Abstract
Bone defects caused by femoral and tibial tunnel enlargement can pose a significant technical challenge when planning to perform revision anterior cruciate ligament reconstruction. A number of options have been described for managing osseous deficiencies, including the use of large autograft or allograft bone dowels to provide sufficient tunnel fill and subsequent structural support for revision surgery. These techniques can be time-consuming and technically demanding to ensure proper tunnel fill and press-fit stability of the bone graft. We describe our preferred technique for arthroscopic bone grafting using a mixture of demineralized cortical bone graft augmented with platelet-rich plasma delivered through a simple delivery system.
Anterior cruciate ligament (ACL) reconstruction remains the gold-standard treatment for young active patients with functional instability after an ACL injury. As the number of primary ACL reconstructions is increasing, the need for revision ACL reconstruction is also increasing, with an estimated 13,000 revision ACL reconstructions per year.1 Successful revision ACL reconstruction requires an understanding of the primary cause of failure, careful preoperative planning, meticulous surgical execution, proper postoperative rehabilitation, and appropriate patient counseling.2
Although there are many strategies for revision ACL reconstruction, many patients will require 2-stage revision ACL reconstruction surgery because of tunnel widening. There is no widely accepted value for tunnel dimensions that can be treated with single-stage versus 2-stage revision surgery; however, many authors recommend a 2-stage procedure when tunnel widening greater than 10 to 15 mm is present (Fig 1).2 Ultimately, the decision to proceed with staged surgery is dependent on many factors, including tunnel position and the degree of osteolysis. Excessive tunnel widening can reduce graft apposition within the tunnels at the time of graft fixation, thereby placing graft stability and subsequent incorporation at greater risk of failure. Although surgical indications for staged revision ACL reconstruction should largely be based on surgeon comfort and ability to achieve stable graft fixation at the time of surgery, our recommended indications for a 2-stage approach include cases of excessive tunnel osteolysis (>12 mm) or tunnel malpositioning that precludes avoidance of primary tunnels. In this article, we describe our approach for arthroscopic delivery of bone allograft matrix augmented with platelet-rich plasma (PRP) to facilitate biological consolidation.
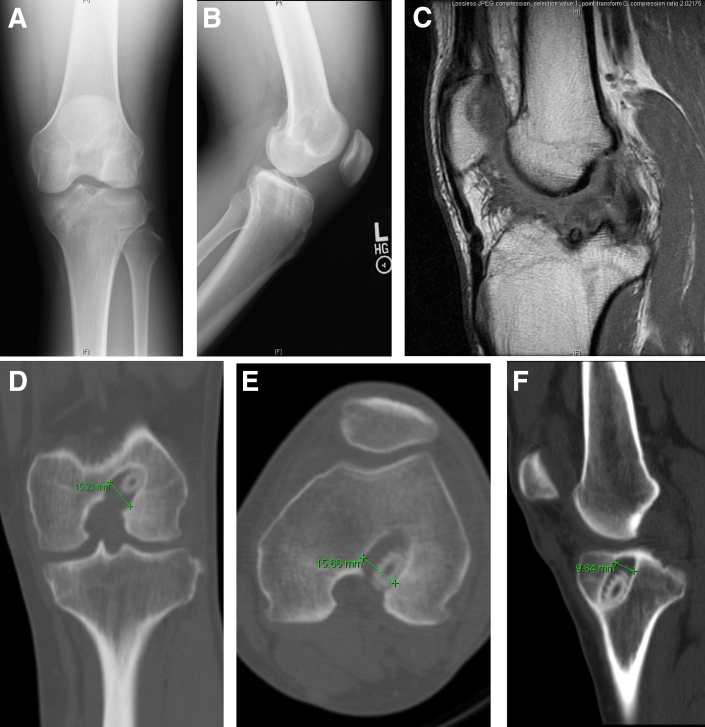
Fig 1.
(A, B) Anteroposterior and lateral knee radiographs showing bone tunnel positioning, widening, and retained biocomposite screw. (C) Sagittal magnetic resonance imaging showing insufficiency of the anterior cruciate ligament graft. (D-F) Coronal and axial computed tomography images showing bone tunnel dilatation (femoral, 15.7 mm; tibial, 9.8 mm). We elected not to graft the tibia because the tunnel dimensions were acceptable.
Surgical Technique
Preoperative Setup
The patient is placed under general or spinal anesthesia and positioned supine on the operative table with a post secured at the level of the upper thigh on the operative side. In addition, we place a secure foot post at the level of the mid calf to help maintain variable degrees of knee flexion throughout the procedure. The post is placed in a position that will securely facilitate 90° to 110° of knee flexion. A tourniquet is applied to the proximal leg; however, it is not typically used. The knee is examined to confirm preoperative findings.
After induction of anesthesia, approximately 80 mL of peripheral whole blood is collected from the intravenous line to prepare the PRP. The preferred technique of the senior author (K.J.J.) is to routinely augment the injectable bone graft material with PRP; however, other biologics such as bone marrow aspirate concentrate can also be used. The venous blood is placed into the centrifuge and prepared according to the protocol established by Arthrex (Naples, FL) for the Angel Processing System.
Diagnostic Arthroscopy
By use of standard anterolateral and anteromedial arthroscopic portals, a full diagnostic arthroscopy of the knee is performed (Video 1). The failed ACL graft is identified and assessed for mode of failure (e.g., failure of biological healing, inaccurate tunnel placement, or traumatic tear). A thorough examination evaluating for concomitant chondral and meniscal injury is performed.3, 4 Standard arthroscopic biters are used to perform morcellation of the graft tissue, and the combination of a 4.5 mm arthroscopic shaver and an ArthroCare device (ArthroCare, Austin TX) is used to excise the graft material and clearly expose the ACL tunnels. To adequately visualize the entire femoral tunnel, we recommend using a 70° arthroscope placed in the anterolateral portal. The knee can be placed in variable degrees of flexion to facilitate access to the inside of the tunnel because it is extremely important to remove all soft tissue and retained instrumentation. Next, a 5.5 mm arthroscopic shaver or burr is used to carefully debride the inner margins of the tunnel of any sclerotic bone (Fig 2).
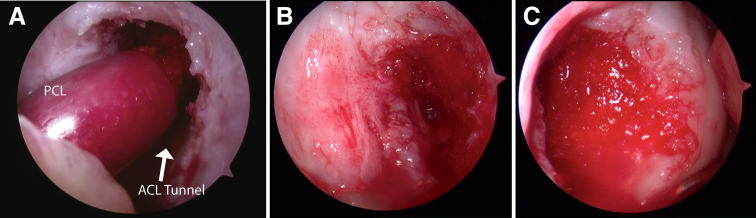
Fig 2.
(A) Arthroscopic view of the OsteoPrecision cannula inserted through the anteromedial portal under dry conditions and the graft material being injected under direct visualization, delivering the injectable bone graft with the knee drained of fluid. (ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.) (B) Arthroscopic view of the entire femoral tunnel through the anterolateral portal with a 70° arthroscope. (C) Arthroscopic view of the femoral tunnel after complete graft fill.
Preparation of Bone Graft
As the surgeon prepares the bone tunnels for graft implantation, the surgical assistant can prepare the arthroscopic graft-delivery device and bone graft material. The OsteoPrecision Graft Delivery Device kit (Arthrex) is opened and assembled on the back table. Next, 5 mL of StimuBlast DBM Putty (Arthrex) and 5 mL of FlexiGRAFT cortical fibers (Arthrex) are manually mixed together along with the previously obtained PRP. The PRP serves as a biological augmentation for graft healing as well as a hydrating substance to reduce viscosity and facilitate easy flow of the bone graft material through the device. We recommend a minimum of 10 mL of graft material per tunnel; however, this can vary based on the amount of preoperative tunnel osteolysis observed on advanced imaging. Once the bone graft mixture is complete, it is transferred into the OsteoPrecision syringe and the threaded cannula and stylet are reassembled for use.
Arthroscopic Delivery of Bone Graft
The knee is flexed to approximately 90° to 100° and stabilized with the foot post. With the 70° arthroscope in the anterolateral portal, the OsteoPrecision cannula is inserted through the anteromedial portal into the intercondylar notch and advanced to the end of the femoral tunnel. The stylet is slowly advanced to deliver the bone graft, which can be observed through the clear delivery cannula. With the cannula “bottomed out” within the femoral tunnel, increased pressure is experienced as the tunnel fills with the graft material. The cannula should be carefully withdrawn to allow controlled fill of the entire tunnel (Fig 2). We prefer to perform this part of the procedure under dry conditions; however, the material can be safely injected with the knee joint insufflated. Once the entire tunnel is completely filled with bone graft, a freer elevator is used to contour the graft at the tunnel entrance. All excess fluid is removed from the knee joint, and the arthroscopic portals are closed with absorbable sutures.
Postoperative Management
Postoperatively, the patient is allowed to immediately bear full weight with crutches, and no postoperative immobilization is necessary. Supervised active and passive range-of-motion exercises, as well as quadriceps, hip, and core strengthening, are initiated 1 week after surgery. We routinely obtain a repeat computed tomography scan 5 to 6 months after the procedure to assess bone graft incorporation.5 If satisfactory tunnel fill is observed, we proceed with revision ACL reconstruction shortly thereafter.
Discussion
Failure of primary ACL reconstruction is often multifactorial, and tunnel osteolysis remains a challenging technical problem. Although drilling techniques (e.g., anteromedial or retrograde) can facilitate avoidance of nonanatomic tunnels, excessive tunnel widening often necessitates the use of a staged approach with bone grafting to facilitate successful ACL graft fixation and incorporation. Many options for bone graft material exist, including iliac crest autograft, anterior tibial plateau autograft, Gerdy tubercle autograft, large allograft bone dowels, and crushed cancellous bone allograft. Potential disadvantages to using autograft bone include donor-site morbidity and limited volume. In addition, drawbacks to using large single-allograft bone dowels include technical demand and increased operative time to ensure an appropriate press fit, as well as a higher cost, and although they are osteoconductive, they are not osteoinductive (Table 1).2 Last, the existing tunnels often have an irregular shape, thereby making complete tunnel fill challenging to achieve with cylindrical dowels. In our simplified technique, the combination of cortical allograft fibers and devitalized bone matrix with PRP creates a malleable graft composite that is easy to administer using an arthroscopic delivery system. Furthermore, there may be an advantage of the graft material being both osteoconductive and osteoinductive in this scenario.6
Table 1.
Bone Graft Options in Revision Anterior Cruciate Ligament Reconstruction
| Bone Graft Type | Benefits | Drawbacks |
|---|---|---|
| Iliac crest autograft | Can be harvested in dowels, can be a structural graft, large volume available | Donor-site morbidity |
| Anterior tibial plateau autograft | Available from same incision | Technically difficult when avoiding tibial tunnel, limited quantity |
| Gerdy tubercle autograft | Locally available | Limited quantity |
| Crushed cancellous allograft | No donor-site morbidity, large quantity | Osteoconductive only, cost |
| Our described injectable bone allograft∗ | No donor-site morbidity, osteoconductive and osteoinductive, technically less challenging to fill bone defects, complete fill of irregularly shaped tunnels | Cost |
Devitalized cortical bone, devitalized bone matrix putty, and platelet-rich plasma.
The complexities of revision ACL reconstruction require thoughtful technical consideration that should be individualized to the patient. Arthroscopic bone graft techniques can be challenging and time-consuming, but this simplified technique can be used to efficiently address large, irregularly shaped bone tunnel defects with reliable graft incorporation and structural integrity to support revision ACL graft fixation and healing (Table 2). We have used this technique in various clinical scenarios with favorable clinical outcomes (Fig 3). Prospective evaluation of staged revision ACL reconstruction is under way to determine the long-term success of this technique.
Table 2.
Pearls and Pitfalls
| Pearls |
| The surgeon should use a 70° arthroscope to adequately visualize the entire femoral tunnel and ensure adequate debridement of all soft tissue and retained instrumentation. |
| A foot post positioned at the end of the bed can be helpful to achieve varying degrees of knee flexion and facilitate easy access to the femoral tunnel. |
| The surgeon should be sure to “bottom out” the cannula stylet into the femoral tunnel and allow the bone graft to gently push the stylet out of the tunnel as it is being filled. This will ensure complete fill of the tunnel. |
| Although the bone graft can be injected while the joint is filled with irrigation fluid, we find it easier to administer the graft under dry conditions. |
| Pitfalls |
| The surgeon should not manually withdraw the stylet as the bone graft is injected into the tunnel. Doing so may cause incomplete tunnel fill in some areas. |
| The surgeon should not underestimate the amount of bone graft needed for each tunnel to ensure there will be enough for complete fill. |
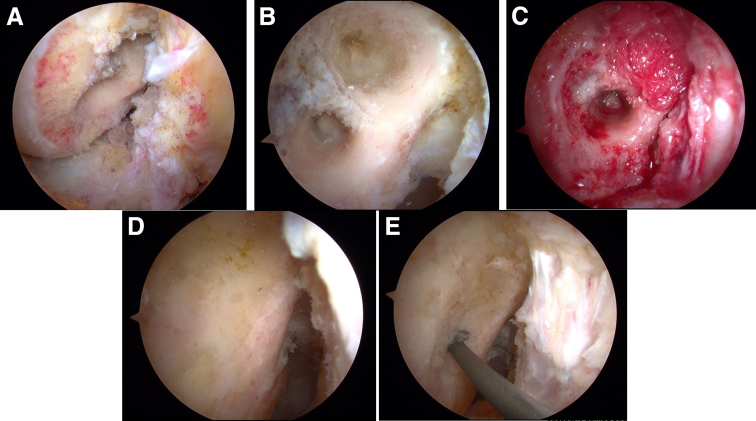
Fig 3.
Additional case of a 28-year-old patient with failed double-bundle anterior cruciate ligament (ACL) reconstruction and excessive loss of bone stock requiring bone grafting of the femoral tunnels. (A, B) Arthroscopic images showing the tunnels after debridement. (C) Arthroscopic view of the anteromedial bundle tunnel after complete allograft fill. (D, E) At the time of revision ACL reconstruction, the tunnels were found to be completely filled with bone. Given the complete graft consolidation, we were able to perform anatomic drilling and ACL graft placement.
Footnotes
The authors report the following potential conflict of interest or source of funding: K.T.Y. receives support from Orthopaedic Research and Education Foundation (OREF). Research grant. G.M.M. receives support from H&H Lee Foundation. Resident research grant. K.J.J. receives support from Musculoskeletal Transplant Foundation (MTF). Research grant support. Arthrex. Educational support. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step video demonstrating the arthroscopic delivery of injectable bone graft for staged revision anterior cruciate ligament reconstruction.
References
- 1.Leroux T., Wasserstein D., Dwyer T. The epidemiology of revision anterior cruciate ligament reconstruction in Ontario, Canada. Am J Sports Med. 2014;42:2666–2672. doi: 10.1177/0363546514548165. [DOI] [PubMed] [Google Scholar]
- 2.Erickson B.J., Cvetanovich G., Waliullah K. Two-stage revision anterior cruciate ligament reconstruction. Orthopedics. 2016;39:e456–e464. doi: 10.3928/01477447-20160324-01. [DOI] [PubMed] [Google Scholar]
- 3.Chen J.L., Allen C.R., Stephens T.E. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: A MARS cohort study. Am J Sports Med. 2013;41:1571–1578. doi: 10.1177/0363546513487980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MARS Group Meniscal and articular cartilage predictors of clinical outcome after revision anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:1671–1679. doi: 10.1177/0363546516644218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uchida R., Toritsuka Y., Mae T., Kusano M., Ohzono K. Healing of tibial bone tunnels after bone grafting for staged revision anterior cruciate ligament surgery: A prospective computed tomography analysis. Knee. 2016;23:830–836. doi: 10.1016/j.knee.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Triplett S., Gonzales K., Chen S. LifeNet Health; Virginia Beach, VA: 2012. DBM fibers and cancellous bone induce spinal fusion in the athymic rat PLF model. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step video demonstrating the arthroscopic delivery of injectable bone graft for staged revision anterior cruciate ligament reconstruction.