Abstract
We describe an arthroscopic technique for the treatment of labral pathology and femoroacetabular impingement that provides excellent access to the central and peripheral compartments while preserving the biomechanically crucial components of hip joint stability. The hip capsule and the ligaments within it have been shown to be integral to hip biomechanical stability. Other popular techniques such as interportal and T-capsulotomy inherently damage the capsuloligamentous complex of the hip and can be associated with postoperative gross instability, micro-instability, heterotopic ossification, and seroma. Capsular closure may mitigate some of these effects but has been associated with capsular insufficiency and requires postoperative restrictions that can be prolonged. Our surgical technique focuses on careful portal placement, replacement when necessary, use of a switching stick to maximize peripheral compartment visualization, and joint access in the most minimally invasive manner while avoiding complications associated with extended capsulotomy. The objective of this Technical Note is to describe a technique by which full access to the joint can be obtained while not disrupting the biomechanics of the joint capsule.
The correction of femoroacetabular impingement and the labral pathology that accompanies this abnormality is a rapidly evolving segment of orthopedics. Although open surgical dislocation or a mini-open anterior approach were originally required to perform labral manipulation and femoral/acetabular osteoplasty, it has more recently been shown that arthroscopic procedures provide the same efficacy by a minimally invasive approach.1, 2 Because of the anatomic constraints of the hip joint, adequate visualization and access to pathology during arthroscopy present a challenge. Several methods of managing the hip capsule have become popular and are effective for overcoming these technical challenges.3 The hip capsule provides both static and dynamic stability to the joint and disruption of this structure and the ligaments within it has been implicated in postoperative pain, micro-instability, gross anterior dislocation, heterotopic ossification, and seroma formation.3, 4, 5 Management of this capsule has been a contentious issue in recent years.6
The most accepted current techniques of capsular management are interportal capsulotomy and T capsulotomy that fully expose the femoral head and femoral head-neck junction, respectively. Both of these techniques fully transect the iliofemoral ligament, which serves to resist anterior subluxation and stabilize extension.7 Bayne et al.8 showed that disruption of the capsule by today's popular techniques biomechanically alters the joint in a cadaver model. Biomechanics may be restored with routine capsular closure in the immediate operative period but some patients have been shown to develop capsular insufficiency despite closure, likely negating this restoration.9 Additionally, disruption of the capsule with repair requires postoperative restrictions of motion that can lead to postoperative pain and stiffness. We report on a surgical technique that avoids alteration of the capsule and therefore preserves native anatomy and biomechanics of the joint while evading potential complications.
Surgical Technique
Patient Positioning
The patient undergoes general anesthesia and is positioned supine on a hip traction table (Advanced Supine Hip Positioning System; Smith & Nephew, Andover, MA) against a perineal post wrapped in a viscoelastic surgical pad and plastic bag. The feet and ankles are well padded and placed in boots. The patient is fully paralyzed prior to the application of traction. The nonoperative leg is positioned under traction first at a 45° abduction angle from the bed to allow room for the C-arm. The operative leg is placed with the patella directly upward and the hip pushed into valgus by the perineal post (Fig 1). This position will achieve maximum joint accessibility and decrease the chances of iatrogenic damage to the cartilage or labrum by portal placement. The patient is draped and prepared in the usual sterile manner (Video 1).
Fig 1.
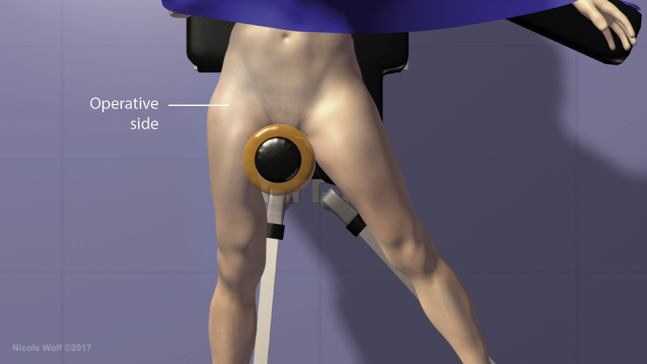
After induction and paralyzation, the patient is positioned supine on the hip traction table with an included perineal post. The feet and ankles must be well padded, with the nonoperative leg positioned under traction first at a 45° abduction angle. The operative leg (right) is placed with the patella directly upward and the hip pushed into valgus by the perineal post.
Arthroscopic Portal Placement
The anterolateral portal is established first under fluoroscopic guidance 1 cm anterior to the greater trochanter at a roughly 15° to 20° cephalad angle parallel to the floor. A 17-gauge cannulated needle and then nitinol wire shuttle, followed by a 5.0-mm obturator and cannula (Fig 2). This portal serves as the primary viewing portal for the placement of accessory portals. The anterior portal is established under arthroscopic visualization of the anterior triangle. The skin site for this portal is located at the intersection of a vertical line drawn at the anterior superior iliac spine and a horizontal line at the level of the anterolateral portal (Fig 3). The scope is then switched to the anterior portal and is used to visualize the anterolateral portal and confirm that it has not been placed through the labrum. The location that the anterolateral portal punctures through the capsule can be adjusted if it has violated the labrum or to better access pathology (Fig 4) (Table 1). If the labral pathology being addressed is located more superiorly along the acetabulum, the anterolateral portal can be adjusted anteriorly to aid in better visualization. The midanterior portal is placed at a location distal and equidistant from the anterior and anterolateral portals. The Dienst portal is placed one-third the distance between the anterior superior iliac spine and the anterolateral portal. If all portals are placed correctly, a quadrilateral arrangement is formed on the skin (Fig 5). Intermittent radiofrequency ablation can be used sparingly to create a rind around each of the portals and increase viewing and instrument maneuverability if desired. Ablation should only be used below the level of the capsule with a high fluid flow to avoid capsular and chondral injury (Video 1).
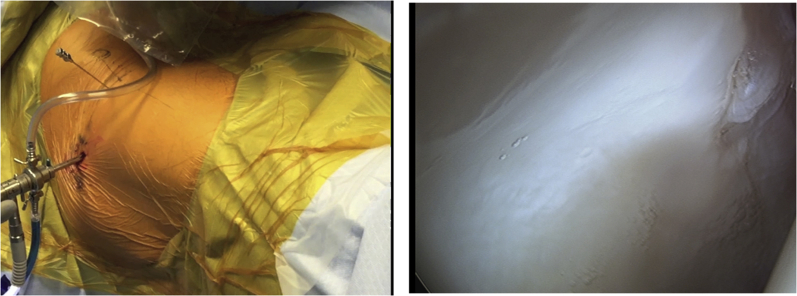
Fig 2.

The anterolateral portal is established first using fluoroscopic guidance 1 cm anterior to the (right) greater trochanter at a 15°-20° cephalad angle parallel to the floor with the patient in the supine position. A 17-gauge cannulated needle and then nitinol wire shuttle, followed by a 5.0-mm obturator and cannula are used.
Fig 3.
The anterior portal is established after the anterolateral portal, using the latter to arthroscopically visualize placement. The skin site for this portal is located at the intersection of a vertical line drawn at the anterior superior iliac spine and a horizontal line at the level of the anterolateral portal. The patient is in the supine position. The image on the right is of the hip labrum as viewed through the anterolateral portal.
Fig 4.
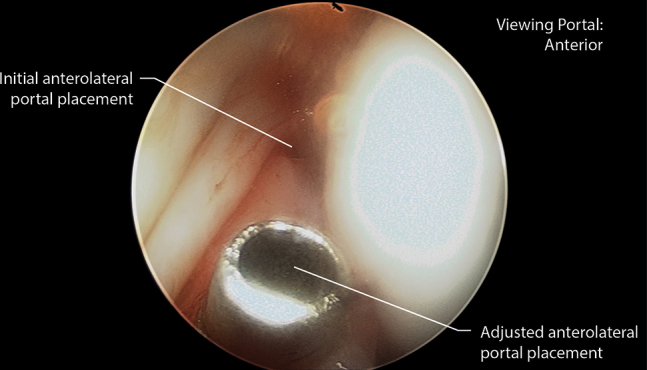
As seen through the anterior portal of the right hip with the patient supine, the location that the anterolateral portal punctures through the capsule can be visualized and adjusted if it has violated the labrum or to better access pathology.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Anterolateral portal can be readjusted while viewing through the anterior portal Radio-ablation to establish portals should only be used below the level of the capsule with high fluid flow If pincer lesions extend laterally, the working portal can be switched to the anterolateral portal A switching stick can be used through the anterior portal to push the capsule away from femoral cam lesions Additional portals can be made distal or proximal to the anterior portal to address medial and lateral cam lesions |
Significant surgical experience is required to address femoral lesions When placing the anterolateral portal, there is a potential for skiving of articular cartilage Excessive use of radioablation can damage articular surfaces if used above the level of the capsule or with insufficient fluid flow Very large cam lesions may require interportal or T-capsulotomy to address |
Fig 5.
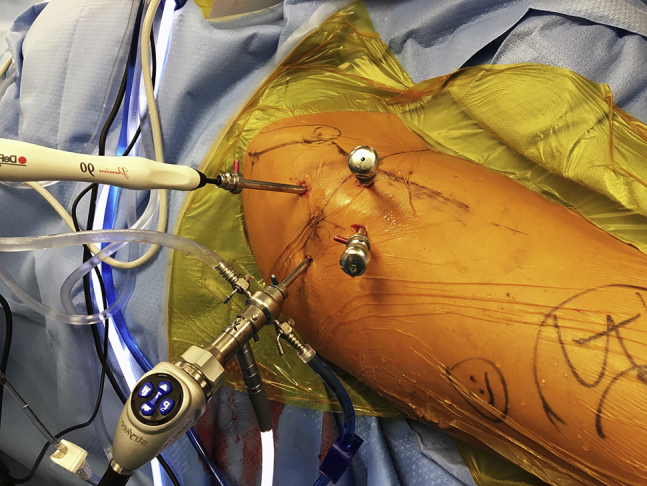
When all portals are placed correctly a quadrilateral arrangement is formed on the skin. The midanterior portal is placed at a location distal and equidistant from the anterior and anterolateral portals. The Dienst portal is placed one-third the distance between the anterior superior iliac spine and the anterolateral portal. This image depicts the right hip in the supine position.
Acetabuloplasty and Labral Fixation
Once adequate visualization of the lesion is obtained, a knife rasp inserted through the Dienst portal is used to elevate the capsule and labrum from the acetabulum starting 3 to 5 mm above the capsulolabral junction (Fig 6). Next, acetabular recession is performed with a 4-mm round abrader through the midanterior or Dienst portal while viewing through the anterolateral or midanterior portal. The burr is used on high-speed reverse mode to avoid disruption of the adjacent labrum and/or chondrolabral junction. The burr can be used directly up to the chondrolabral junction without perforating the junction due to the elastic properties of the junction, especially in the young patient (Fig 7). If the pincer extends laterally out of the reach of the anterior or midanterior portals, the working portal can be switched to the anterolateral portal while viewing through the anterior or midanterior portals (Table 1). The labrum is then secured to the newly recessed acetabular rim using 2.3-mm Osteoraptor suture anchors (Smith & Nephew) (Fig 8). The suture is shuttled between the Dienst and midanterior cannulae in a vertical mattress configuration with the knot tied away from the articular surface of the joint. The obturator and cannula of the midanterior portal can be redirected to pierce the capsule more medially or laterally to achieve ideal anchor placement or to more easily retrieve suture (Video 1).
Fig 6.
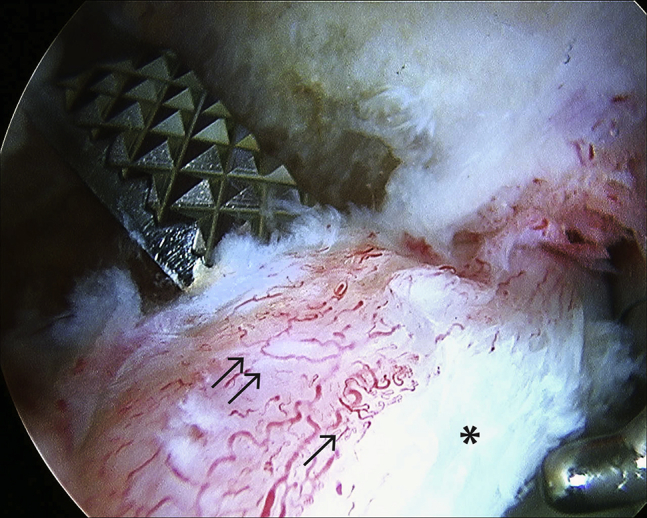
The first step in performing the acetabuloplasty is separation of the anterolateral labrum from the acetabulum. A knife rasp inserted through the Dienst portal is used to elevate the capsule and labrum from the acetabulum starting 3-5 mm above the capsulolabral junction. Arrows indicate the significant blood flow found at the capsulolabral junction that is preserved using this technique. The asterisk indicates the damaged labral surface. This image depicts the labrum of the right hip as viewed through the anterolateral portal with the patient in the supine position.
Fig 7.

The labrum of a young patient, seen here, is tolerant to direct contact from a 4-mm round abrader on high-speed reverse mode. The burr can be used directly up to the chondrolabral junction without perforating the junction because of the elastic properties of the junction. In older patients, direct contact of the burr to the labrum should be avoided. This image depicts the labrum of a left hip as viewed through the anterolateral portal with the patient in the supine position.
Fig 8.
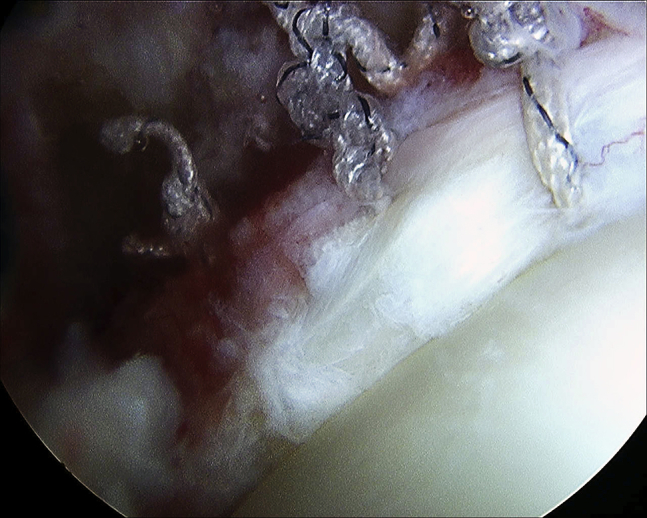
The labrum is secured to the recessed acetabular rim using 2.3-mm Osteoraptor suture anchors. Suture is shuttled between the Dienst and midanterior cannulae in vertical mattress configuration with the knot tied away from the articular surface of the joint. The suture can also be tied in looped fashion around the labrum as seen in the suture on the far right. This image depicts the labrum of the right hip as viewed through the anterolateral portal with the patient in the supine position.
Femoroplasty
Femoral cam lesions can be addressed with minimal changes to portal placement. Traction is released and the joint is flexed to 40° to 45° to relax the anterior capsule and access the peripheral compartment. A scope is introduced through the anterolateral portal and a switching stick is used through the anterior portal to improve visualization by pushing the capsule away from the femoral neck (Fig 9). An additional portal can be made distal or proximal to the anterolateral portal if the cam lesion is located more anteromedially or in the lateral gutter, respectively (Table 1). This portal is established using a spinal needle under fluoroscopy as a guide (Video 1).
Fig 9.
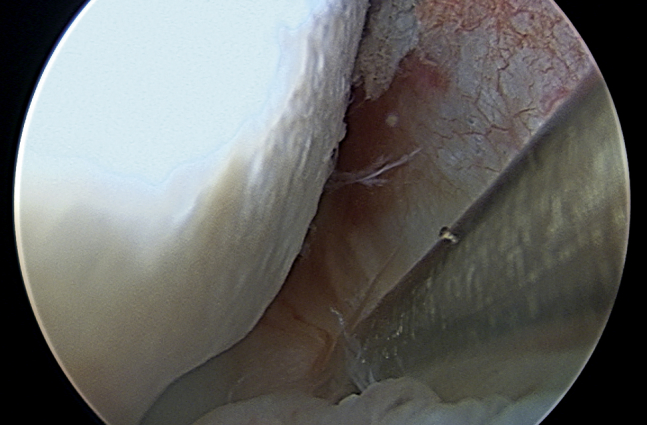
As the capsule has not been removed or reflected away from the peripheral compartment, a switching stick is often needed to push the capsule away from the femoral neck. This image depicts the labrum of the right hip as viewed through the midanterior portal with the patient in the supine position.
Postoperative Rehabilitation
Postoperatively, patients are encouraged to lightly weight bear with crutch assistance for 6 weeks. No braces or formal physical therapies are used. At 6 weeks, patients may use a stationary bike with no resistance. At 10 weeks, they may use an elliptical trainer on low resistance or swim with a paddle board. After 4 months, patients can begin lower extremity strengthening with short-arc leg presses and hamstring curls. Patients are allowed to then layer in activities with the goal of returning to normal function at 6 months postoperatively.
Discussion
Management of the hip capsule during arthroscopy for labral repair can have direct effects on the biomechanics of the joint as well as the development of complications. Both interportal and T capsulotomies have been associated with several clinically adverse events. Duplantier et al. reported a systematic review of a number of gross anterior dislocations after each type of capsulotomy, with or without capsular repair.4 Safran has proposed micro-instability as a source of postoperative pain in patients who have had extensive capsulotomy owing to compromise of the structural integrity of the capsule.5 McCormick et al. reported a cohort of patients who required revision arthroscopy in the absence of persistent femoroacetabular impingement and were found to have gross capsular irregularities at the site of previous capsulotomy.10 The development of heterotopic ossification has been linked to excessive soft tissue damage, and an intact capsule can help protect periarticular muscle from iatrogenic damage. In one study, 36% of patients undergoing hip arthroscopy with interportal capsulotomy developed heterotopic ossification regardless of capsular closure status.11 In addition to potential postoperative complications, the capsular closure of large capsulotomies requires limitation of extension and external rotation in the postoperative period. These limitations are associated with increased postoperative pain and stiffness.9 If extended T capsulotomy is utilized, the defect must be closed to seal the hip joint.
Our proposed technique of “puncture capsulotomy” has a number of advantages and avoids the pitfalls of the more popular techniques by innately preserving the anatomy and biomechanics of the hip joint (Table 2). The iliofemoral ligament, which is transected in both interportal and T-capsulotomy, is left intact in our technique, eliminating the possibility of gross anterior dislocation. The micro-instability and persistent pain that can occur with traditional capsulotomy are unlikely to occur with the minimally invasive puncture capsulotomy technique. Maintenance of the capsule also protects the soft tissues adjacent to the capsule from excessive trauma by instrumentation, which has been shown to lead to less postoperative pain and less development of heterotopic ossification.12 The postoperative range-of-motion limitations required after capsular closures can be avoided entirely with this technique.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Native biomechanics of the hip static stabilizers are preserved Iliofemoral ligament is preserved, eliminating risk of anterior dislocation Soft tissues are minimally disturbed, decreasing the risk of heterotopic ossification Postoperative range-of-motion restrictions are unnecessary |
Significant surgical experience required to address femoral lesions in particular Approach is not always ideal for pathologies such as loose bodies or pigmented villonodular synovitis |
The greatest limitation of this technique is technical difficulty. One of the more significant causes of failure in hip arthroscopy for femoroacetabular impingement is insufficient femoral osteoplasty, and significant surgical experience is required to address this pathology using puncture capsulotomy.13 We encourage redirection of cannulae when necessary for ideal placement of portals during the procedure. Another disadvantage of this approach to hip arthroscopy is its limited applicability when addressing pathologies such as very large cam lesions, loose bodies, or pigmented villonodular synovitis. These conditions may require more extensile capsulotomy to address appropriately (Table 2).
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video describes the patient positioning, portal placement, acetabuloplasty, and femoroplasty techniques that can be performed with minimal disruption of the hip capsule. This technique favors the use of puncture capsulotomy and careful portal placement and replacement over larger capsulotomies to access distant areas of the joint. This method preserves the native biomechanics of the hip capsule.
References
- 1.Ganz R., Gill T.J., Gautier E., Ganz K., Krugel N., Berlemann U. Surgical dislocation of the adult hip: A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A., Zaltz I., De La Torre K., Kelly B.T. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39:20s–28s. doi: 10.1177/0363546511412734. [DOI] [PubMed] [Google Scholar]
- 3.Harris J.D., Slikker W., 3rd, Gupta A.K., McCormick F.M., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–e94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duplantier N., McCulloch P., Nho S., Mathier R., III, Lewis B., Harris J. Hip dislocation of subluxation after hip arthroscopy: A systematic review. Arthroscopy. 2016;32:1428–1434. doi: 10.1016/j.arthro.2016.01.056. [DOI] [PubMed] [Google Scholar]
- 5.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Harris D. Capsular management in hip arthroscopy. Clin Sports Med. 2016;35:373–389. doi: 10.1016/j.csm.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Hewitt J.D., Glisson R.R., Guilak F., Vail T.P. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17:82–89. doi: 10.1054/arth.2002.27674. [DOI] [PubMed] [Google Scholar]
- 8.Bayne C.O., Stanley R., Simon P. Effect of capsulotomy on hip stability—A consideration during hip arthroscopy. Am J Orthop. 2014;43:160–165. [PubMed] [Google Scholar]
- 9.Domb B., Philippon M., Giordano B. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 10.McCormick F., Slikker W., Harris J.D. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
- 11.Amar E., Warschawski Y., Sampson T., Atoun E., Steinberg E., Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthroscopy. 2015;31:225–230. doi: 10.1016/j.arthro.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Bedi A., Kelly B.T., Khanduja V. Arthroscopic hip preservation surgery: Current concepts and perspective. J Bone Joint. 2013;95:10–19. doi: 10.1302/0301-620X.95B1.29608. [DOI] [PubMed] [Google Scholar]
- 13.Saadat E., Martin S.D., Thornhill T.S. Factors associated with the failure of surgical treatment for femoroacetabular impingement: Review of the literature. Am J Sports Med. 2014;42:1487–1495. doi: 10.1177/0363546513500766. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video describes the patient positioning, portal placement, acetabuloplasty, and femoroplasty techniques that can be performed with minimal disruption of the hip capsule. This technique favors the use of puncture capsulotomy and careful portal placement and replacement over larger capsulotomies to access distant areas of the joint. This method preserves the native biomechanics of the hip capsule.