Abstract
The crossing internal suture augmentation technique is an all-inside technique of anterior cruciate ligament reconstruction with augmentation of the hamstring tendon autograft with a braided ultrahigh-molecular-weight polyester–polyethylene suture tape resting on the adjustable cortical buttons on both the femoral and tibial sides. The internal suture augmentation acts as a backbone supporting and protecting the graft until the process of healing and ligamentization of the graft is completed. The ends of the suture tape are tied on the tibial button and additionally fixed to the tibia with a knotless anchor as a backup fixation with the knee in full extension. The technique has the advantages of being minimally invasive with small incisions and allowing preservation of the bone stock through the use of sockets. It also allows early return to activity thanks to the more secure rehabilitation and prevents early failure and stretching of the graft.
Advancement of arthroscopic techniques has led to development of techniques to improve outcomes. This is reflected in the management of anterior cruciate ligament (ACL) rupture, which has encountered numerous advancements in the past few years. The introduction of the trans-portal technique for drilling the femoral tunnel in the past 10 years1 resulted in a more anatomic placement with a better restoration of knee kinematics and reduction of osteoarthritis.2, 3 In addition, the use of different cortical fixation devices and the introduction of the all-inside technique for drilling of sockets instead of tunnels are proposed to achieve a more secure and conservative reconstruction with bone stock preservation.4
ACL reconstruction failure remains a problem that provokes further development and improvements of the currently used techniques. Failure of ACL reconstruction may be due to recurrent instability (either early or late), stiffness, or residual pain.5 Although the satisfaction rate after ACL reconstruction is reported to be high, the absolute number of failed reconstructions increased owing to the increased number of operated patients.6 Revision surgery is indicated if there is complete rupture of the graft, a grade 2 or 3 pivot-shift test, or subjective instability interfering with normal daily activities.7
The idea of augmenting a ligament repair or reconstruction has been proposed in many sites, including the medial collateral ligament, acromioclavicular joint, and posterior cruciate ligament, as well as performing ACL reconstruction with allograft. The aim is to protect the repair or the graft until complete healing and ligamentization occur.8 Preliminary results in a canine model showed good results with the use of a quadriceps tendon allograft with suture augmentation (i.e., a quadriceps tendon allograft with an internal brace) without the occurrence of synovitis or premature arthritis.9
In this article we describe an augmentation technique for ACL reconstruction using hamstring autograft with an ultrahigh-molecular-weight polyethylene–polyester tape fixed on both the femoral and tibial buttons in an all-inside manner. A backup fixation with a bio-knotless anchor (SwiveLock; Arthrex, Naples, FL) is added distal to the exit of the tibial socket.
The suture tape is believed to be integrated in the graft fibers and will protect them from acute failure and stretching in the early postoperative period between 6 and 12 weeks. In this period the graft is still undergoing healing and revascularization until complete ligamentization takes place. Loads exceeding the graft capacity during this time can lead to plastic deformation or even rupture.6, 10, 11
In addition, reduction of arthrofibrosis may be achieved by this technique because of the earlier and more secure rehabilitation with earlier restoration of the full range of extension.12 This is of particular benefit in revision cases. The advantages and disadvantages of the technique are summarized in Table 1. The described technique is basically a modification of the all-inside ACL GraftLink technique (Arthrex) described by Lubowitz4 incorporating the subsequent modification by Smith et al.13 and Smith and Bley14 (allograft with internal brace).
Table 1.
Advantages and Disadvantages of Crossing Internal Suture Augmentation Technique
| Advantages |
| Protection of the ACL graft from excessive accidental acute loads during the early postoperative period, thus preventing early failure due to implant failure |
| Protection of the ACL graft from excessive chronic loads that may result in stretching and relaxation of the graft |
| Possibility of more secure rehabilitation at an earlier phase, thus potentially being beneficial in contact and professional athletes and patients with a high BMI, as well as patients with osteoporosis |
| Expected special value when using allograft and when used in patients with a smaller graft diameter because of thin tendons |
| Disadvantages |
| Potential stress shielding if the tension of the FiberTape is higher than the tension of the graft—however, this point needs further research |
| Higher costs than the standard technique (cost of the additional FiberTape and the SwiveLock anchor) |
| Potential for over-tightening the joint and limitation of extension |
ACL, anterior cruciate ligament; BMI, body mass index.
Surgical Technique
The indications for the technique are patients with acute or chronic ACL complete ruptures (Video 1). The technique is thought to be advantageous in patients with a high body mass index (>30), contact and professional athletes, patients with osteoporotic bone, and patients undergoing a revision ACL reconstruction and in need of early rehabilitation.
Hamstring tendons are used for reconstruction, and graft preparation essentially follows the steps described by Lubowitz4 for preparation of the GraftLink construct. In addition, FiberTape (Arthrex) is used to augment the construct, extending between the femoral and tibial buttons and tied over the tibial button. Secondary backup fixation of the FiberTape into the tibia is performed with a Bio-SwiveLock anchor (Arthrex). Collagen-coated FiberTape is preferred because of the probable better tissue integration.
Use of a graft preparation station (Arthrex) allows easier preparation and tensioning of the tendon graft (Fig 1). A strong nonabsorbable suture is used for graft preparation (No. 2 FiberWire; Arthrex). The semitendinosus tendon alone is usually sufficient for preparation of a 4-fold graft of adequate diameter, usually not less than 8 mm. With a thinner graft diameter, the gracilis may be harvested and added to increase the bulk of the graft.
Fig 1.

Preparation and tensioning of semitendinosus tendon graft on a graft preparation station in a GraftLink configuration. Two TightRope buttons (arrows) are mounted on both arms of the preparation station with the quadruple folded semitendinosus tendon prepared between their loops.
The described technique is based on using 2 adjustable cortical suspensory devices (TightRope [Arthrex] or Rigidloop Adjustable [DePuy Synthes]) on both the femoral and tibial sides. The use of the no-button TightRope is optional on the tibial side for an easier and more secure fixation. After graft preparation as described with the GraftLink technique,4 a braided ultrahigh-molecular-weight polyethylene–polyester suture tape (No. 2 FiberTape) is passed through the holes of the femoral TightRope button so that both suture ends are directed inferiorly in line with the graft toward the tibial side (Fig 2). The graft initially should measure between 5 and 7 cm in length and should be tensioned on the graft preparation station to eliminate creep; however, the graft should not exceed 7.5 cm in length at the end. The graft is stitched in a circular fashion about 1 cm from the femoral end with a strong suture (No. 2 FiberWire). The starting point of stitching should be from within the graft to outside; the suture is then passed circumferentially around the graft 2 times and finally passed from outside to inside the graft to tie the knot within the material of the graft itself (Fig 3).
Fig 2.
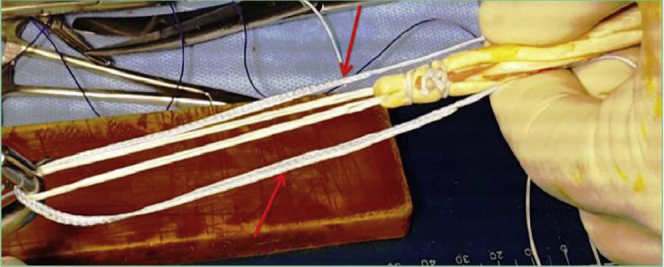
The 2 ends of the FiberTape suture are threaded through the holes of the femoral TightRope button from proximal to distal so that both suture ends are directed inferiorly in line with the graft (arrows).
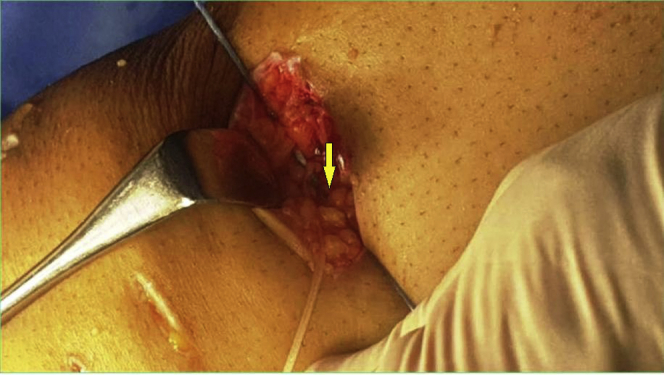
Fig 3.
The graft is stitched in a circumferential fashion with a No. 2 FiberWire about 1 cm from the femoral end (arrow). Care should be taken to ensure that the final knot will be buried within the substance of the graft (between its strands).
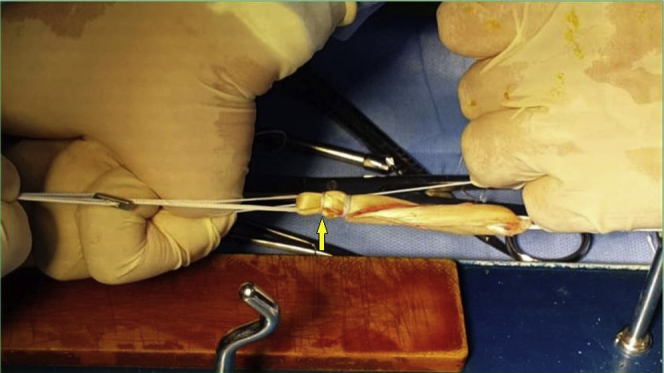
One end of the No. 2 FiberTape (which was passed through the TightRope button) is passed between the strands of the graft in the proximal 1 cm above the circumferential stitch and retrieved to the opposite side. The same is done with the other suture limb, which is passed in the opposite direction so that both sutures cross each other inside the proximal 1 cm of the graft (Fig 4). Both suture limbs are passed once again between the graft strands from each side to the other, crossing each other in the interval distal to the circumferential stitch (Fig 5). This ensures that the sutures will be completely covered by the soft tissue of the graft and will not appear intra-articularly. The low profile of the FiberTape will support the graft from inside without significantly increasing the overall graft diameter. The ends of the FiberTape are passed through the holes of the tibial-side TightRope button in line with its flipping FiberWire sutures (Fig 6). This step will be performed at a later stage (after graft passage) when using the no-button TightRope system.
Fig 4.
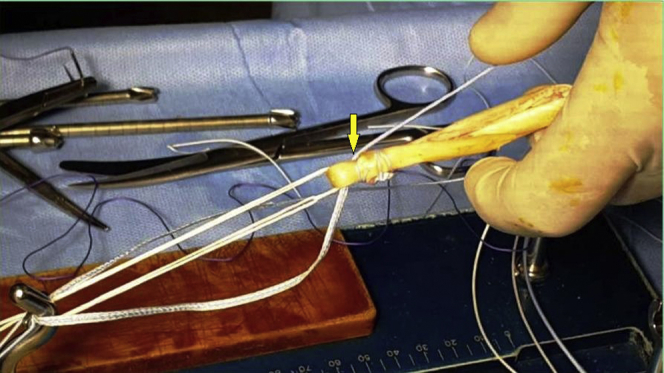
One end of the FiberTape (which was passed through the femoral button) is passed between the strands of the graft in the proximal 1 cm between the femoral end and the circumferential stitch to exit on the other side (arrow). The same is done for the other suture limb so that they cross each other within the substance of the proximal 1 cm of the graft.
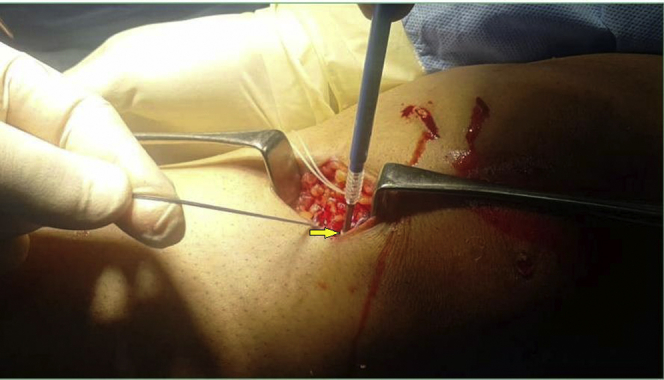
Fig 5.
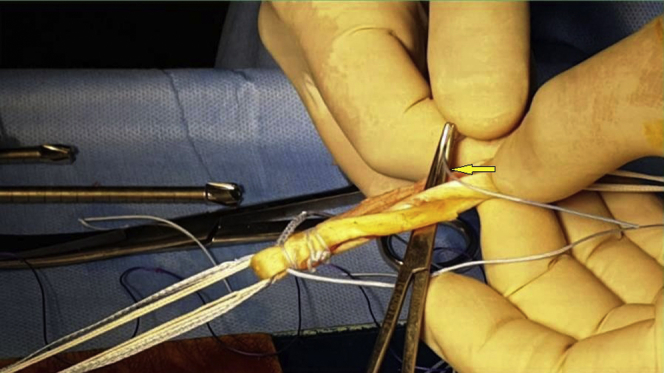
Both suture limbs are passed through the graft from each side to the other using a mosquito clamp (arrow) so that they cross each other inside the graft, in the interval distal to the circumferential stitch.
Fig 6.
The tapered ends of the FiberTape suture are passed through the button holes of the tibial TightRope (arrow) so that they are directed from superior toward the ends of the white tightening sutures.
The femoral and tibial ends of the graft are marked at a distance corresponding to the graft length planned to be placed inside the femoral and tibial sockets. This is usually 15 to 25 mm according to the available length of the graft, ensuring that at least 3 cm remains for the intra-articular length of the ACL. The overall graft length must be 1 cm shorter than the overall length of the intra-articular portion plus the intraosseous distance that will be traveled by the graft (Fig 7).
Fig 7.
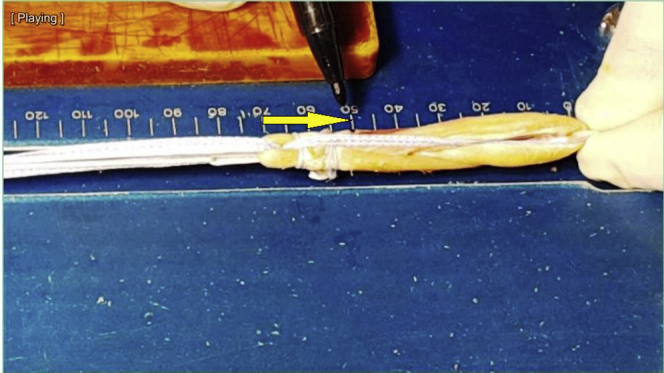
The graft length is measured (7 cm in this case) and marked at 2 cm from the femoral end (arrow) as well as from the tibial end (corresponding to the length of the intraosseous femoral and tibial sockets).
All-inside ACL reconstruction is performed using an anatomic single-bundle technique as described by Lubowitz.4 A FlipCutter (Arthrex) of the desired socket diameter can be optionally used to drill the femoral socket after its introduction in an outside-in manner according to the surgeon's preference. However, with this technique, it must be used on the tibial side to drill the socket to the desired length in a retrograde fashion (Fig 8). The graft is fixed first on the femoral side by pulling the traction sutures of the TightRope until it is flipped over the lateral femoral cortex. The TightRope system is tightened securely by pulling the shortening white sutures alternately to pull the graft into the femoral socket until the marks on the graft reach the femoral socket orifice. The FiberTape ends are pulled downward and tensioned carefully many times during tightening of the TightRope system (while pulling the graft upward). This is essential to avoid any slackness or redundancy of the FiberTape inside the graft. The tibial-side TightRope with FiberTape sutures is then passed through the tibial socket from the intra-articular side to outside the knee by use of a shuttle suture. The TightRope is flipped using the blue sutures.
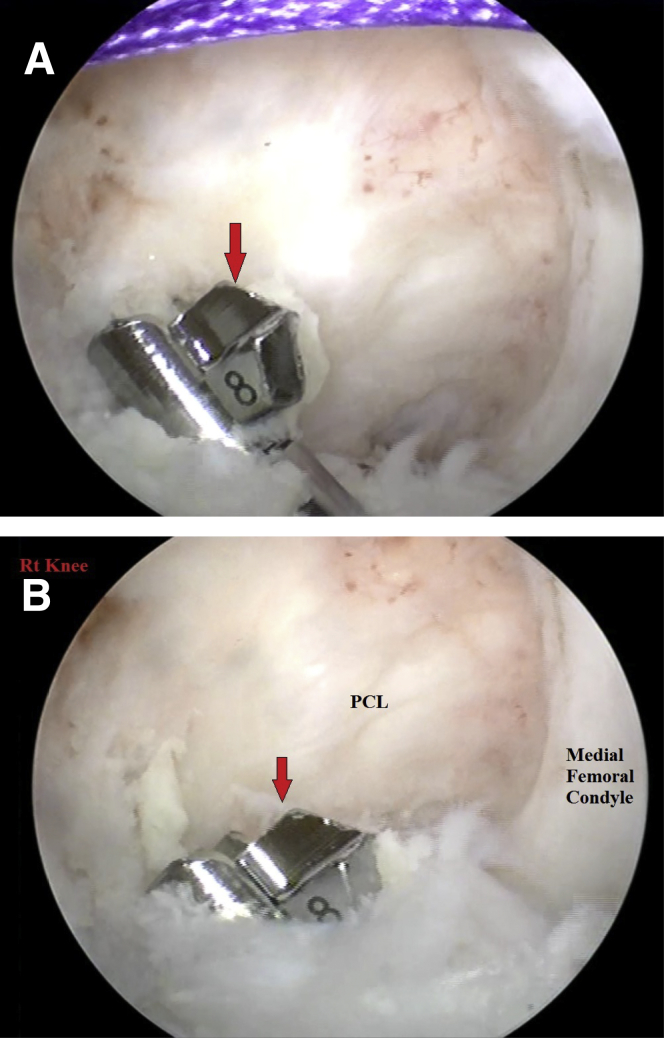
Fig 8.
Creation of the tibial socket with the FlipCutter (arrows) after flipping in the horizontal direction (A) in a retrograde fashion (B) to the desired length according to the available graft length (right [Rt] knee viewed from anterolateral portal in 90° of knee flexion). (PCL, posterior cruciate ligament.)
The knee is cycled in flexion and extension many times while traction is applied on the 4 suture limbs (2 white and 2 blue sutures) of the tibial TightRope (excluding the 2 ends of the FiberTape suture) to tension the graft. The shortening white sutures of the tibial TightRope, followed once again by the femoral TightRope system, are tightened firmly in 30° of knee flexion. The femur should be elevated to produce a posterior-drawer position of the tibia.
Next, an arthroscopic evaluation of the graft position and tension in the full range of motion, particularly in extension, should be performed (Fig 9). After secure fixation of the graft, the FiberTape is tightened by pulling its ends downward and is knotted over the tibial button with the knee in full extension (Fig 10). The ends of the FiberTape suture are then fixed to the tibia with a 5.5-mm Bio-SwiveLock anchor (Fig 11). A 4.5 mm drill is used to drill the tibia about 1.5 to 2 cm distal to the tibial TightRope button and anterior to the medial ligament, followed by tapping with the specific 5.5-mm tap. Because the cortical bone in this site is hard, this step is essential to avoid breakage of the anchor. The ends of the FiberTape suture are checked once again and pulled distally to ensure they are not trapped at any point through the graft or at the tibial TightRope button. The ends of the FiberTape suture are passed through the end of the Bio-SwiveLock anchor and fixed into the hole under continuous traction. The knee must be in full extension to avoid over-tightening of the knee and limitation of full extension later. Full range of motion of the knee is checked once again. A summary of the pearls and pitfalls of the technique is given in Table 2.
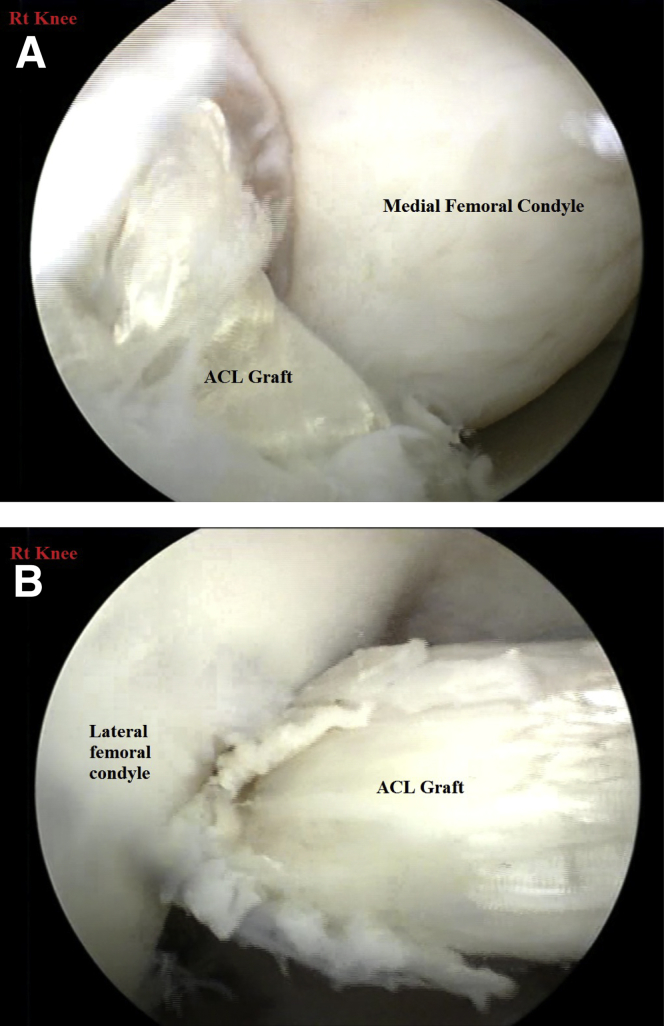
Fig 9.
Arthroscopic evaluation of the graft position in relation to the notch and assessment of its tension in both flexion (A) and extension (B) (right [Rt] knee viewed from anterolateral portal). (ACL, anterior cruciate ligament.)
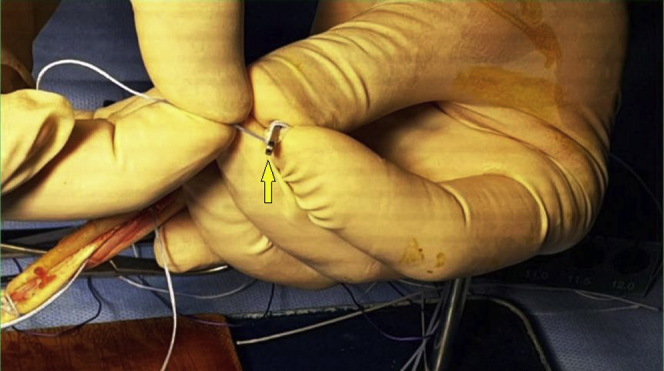
Fig 10.
After passage of the femoral and then the tibial TightRope buttons and tightening of the white shortening sutures, the FiberTape is tightened and knotted over the tibial button (arrow) with the knee in full extension (right knee in supine position in full extension).
Fig 11.
The ends of the FiberTape are fixed to the tibia 1 to 2 cm below the exit of the tibial socket (arrow) using a 5.5-mm Bio-SwiveLock anchor with the knee in full extension (right knee in supine position in full extension).
Table 2.
Pearls and Pitfalls
| Pearls |
| Good and meticulous preparation of the graft should be performed so that the FiberTape is completely buried inside the graft to avoid intra-articular exposure and possible synovitis or irritation of the articular surface. |
| The 2 ends of the FiberTape should be pulled separately and independently on the graft after tightening both the femoral TightRope and tibial TightRope to ensure that the suture is not redundant inside the graft material. |
| Pitfalls |
| The surgeon should avoid over-tightening during fixation of the FiberTape using the Bio-SwiveLock by keeping the knee in full extension and checking ROM immediately thereafter. |
ROM, range of motion.
Postoperative Rehabilitation
The higher degree of stability believed to result from this technique allows immediate postoperative full weight bearing and full range of motion, as tolerated by the patient and permitted by the state of quadriceps and muscular control of knee movement. Return to full and active competitive sports can be permitted after 6 to 9 months postoperatively. A hinged knee brace is recommended for a minimum of 6 weeks after surgery and adjusted to allow knee motion from 0° to 120°.
Discussion
Our technique is essentially an all-inside ACL reconstruction as described by Lubowitz4 with the GraftLink preparation. In addition, a FiberTape suture is placed in the core of the hamstring graft extending between both the femoral and tibial adjustable cortical buttons.
Protection of the ACL graft during early postoperative activities is mandatory to prevent stretching and failure of the reconstruction. The idea of using an internal brace to protect a ligamentous repair is already well known, and internal bracing is performed in many sites such as the medial collateral ligament and Achilles tendon.4, 14 The use of the internal brace to splint the hamstring tendon autograft is theoretically beneficial to allow an early postoperative rehabilitation program that can also prevent arthrofibrosis. This can increase the degree of patient satisfaction with the results. The technique needs further laboratory and clinical evaluations to evaluate the actual results, as well as the effect of elimination of part or all of the stresses on the actual ligamentization of the graft and the clinical behavior of the resultant collagen fibers. The question of possible stress shielding remains unanswered and requires histologic evaluation of the graft after the end of the proposed ligamentization process. In addition, radiologic evaluation of the sockets is mandatory to assess whether there is any effect of the FiberTape on the bony walls of the femoral and tibial sockets' diameters with time. An advantage of the internal brace is the possibility of earlier achievement of a more secure range of motion as well as weight bearing while protecting the repair site during the early rehabilitation phase.
Similar techniques for preparation of the ACL graft tendon have been described using allograft tissue,9, 14 in which a FiberTape is used to secure the construct until the healing process is finished, which usually takes a longer time when using an allograft. However, in such a technique, the FiberTape is suspended over the suture loop of the femoral TightRope, which we think may be a weak point and may be subject to earlier loosening or even failure of the loop of the femoral TightRope because of the higher stresses. In addition, there is a possible sawing effect of the hard FiberTape on the suture loop of the femoral TightRope.
In our technique the FiberTape is looped through the femoral TightRope button and passed through and knotted over the tibial TightRope button. Therefore, there will be mostly no chance of a change in the length of the FiberTape between the femoral and tibial buttons, particularly when the ends of the FiberTape are fixed to the tibia through the knotless SwiveLock anchor. This results in neutralization of the forces over the knot on the tibial TightRope button. Our technique can be used with both allograft and autograft to minimize the chances of stretching and failure. Special indications for its use with autograft were mentioned earlier. The technique is completely different from the artificial ligament systems described in the literature to be used alone for ACL reconstruction.
Footnotes
The authors report the following potential conflict of interest or source of funding: A.B.I. receives support from Arthrex, Arthrosurface, Medi Bayreuth. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Crossing internal brace technique for augmentation of all-inside anterior cruciate ligament graft preparation using femoral and tibial TightRope system. A FiberTape suture is used to augment the GraftLink construct extending between both the femoral and tibial buttons. The ends of the FiberTape sutures are tied over the tibial button and further fixed to the tibia by use of a Bio-SwiveLock knotless anchor with the knee in full extension.
References
- 1.Steiner M.E., Battaglia T.C., Heming J.F., Rand J.D., Festa A., Baria M. Independent drilling outperforms conventional transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:1912–1919. doi: 10.1177/0363546509340407. [DOI] [PubMed] [Google Scholar]
- 2.Nicholson J.A., Sutherland A.G., Smith F.W. Single bundle anterior cruciate reconstruction does not restore normal knee kinematics at six months: An upright MRI study. J Bone Joint Surg Br. 2011;93:1334–1340. doi: 10.1302/0301-620X.93B10.26481. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N., Longo U.G., Gougoulias N., Loppini M., Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–25. doi: 10.1136/bjsm.2009.069526. [DOI] [PubMed] [Google Scholar]
- 4.Lubowitz J.H. All-inside anterior cruciate ligament graft link: Graft preparation technique. Arthrosc Tech. 2012;1:e165–e168. doi: 10.1016/j.eats.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Kamath G.V., Redfern J.C., Greis P.E., Burks R.T. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 7.Noyes F.R., Barber-Westin S.D. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131–1143. doi: 10.2106/00004623-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Nancoo T.J., Lord B., Yasen S.K., Smith J.O., Risebury M.J., Wilson A.J. Transmedial all-inside posterior cruciate ligament reconstruction using a reinforced tibial inlay graft. Arthrosc Tech. 2013;2:e381–e388. doi: 10.1016/j.eats.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook J.L., Smith P., Stannard J.P. A canine arthroscopic anterior cruciate ligament reconstruction model for study of synthetic augmentation of tendon allografts. J Knee Surg. 2017;30:704–711. doi: 10.1055/s-0036-1597618. [DOI] [PubMed] [Google Scholar]
- 10.Clancy W.G., Jr., Narechania R.G., Rosenberg T.D., Gmeiner J.G., Wisnefske D.D., Lange T.A. Anterior and posterior cruciate ligament reconstruction in rhesus monkeys. J Bone Joint Surg Am. 1981;63:1270–1284. [PubMed] [Google Scholar]
- 11.Drez D.J., Jr., DeLee J., Holden J.P., Arnoczky S., Noyes F.R., Roberts T.S. Anterior cruciate ligament reconstruction using bone-patellar tendon-bone allografts. A biological and biomechanical evaluation in goats. Am J Sports Med. 1991;19:256–263. doi: 10.1177/036354659101900308. [DOI] [PubMed] [Google Scholar]
- 12.Getelman M.H., Friedman M.J. Revision anterior cruciate ligament reconstruction surgery. J Am Acad Orthop Surg. 1999;7:189–198. doi: 10.5435/00124635-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Smith J.O., Yasen S.K., Palmer H.C., Lord B.R., Britton E.M., Wilson A.J. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845–1851. doi: 10.1007/s00167-016-4150-x. [DOI] [PubMed] [Google Scholar]
- 14.Smith P.A., Bley J.A. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. doi: 10.1016/j.eats.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Crossing internal brace technique for augmentation of all-inside anterior cruciate ligament graft preparation using femoral and tibial TightRope system. A FiberTape suture is used to augment the GraftLink construct extending between both the femoral and tibial buttons. The ends of the FiberTape sutures are tied over the tibial button and further fixed to the tibia by use of a Bio-SwiveLock knotless anchor with the knee in full extension.