Abstract
Purpose of review: The burden of disability from ischemic stroke continues to intensify. Any acute therapeutic option that reduces disability after ischemic stroke should be encouraged and further studied. In particular, the need for an effective treatment in patients with large vessel occlusion has been long overdue.
Recent findings: Consistent trial evidence has answered this need in an emphatic fashion, demonstrating improved functional outcomes with endovascular therapy following better patient selection, new device technology, and reduced treatment times. The article discusses the current evidence and guidelines and highlights the inherent complexities of a specialized intervention whose demand will grow exponentially. The scope for future investigation especially using advanced imaging to expand patient selection will be considered.
Summary: Endovascular thrombectomy is an established and highly efficacious acute treatment for ischemic stroke that we need to apply and implement to maximize benefit to the population.
Until recently, evidence-based therapy for acute ischemic stroke was limited to IV recombinant tissue plasminogen activator (IV-rtPA) within 4.5 hours of symptom onset. Uptake of IV-rtPA has risen gradually since the first landmark publication establishing its efficacy.1 Meta-analysis confirmed better functional outcomes with shorter onset-to-needle times regardless of age or stroke severity, prompting local and national initiatives that successfully promoted models of care focusing on efficiency and improved workflow.2,3 Patients with severe strokes due to proximal large vessel occlusion remained a challenge as the probability of recanalization with IV-rtPA alone remained modest.4 To facilitate timely reperfusion, endovascular thrombectomy was studied, as intra-arterial thrombolysis alone had not been shown to be more effective than IV-rtPA.5 Neutral endovascular trials published in 2013 were limited by long treatment delays, low recanalization rates with early generation device technology, and heterogeneous patient characteristics, often without requiring proven vessel occlusion.
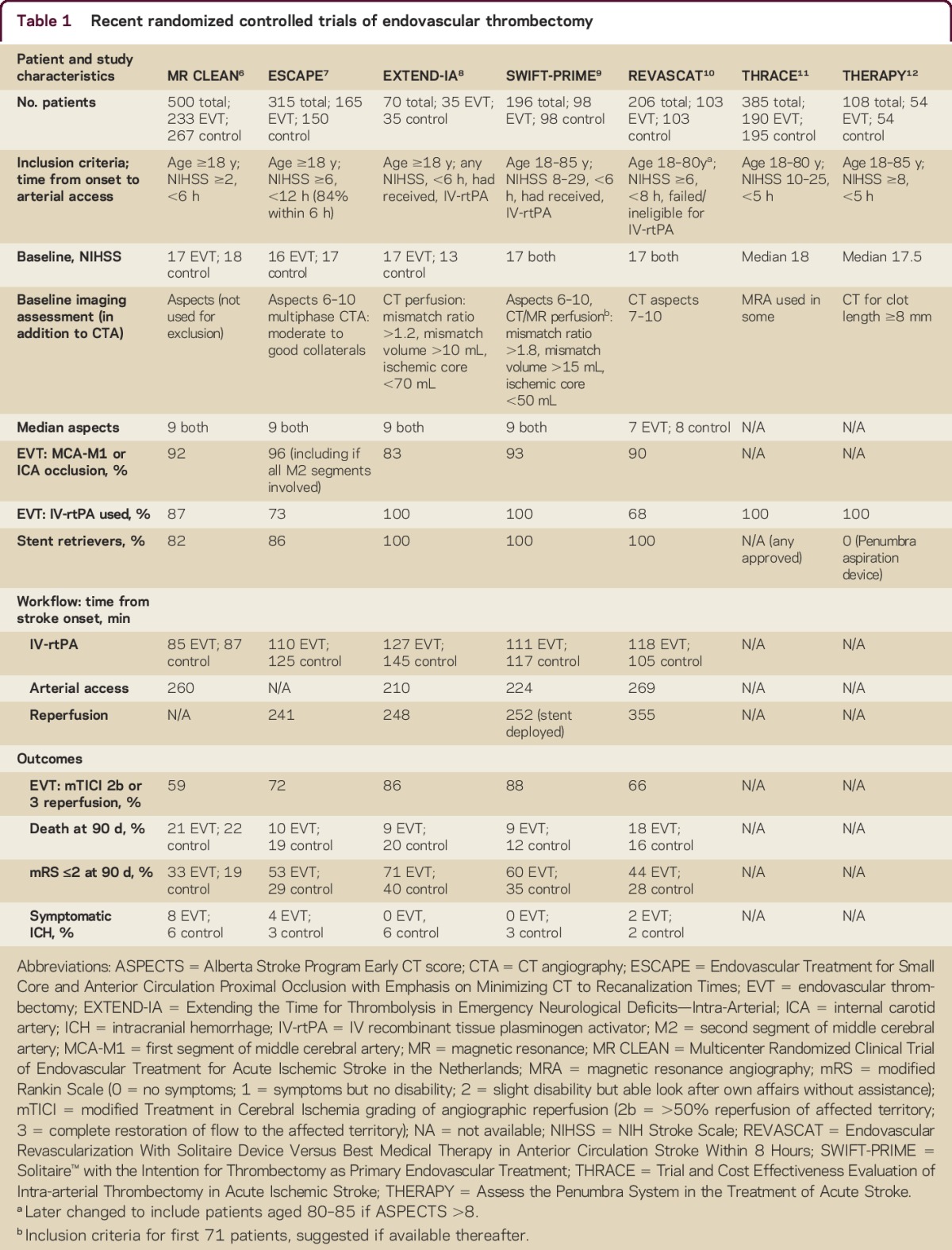
Now, 5 published randomized controlled trials have established the efficacy of endovascular thrombectomy,6–10 with 2 further trials yet to be published11,12 (table 1). Improved reperfusion and functional outcomes were observed without increased adverse effects, including symptomatic intracranial hemorrhage. These trials combined more effective stent retriever devices with faster workflow to reduce treatment delays and imaging to prove large vessel occlusion and, in several cases, exclude patients with large areas of irreversibly injured brain using perfusion or collateral imaging. The majority had intracranial internal carotid artery and proximal middle cerebral artery occlusion and achieved arterial puncture within 6 hours. Most trials included a proportion of patients who required transfer from a peripheral hospital (primary stroke center) to the endovascular-equipped comprehensive stroke center. Trial selection criteria varied but the largest and most inclusive trial (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands [MR CLEAN]) was robustly positive, indicating the broad generalizability of this treatment. There were relatively few patients treated beyond 6 hours after onset, with mild neurologic deficit (e.g., NIH Stroke Scale sore <6), or with distal (M2) occlusion. Subsequent meta-analysis may clarify effects in these subgroups. Patients with posterior circulation occlusion were also not included in these trials. However, further trials are ongoing to definitively assess effectiveness in the extended time window (Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy [POSITIVE] [NCT01852201] 6–12 hours and DWI/PWI and CTP Assessment in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention [DAWN] [NCT02142283] 6–24 hours) and in basilar artery occlusion (Basilar Artery International Cooperation Study [BASICS] NCT01717755).
Table 1 Recent randomized controlled trials of endovascular thrombectomy
These definitive trials have led to updated US, Canadian, and European guidelines.13–15 However, they also generate further important questions. Systems of care for patient triage and interhospital transfer networks require development. Demand for trained neurointerventionalists will substantially increase and training of the entire stroke team (from ambulance paramedics to endovascular suite staff) to achieve efficient and safe workflow is crucial. Whether it is more efficient to transport a patient to a primary stroke center for initial imaging and IV-rtPA before selected transfer of patients with large vessel occlusion or instead transport direct (bypassing the primary center) to a comprehensive stroke center for patients meeting simple clinical severity criteria16 remains uncertain and will likely vary according to local geographical considerations. The optimal approach to making IV-rtPA and endovascular treatment decisions in parallel during the imaging process in order for one treatment not to delay the other is also a critical area for development. The concept of waiting to assess failure of IV-rtPA is strongly discouraged.
The package of IV-rtPA for all eligible patients combined with immediate endovascular thrombectomy is recommended in the American Heart Association guideline update.13 This also ensures patients who are not eligible for endovascular thrombectomy (e.g., inappropriate vascular anatomy) still benefit from timely systemic thrombolysis. However, analogous to management of ST-elevation myocardial infarction, further trials may examine whether a direct to endovascular approach could be appropriate when it is immediately available. There may be further advances in thrombolytic efficacy, for example using tenecteplase or a combination of rtPA with argatroban or eptifibitide.17,18 The potential to slow progression of the ischemic cascade using cytoprotective strategies that have previously failed may now be revisited in the era of highly effective reperfusion.19
Implementation of acute stroke therapies including thrombectomy at the population level is being explored. This includes promoting community awareness of acute stroke symptoms and implications and optimizing emergency triage protocols to assist its timely recognition.3,20 Adopting established models of care has been shown21 but finite resources and personnel will likely limit applicability to all settings. A culture that encourages data collection for consecutive patients will identify delays in current protocols to improve performance measures.3,22
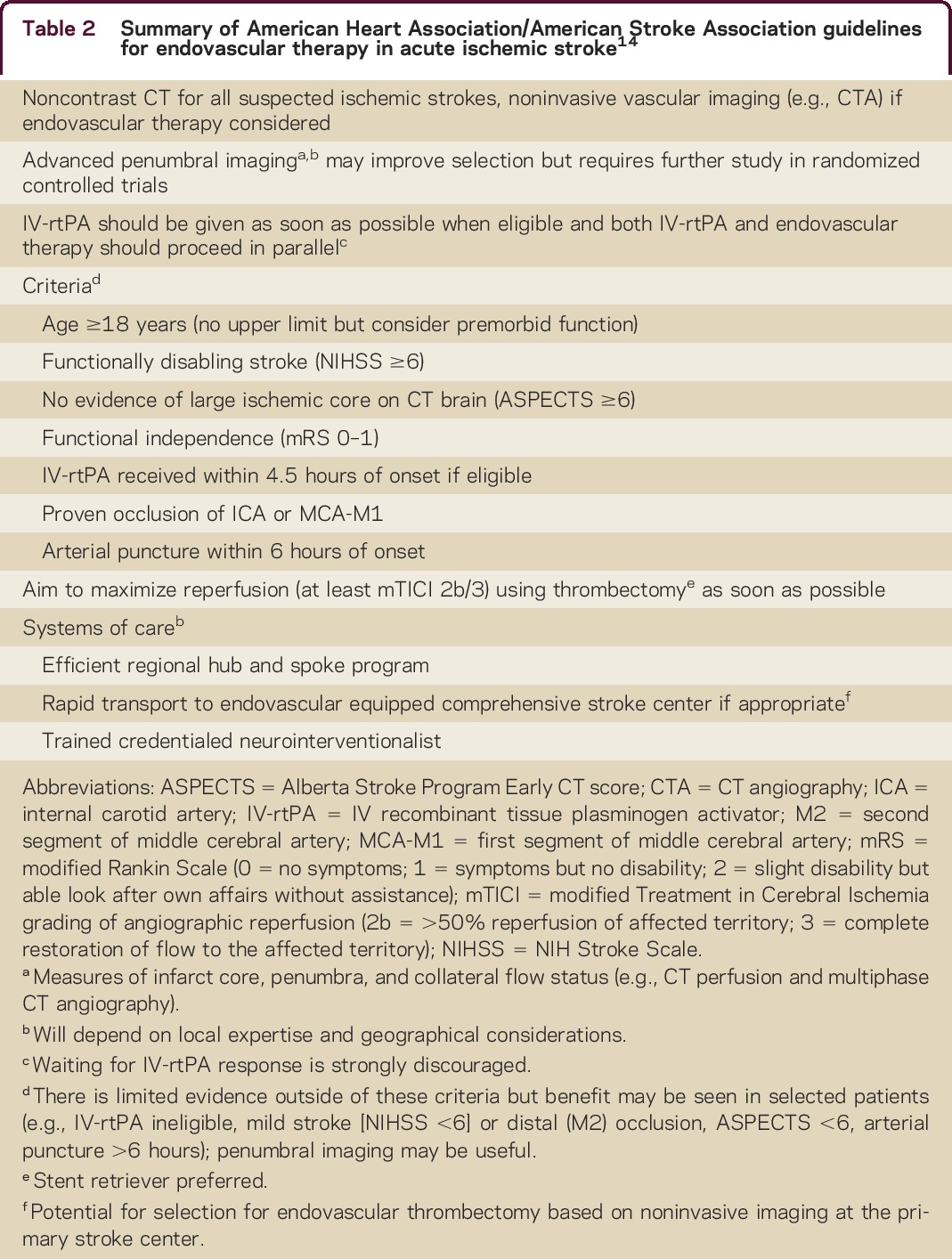
Minimizing time from onset to reperfusion is essential to maximize the population benefit, with shorter onset-to-needle and onset-to-reperfusion times clearly associated with better outcomes.2,23 However, at an individual level, there are patients with salvageable brain tissue well beyond 6 hours after stroke onset, and recent studies have indicated the feasibility of identifying these individuals using brain imaging.7,24 Noncontrast CT provides some information on the extent of irreversible injury (e.g., Alberta Stroke Program Early CT Score [ASPECTS] > 6). Specificity is high but sensitivity is modest, particularly in the first 1–2 hours after stroke onset, and interrater agreement is also imperfect. Thresholded cerebral blood flow or cerebral blood volume using perfusion imaging (as used in Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial [EXTEND-IA] and most Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment [SWIFT PRIME] patients) has greater sensitivity for large ischemic core and can be standardized using automated software.8,9 Collateral scoring of CT angiography (CTA) as performed in the Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trial can similarly identify patients likely to have a large area of irreversible injury but should be assessed using a multiphase acquisition (as used in most ESCAPE trial patients) as standard static CTA tends to underestimate collateral flow, which, by its nature, is delayed, leading to unwarranted exclusion of patients who may benefit from thrombectomy.7,25 Imaging-based selection may lead to effective treatment in an extended time window to include late presenting and wake-up stroke patients. However, improved functional outcomes will need to be demonstrated in randomized trials before this approach is widely accepted. A summary of current guidelines is presented in table 2.
Table 2 Summary of American Heart Association/American Stroke Association guidelines for endovascular therapy in acute ischemic stroke14
Endovascular thrombectomy is transforming outcomes for those who have the most devastating of ischemic strokes. However, there is still much work to be done and medical champions must demonstrate leadership to implement the new evidence and guidelines. Further work to better understand treatment effect in subgroups underrepresented in the trials, streamline treatment delivery, and expand access to geographically disadvantaged areas is required to maximize the effect of this new era in stroke reperfusion therapy.
AUTHOR CONTRIBUTIONS
Lai Yin Law drafted the manuscript. All authors made revisions to this article for intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
L.Y. Law reports no disclosures. B.C.V. Campbell receives grant support from the National Health and Medical Research Council of Australia, the National Heart Foundation of Australia, the National Stroke Foundation of Australia, the Royal Australasian College of Physicians, and the Royal Melbourne Hospital Foundation. He was co-principal investigator of the EXTEND-IA trial, which was in part supported by an unrestricted grant from Medtronic. T. Wijeratne serves on the editorial board of Neurology: Clinical Practice. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000217.
Correspondence to: twijeratne@gmail.com
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000217.
Received September 07, 2015
Accepted December 01, 2015
Footnotes
Correspondence to: twijeratne@gmail.com
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the authors is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0000000000000217.
REFERENCES
- 1.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581–1587. [DOI] [PubMed]
- 2.Emberson J, Lees KR, Lyden P, et al.. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–1935. [DOI] [PMC free article] [PubMed]
- 3.Fonarow GC, Zhao X, Smith EE, et al.. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 2014;311:1632–1640. [DOI] [PubMed]
- 4.Bhatia R, Hill MD, Shobha N, et al.. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke real-world experience and a call for action. Stroke 2010;41:2254–2258. [DOI] [PubMed]
- 5.Ciccone A, Valvassori L, Nichelatti M, et al.. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013;368:904–913. [DOI] [PMC free article] [PubMed]
- 6.Berkhemer OA, Fransen PS, Beumer D, et al.. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. [DOI] [PubMed]
- 7.Goyal M, Demchuk AM, Menon BK, et al.. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–1030. [DOI] [PubMed]
- 8.Campbell BC, Mitchell PJ, Kleinig TJ, et al.. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–1018. [DOI] [PubMed]
- 9.Saver JL, Goyal M, Bonafe A, et al.. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285–2295. [DOI] [PubMed]
- 10.Jovin TG, Chamorro A, Cobo E, et al.. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296–2306. [DOI] [PubMed]
- 11.Bracard S, Ducrocq X, Guillemin F, eds. Thrace Study: Intermediate Analysis Results. Glasgow: European Stroke Organization Conference; 2015.
- 12.Mocco J, Zaidat O, von Kummer R, eds. Results of the THERAPY Trial: A Prospective Randomized Trial to Define the Role of Mechanical Thrombectomy as Adjunctive Treatment to IV R-TPA in Acute Ischemic Stroke. Glasgow: European Stroke Organization Conference; 2015.
- 13.Powers WJ, Derdeyn CP, Biller J, et al.. 2015 AHA/ASA focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:3020–3035. [DOI] [PubMed]
- 14.Casaubon LK, Boulanger JM, Blacquiere D, et al.. Canadian stroke best practice recommendations: hyperacute stroke care guidelines, update 2015. Int J Stroke 2015;10:924–940. [DOI] [PubMed]
- 15.European Stroke Organisation. Consensus Statement on Mechanical Thrombectomy in Acute Ischemic Stroke: ESO-Karolinska Stroke Update 2014 in Collaboration with ESMINT and ESNR. 2015. Available at: http://2014.strokeupdate.org/consensus-statement-mechanical-thrombectomy-acute-ischemic-stroke. Accessed August 18, 2015.
- 16.de la Ossa NP, Carrera D, Gorchs M, et al.. Design and validation of a prehospital stroke scale to predict large arterial occlusion the rapid arterial occlusion evaluation scale. Stroke 2014;45:87–91. [DOI] [PubMed]
- 17.Parsons M, Spratt N, Bivard A, et al.. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N Engl J Med 2012;366:1099–1107. [DOI] [PubMed]
- 18.Fisher M, Saver JL. Future directions of acute ischaemic stroke therapy. Lancet Neurol 2015;14:758–767. [DOI] [PubMed]
- 19.Yenari MA, Hemmen TM. Therapeutic hypothermia for brain ischemia: where have we come and where do we go? Stroke 2010;41(10 suppl):S72–S74. [DOI] [PMC free article] [PubMed]
- 20.Ekundayo OJ, Saver JL, Fonarow GC, et al.. Patterns of emergency medical services use and its association with timely stroke treatment findings from Get with the Guidelines-Stroke. Circ Cardiovasc Qual Outcomes 2013;6:262–269. [DOI] [PubMed]
- 21.Meretoja A, Weir L, Ugalde M, et al.. Helsinki model cut stroke thrombolysis delays to 25 minutes in Melbourne in only 4 months. Neurology 2013;81:1071–1076. [DOI] [PubMed]
- 22.Mehta BP, Leslie-Mazwi TM, Chandra RV, et al.. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc 2014;3:e000963. [DOI] [PMC free article] [PubMed]
- 23.Khatri P, Yeatts SD, Mazighi M, et al.. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 2014;13:567–574. [DOI] [PMC free article] [PubMed]
- 24.Lansberg MG, Straka M, Kemp S, et al.. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): a prospective cohort study. Lancet Neurol 2012;11:860–867. [DOI] [PMC free article] [PubMed]
- 25.Menon BK, d'Esterre CD, Qazi EM, et al.. Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology 2015;275:510–520. [DOI] [PubMed]


