Abstract
Hamstring autografts are frequently used for anterior cruciate ligament reconstruction. The inherent variability in graft diameter has been stated as a disadvantage in its use because the presence of smaller graft diameters has been correlated with increased risk of re-rupture. Several techniques have been described to address this concern. Modifications of the basic Graftlink technique allows for increased control over final graft diameter using a standard harvest of the semitendinosus tendon with or without the gracilis tendon, and results in a graft of adequate length and diameter in all patients with rigid cortical fixation on the femur and tibia.
Hamstring autografts are frequently used for anterior cruciate ligament (ACL) reconstruction. The inherent variability in graft diameter has been stated as a disadvantage in its use.1
Graft diameter has been correlated with the increased risk of re-rupture. Magnussen et al.2 had evaluated hamstring autograft diameter as a predictor for graft failure and its need for revision. In a study of 256 patients with hamstring autograft ACL reconstruction, grafts larger than 8.5 mm had a 1.7% revision rate, and grafts between 8.0 and 8.5 mm and 7.5 and 8.0 mm had a revision rate of 6.5% and 6.2%, respectively. In the same study, grafts that ranged from 7.0 to 7.5 mm and 7 mm or less had a revision rate of 11.3% and 33%, respectively.
Preoperative determination of hamstring graft size is challenging. Magnetic resonance imaging and ultrasound scanning have been used to predict hamstring graft sizes with moderate success.3 Anthropometric data collection has also been used with more success in the literature4 though the confidence intervals remain too large for an accurate clinical use.
To increase the final graft size obtained from a standard hamstring harvest, several techniques have been described.1, 5, 6 These techniques use an increased number of hamstring strands to increase graft diameter as required. We have developed a working algorithm to avoid undesirable small graft diameter and to tailor the final graft diameter to the most appropriate for each given patient. Adjustable cortical fixation in both the femur and tibia makes this possible. Although this results in shorter graft lengths that may raise some concerns, the basic science data show that 15 mm of graft in each tunnel is sufficient to ensure histologic maturity and biomechanical strength of the tendon-bone junction,7 mitigating that risk.
In this Technical Note, we present a simple modification of the Graftlink (Arthrex, Naples, FL) preparation technique, and a working surgical algorithm. This technique has the advantage of giving some control to the surgeon over the resulting final graft diameter. It can be prepared to match the size and demands of the individual patient using a standard harvest of the semitendinosus tendon (ST) with or without the gracilis tendon (GT) and allows creation of a graft of adequate length and diameter in all patients with rigid cortical fixation on the femur and tibia.
Technique
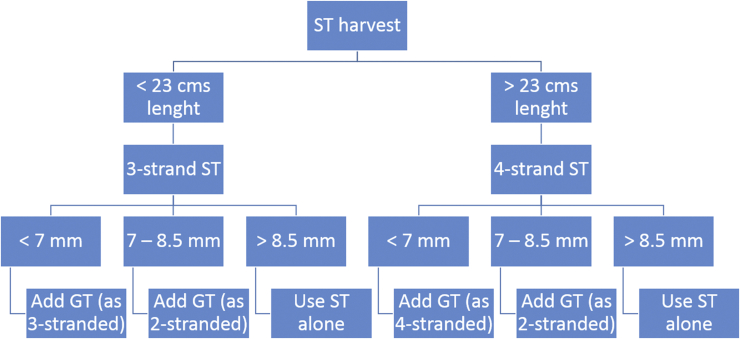
In Figure 1, we present a flowchart for graft configuration depending on the desired graft diameter and the length of the tendons harvested.
Fig 1.
Algorithm for graft preparation depending on the inital ST graft diameter. (GT, gracilis tendon; ST, semitendinosus tendon.)
Via an anteromedial incision the sartorius fascia is identified. A small incision is made along the line of the hamstring tendons, and the ST is harvested from the deep surface of the sartorius fascia and cleared of any residual muscular tissue.8 Its length is measured. Using the chart shown in Figure 1 a decision is made to either triple or quadruple the graft. With an Alice clamp on either end, the graft is folded twice to create a temporary 4-strand graft that can be sized with the sizing tubes. Depending on the diameter obtained, the decision to add the GT, and the configuration in which to use it, can be made (Fig 1). If the graft diameter is >8.5 mm, the ST alone is used (see Video 1). If the graft diameter is <8.5 mm, the GT is harvested in the same fashion, and added to the construct as per Figure 1. If it is <7 mm, the GT is sutured to the ST using a baseball stitch of 0-FiberWire (Arthrex) to create 2 strands that can either be tripled or quadrupled depending on its length.
Using the Arthrex preparation station, a TightRope button (Arthrex) and suture are set up at one end, and a single TightRope ABS (Arthrex) loop is set up at the other end. The ST (with or without the GT added) is passed through the ABS loop and its 2 free ends are sutured together with a FiberLoop (Arthrex). This free end is then passed through the loop of the TightRope end (Fig 2) and back to the tibial end. It is docked in the center of the graft by passing 1 suture of the FiberLoop between the 2 strands and drawing the graft into the center of the strands (Fig 3). If required, the GT is prepared (Fig 4) by putting a No. 2 Ethibond (Ethicon, Somerville, NJ) suture at each end in a locking suture configuration. It is passed through the TightRope loop (Fig 5) at the femoral end of the graft and tensioned over the 4-strand ST to create a 6-strand construct. A cerclage suture of No. 0 FiberWire is then placed at each end, 20 mm from the end of the graft, taking care to make a pass through each strand (Fig 6). If needed, a second cerclage suture can be added at the tibial end 10 mm away from the previous one (see Video 1).
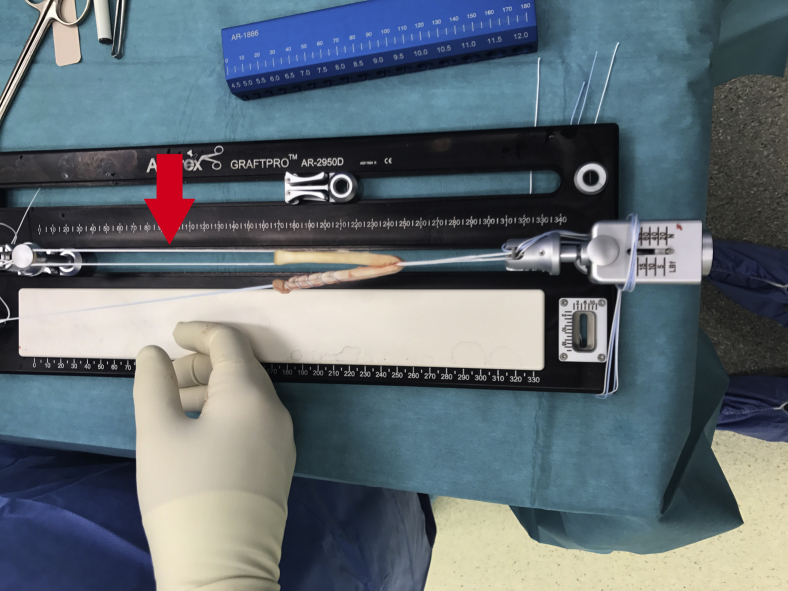
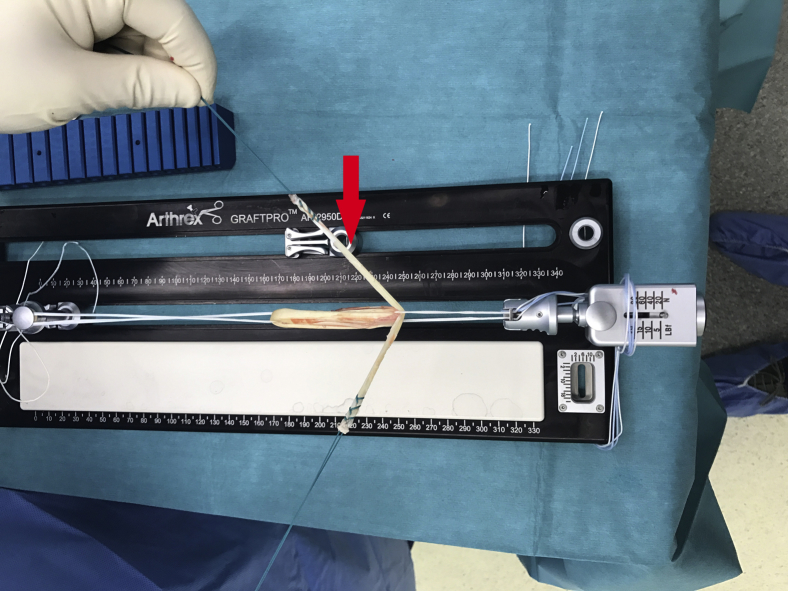
Fig 2.
The semitendinosus tendon is passed through the ABS loop (red arrow) and its 2 free ends are sutured together with a FiberLoop. This free end is then passed through the loop of the TightRope.
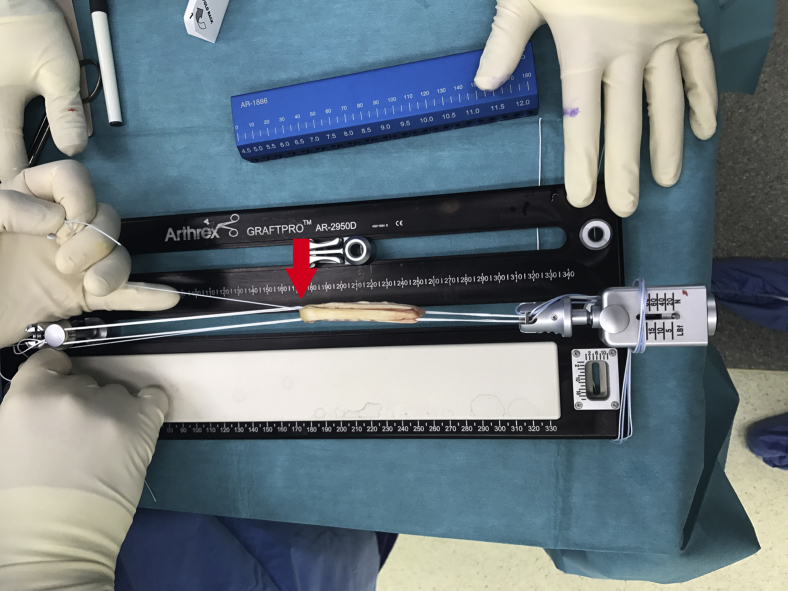
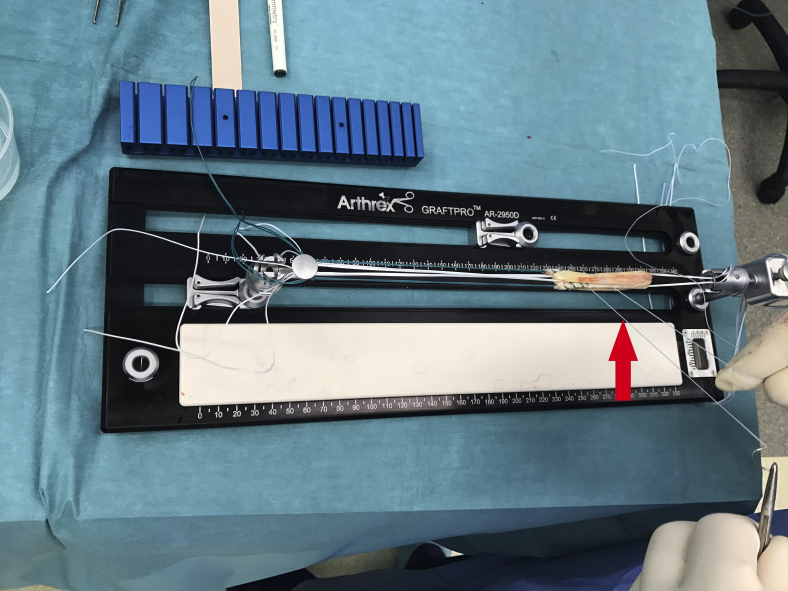
Fig 3.
Free end of the semitendinosus tendon 4-strand graft docked (red arrow) in the center of the graft by passing 1 suture of the FiberLoop between the 2 strands and drawing the graft into the center of the strands.
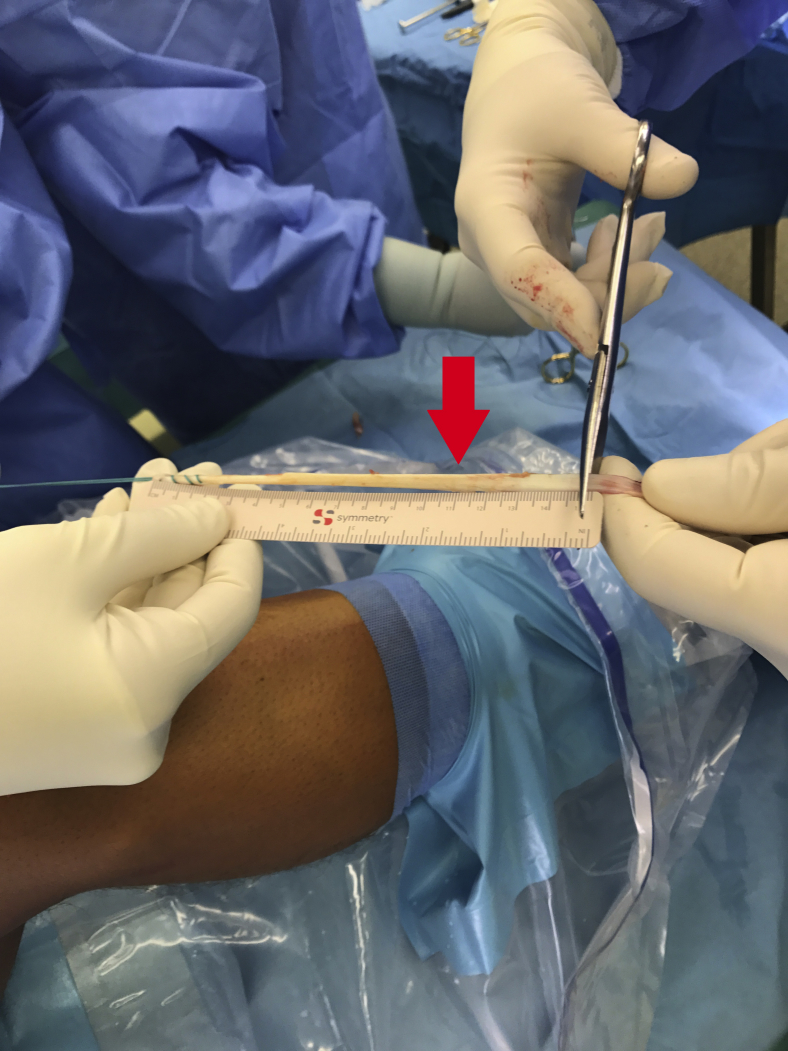
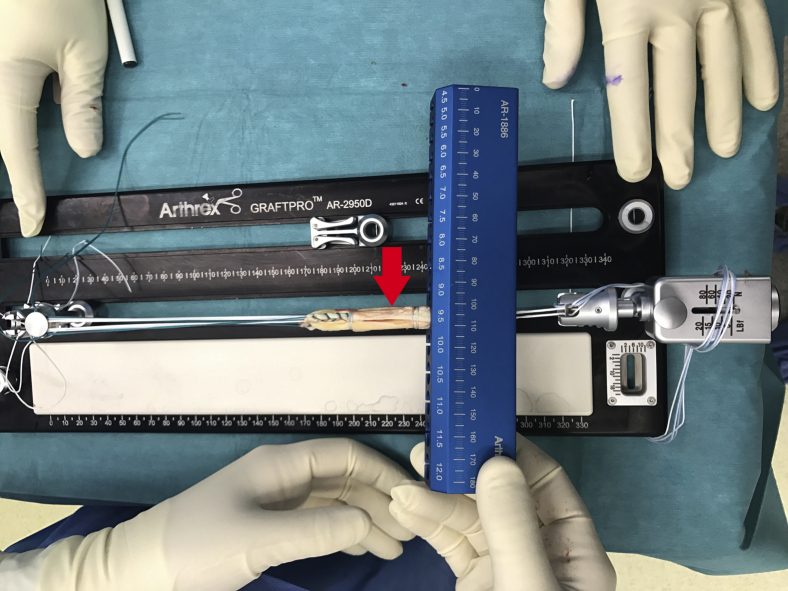
Fig 4.
Preparation of the secondarily harvested gracilis tendon (red arrow).
Fig 5.
Gracilis tendon (red arrow) passed through the loop of the cortical fixation button to enlarge the initial semitendinosus tendon-4 graft.
Fig 6.
A cerclage suture of No. 0 FiberWire (red arrow) is then placed at each end, 20 mm from the end of the graft taking care to make a pass through each strand.
The graft is again resized in diameter and length for final conformation (Figs 7 and 8). Generally, the femoral end is initially 0.5 mm bigger than the tibial end. The sizing tube is left in situ over the femoral end to facilitate some graft compression of this femoral end, resulting in an equal diameter to the tibial end of the graft as well as easier graft passage, and the construct is left under tension while the tunnels are created.
Fig 7.
Diameter measurement of the final 6-strand graft (red arrow).
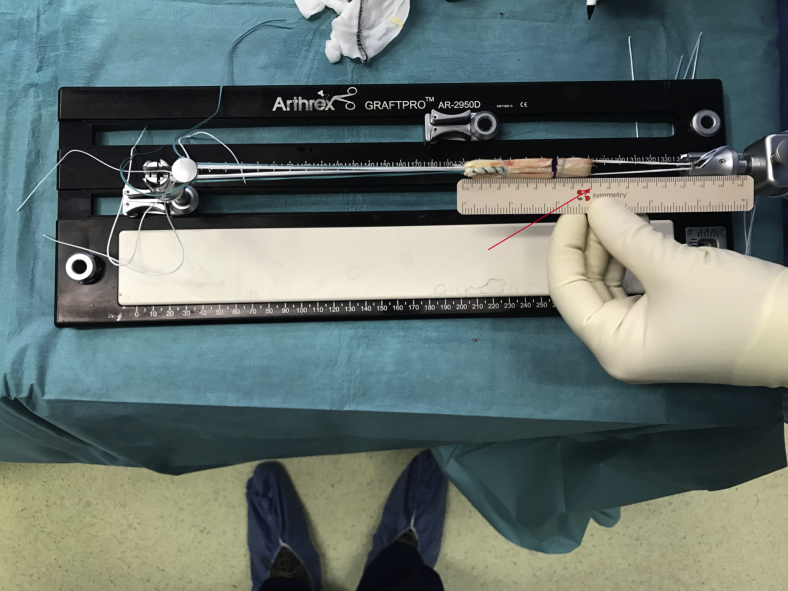
Fig 8.
Length measurement of the final 6-strand graft at 70 mm (red arrow).
On the femur a socket is created using the diameter of the femoral end of the graft, to a depth of 20 mm. The tibial tunnel is a complete tunnel drilled in an antegrade fashion with the same diameter as the tibial (and femoral) end of the graft. The suture ends of the graft are shuttled up the tibial tunnel, across the joint, and the button is flipped against the femoral cortex. The graft is “shucked” to confirm seating of the button against cortex that can be easily felt. The free ends of the femoral TightRope are then tensioned to draw the graft up into the tunnels, docking the femoral end in the femoral socket. The knee is brought into full extension and the tibial TightRope ABS suture is tensioned against the button for tibial cortical fixation. In 6-strand constructs, the free Ethibond sutures are tied over the TightRope button. In this way we have suspensory fixation at either end, allowing each tunnel aperture to be completely filled with graft, and solid cortical fixation at both femur and tibia.
Discussion
Cadaveric analysis has shown a linear correlation between maximum load to failure and graft cross-sectional area.9 This finding has been corroborated in several clinical studies.2, 10, 11, 12 To obtain the better possible rates of graft survival in hamstring autograft ACL surgery, a minimum graft diameter of 8.0 or 8.5 mm is mandatory depending on the study. Standard hamstring preparation techniques result in a majority of patients having graft diameters below this threshold, and allow little scope to alter the diameter during the case.
The primary advantage (Tables 1 and 2) of this technique is that it allows the surgeon to use his or her standard harvest technique and make modifications to the use of ST and GT to fine tune graft diameter as required. It results in sufficient graft diameters in all cases using a simple workflow (Fig 1), using only autograft tissue. This technique allows for all strands of the graft to be suspended over solid cortical fixation. This has all the advantages of suspensory fixation (no graft damage by interference screw insertion, the center of the drilled tunnel being the center of the actual graft, circumferential apposition between the graft and bone) with the added advantage of adjustable suspensory fixation allowing retensioning after intraoperative knee cycling to obtain optimal time zero tension. It can be used either as an all-inside technique, or with a standard complete tibial tunnel.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Aim for a graft diameter that matches the size and activity demands of the patient. Harvest the ST first and measure its quadrupled diameter. If needed, the GT can then be harvested and added. | Do not make the graft longer than 70 mm. Trim the harvested ST tendon to 27 cm. A longer graft may become proud on the tibial end making it necessary to change from adjustable suspensory fixation to a post. It is more common to have a graft that is too long than one that is too short. |
| Cerclage sutures at both ends of the graft increase strength, and allow for improved tubularization and graft passage. | Trim the GT graft to 15 cm if you are using it 2 stranded (most of the cases) to avoid proud grafts coming off the tibial tunnel and interfering with suspensory fixation in the tibia. |
| Compression tubes can be used for enhanced tubularization and graft downsizing for easier passage. In the absence of formal compression tubes, the sizing blocks or tubes can be used for this purpose. | |
| When using the full tibial tunnel technique the TightRope RT loop can be initially lengthened to allow passage and flipping of the RT button on the femur before engagement of the graft in the tibial tunnel. This allows for a more controlled perception of button passage and seating on the femoral cortex and minimizes the risk of interposed soft tissue beneath the button. | |
| Perform final tensioning in full extension. With a larger graft and the cortical fixation the construct is very rigid. Tensioning in any degree of flexion is more likely to result in fixed flexion. Any retensioning after cycling the knee should only be performed in full extension. |
GT, gracilis tendon; ST, semitendinosus tendon.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Consistently larger grafts than using the 4-strand ST-G technique. Ability to alter the graft diameter by the addition of GT in either a double or quadruple fashion as required. Control of graft length (by the quadruple or triple graft technique). Adjustable suspensory fixation allowing for retensioning after cycling. Advantages of suspensory fixation (no graft damage by screw, circumferential apposition of graft to bone, control of center of the graft not just center of the tunnel). Can be used for all-inside or standard tibial tunnel techniques. All-inside allows for less bone removal. Utility in pediatric cases—bigger grafts from smaller tendons, absence of intraosseous fixation, all-inside technique for physeal sparing. |
Necessarily needs suspensory fixation—not suitable for interference screw fixation. |
GT, gracilis tendon; ST-G, semitendinosus-gracilis.
Other techniques have been described to address insufficient graft size; Calvo et al.1 described the use of a 5-strand technique with satisfactory results in terms of increased average graft diameter; however, they still report the presence of 8-mm grafts in their study. Allograft augmentation techniques to obtain a hybrid graft of increased graft diameter have also been described. A retrospective study by Burrus et al.13 described a failure rate of 13.8% for patients with ACL reconstructions with a hybrid graft versus 3.4% for patients reconstructed only with autograft. More recently, Darnley et al.14 in another study reported a 18.5% revision rate in hybrid grafts versus a 7.4% revision rate in hamstring autografts. These reported relatively higher re-rupture rates for hybrid constructs are concerning particularly in young and active patients.
The limitation of this technique includes the necessary use of suspensory fixation on both the femoral and tibial sides because the length of the grafts does not allow the use of intratunnel fixation (e.g. interferential screws). Suspensory fixation used both in femur and in tibia had shown excellent results in terms of graft maturation, tunnel integration, and tunnel widening.15 Concerns may exist with graft length. This concern is offset by the option of tripling instead of quadrupling the ST if needed for extra length. However, in their basic science articles, Miller et al.16 measured the intra-articular length of the ACL in cadaveric knees finding an average intra-articular graft length of 23.56 mm (standard deviation 0.98 mm) and Qi et al.7 demonstrated that only 15 mm of graft is needed in the tunnels to ensure the histologic maturity and biomechanical strength of the tendon-bone junction. Taking these data into our clinical setting means that even with a 6-cm total graft length (obtained from a 23-cm harvest) the minimum of 15-mm graft in both tunnels will be assured.
In conclusion, we believe that our customized approach to prepare a hamstring autograft is a valid option when a surgeon wants to obtain grafts of diameter larger than 8.5 mm on a regular basis using a standard harvest of autograft tissue and a simple workflow. More important than absolute graft size is the ability to obtain a graft dimension that is appropriate for each individual based on his or her size and demands. This technique allows for the construction of a 4-, 5-, 6-, or 8-strand graft as needed to alter length and diameter for each individual patient with the same graft harvest. We aim to perform comparative studies to validate its outcomes.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.F. receives consultancy fees, royalties, and payment for development of educational presentations from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Preparation of a 4-strand ST graft using the Graftlink technique. The video shows in detail technical aspects needed to perform a correct graft preparation, with the final result ending in a graft larger than 8.5 mm.
References
- 1.Calvo R., Figueroa D., Figueroa F. Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: Clinical outcomes with a minimum 2-year follow-up. Arthroscopy. 2017;33:1007–1013. doi: 10.1016/j.arthro.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 2.Magnussen R.A., Lawrence J.T., West R.L., Toth A.P., Taylor D.C., Garrett W.E. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 3.Conte E.J., Hyatt A.E., Gatt C.J., Jr., Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882–890. doi: 10.1016/j.arthro.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 4.Ho S.W., Tan T.J., Lee K.T. Role of anthropometric data in the prediction of 4-stranded hamstring graft size in anterior cruciate ligament reconstruction. Acta Orthop Belg. 2016;82:72–77. [PubMed] [Google Scholar]
- 5.Lavery K.P., Rasmussen J.F., Dhawan A. Five-strand hamstring autograft for anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3:e423–e426. doi: 10.1016/j.eats.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee R.J., Ganley T.J. The 5-strand hamstring graft in anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3:e627–e631. doi: 10.1016/j.eats.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qi L., Chang C., Jian L., Xin T., Gang Z. Effect of varying the length of soft-tissue grafts in the tibial tunnel in a canine anterior cruciate ligament reconstruction model. Arthroscopy. 2011;27:825–833. doi: 10.1016/j.arthro.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 8.Williams R.J., III, Hyman J., Petrigliano F., Rozental T., Wickiewicz T.L. Anterior cruciate ligament reconstruction with a four-strand hamstring tendon autograft. Surgical technique. J Bone Joint Surg Am. 2005;87(Suppl 1 pt 1):51–66. doi: 10.2106/JBJS.D.02805. [DOI] [PubMed] [Google Scholar]
- 9.Hamner D.L., Brown C.H., Jr., Steiner M.E., Hecker A.T., Hayes W.C. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: Biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81:549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Mariscalco M.W., Flanigan D.C., Mitchell J. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29:1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park S.Y., Oh H., Park S., Lee J.H., Lee S.H., Yoon K.H. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1111–1118. doi: 10.1007/s00167-012-2085-4. [DOI] [PubMed] [Google Scholar]
- 12.Kamien P.M., Hydrick J.M., Replogle W.H., Go L.T., Barrett G.R. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1808–1812. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 13.Burrus M.T., Werner B.C., Crow A.J. Increased failure rates after anterior cruciate ligament reconstruction with soft-tissue autograft-allograft hybrid grafts. Arthroscopy. 2015;31:2342–2351. doi: 10.1016/j.arthro.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Darnley J.E., Léger-St-Jean B., Pedroza A.D., Flanigan D.C., Kaeding C.C., Magnussen R.A. Anterior cruciate ligament reconstruction using a combination of autograft and allograft tendon: A MOON Cohort Study. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116662249. 2325967116662249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colombet P., Graveleau N., Jambou S. Incorporation of hamstring grafts within the tibial tunnel after anterior cruciate ligament reconstruction: Magnetic resonance imaging of suspensory fixation versus interference screws. Am J Sports Med. 2016;44:2838–2845. doi: 10.1177/0363546516656181. [DOI] [PubMed] [Google Scholar]
- 16.Miller M.D., Olszewski A.D. Cruciate ligament graft intra-articular distances. Arthroscopy. 1997;13:291–295. doi: 10.1016/s0749-8063(97)90023-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preparation of a 4-strand ST graft using the Graftlink technique. The video shows in detail technical aspects needed to perform a correct graft preparation, with the final result ending in a graft larger than 8.5 mm.