Abstract
Posterolateral corner injuries are a severe and often unrecognized pathology. Injuries to these structures are difficult to identify using magnetic resonance images. Physical examination tests including the dial test, frog-leg test, and varus stress test can be difficult to perform. In addition it is difficult to correctly evaluate the results in a multiligament injury setting. The correct diagnosis of this pathology is essential to determine the proper treatment and improve outcomes. Furthermore, failure to recognize this pathology is associated with a high risk of failure following isolated anterior cruciate ligament reconstructions. The purpose of this Technical Note is to present an alternative method for the evaluation of posterolateral corner injuries using radiographic images.
Posterolateral instability is a difficult pathology for any orthopaedic surgeon, even the most experienced in ligament surgery. The difficulty begins with proper diagnosis of which structures of the lateral complex are injured and need to be addressed with surgery. There are several physical examinations that can be used to aid in the correct diagnose, including the varus stress test, the external rotation test, the dial test, the frog-leg test, and the reverse pivot shift test.1, 2, 3, 4, 5, 6, 7, 8, 9 Despite the number of clinical tests, there is a lack of radiographic tests to aid in diagnosis.
While varus stress x-rays have been shown to be a reliable tool to aid in diagnosis of posterolateral corner injuries,10 they do not take into account the rotational instability associated with the insufficiency of some posterolateral corner structures. A radiographic test for rotational instability would be important as it could be performed in any office faster than magnetic resonance imaging (MRI) and with lower cost. However, as the radiographic test does not directly show the injury, this test needs to be reliable and reproducible, with easy interpretation and without excess intraevaluator variability in order to be really useful. If feasible, another advantage would be to help evaluate the efficacy of the treatment, comparing preoperative or pretreatment images with subsequent follow-up images. We believe our radiographic technique fits these criteria and can be used in association with a thorough physical examination, MRI, and varus stress x-rays to help fully characterize injuries to the posterolateral corner and guide treatment options. The purpose of this Technical Note is to present a radiographic test that can help further describe posterolateral corner injuries, particularly their rotational instability, in an objective and reproducible manner.
Technique
Patient Position
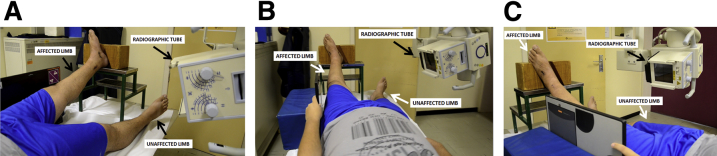
The patient is placed supine on the table (Video 1). The radiographic tube must be placed 1 m from the patient. The affected leg is raised 35 cm high with the heel placed in customized fixture in 15° of external rotation (Fig 1). The patient is asked to relax the inferior limb muscles, and the radiographic tube (Siemens) is placed in 15° of caudal inclination, with the radiographic film cassette (Siemens) over the table and perpendicular to the radiographic tube (Siemens); the image is then obtained. The same technique is applied for the unaffected side, keeping the leg at the exact same height (35 cm) with the same amount of external rotation (15°; Fig 2).
Fig 1.
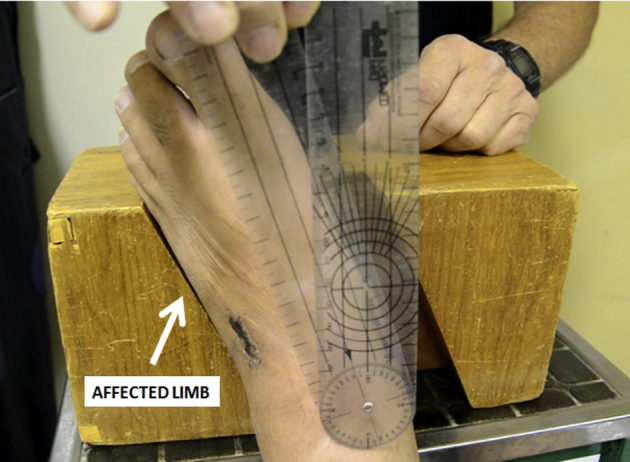
Posterolateral corner radiographic technique performed in a left limb. The patient is placed supine on the table. The affected limb is raised 35 cm and placed in a customized fixture with 15° of external rotation. A goniometer can be used to ensure the correct rotation of the limb.
Fig 2.
Radiographic technique performed in a left limb for the diagnosis of posterolateral corner injury. Once the affected limb is in the correct position, the radiographic tube is placed in 15° of caudal inclination, with the radiographic film cassette over the table and perpendicular to the radiographic tube. Parts A (Oblique left), B (parallel), and C (oblique right) all demonstrate proper setup for examination of the affected limb.
Radiographic Evaluation
Once the technique is performed in both limbs, the radiographic images are evaluated. The middle aspect of the femoral shaft is identified, and a longitudinal line is drawn following the longitudinal axis of the femur (Fig 3). Then a new line perpendicular to the first line is drawn at the distal aspect of the femoral condyles (Fig 4). A third line is drawn parallel to the tibial plateau as is usually done to evaluate the tibial slope (Fig 5). The angle created between the second and third lines is evaluated and recorded. The same steps are performed for both knees, and the difference between both sides is evaluated. Differences over 5° between both sides suggest injury. Advantages and disadvantages as well as pearls and pitfalls associated with the technique are summarized in Tables 1 and 2, respectively.
Fig 3.
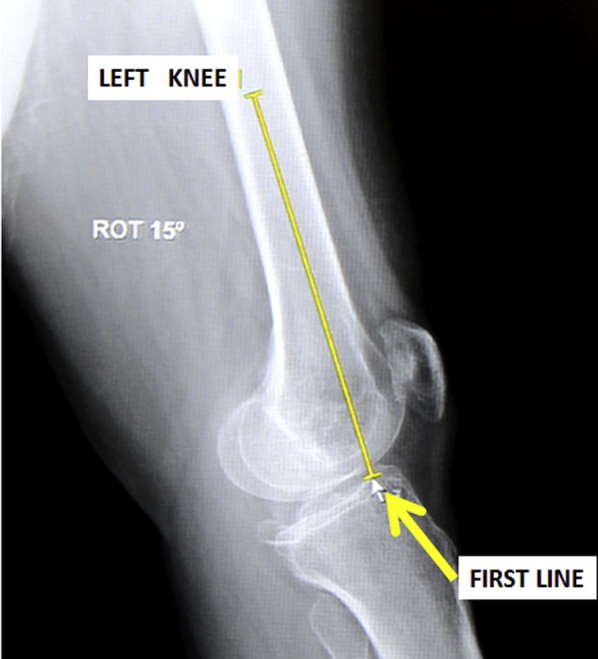
Once the radiographic images are obtained in both limbs, using the same technique, the measurement begins. The first line for the radiographic evaluation is performed in a left knee lateral radiograph. The middle aspect of the femoral shaft is identified, and a line is drawn until the joint line (yellow line).
Fig 4.
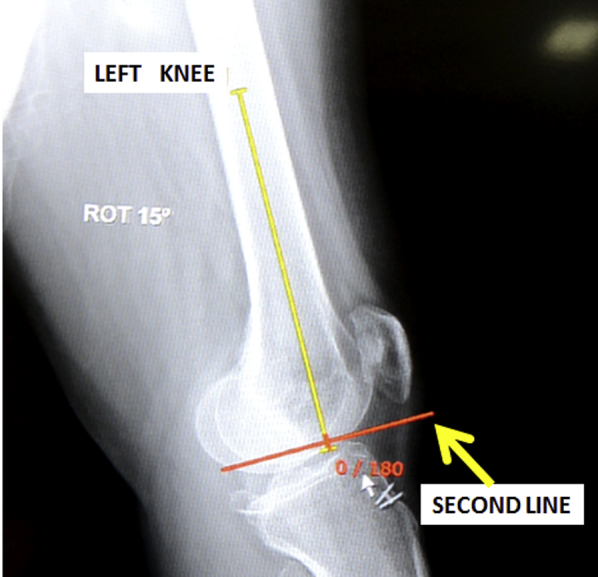
Following the first line (yellow line), the second line is performed in a left knee for the diagnosis of posterolateral corner injury. This line should be perpendicular to the first line and drawn in the distal aspect of the femoral condyles (red line).
Fig 5.
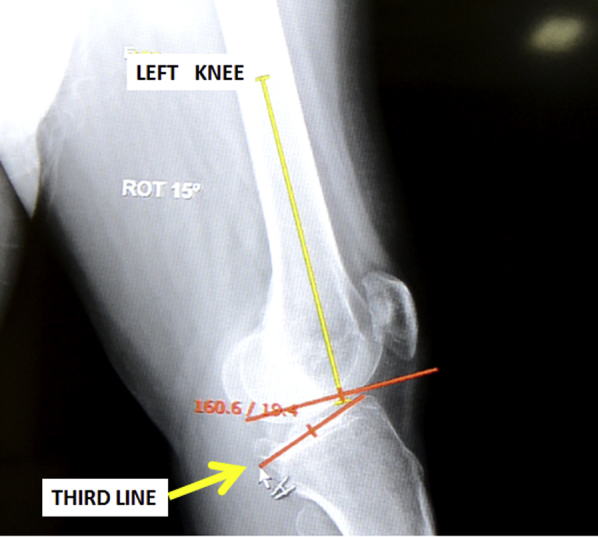
The third line is shown in a lateral left knee radiograph. Following the first 2 lines, the third and last line is drawn following the tibial slope. Then the angle between the second line and this third line should be measured. In this case, the angle was 19.4°, and this result must be compared with the unaffected limb measurements, using the same steps.
Table 1.
Advantages and Disadvantages of Our Technique
| Advantages | Disadvantages |
|---|---|
| Easy to perform and does not require the physician inside the radiographic room, decreasing the radiation exposure to health care employees. | Requires 2 radiographs, one for the affected and another for the nonaffected knee. |
| Low cost and reproducible. | Does not differentiate the injured structures. |
| This technique is able to compare the affected and the unaffected limb. | This technique is not validated, therefore sensitivity and specificity are unknown. |
Table 2.
Pearls and Pitfalls of Our Technique
| Pearls | Pitfalls |
|---|---|
| A through physical examination is key to ensure the correct patient indication for this test. | Ensure that the contralateral limb physical examination is normal, as it will be used as a reference for normal values. |
| Ensure the correct position of external rotation of the limbs using a goniometer. | Differences in external rotation between the sides may provide differences in the radiographic measurement. |
| Use a fixture to keep the limb in 15° of external rotation, avoiding the use of a physician inside the room to keep this position. |
Discussion
This Technical Note describes our preferred method for assessing the rotational instability associated with posterolateral corner injuries. We believe we have described in detail how this examination can be used in combination with a thorough physical exam, MRI, and varus stress x-rays to more fully evaluate injuries to the posterolateral corner.
Isolated posterolateral corner injuries are rare, accounting for only 28% of all posterolateral corner injuries,11 and are often unrecognized injuries.12 As a consequence, a delayed diagnosis can be a cause of poor outcomes, chronic pain, posterolateral instability, and cartilage damage.12, 13
In recent years, a better understanding of the anatomy and biomechanics of these injuries has also provided more information on the importance of the correct diagnosis, particularly the effect of untreated posterolateral corner injuries on native and reconstructed anterior and posterior cruciate ligaments.14, 15 These lesions can occur as a result of direct or indirect trauma,16, 17 usually from traffic accidents or sports activities. Time to presentation following injury can significantly affect the physical examination. In acute cases, swelling, difficulty or incapacity in walking, pain in the posterolateral structures, and ecchymosis may be present. For chronic injuries, instability and difficulty competing in athletics, especially those that require abrupt changes in direction, may be the only complaint. Several special tests for the diagnosis of this pathology have been well described. However, physical examination findings can be dominated by other concomitant ligament injuries (i.e., anterior and posterior cruciate ligament injuries),18 and therefore imaging modality is crucial to evaluate patients with these complex injuries.18
Imaging modalities for these lesions, although helpful, are limited. The position of the posterolateral structures, anatomic variation, and the oblique orientation of these structures make the diagnosis of these injuries difficult via MRI. Furthermore, there is a significant decrease in the specificity of diagnosis of ligament injuries through MRI when a multiligament knee injury is present, which corresponds to the majority of posterolateral corner injuries.19
In contrast, varus stress radiography has been reported to be an objective and repeatable exam for evaluating posterolateral corner injuries and can be as a complement in the diagnostic approach to these injuries.10, 20 We recognize that some studies have shown corresponding amounts of lateral compartment opening on varus stress radiographs with the severity of the lesion on MRI.20 In a biomechanic study performed by LaPrade et al., the radiographic measurement of lateral gapping during varus stress radiographs revealed significant differences regarding the affected structures: isolated fibular collateral injuries had a mean increase of 2.7 mm in lateral gapping compared with the intact knee. This difference increased to 4.0 mm for a complete grade III posterolateral corner injury.10
Although varus stress radiography seems to be a feasible and reproducible way to define the affected structures, we believe that our radiographic method may also contribute to the diagnosis of this pathology. In our test, the posterolateral instability can be visualized as an objective side-to-side difference. Furthermore, our test does not require a physician in the room to manually apply the varus stress, decreasing the radiation exposure. While we suggest the use of our technique, further studies are necessary to validate the sensitivity and specificity of our test for posterolateral corner injuries in isolation or in combination with multiligament injuries.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
With the patient positioned supine on the table, the radiographic tube is placed 1 m from the knee that will be radiographically evaluated. The unhealthy left inferior leg is raised 35 cm, with the heel placed in a customized fixture in 15° of external rotation. The patient must relax the inferior limb muscles; the radiographic tube is then placed in 15° of caudal inclination, with the radiographic film cassette over the table and perpendicular to the radiographic tube. The image is then obtained. The same technique is applied for the healthy inferior limb. Once the technique is performed in both limbs, the radiographic images are evaluated. The middle aspect of the femoral shaft is identified, and a longitudinal line is drawn following the longitudinal axis of the femur. The second line should be perpendicular to the first line, at the distal aspect of the femoral condyles. Following this, the last line is drawn parallel to the tibial plateau, as is usually done to evaluate the tibial slope. The angle created between the second and third lines is evaluated and recorded. The same steps are performed for both knees, and the difference between the results on both sides is evaluated.
References
- 1.Bahk M.S., Cosgarea A.J. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc. 2006;14:12–19. doi: 10.1097/00132585-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Cooper J.M., McAndrews P.T., LaPrade R.F. Posterolateral corner injuries of the knee: Anatomy, diagnosis, and treatment. Sports Med Arthrosc. 2006;14:213–220. doi: 10.1097/01.jsa.0000212324.46430.60. [DOI] [PubMed] [Google Scholar]
- 3.Djian P. Posterolateral knee reconstruction. Orthop Traumatol Surg Res. 2015;101:S159–S170. doi: 10.1016/j.otsr.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 4.Ellera Gomes J.L., Leie M.A., Ramirez E., Gomes T.E. Frog-leg test maneuver for the diagnosis of injuries to the posterolateral corner of the knee: A diagnostic accuracy study. Clin J Sport Med. 2016;26:216–220. doi: 10.1097/JSM.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade R.F., Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Rel Res. 2002:110–121. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Krause D.A., Levy B.A., Shah J.P., Stuart M.J., Hollman J.H., Dahm D.L. Reliability of the dial test using a handheld inclinometer. Knee Surg Sports Traumatol Arthrosc. 2013;21:1011–1016. doi: 10.1007/s00167-011-1873-6. [DOI] [PubMed] [Google Scholar]
- 7.Martin R.K., Berdusco R., MacDonald P.B. Physical examination and imaging studies in posterolateral corner injuries. J Knee Surg. 2015;28:435–440. doi: 10.1055/s-0035-1559803. [DOI] [PubMed] [Google Scholar]
- 8.Veltri D.M., Warren R.F. Anatomy, biomechanics, and physical findings in posterolateral knee instability. Clin Sports Med. 1994;13:599–614. [PubMed] [Google Scholar]
- 9.Shen J., Zhang H., Lv Y. Validity of a novel arthroscopic test to diagnose posterolateral rotational instability of the knee joint: The lateral gutter drive-through test. Arthroscopy. 2013;29:695–700. doi: 10.1016/j.arthro.2012.10.031. [DOI] [PubMed] [Google Scholar]
- 10.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 11.Geeslin A.G., LaPrade R.F. Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. Am J Sports Med. 2010;38:2502–2508. doi: 10.1177/0363546510376232. [DOI] [PubMed] [Google Scholar]
- 12.Welsh P., DeGraauw C., Whitty D. Delayed diagnosis of an isolated posterolateral corner injury: A case report. J Can Chiropr Assoc. 2016;60:299–304. [PMC free article] [PubMed] [Google Scholar]
- 13.Covey D.C. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83:106–118. doi: 10.2106/00004623-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 15.Markolf K.L., Graves B.R., Sigward S.M., Jackson S.R., McAllister D.R. Popliteus bypass and popliteofibular ligament reconstructions reduce posterior tibial translations and forces in a posterior cruciate ligament graft. Arthroscopy. 2007;23:482–487. doi: 10.1016/j.arthro.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaPrade R.F., Terry G.C. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433–438. doi: 10.1177/036354659702500403. [DOI] [PubMed] [Google Scholar]
- 17.Chahla J., Moatshe G., Dean C.S., LaPrade R.F. Posterolateral corner of the knee: Current concepts. Arch Bone Joint Surg. 2016;4:97–103. [PMC free article] [PubMed] [Google Scholar]
- 18.Rosas H.G. Unraveling the posterolateral corner of the knee. Radiographics. 2016;36:1776–1791. doi: 10.1148/rg.2016160027. [DOI] [PubMed] [Google Scholar]
- 19.Rubin D.A., Kettering J.M., Towers J.D., Britton C.A. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170:1207–1213. doi: 10.2214/ajr.170.5.9574586. [DOI] [PubMed] [Google Scholar]
- 20.Gwathmey F.W., Jr., Tompkins M.A., Gaskin C.M., Miller M.D. Can stress radiography of the knee help characterize posterolateral corner injury? Clin Orthop Rel Res. 2012;470:768–773. doi: 10.1007/s11999-011-2008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
With the patient positioned supine on the table, the radiographic tube is placed 1 m from the knee that will be radiographically evaluated. The unhealthy left inferior leg is raised 35 cm, with the heel placed in a customized fixture in 15° of external rotation. The patient must relax the inferior limb muscles; the radiographic tube is then placed in 15° of caudal inclination, with the radiographic film cassette over the table and perpendicular to the radiographic tube. The image is then obtained. The same technique is applied for the healthy inferior limb. Once the technique is performed in both limbs, the radiographic images are evaluated. The middle aspect of the femoral shaft is identified, and a longitudinal line is drawn following the longitudinal axis of the femur. The second line should be perpendicular to the first line, at the distal aspect of the femoral condyles. Following this, the last line is drawn parallel to the tibial plateau, as is usually done to evaluate the tibial slope. The angle created between the second and third lines is evaluated and recorded. The same steps are performed for both knees, and the difference between the results on both sides is evaluated.