Abstract
A subscapularis complete tear presents its own challenges in management. The glenohumeral biomechanics and force couple are reliant on a competent and functioning subscapularis muscle. An irreparable subscapularis makes those same challenges even more difficult to address. Traditionally, this problem has been addressed with tendon transfers, including pectoralis major or latissimus dorsi. These techniques can alter the ideal biomechanics of the shoulder and have high rates or failure. Iliotibial autograft or tibialis anterior have also been wrought with high failure rates. Recently, the superior capsular reconstruction has been described for irreparable tears of the supraspinatus and infraspinatus. Theoretically, this procedure can act as a check rein against subluxation, and may serve to reconnect the force couples of the rotator cuff. Anterior escape may represent a similar challenge when the irreparable rotator cuff tendon is the subscapularis. To address this, we describe an open anterior capsule reconstruction technique with an acellular dermal graft. We theorize that this procedure may serve in a similar capacity to its superior capsular counterpart.
Glenohumeral biomechanics and joint stability depend on a functional subscapularis muscle (SSC).1, 2 Following shoulder arthroplasty, subscapularis failure can be disabling and even lead to conversion to a reverse arthroplasty.3, 4
Historically, surgical approaches to the irreparable SSC relied on nonanatomic approaches, such as pectoralis major or latissimus dorsi tendon transfers. These procedures may lead, however, to altered biomechanics and a high retear rate and complications, including nerve injuries.5, 6, 7, 8
Other attempts to address the irreparable SSC include allograft options to address anterior instability. These included augmented repair with the tibialis anterior or iliotibial band, though these techniques have also shown a high failure rate.9, 10, 11
Recently, superior capsule reconstruction (SCR) has proven to be a viable option in the setting of irreparable supraspinatus and/or infraspinatus tears. Originally described with autograft tensor fascia lata, more recently, this technique has addressed the deficiency with human dermal allograft.12 This patch may provide a static stabilizing effect, as well as a scaffold for rotator cuff reincorporation.13 The early results of the SCR are promising for superior cuff pathology. We theorize that the same effect can be applied to anterior rotator cuff deficiency with a similar approach.
The purpose of this article is to describe in detail the technique of open anterior capsule reconstruction with an acellular dermal allograft. Of note, we are in the process of publishing our arthroscopic anterior capsule reconstruction (ACR) as well. In our experience, the arthroscopic ACR is attempted as a primary surgery or if we feel as though subscapularis repair is possible. Our open approach to ACR is employed for revision, open surgery, or when the subscapularis is deemed irreparable from clinical and radiographic analysis.
Surgical Technique
Preparation and Workup
The patient evaluation is begun with a thorough history and physical, as with all patients in our practice. History given by patients with subscapularis pathology may include prior open or arthroscopic surgery of the shoulder, arthroplasty (or other procedures requiring subscapularis take-down), weakness with internal rotation, and/or history of repetitive anterior dislocations. The history may lead one to suspect subscapularis pathology, and this can be further elucidated during the physical examination portion of the encounter. Pseudoparalysis or anterior superior escape with tight posterior capsule may increase suspicion for massive irreparable subscapularis tears.
On physical examination, one must pay close attention to increased side-to-side comparison of passive external rotation measurements, a positive lift-off test, belly press, and bear hug test. The patient may display a positive internal rotation lag sign, in which the patient is unable to actively hold the arm/humerus in maximum internal rotation. Positive findings on physical examination lead to advanced imaging modalities, such as magnetic resonance imaging, or computed tomography arthrogram versus ultrasonography in the case of pre-existing arthroplasty. The advanced images should be critically reviewed looking for presence of subscapularis tear, size of tear, degree of retraction, fatty infiltration of muscle, muscle atrophy, and associated pathology.
The patient should be counseled on the risks and benefits of operative interventions, to include repair versus anterior capsule reconstruction, especially in the physiologically young. Outside the scope of this paper, but certainly for the elderly, low-demand patients, a reverse arthroplasty is an option to consider. The convalescence period should also be discussed. As always, the possibility of nonoperative management should also be offered to the patient.
Starting the Case
The patient is identified in the preoperative holding room and the operative extremity is marked. We also prefer the use of regional interscalene nerve block for shoulder procedures.
Our preference for open shoulder surgery is for beach chair position. We use an attachment for the top of the standard operating table that provides a head holder and ensures that the operative extremity's scapula is free from contact with the table. These attachments are available from different manufacturers and should be placed on the bed before the patient is moved. After induction of general endotracheal anesthesia, the patient is positioned on the table, and care is taken to ensure the endotracheal tube is on the contralateral side of the mouth from the operative field. The head and neck are secured and positioned in a manner that provides neutral neck flexion/extension and lateral bending as well as rotation. It is sometimes necessary to adjust the head/neck position until after the patient is sat up. The hips are flexed and knees flexed prior to sitting up. Next, the patient's back is elevated to about 45° into the beach chair position.
A pneumatic arm holder is used to hold the arm and allow freedom of movement, during the case. The operative extremity is prepped and draped in the normal sterile fashion. An ideal field should include the sternoclavicular joint medially up to the base of the neck, and posteriorly down the medial border of the scapula and around the axilla, and finally anteriorly below the nipple to rejoin the drape at the sternoclavicular joint.
Our approach is through a standard deltopectoral approach. The incision should be carried from just proximal medial to the coracoid tip and drop inferolaterally toward the deltoid tuberosity at a 45° angle. The incision should be between 8 and 10 cm and can certainly be extended if needed during the case. The interval is identified by the cephalic vein and its associated fat stripe. The vein is retracted medial or lateral, whichever provides the easiest, most tension-free excursion. We recommend working superiorly initially, just distal to the coracoid, and then bluntly divide the interval between pectoralis and deltoid, as seen in the technique video (Video 1). The pectoralis major tendon is followed to its humeral attachment, and then the upper 1 cm of tendon is released to assist with exposure. Next a Cobb elevator is used to free up the subdeltoid space and its associated adhesions, as described in the attached video; note the identification of the coracoacromial ligament and the use of the Cobb to free up the subdeltoid space, by traveling lateral from the subacromial space. A brown retractor is placed under the deltoid and above the rotator cuff. Medially a Kolbel self-retainer can be used or a Gelpi self-retainer to keep the pectoralis out of view. The clavipectoral fascia is often scarred in this area, and care is taken to clear this tissue lateral to the conjoined tendon. Often, the humeral head is visible because of the torn subscapularis. Because of the high incidence of concomitant biceps pathology, we normally tenotomize the long head of the biceps and tenodese this to the pectoralis tendon at its insertion into the humerus, as shown in the technique video. The residual stump is removed at the level of the superior labrum and discarded. A Fukuda retractor is placed into the glenohumeral joint and used to move the humeral head inferior and posterior, out of the working field. This can be useful when removing the residual biceps tendon, but should be removed when measuring for and tensioning the anterior capsule graft. Once the subscapularis is visualized, efforts should be made to perform a 360° release of the residual tendon and attempt primary repair back to the lesser tuberosity. If this is not possible, we begin preparation for the anterior capsular reconstruction.
Subscapularis Bed Preparation
In the presence of a large, irreparable subscapularis tear, the exposure to the anterior glenoid is critical for the anterior capsular reconstruction. First, we prepare the anterior glenoid for placement of our medialmost suture anchors. Our preference is for 3 anchors along the glenoid rim, medial enough to keep the anchor and necessary taps out of the glenoid cartilage. The superior most is placed around 1 o'clock on a right shoulder, another at 3 o'clock and one at 5 o'clock. A motorized burr is used to gently decorticate the future contact area of the acellular dermal graft to the bony glenoid.
Graft Sizing and Preparation
Our choice for reconstruction material is the ArthroFlex decellularized dermal allograft (Arthrex, Naples, FL). Our standard size is 40 mm × 70 mm × 3 mm. The allograft must be cut down to a workable size. A malleable rule or paper ruler should be used to measure the 4 dimensions of the proposed graft. The Fukuda should be removed when sizing and tensioning the graft. We measure the superior to inferior dimension from the 1-o'clock to 5-o'clock position on the glenoid and use this same number for the lateral side, effectively making a rectangular surface for healing. We add 5 mm to this number to allow placement of suture with a cuff of tissue to prevent cutout of the stitch, and to provide extra surface area for healing. When measuring the medial to lateral dimension, we ensure that the glenohumeral joint is reduced, and the humerus is in 30° of abduction, 30° of external rotation, and neutral forward elevation. This will allow for proper tensioning of the anterior capsule. Once the arm position is satisfactory, we measure from the proposed medial anchors, laterally to the lesser tuberosity, and add 15 mm to the number. The addition of 15 mm will allow for a double-row fixation laterally, and excess graft is easily removed with scalpel. The finished, cut graft should be rectangular or trapezoidal in shape.
Graft Insertion and Medial (Glenoid) Fixation
Next, we place three 3.0-mm Arthrex SutureTaks sequentially at the 1-, 3-, and 5-o'clock positions along the glenoid, as seen in the technique video. These are single-loaded anchors with No. 2 FiberWire (Arthrex). The inter-anchor distance should be measured and the corresponding distance marked on the medial side of the graft to provide a template. We use an antegrade rotator cuff suture passer to pass the limbs of the previously placed single-loaded SutureTaks, in a horizontal mattress fashion. These are tied securely and the free ends of the suture are cut, as seen in Figures 1 and 2. The medial graft is now securely fixed to the glenoid.
Fig 1.
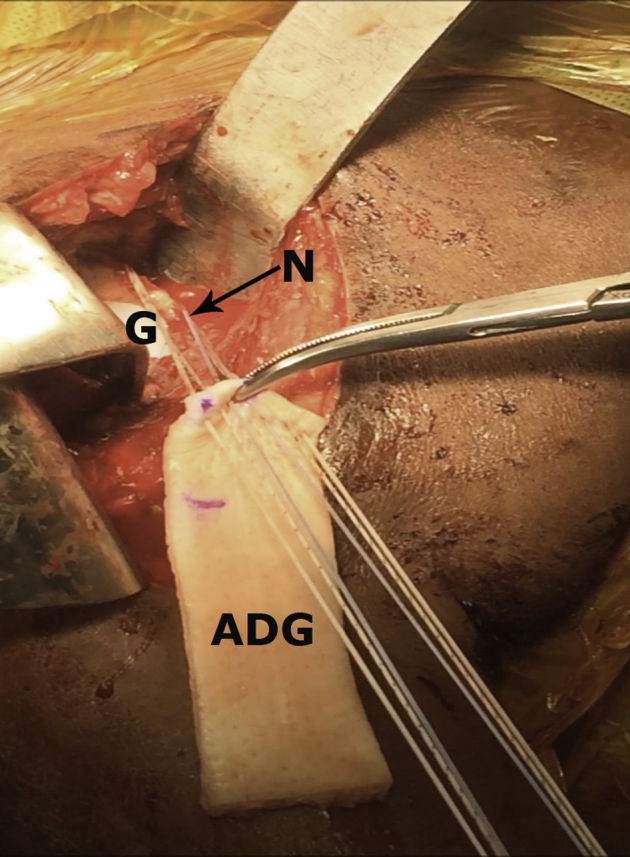
The patient is in the beach chair position. Medial is right and lateral is to the left. Initial part of acellular dermal graft (ADG) implantation to the glenoid neck (N). Glenoid (G) is exposed, glenoid neck (N) is biologically prepared. Sutures have been passed in a horizontal mattress fashion.
Fig 2.
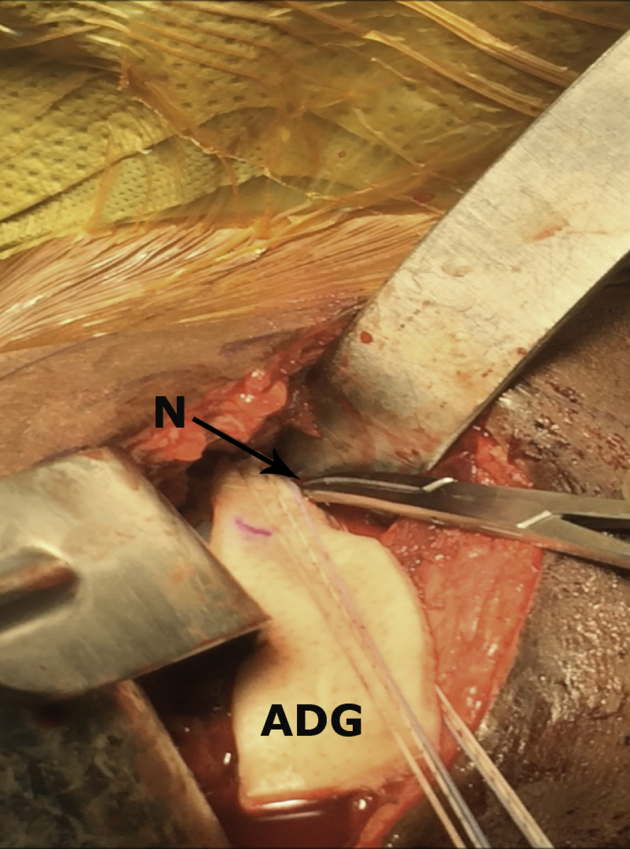
The patient is in the beach chair position. Medial is right and lateral is to the left. Acellular dermal graft (ADG) positioning at the glenoid neck (N). The hemostat is used to hold graft in place while suture limbs are being tied, first to the glenoid side.
Lateral (Humerus) Fixation
For the lateral fixation, we ensure the glenohumeral joint is reduced and centered and the arm is in neutral forward elevation with about 30° of abduction and 30° of external rotation. Again, the lesser tuberosity is gently decorticated. The patch is then brought over the lesser tuberosity to provide the best anatomic coverage in the superior to inferior aspect. We then place two 4.75-mm SwiveLock (Arthrex) anchors into the native lesser tuberosity, loaded with a FiberTape (Arthrex) each. Using the antegrade suture passer, the FiberTapes are passed through the allograft, as seen in the accompanying video. The FiberTape welds are then cut to provide 4 free limbs of suture. At this juncture, we complete a knotless transosseous equivalent double row fixation laterally. The lateral aspect of the lesser tuberosity is located, and biologically prepared. At this time if there is excess graft it may be sharply excised (Figs 3 and 4). Next, one limb from each lesser tuberosity anchor is placed into a lateral-row SwiveLock, 4.75-mm or larger if there is concern of bone quality. This step is executed for the superior and inferior lateral-row anchor. Care is taken to adequately tension the limbs as the anchor is deployed to provide even contact pressure of the graft to bone. Excess suture limbs are cut (Fig 5). As outlined in Table 1, much of the success of this technique hinges on proper sizing and fixation of the graft.
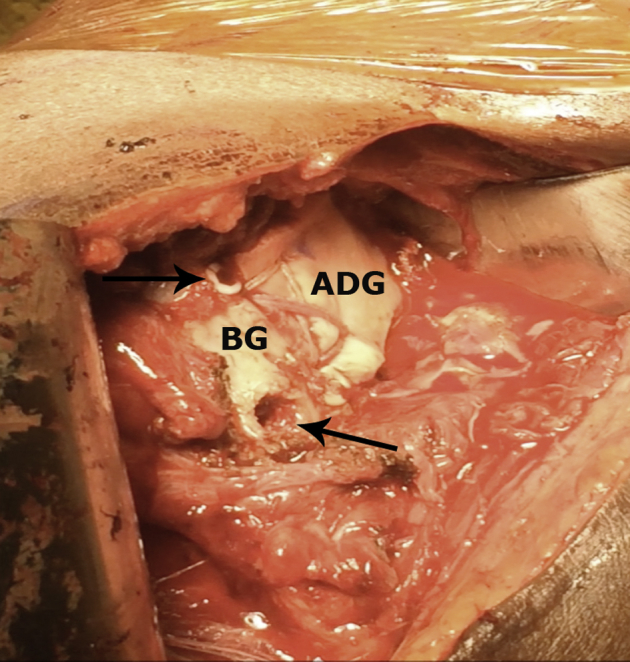
Fig 3.
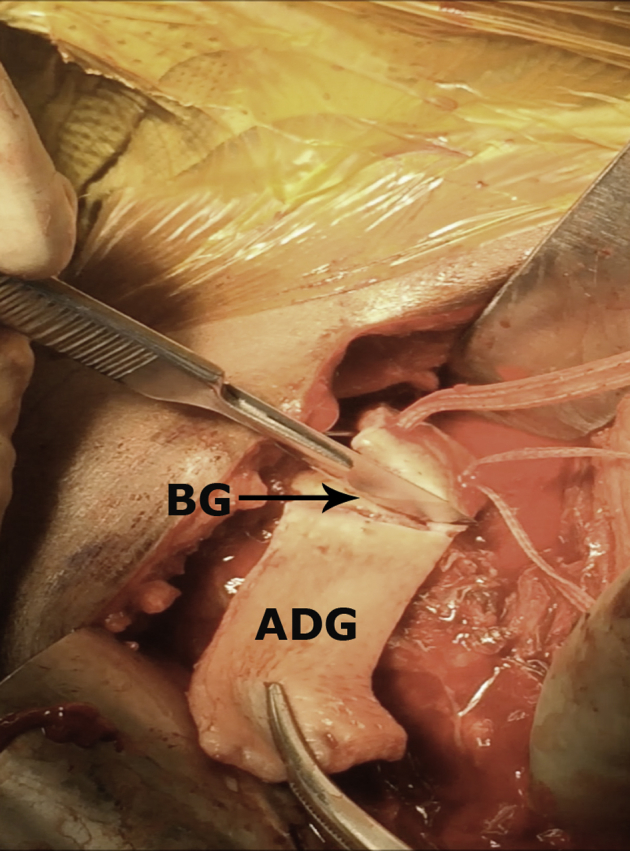
The patient is in the beach chair position. Medial is right and lateral is to the left After medial fixation, the acellular dermal graft (ADG) is cut down to its appropriate size before its lateral fixation to the bicipital groove (BG). Prior to cutting excess graft, ensure that the arm is in 30° of abduction and 30° of external rotation to ensure appropriate tension.
Fig 4.
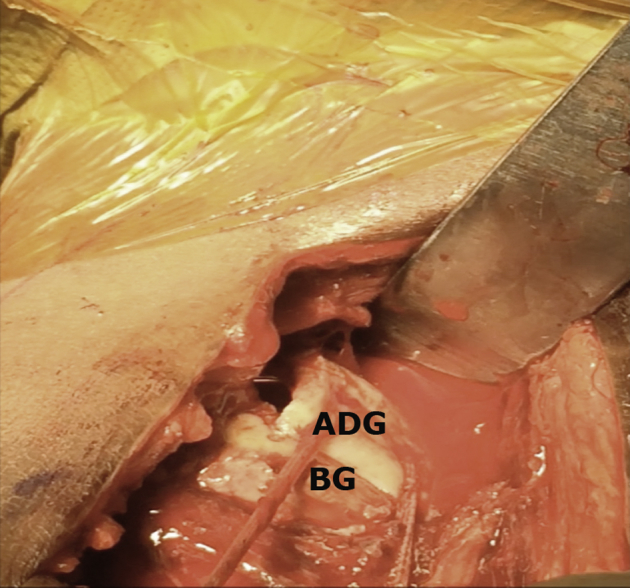
The patient is in the beach chair position. Medial is right and lateral is to the left Acellular dermal graft (ADG) is prepared for the double-row lateral fixation. The medial row has been secured and FiberTapes are passed through the graft and dragged laterally, in preparation of knotless lateral row fixation in the bicipital groove (BG). The arm is maintained in 30° of both abduction and external rotation.
Fig 5.
The patient is in the beach chair position. Medial is right and lateral is to the left. Final view of anterior capsule reconstruction (ACR) with an acellular dermal graft (ADG). Arrows are pointing lateral anchors used for the double-row fixation. Note with the transosseous equivalent lateral fixation that there is excellent graft compression to the previously prepared bone bed along the lesser tuberosity. (BG, bicipital groove.)
Table 1.
Pearls and Pitfalls of Open Anterior Capsule Reconstruction
| Pearls | Pitfalls |
|---|---|
| 1. Ensure adequate exposure of anterior glenoid and lesser tuberosity | 1. Accepting poor glenoid exposure |
| 2. Fixation of graft done with arm in 30° of abduction and 30° external rotation | 2. Securing the graft with arm in abduction or internal rotation |
| 3. Leave extra length in allograft to be trimmed out once fixed in vivo | 3. Failure to template anchor spacing, before passing sutures through graft |
| 4. Measure anchor spacing and mark allograft to corresponding points for suture passing | 4. Failure to recognize concomitant rotator cuff pathology |
Final Inspection, Closure, and Postoperative Rehabilitation
The arm may now be ranged through gentle motion while inspecting the graft for adequate fixation and coverage (Video 1). For closure, we begin with placing figure-of-8 stitches with No. 2 permanent suture in the inferior graft edge to any remaining native capsule. The same is then done superior along the lateral half of the graft to close the re-created rotator interval, sewing superior anterior capsule graft to the anterior edge of the supraspinatus tendon. Medially if any residual subscapularis tendon exists, it may be sewn to the graft with No. 2 permanent suture, to provide a biologic bridge such that when the subscapularis is fired, it will pull on the graft and may resemble normal function. The wound is copiously irrigated and the deltopectoral interval is reapproximated with a few absorbable sutures. Subcutaneous layers and skin are closed with absorbable suture, and a postoperative sling with abduction pillow are applied. Postoperatively, the patient is treated with a typical subscapularis tendon repair protocol, shoulder immobilization in a sling with external rotation limited to 30°. Active elbow, wrist, and hand exercises are allowed. Gentle passive glenohumeral joint motions are also allowed. After 6 weeks, motion is progressed and strengthening is allowed no sooner than 12 weeks postoperatively. Typical return to full activity with symmetric motion and strength is approximately 6 months.
Discussion
The biomechanics of the glenohumeral joint are undoubtedly adversely affected by the irreparable subscapularis tear.1, 2, 7, 9, 14, 15 The presence of a functional subscapularis is paramount for anterior shoulder stability in both the native shoulder and arguably more important in shoulder arthroplasty. Thus, the loss of a functional subscapularis can compromise stability.3, 4, 15, 16, 17
Jackson et al.18 reported a rerupture rate of 47% after total shoulder arthroplasty.17 Though some subscapularis failures, following surgery, are not symptomatic, revision surgery is still required in many instances of retear.3, 4, 19 To date, muscle transfer is the most common treatment for this subscapularis retear.7, 15, 17, 20, 21, 22
The pectoralis major tendon transfer is often suggested as a reasonable option for irreparable SSC tear, and transfers of trapezius muscle, latissimus dorsi, and pectoralis minor are also described. Although functional improvement following these transfers is reasonable, the joint kinematics are altered and, further, they are dependent on a functional rotator cuff to be successful.
Shin et al., in a recent systematic review, looked at the range of motion after a pectoralis major transfer. They noted significant changes in forward elevation (from 102.3° to 130.3°) and in abduction (from 108.1° to 135.4°). However, significant reduction in external rotation (from 55.6° to 44.7°). Only 1 study reports change in internal reduction, which showed no significant difference from 77° to 78°. Additionally, each of these procedures alters native anatomy and biomechanics, and the overall failure rate may reach close to 13%.5, 6, 7, 15, 17, 21, 22, 23, 24
These transfer procedures do put nerves at risk. Ruiz-Iban et al. reported that in 21% of specimens, there was not enough space between coracoid process and musculocutaneous nerve branches for the pectoralis major transfer. Contact between transferred tendon and nerve structures was found in close to half.8 The axillary nerve is also at risk with muscle transfers; Elhassan et al.5 reported impingement between nerve and tendons when combined latissimus dorsi and teres major transfer was performed on cadavers.
Furthermore, Lee et al.25 reported that harvesting of latissimus dorsi tendon results in patient-reported discomfort in 41% of cases, and objectively evaluated shoulder disability is described in 20% of cases. Moreover, incidence of iatrogenic permanent axillary and musculocutaneous nerves dysfunction is also reported in the literature.7
Application of different tissue augments and have also been described.26, 27 Some authors recommended not using allograft for a treatment of massive rotator cuff lesions, others report significant outcome improvement when used.28, 29 Snyder et al. have shown good integration and minimal immunologic risk with free allograft. This graft has also no donor site morbidity and is accessible, durable, and easy to prepare.12, 30 Early promising results of SCR for irreparable rotator cuff tears have prompted us to adapt this technique for the anterior capsule reconstruction, which is discussed here. Table 2 lists the pros and cons of our open approach to the anterior capsule reconstruction. We have employed this technique for irreparable SSC in the setting of chronic lesions, revision instability cases, as well as in patients with symptomatic subscapularis insufficiency after total shoulder replacement.
Table 2.
Advantages and Disadvantages of Open Anterior Capsular Reconstruction
| Advantages | Disadvantages |
|---|---|
| 1. Preservation of bone stock | 1. Limited case numbers |
| 2. Future arthroplasty options are still viable | 2. No long-term outcomes data |
| 3. Outpatient procedure | 3. Use of allograft is not suitable for all patients |
| 4. Concomitant pathology addressed via same approach | 4. Slower progression of therapy vs reverse total shoulder |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.M.T. is a paid consultant for Arthrex, DePuy, and Mitek. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for an anterior capsule reconstruction for irreparable subscapularis tears. Patient is positioned in a beach chair position. Approach is through a standard deltopectoral approach. Working superiorly initially, start just distal to the coracoid, and then bluntly divide the interval between the pectoralis and deltoid. The pectoralis major tendon is followed to its humeral attachment, and then the upper 1 cm of tendon is released to assist with exposure. Next a Cobb elevator is used to free up the subdeltoid space and its associated adhesions. A Fukuda retractor is placed into the glenohumeral joint and used to move the humeral head inferior and posterior, out of the working field. Once the subscapularis is visualized, efforts should be made to perform a 360° release of the residual tendon and attempt primary repair back to the lesser tuberosity. We prepare the anterior glenoid for placement of our medial-most suture anchors. Our preference is for 3 anchors along the glenoid rim, medial enough to keep the anchor and necessary taps out of the glenoid cartilage. The superior-most is placed around 1 o'clock on a right shoulder, another at 3 o'clock and one at 5 o'clock. The graft is the ArthroFlex decellularized dermal allograft (Arthrex). A malleable rule or paper ruler should be used to measure the 4 dimensions of the proposed graft. We measure the superior to inferior dimension from the 1-o'clock to 5-o'clock position on the glenoid and use this same number for the lateral side, effectively making a rectangular surface for healing. We add 5 mm to this number to allow placement of suture with a cuff of tissue to prevent cutout of the stitch, and to provide extra surface area for healing. When measuring the medial to lateral dimension, we ensure the glenohumeral joint is reduced and that the humerus is in 30° of abduction, 30° of external rotation, and neutral forward elevation. Once the arm position is satisfactory, we measure from the proposed medial anchors, laterally to the lesser tuberosity, and add 15 mm to the number. The addition of 15 mm will allow for a double-row fixation laterally and excess graft is easily removed with a scalpel. The finished, cut graft should be rectangular or trapezoidal in shape. Three 3.0-mm Arthrex SutureTaks sequentially at the 1-, 3-, and 5-o'clock positions along the glenoid. These are single-loaded anchors with No. 2 FiberWire (Arthrex), an antegrade rotator cuff suture passer to pass the limbs of the previously placed single-loaded SutureTaks, in a horizontal mattress fashion. These are tied securely and the free ends of the suture are cut. For lateral fixation, the glenohumeral joint is reduced and centered, and arm is in neutral forward elevation with about 30° of abduction and 30° of external rotation. Again, the lesser tuberosity is gently decorticated. The patch is then brought over the lesser tuberosity to provide the best anatomic coverage in the superior to inferior aspect. We then place and secure two 4.75-mm SwiveLock (Arthrex) anchors into the native lesser tuberosity, loaded with a FiberTape (Arthrex) each. Next, 1 limb from each lesser tuberosity anchor is placed into a lateral-row SwiveLock, 4.75 mm or larger if there is concern of bone quality. This step is executed for the superior and inferior lateral row anchor. The arm may now be ranged through gentle motion while inspecting the graft for adequate fixation and coverage. All incisions are then closed.
References
- 1.Burkhart S.S. Arthroscopic treatment of massive rotator cuff tears: Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;267:45–56. [PubMed] [Google Scholar]
- 2.Ticker J.B., Burkhart S.S. Why repair the subscapularis? A logical rationale. Arthroscopy. 2011;27:1123–1128. doi: 10.1016/j.arthro.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Ives E.P., Nazarian L.N., Parker L., Garrigues G.E., Williams G.R. Subscapularis tendon tears: A common sonographic finding in symptomatic postarthroplasty shoulders. J Clin Ultrasound. 2013;41:129–133. doi: 10.1002/jcu.21980. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong A., Lashgari C., Teefey S., Menendez J., Yamaguchi K., Galatz L.M. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2006;15:541–548. doi: 10.1016/j.jse.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Elhassan B., Christensen T.J., Wagner E.R. Feasibility of latissimus and teres major transfer to reconstruct irreparable subscapularis tendon tear: An anatomic study. J Shoulder Elbow Surg. 2014;23:492–499. doi: 10.1016/j.jse.2013.07.046. [DOI] [PubMed] [Google Scholar]
- 6.Gavriilidis I., Kircher J., Magosch P., Lichtenberg S., Habermeyer P. Pectoralis major transfer for the treatment of irreparable anterosuperior rotator cuff tears. Int Orthop. 2010;34:689–694. doi: 10.1007/s00264-009-0799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shin J.J., Saccomanno M.F., Cole B.J., Romeo A.A., Nicholson G.P., Verma N.N. Pectoralis major transfer for treatment of irreparable subscapularis tear: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:1–10. doi: 10.1007/s00167-014-3229-5. [DOI] [PubMed] [Google Scholar]
- 8.Ruiz-Ibán M.Á., Murillo-González J.A., Díaz-Heredia J., Avila-Lafuente J.L., Cuéllar R. Pectoralis major transfer for subscapular deficiency: Anatomical study of the relationship between the transferred muscle and the musculocutaneous nerve. Knee Surg Sports Traumatol Arthrosc. 2013;21:2177–2183. doi: 10.1007/s00167-013-2432-0. [DOI] [PubMed] [Google Scholar]
- 9.Gerber C., Hersche O., Farron A. Isolated rupture of the subscapularis tendon. Results of operative repair. J Bone Joint Surg. 1996;78:1015–1023. doi: 10.2106/00004623-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Iannotti J.P., Antoniou J., Williams G.R., Ramsey M.L. Iliotibial band reconstruction for treatment of glenohumeral instability associated with irreparable capsular deficiency. J Shoulder Elbow Surg. 2002;11:618–623. doi: 10.1067/mse.2002.126763. [DOI] [PubMed] [Google Scholar]
- 11.Braun S., Horan M.P., Millett P.J. Open reconstruction of the anterior glenohumeral capsulolabral structures with tendon allograft in chronic shoulder instability. Oper Orthop Traumatol. 2011;23:29–36. doi: 10.1007/s00064-010-0011-9. [DOI] [PubMed] [Google Scholar]
- 12.Tokish J.M., Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4:e833–e839. doi: 10.1016/j.eats.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44:1423–1430. doi: 10.1177/0363546516631751. [DOI] [PubMed] [Google Scholar]
- 14.Osti L., Soldati F., Buono A.D., Buda M. Arthroscopic repair of the subscapularis tendon: Indications, limits and technical features. Muscles Ligaments Tendons J. 2013;3:213. [PMC free article] [PubMed] [Google Scholar]
- 15.Wirth M.A., Rockwood C.A. Operative treatment of irreparable rupture of the subscapularis. J Bone Joint Surg Am. 1997;79:722–731. doi: 10.2106/00004623-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Moeckel B.H., Altchek D.W., Warren R.F., Wickiewicz T.L., Dines D.M. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am. 1993;75:492–497. doi: 10.2106/00004623-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Elhassan B., Ozbaydar M., Massimini D., Diller D., Higgins L., Warner J.J. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis. J Bone Joint Surg Am. 2008;90:1059–1065. doi: 10.1302/0301-620X.90B8.20659. [DOI] [PubMed] [Google Scholar]
- 18.Jackson J.D., Cil A., Smith J., Steinmann S.P. Integrity and function of the subscapularis after total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:1085–1090. doi: 10.1016/j.jse.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Levy D.M., Abrams G.D., Harris J.D., Bach B.R., Jr., Nicholson G.P., Romeo A.A. Rotator cuff tears after total shoulder arthroplasty in primary osteoarthritis: A systematic review. Int J Shoulder Surg. 2016;10:78. doi: 10.4103/0973-6042.180720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Namdari S., Voleti P., Baldwin K., Glaser D., Huffman G.R. Latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Bone Joint Surg Am. 2012;94:891–898. doi: 10.2106/JBJS.K.00841. [DOI] [PubMed] [Google Scholar]
- 21.Nelson G.N., Namdari S., Galatz L., Keener J.D. Pectoralis major tendon transfer for irreparable subscapularis tears. J Shoulder Elbow Surg. 2014;23:909–918. doi: 10.1016/j.jse.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 22.Goutallier D., De Abreu L., Postel J.M., Le Guilloux P., Radier C., Zilber S. Is the trapezius transfer a useful treatment option for irreparable tears of the subscapularis? Orthop Traumatol Surg Res. 2011;97:719–725. doi: 10.1016/j.otsr.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 23.Konrad G.G., Sudkamp N.P., Kreuz P.C., Jolly J.T., McMahon P.J., Debski R.E. Pectoralis major tendon transfers above or underneath the conjoint tendon in subscapularis-deficient shoulders. J Bone Joint Surg Am. 2007;89:2477–2484. doi: 10.2106/JBJS.F.00811. [DOI] [PubMed] [Google Scholar]
- 24.Jost B., Puskas G.J., Lustenberger A., Gerber C. Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears. J Bone Joint Surg Am. 2003;85:1944–1951. doi: 10.2106/00004623-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Lee K.-T., Mun G.H. A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer. Plastic Reconstruct Surg. 2014;134:303–314. doi: 10.1097/PRS.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 26.Longo U.G., Lamberti A., Petrillo S., Maffulli N., Denaro V. Scaffolds in tendon tissue engineering. Stem Cells Int. 2012;2012:517165. doi: 10.1155/2012/517165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricchetti E.T., Aurora A., Iannotti J.P., Derwin K.A. Scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2012;21:251–265. doi: 10.1016/j.jse.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Moore D.R., Cain E.L., Schwartz M.L., Clancy W.G., Jr. Allograft reconstruction for massive, irreparable rotator cuff tears. Am J Sports Med. 2006;34:392–396. doi: 10.1177/0363546505281237. [DOI] [PubMed] [Google Scholar]
- 29.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 30.Snyder S.J., Arnoczky S.P., Bond J.L., Dopirak R. Histologic evaluation of a biopsy specimen obtained 3 months after rotator cuff augmentation with GraftJacket Matrix. Arthroscopy. 2009;25:329–333. doi: 10.1016/j.arthro.2008.05.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for an anterior capsule reconstruction for irreparable subscapularis tears. Patient is positioned in a beach chair position. Approach is through a standard deltopectoral approach. Working superiorly initially, start just distal to the coracoid, and then bluntly divide the interval between the pectoralis and deltoid. The pectoralis major tendon is followed to its humeral attachment, and then the upper 1 cm of tendon is released to assist with exposure. Next a Cobb elevator is used to free up the subdeltoid space and its associated adhesions. A Fukuda retractor is placed into the glenohumeral joint and used to move the humeral head inferior and posterior, out of the working field. Once the subscapularis is visualized, efforts should be made to perform a 360° release of the residual tendon and attempt primary repair back to the lesser tuberosity. We prepare the anterior glenoid for placement of our medial-most suture anchors. Our preference is for 3 anchors along the glenoid rim, medial enough to keep the anchor and necessary taps out of the glenoid cartilage. The superior-most is placed around 1 o'clock on a right shoulder, another at 3 o'clock and one at 5 o'clock. The graft is the ArthroFlex decellularized dermal allograft (Arthrex). A malleable rule or paper ruler should be used to measure the 4 dimensions of the proposed graft. We measure the superior to inferior dimension from the 1-o'clock to 5-o'clock position on the glenoid and use this same number for the lateral side, effectively making a rectangular surface for healing. We add 5 mm to this number to allow placement of suture with a cuff of tissue to prevent cutout of the stitch, and to provide extra surface area for healing. When measuring the medial to lateral dimension, we ensure the glenohumeral joint is reduced and that the humerus is in 30° of abduction, 30° of external rotation, and neutral forward elevation. Once the arm position is satisfactory, we measure from the proposed medial anchors, laterally to the lesser tuberosity, and add 15 mm to the number. The addition of 15 mm will allow for a double-row fixation laterally and excess graft is easily removed with a scalpel. The finished, cut graft should be rectangular or trapezoidal in shape. Three 3.0-mm Arthrex SutureTaks sequentially at the 1-, 3-, and 5-o'clock positions along the glenoid. These are single-loaded anchors with No. 2 FiberWire (Arthrex), an antegrade rotator cuff suture passer to pass the limbs of the previously placed single-loaded SutureTaks, in a horizontal mattress fashion. These are tied securely and the free ends of the suture are cut. For lateral fixation, the glenohumeral joint is reduced and centered, and arm is in neutral forward elevation with about 30° of abduction and 30° of external rotation. Again, the lesser tuberosity is gently decorticated. The patch is then brought over the lesser tuberosity to provide the best anatomic coverage in the superior to inferior aspect. We then place and secure two 4.75-mm SwiveLock (Arthrex) anchors into the native lesser tuberosity, loaded with a FiberTape (Arthrex) each. Next, 1 limb from each lesser tuberosity anchor is placed into a lateral-row SwiveLock, 4.75 mm or larger if there is concern of bone quality. This step is executed for the superior and inferior lateral row anchor. The arm may now be ranged through gentle motion while inspecting the graft for adequate fixation and coverage. All incisions are then closed.


