Abstract
Background:
It is not convenient or always possible to address parent requests for prescription refills after hours. The primary objective of this quality improvement study was to decrease the number of refill requests received outside of regular business hours. A secondary objective was to reduce the negative effects of call fatigue and related exhaustion for physicians taking calls.
Methods:
Voluntary participation in this quality improvement project was solicited from the Child Neurology Division at a single academic, tertiary, metropolitan children's hospital. Study design was developed from a project charter, fishbone diagram, process map, driver diagram, and plan-do-study-act worksheet. A peer-reviewed letter was mailed to all clinic patient families and signs were displayed in the clinic space as notification of a policy change. A peer-reviewed script was provided to the Children's Mercy Contact Center triage personnel addressing after-hours refill requests. The number of refill requests received during each after-hours call shift was recorded from April 1, 2015, to March 31, 2016, with a primary outcome measure of the monthly number of refill requests.
Results:
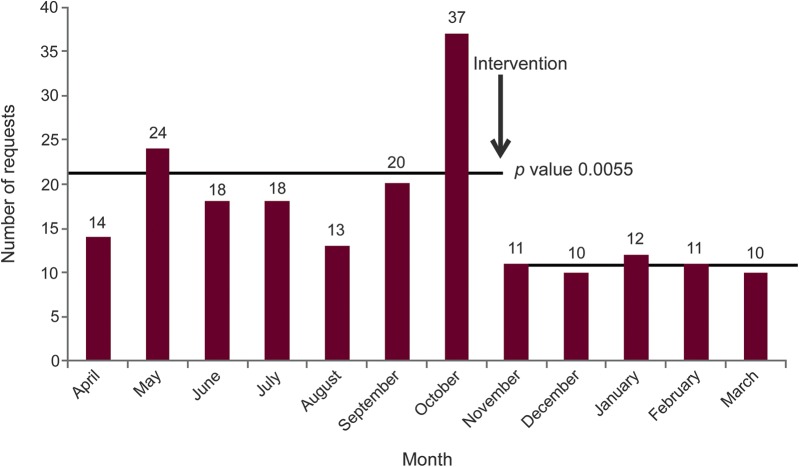
Postintervention, the average number of refill requests after hours decreased by 39% from 21 to 11 per month (p = 0.0055).
Conclusions:
This simple intervention has promise to limit prescription refill requests made after hours and improve physician quality of life. Continued data collection will help establish the sustainability of the effect made by this intervention.
Medication nonadherence is a growing, multifactorial problem among children with chronic conditions,1 including neurologic and developmental disorders. Delayed medication acquisition contributes to nonadherence to prescribed regimens.2,3 Sometimes urgent requests for refills are received outside of business hours by on-call providers.
After-hours on-call responsibilities have been cited as one of the most stressful aspects of physician responsibilities4 and call fatigue contributes to physician burnout.5 Child Neurology resident trainees at our institution provide proportionate first-call coverage an average of 7–11 nights per month, from 17:00 to 08:00 hours. This coverage includes fielding calls from all medical facilities and clinic patients' families in Kansas and the western third of Missouri. Call shifts can be busy, particularly during winter months. It is not convenient or always possible to address parent requests for prescription refills after hours. Some antiepileptic and tone management medications are controlled substances and require a faxed written prescription, and physicians may be busy concentrating on acute neurologic emergencies.
Patient safety is paramount. As part of a larger effort to foster medication adherence and avoid lapses in pharmacologic management of pediatric neurologic conditions, the primary objective of this quality improvement study was to decrease the number of refill requests received outside of regular business hours. A secondary objective was to reduce the negative effects of call fatigue and related exhaustion for physician trainees.
METHODS
Standard protocol approvals, registrations, and patient consents
This quality improvement project did not involve human research subjects.
Voluntary participation in this quality improvement project was solicited from the Child Neurology Division Clinic Director and Service Line Director at a single academic, tertiary, metropolitan children's hospital (Children's Mercy, Kansas City, Missouri). Study design was developed from a project charter, fishbone diagram, process map, driver diagram, and plan-do-study-act worksheet, with the intervention that follows chosen for its likelihood to lead to change in the primary endpoint in the desired direction, to contribute to unintended effects, and ease of implementation. Prior to the study intervention, refill requests were received and addressed at all hours, including by the on-call physician when received outside of business hours, as defined as Monday through Friday from 08:00 to 17:00 hours.
A peer-reviewed letter (appendix e-1 at Neurology.org/cp) was mailed to all Child Neurology Clinic patients and their families notifying them of a policy change that would limit fulfillment of prescription refill requests to during business hours. Peer-reviewed signs were displayed in the clinic examination rooms at the 2 hospital campuses with Child Neurology Clinics (Adele Hall campus, Kansas City, Missouri, and Kansas campus, Overland Park, Kansas) advertising the policy change. Providers and clinic personnel were encouraged to review the policy change during clinic visits. A peer-reviewed script (appendix e-2) was provided to the Children's Mercy Contact Center triage personnel for use when addressing refill requests received after hours, as defined as between 17:00 and 08:00 hours daily, after implementation of the new policy. Contact Center personnel were encouraged to continue to forward any refill requests they determined to be urgent; for example, when patients were completely out of antiseizure medication. No other changes in policy, prescribing practices, or functionality occurred during the study period. The number of refill requests forwarded on to the physician on-call after hours was logged daily by the postcall physician and monthly data were entered into a Microsoft Excel spreadsheet from April 1, 2015, to March 31, 2016. The primary outcome measure was the number of refill requests received per month. With a skewness level of 12, statistical analysis was performed using the Mann-Whitney U test with results reported as median values and the interquartile range (IQR) (25th and 75th percentiles).
RESULTS
The average number of refill requests received per month outside of regular business hours preintervention was 21 (range 13–37, median 18, mode 18, IQR 16–22) (figure). The average number of refill requests received per month postintervention was 11 (range 10–12, median 11, mode 10 and 11, IQR 10–11), representing a 48% reduction (p = 0.0055).
Figure. Prescription refill requests.
Number of prescription refill requests received after hours during the study period. Time of intervention denoted by the arrow. Preintervention and postintervention averages of 21 and 11 requests per month, respectively, indicated by the solid lines (p = 0.0055).
DISCUSSION
With a relatively simply intervention consisting of a written letter, posted signs, and verbal review of the policy change, this study showed an appreciable decrease in the number of refill requests made by parents after hours. Continued data collection will help establish the sustainability of the effect made by this intervention. Scheduled medication acquisition can improve medication adherence and positively influence patient outcomes by potentially preventing neurologic emergencies, emergency department visits, or hospital admission. Future assessment of balancing measures such as patient/family dissatisfaction, emergency department visits, or hospital admission rates as a result of running out of medication, as well as assessment of additional balancing measures including call volume during business hours, will verify the favorability of this intervention. Quality of life assessments of physicians sharing call responsibility will determine if this intervention has resulted in diminished call fatigue aside from anecdotal improvement, thereby preventing physician burnout.
There are some limitations to this study. While data were collected over a full calendar year, covering all seasons, preintervention data were collected during the late spring, summer, and early fall months, while postintervention data were collected during the late fall, winter, and early spring months. It is possible the number of parent requests for refills varies by season. Continued data collection could potentially characterize this behavior. Two additional Children's Mercy campuses (Northland, East) where neurology patients are sometimes seen were not included in the signage posting, which could have affected the number of refill requests received. Urgency for refill requests was not clearly defined and could have affected the number of refill requests received.
Supplementary Material
ACKNOWLEDGMENT
The authors thank the Children's Mercy Fellow Continuous Quality and Practice Improvement course instructors and coaches for assistance in the development of the study design and Children's Mercy senior biostatistician Brian Lee, MPH, PhD, for assistance in statistical analysis.
Footnotes
Editorial, page 379
Supplemental data at Neurology.org/cp
AUTHOR CONTRIBUTIONS
B. Zuccarelli: study concept and design, acquisition of data, analysis and interpretation of data, draft of manuscript. K.A. Coffman: study supervision, critical revision of manuscript for intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
B. Zuccarelli reports no disclosures. K.A. Coffman serves on the editorial board of Journal of Child Neurology. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Rapoff MA. Adherence to Pediatric Medical Regimens. 2nd ed New York: Springer; 2010. [Google Scholar]
- 2.Aylward BS, Rausch JR, Modi AC. An examination of 1-year adherence and persistence rates to antiepileptic medication in children with newly diagnosed epilepsy. J Pediatr Psychol 2015;40:66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol 1997;50:105–116. [DOI] [PubMed] [Google Scholar]
- 4.Hallam L. Primary medical care outside normal working hours: review of published work. BMJ 1994;308:249–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ziebertz CM, van Hooff ML, Beckers DG, Hooftman WE, Kompier MA, Geurts SA. The relationship of on-call work with fatigue, work-home interference, and perceived performance difficulties. Biomed Res Int 2015;2015:643413. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.