employees and dependents: employee visits/person/year
Appendix S3B. Comparison between CSI employees and dependents: dependent visits/person/year
Appendix S4: Poisson regression results (coefficients on which Table 2 is based)
Appendix S5. Comparison of baseline characteristics between CSI and control subjects
ACKNOWLEDGEMENTS
We thank the leadership team at California Steel Inc. who helped launch and guide the Family Health Center (FHC) and have acted as wonderful partners in this pilot: Brett Guge, Executive Vice President, Finance and Administration; Rod Hoover, Manager of Human Resources; Brad Bray, Manager, Safety and Plant Protection; and, Kyle Schulty, Manager, Communications and Corporate Services. We thank Jeffrey Petrilla, MD, Physician in Charge, CSI Family Health Center, who has managed the Family Health Center, shared his insights, and most importantly cares for the patients at FHC. We also especially want to thank those at Kaiser Permanente who helped launch and guide FHC: William Caswell, SVP, Operations, Chief Operating Officer; Kathy Kigerl, RN, MN, Chief Administrative Officer; Amanda Hauser, Project Manager Lead; and Arthur Moore, Practice Specialist. We want to thank those at Kaiser Permanente's Fontana and Ontario Medical Centres who supported this pilot including: David Quam, MD, the Area Medical Director and Annie Russell, RN, MSN, MBA, Chief Administrative Officer. Finally, we want to thank Jin‐Wen Y. Hsu, PhD, Biostatistician III, and Lie Hong Chen, Biostatistician II, at the Department of Research and Evaluation, who assembled and analysed the data; and John L. Adams PhD, Principal Senior Statistician at the Kaiser Permanente Center for Effectiveness and Safety Research, who offered statistical guidance, for their thoughtful help at many stages in this study. No compensation was received by any of these individuals.
Glass DP, Kanter MH, Jacobsen SJ, Minardi PM. The impact of improving access to primary care. J Eval Clin Pract. 2017;23:1451–1458. https://doi.org/10.1111/jep.12821
REFERENCES
- 1. Shi L. The impact of primary care: a focused review. Forensic Sci. 2012;2012:432892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American College of Physicians . How is a shortage of primary care physicians affecting the quality and cost of medical care? A comprehensive evidence review. White Paper: 2008.
- 3. Cheung PT, Wiler JL, Lowe RA, Ginde AA. National study of barriers to timely primary care and emergency department utilization among Medicaid beneficiaries. Ann Emerg Med. 2012;60(1):4–10.e2. [DOI] [PubMed] [Google Scholar]
- 4. Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, Wright SM. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142–148. [DOI] [PubMed] [Google Scholar]
- 5. Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can primary care visits reduce hospital utilization among Medicare beneficiaries at the end of life? J Gen Intern Med. 2008;23(9):1330–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries' quality of care. Health Aff (Millwood). 2004. Jan‐Jun; Suppl Web Exclusives:W4‐184‐97. [DOI] [PubMed] [Google Scholar]
- 7. Ferrante JM, McCarthy EP, Gonzalez EC, et al. Primary care utilization and colorectal cancer outcomes among Medicare beneficiaries. Arch Intern Med. 2011;171(19):1747–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jerant A, Fenton JJ, Franks P. Primary care attributes and mortality: a national person‐level study. Ann Fam Med. 2012;10(1):34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roetzheim RG, Ferrante JM, Lee JH, et al. Influence of primary care on breast cancer outcomes among Medicare beneficiaries. Ann Fam Med. 2012;10(5):401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Quarterly. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations' health: assessing the evidence. Health Affairs (Project Hope). 2005; Jan‐Jun;Suppl Web Exclusives:W5‐97‐W5‐107. [DOI] [PubMed] [Google Scholar]
- 12. Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47(3):213–220. [PubMed] [Google Scholar]
- 13. Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010‐2025. Ann Fam Med. 2012;10(6):503–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Project Hope). 2010;29(5):766–772. [DOI] [PubMed] [Google Scholar]
- 15. Weisz D, Gusmano MK, Wong G, Trombley J. Emergency department use: a reflection of poor primary care access? Am J Manag Care. 2015;21(2):e152–e160. [PubMed] [Google Scholar]
- 16. Pugno PA, McGaha AL, Schmittling GT, DeVilbiss A, Kahn NB Jr. Results of the 2007 national resident matching program: family medicine. Fam Med. 2007;39(8):562–571. [PubMed] [Google Scholar]
- 17. Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students' career choices regarding internal medicine. JAMA. 2008;300(10):1154–1164. [DOI] [PubMed] [Google Scholar]
- 18. Shipman SA, Sinsky CA. Expanding primary care capacity by reducing waste and improving the efficiency of care. Health Aff (Millwood). 2013;32(11):1990–1997. [DOI] [PubMed] [Google Scholar]
- 19. Shahly V, Kessler RC, Duncan I. Worksite primary care clinics: a systematic review. Popul Health Manag. 2014;17(5):306‐315. [DOI] [PubMed] [Google Scholar]
- 20. Raven MC, Kotchko SM, Gould DA. Can targeted messaging encourage PCP contact before ED visits? Am J Manag Care. Jan 2013;19(1):41–45. [PubMed] [Google Scholar]
- 21. Sherman BW. Worksite clinics and the patient‐centered medical home: competition or collaboration? Am J Manag Care. 2010;16(5):323–325. [PubMed] [Google Scholar]
- 22. Johnston JM, Smith JJ, Hiratsuka VY, Dillard DA, Szafran QN, Driscoll DL. Tribal implementation of a patient‐centred medical home model in Alaska accompanied by decreased hospital use. Int J Circumpolar Health. 2013;72 https://doi.org/10.3402/ijch.v72i0.20960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Driscoll DL, Hiratsuka V, Johnston JM, et al. Process and outcomes of patient‐centered medical care with Alaska native people at Southcentral foundation. Ann Fam Med. 2013;11(Suppl 1):S41–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gottlieb K. The Nuka system of care: improving health through ownership and relationships. Int J Circumpolar Health. 2013;72 https/doi.org/10.3402/ijch.v72i0.21118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. The Kaiser Family Foundation . Employer Health Benefits: Annual Survey, 2012. [Google Scholar]
- 26. Davis KE, Carper K. Use and expenses for office‐based physician visits by specialty, 2009: estimates for the U.S. civilian non‐institutionalized population. Statistical Brief #381. August, 2012. Medical Expenditure Panel Survey. Agency for Healthcare Research and Quality, Rockville, MD; 2012.
- 27. Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321‐328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mirel LB, Carper K. Expenses for hospital inpatient stays, 2010. Statistical Brief #401. February, 2013. Medical Expenditure Panel Survey. Agency for Healthcare Research and Quality, Rockville, MD. [PubMed]
- 29. Austin PC. A tutorial and case study in propensity score analysis: an application to estimating the effect of in‐hospital smoking cessation counseling on mortality. Multivariate Behav Res. 2011;46(1):119–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity‐score matched samples. Stat Med. 2009;28(25):3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bynum JP, Andrews A, Sharp S, McCollough D, Wennberg JE. Fewer hospitalizations result when primary care is highly integrated into a continuing care retirement community. Health Aff (Millwood). 2011;30(5):975–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic variation in expenditures for physicians' services in the United States. N Engl J Med. 1993;328(9):621–627. [DOI] [PubMed] [Google Scholar]
- 33. Cohen R, Lemieux J, Schoenborn J, Mulligan T. Medicare advantage chronic special needs plan boosted primary care, reduced hospital use among diabetes patients. Health Aff (Millwood). 2012;31(1):110–119. [DOI] [PubMed] [Google Scholar]
- 34. Chernew ME, Sabik L, Chandra A, Newhouse JP. Would having more primary care doctors cut health spending growth? Health Aff (Millwood). 2009;28(5):1327–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. The Kaiser Family Foundation . Employer health benefits: annual survey, 2016:35.
- 36. Forrest CB, Starfield B. Entry into primary care and continuity: the effects of access. Am J Public Health. 1998;88(9):1330–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. O'Malley AS, Forrest CB, Mandelblatt J. Adherence of low‐income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. [DOI] [PubMed] [Google Scholar]
- 39. Zahradnik AG. Does providing uninsured adults with free or low‐cost primary care influence their use of hospital emergency departments? J Health Hum Ser Adm. 2008;31(2):240–258. [PubMed] [Google Scholar]
- 40. Raphael JL, Mei M, Brousseau DC, Giordano TP. Associations between quality of primary care and health care use among children with special health care needs. Arch Pediatr Adolesc Med. 2011;165(5):399–404. [DOI] [PubMed] [Google Scholar]
- 41. Momany ET, Flach SD, Nelson FD, Damiano PC. A cost analysis of the Iowa Medicaid primary care case management program. Health Serv Res. 2006;41(4 Pt 1):1357–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Parchman ML, Culler S. Primary care physicians and avoidable hospitalizations. J Fam Pract. 1994;39(2):123–128. [PubMed] [Google Scholar]
- 43. O'Malley AS. After‐hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Aff (Millwood). 2013;32(1):175–183. [DOI] [PubMed] [Google Scholar]
- 44. Rust GY, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE. Practical barriers to timely primary care access: impact on adult use of emergency department services. Arch Intern Med. 2008;168(15):1705–1710. [DOI] [PubMed] [Google Scholar]
- 45. Lowe RA, Localio AR, Schwarz DF, et al. Association between primary care practice characteristics and emergency department use in a medicaid managed care organization. Med Care. 2005;43(8):792–800. [DOI] [PubMed] [Google Scholar]
- 46. Haddy RI, Schmaler ME, Epting RJ. Nonemergency emergency room use in patients with and without primary care physicians. J Fam Pract. 1987;24(4):389–392. [PubMed] [Google Scholar]
- 47. Mortensen K. Access to primary and specialty care and emergency department utilization of medicaid enrollees needing specialty care. J Health Care Poor Underserved. 2014;25(2):801–813. [DOI] [PubMed] [Google Scholar]
- 48. Tao X, Fagan PJ, LeNoach E, Hawkins M, Ross‐Gavin M, Bernacki E. The relationship between a worksite wellness clinic and hospital emergency department visits. J Occup Environ Med. 2015;56:1313–1318. [DOI] [PubMed] [Google Scholar]
- 49. Bertakis KD, Azari R. Patient‐centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229–239. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Trend in fixed cohorts by year*
Appendix S2A. Comparison of trend in # of visits/person/year between CSI Kaiser members vs Inland Empire Kaiser members.
Appendix S2B. Comparison of trend in # of visits/person/year between CSI Kaiser members vs Inland Empire Kaiser members
Appendix S3A. Comparison between CSI employees and dependents: employee visits/person/year
Appendix S3B. Comparison between CSI employees and dependents: dependent visits/person/year
Appendix S4: Poisson regression results (coefficients on which Table 2 is based)
Appendix S5. Comparison of baseline characteristics between CSI and control subjects


