Abstract
PURPOSE
A recently identified and treatable cause of spontaneous intracranial hypotension (SIH) is cerebrospinal fluid (CSF)-venous fistula, and a recently described computed tomography myelogram (CTM) finding highly compatible with but not diagnostic of this entity is the hyperdense paraspinal vein sign. We aimed to retrospectively measure the prevalence of the hyperdense paraspinal vein sign on CTMs in SIH patients without dural CSF leak, in comparison with control groups.
METHODS
Three CTM groups were identified: 1) SIH study group, which included dural CSF leak-negative standard CTMs performed for SIH, with early and delayed imaging; 2) Early control CTMs, which were performed for indications other than SIH, with imaging shortly after intrathecal contrast administration; 3) Delayed control CTMs, which included delayed imaging. CTMs were retrospectively reviewed for the hyperdense paraspinal vein sign by experienced neuroradiologists, blinded to the group assignment. All CTMs deemed by a single reader to be positive for the hyperdense paraspinal vein sign were independently reviewed by two additional neuroradiologists; findings were considered positive only if consensus was present among all three readers. For positive cases, noncontrast CTs and prior CTMs, if available, were reviewed for the presence of the sign.
RESULTS
Seven of 101 (7%) SIH patients had contrast in a spinal/paraspinal vein consistent with the hyperdense paraspinal vein sign; no patient in either control group (total n=54) demonstrated the hyperdense paraspinal vein sign (P = 0.0463). The finding occurred only at thoracic levels. Each patient had a single level of involvement. Six (86%) occurred on the right. Four occurred in female patients (57%). The sign was seen on early images in 3 of 7 cases (43%) and on both early and delayed images in 4 of 7 cases (57%). In 2 of 7 patients (29%), a noncontrast CT covering the relevant location was available and negative for the sign. A prior CTM was available in 2 of 7 patients (29%), and in both cases the hyperdense paraspinal vein sign was also evident.
CONCLUSION
The prevalence of the hyperdense paraspinal vein sign in SIH patients with dural CSF leak-negative standard CTM was 7%. As the sign was not seen in control groups, this sign is highly compatible with the presence of CSF-venous fistula. Since the CTMs were not specifically dedicated to identifying hyperdense paraspinal veins (i.e., they were not dynamic and were not preceded by digital subtraction myelography), the true prevalence of the sign may be higher. Radiologists should scrutinize conventional CTMs for this sign, especially in patients in whom a traditional dural CSF leak is not identified.
Spontaneous intracranial hypotension (SIH) is caused by a spinal dural cerebrospinal fluid (CSF) leak in nearly all cases. The symptoms of SIH can be debilitating and include headache, nausea, vision difficulties, tinnitus, and in more advanced cases, gait disturbance, personality change, and decreased level of consciousness (1). In some cases of SIH, an extradural CSF collection or a leaking diverticulum is present, helping to localize the leak (2, 3). However, in many cases, a cause for the condition is not identified, especially when spinal imaging does not reveal such a collection. In 2014, Schievink et al. (4) reported a series of 3 patients without a traditional CSF leak through a dural defect, but with a novel finding of a direct fistula between the subarachnoid space and paraspinal/spinal epidural veins (a CSF-venous fistula, or CVF) on digital subtraction myelography (DSM) (4). In 2016, Kranz et al. (5) reported an additional 3 cases of surgically confirmed CVF, which were visualized on computed tomography myelography (CTM) as hyperdense paraspinal veins (5). Several additional similar cases have recently been reported (6). The prevalence and operating characteristics of this finding of a hyperdense spinal/paraspinal vein on CTM without other identifiable cause of SIH have not been established. It is important to characterize the prevalence of this finding on CTM, since CTM is likely to be the initial imaging modality to evaluate for a spinal CSF leak in most practices.
The purpose of this study was to retrospectively measure the prevalence of the hyperdense paraspinal vein sign on CTMs in SIH patients without dural CSF leak, in comparison with control groups.
Methods
Institutional review board approval with waived consent was obtained for this Health Insurance Portability and Accountability Act-compliant retrospective research study. All included patients provided authorization for data to be used in research.
Subjects
Three CTM groups were identified: 1) SIH: the study group of patients with clinically diagnosed SIH but a dural CSF leak-negative CTM; 2) Early Control: a control group of patients who underwent CTM for other indications (e.g., degenerative disc disease, back pain) in which CT images were obtained shortly after intrathecal administration of contrast; 3) Delayed Control: a control group of patients who underwent CTM prior to a thermal spine ablation procedure, in which CT images were obtained in delayed fashion following intrathecal contrast administration.
SIH group: A search was performed for CTMs without description of a leak in the radiology report between March 2010 and September 2015, performed for an indication of leak, CSF hypotension, low pressure, SIH or siderosis (related to SIH). We limited our review to patients with clinically diagnosed SIH by neurologists with expertise in SIH, excluding patients with any history of antecedent trauma or spine interventions deemed by the referring clinician to be related to the onset of intracranial hypotension. If a patient had more than one CTM performed during the date range, only the most recent study was included. The search was extended back in time until approximately 100 patients with the appropriate inclusion criteria were identified.
Early Control: A search was performed for CTMs between June 2015 and October 2015, performed for an indication other than SIH. CTMs of only the cervical spine were excluded. CTMs were also excluded for the following reasons: shunt evaluation, cisternography, mixed subdural-subarachnoid injection of contrast, or if the CTM was part of a thermal spine ablation procedure (i.e., Delayed Control patients, see below). The search was extended back in time until approximately 50 patients with the appropriate inclusion criteria were identified. The group was intentionally smaller than the SIH group because of the suspected low pretest probability of finding a hyperdense paraspinal vein sign in a population of patients not suffering from SIH.
Delayed Control: The above search for Early Control patients revealed a small number of patients (n=6) who had recently undergone CTM as part of a thermal spine ablation procedure; these were included as a second control group. The group was much smaller, again due to the low pretest probability, and also due to the inherently smaller available population of such patients in our practice.
CTM technique
Our standard CTM protocol is as follows: a lumbar puncture is performed by using a 22-gauge spinal needle and fluoroscopic guidance. Intrathecal localization is confirmed with a small test injection, and approximately 16 mL of iohexol 180 (Omnipaque 180; GE Healthcare) is injected under fluoroscopic visualization. Spot images are taken of the lumbar, thoracic, and cervical spine, following the contrast while the patient is gradually placed in the Trendelenburg position. The patient is rolled several times to evenly distribute the contrast and transferred to the CT scanner. CTMs are imaged on either a 64- or 128-section scanner with a minimum axial section thickness of 0.75 mm and additional reconstructions in the coronal and sagittal planes. In patients with a high clinical suspicion of SIH and no definite CSF leak on initial CTM images, delayed CT imaging at 2–4 hours is performed.
The median time elapsed from intrathecal contrast administration (time of initial saved fluoroscopic image) to the initial CTM series was 29 min (SIH group, n=101) and 32 min (Early Control, n=48). The median time from contrast administration to delayed CT images was 188 min (SIH group, n=91). In the 6 Delayed Control CTMs, the “initial” CT series was relatively delayed (median interval from initial saved fluoroscopic image was 104 min), with a median interval of 127 min (n=4), 175 min (n=4), and 213 min (n=3) for the subsequent 3 series, respectively.
CTM review
SIH and Early Control cases were reviewed by one of eight experienced board-certified, fellowship-trained, staff neuroradiologists, each of whom has interest in spine imaging and image-guided procedures and routinely works with this patient population. The reviewing radiologist was blinded to the indication for the CTM and the CTM group assignment. The number of readers was high in order to accommodate the significant time expended for imaging review of each case, which were entire spine CTMs with both initial and in nearly all cases delayed images, reviewed in two planes for subtle abnormalities, as described below. Each reader reviewed 12 to 13 SIH group and 5 to 7 Early Control CTMs. Three neuroradiologists including the senior author reviewed all of the Delayed Control CTMs, unblinded to the indication, as ablation needles were typically in place. Reviewers were asked to evaluate the presence of a hyperdense spinal/paraspinal vein (a linear-curvilinear opacity extending from the thecal sac or a nerve root sleeve) (5). Readers reviewed both initial and, when available, delayed CT series. Readers reviewed thin (0.75 mm) section axial images and reformatted coronal images at each spinal level included in the study. Because there is no reference standard for Hounsfield unit (HU) cutoff for the hyperdense paraspinal vein, the determination was made on a subjective basis, not with region-of-interest (ROI) measurement.
Though the hyperdense paraspinal vein finding was subjective, reviewers were asked to only deem the CTMs as positive if they had a very high level of suspicion (i.e., only if they would interpret the studies as positive clinically). All CTMs deemed by a single reader to be positive for a hyperdense paraspinal vein were independently reviewed by two additional neuroradiologists; only if consensus was present among all three readers were the findings considered positive.
For each case considered positive, three additional steps were performed. First, the maximum CT number (in HU) of the hyperdense paraspinal vein finding on the 0.75 mm axial image best demonstrating the finding was determined based on ROI analysis by one of the readers. Second, noncontrast CTs covering the relevant location, if available, were evaluated subjectively by one of the readers for this finding at the designated level. This was performed to ensure that the hyperdense paraspinal vein finding on CTM was truly representative of contrast material, rather than calcification, thrombosis or other cause of hyperdensity. Third, for each case considered positive, prior CTMs covering the relevant location, if available, were evaluated subjectively by one of the readers for this finding at the designated level.
The readers evaluating the CTMs also reviewed all respective saved fluoroscopic images for evidence of a hyperdense paraspinal vein. Several time points were recorded: initial saved fluoroscopic image after intrathecal contrast administration, initial CT series, and if available, any delayed CT series. Relevant time intervals were calculated with respect to the initial saved fluoroscopic image after intrathecal contrast.
Clinical data
For patients in whom the CTM was positive for a hyperdense paraspinal vein, clinical information including presence of headache or other symptoms and duration of symptoms was recorded from review of the electronic medical record. The original radiology report was reviewed to assess if the hyperdense paraspinal veins were described.
Statistical analysis
The relative prevalence of the hyperdense paraspinal vein sign in the SIH group and the combined Early and Delayed Control groups was compared using a Fisher’s exact test. A one-tailed P value of <0.05 was considered statistically significant.
Results
The study design is summarized in Table 1. Forty-eight CTMs were excluded from the SIH group search results (n=149) for the following reasons: iatrogenic leak (n=22), traumatic leak (n=14), prior dural CSF leak (n=4), and a more recent CTM was available and included (n=8). Twenty-six CTMs were excluded from the Early Control search results (n=74) for the following reasons: only the cervical spine was included (n=15), the myelographic study was a shunt evaluation or cisternography (n=4), the study was performed for evaluation or follow-up of a dural CSF leak (n=1), a mixed subdural-subarachnoid injection occurred (n=1), or the studies were part of an ablation procedure and comprised the Delayed Control search results (n=5). No mixed subdural-subarachnoid injections occurred in the SIH Study Group or Delayed Control groups. The final group sizes for the study were: SIH (n=101), Early Control (n=48), and Delayed Control (n=6).
Table 1.
Study design: inclusions and exclusions for the three CTM groups
| Early Control (CTM for non-SIH indications, early CT images) | SIH study group (SIH, dural CSF leak negative CTM) | Delayed Control (CTM prior to spine ablation, late CT images) | |
|---|---|---|---|
| Patients from initial database search, n | 149 | 74 | 6 |
| Exclusion reason, n | Iatrogenic leak (22) Traumatic leak (14) Prior CSF leak (4) More recent CTM available (8) |
Cervical only CTM (15) CTM for shunt evaluation or cisternography (4) CSF leak present (1) Mixed subdural-intrathecal injection (1) Qualified for delayed control group (5) |
None |
|
| |||
| Total excluded patients, n | 48 | 26 | 0 |
|
| |||
| Total included patients, n | 101 | 48 | 6 |
CTM, computed tomography myelogram; SIH, spontaneous intracranial hypotension; CSF, cerebrospinal fluid.
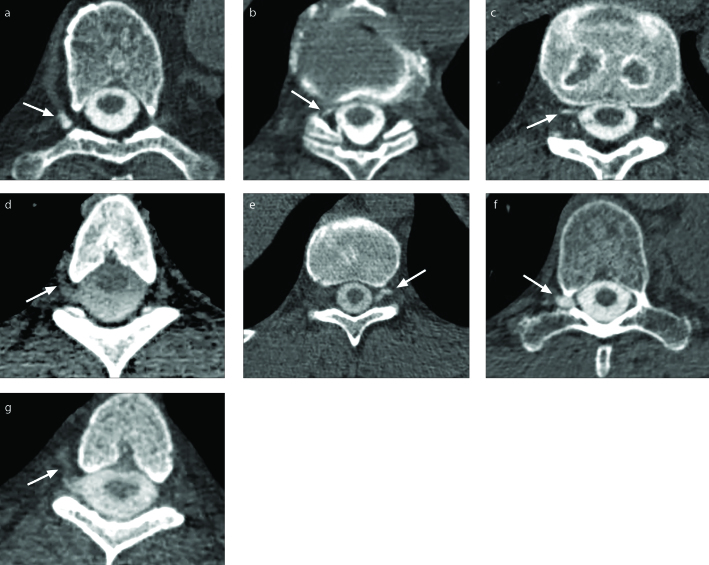
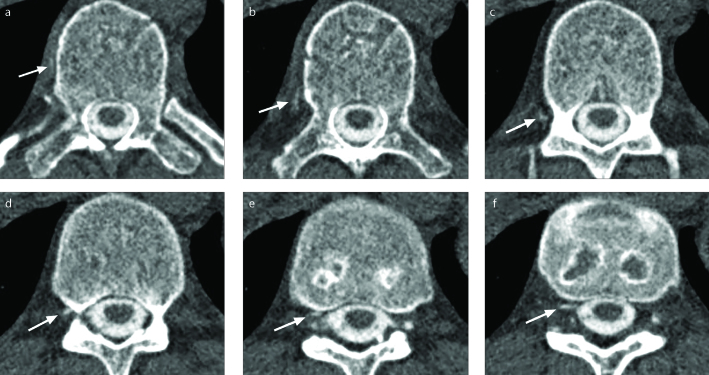
In the SIH group, 7% (7/101) of CTMs were positive for the hyperdense paraspinal vein sign, with consensus agreement in each case by independent review by three neuroradiologists. Representative single axial images from each of the 7 CTMs positive for the hyperdense paraspinal vein sign are depicted in Fig. 1; note that the sign is much more easily appreciated when scrolling through axial images. Fig. 2 demonstrates several axial images from one of these 7 CTMs positive for the sign. None of the 54 CTMs in either control group were positive for the sign. The difference in prevalence of the sign in the SIH group (7/101) and combined control groups (0/54) was statistically significant, P = 0.0463. For the 7 positive cases as a group, the mean and median of the maximum radiodensity of the sign in each individual case were 364 and 399 HU, respectively (range, 99–567). For these 7 cases, a prior or subsequent noncontrast CT covering the relevant location was available in 2 (29%); these unenhanced examinations did not demonstrate a hyperdensity in the respective region of the hyperdense paraspinal vein finding seen on CTM (cases A and F in Fig. 1, Table 2). A prior CTM was available in 2 of 7 cases (29%), preceding the reference CTM by 9 and 8 months (cases D and E, respectively in Fig. 1, Table 2); in both cases, the same hyperdense paraspinal vein finding was evident.
Figure 1. a–g.
Seven cases with a hyperdense paraspinal vein sign on computed tomography myelogram (CTM). Panels (a–g) show a single representative axial CTM image from each case (cases A–G). A contrast opacified hyperdense spinal/paraspinal vein (arrow) is present on each CTM. The characteristics of each patient/CTM are summarized in Table 2. Note that the hyperdense paraspinal vein is better appreciated on consecutive images, as viewed electronically at a picture archiving and communication system (PACS).
Figure 2. a–f.
Case C, hyperdense paraspinal vein sign on CTM. Several representative axial CTM images from case C at T11–12 are ordered from superior to inferior. These demonstrate a linear-curvilinear high attenuation structure extending anteriorly from the right aspect of the thecal sac/nerve root sleeve to the right lateral aspect of the vertebral body, i.e., a hyperdense paraspinal vein sign, compatible with a cerebrospinal fluid venous fistula. The maximum radiodensity of this structure is 419 HU.
Table 2.
Clinical and CTM characteristics of SIH patients with a hyperdense paraspinal vein sign
| Case | A | B | C | D | E | F | G |
|---|---|---|---|---|---|---|---|
| Age (years) | 55 | 84 | 36 | 37 | 54 | 59 | 44 |
| Gender | Male | Female | Male | Female | Female | Female | Male |
| Presenting symptoms | Headache, midthoracic discomfort, mental fogginess, chronic fatigue | Headache, vision changes, imbalance, fatigue, nausea, vomiting | Postural headache, vision changes, nausea, vomiting | Postural headache, nausea, vomiting | Postural headache, nausea | Exertional headache | Postural and exertional headache |
| Duration of symptoms | 2.5 years | 2 months | 2 years | 1 year | 1 year | 4 years | 1 year |
| Level and laterality of hyperdense paraspinal vein sign | T7–T8; Right | T10–T11; Right | T11–T12; Right | T4–T5; Right | T11–T12; Left | T9–T10; Right | T3–T4; Right |
| Maximum radiodensity (HU) | 567 | 384 | 419 | 155 | 399 | 525 | 99 |
| Presence of sign on prior CTM | N/A | N/A | N/A | Present, 9 months prior | Present, 8 months prior | N/A | N/A |
| Presence of hyperdensity on noncontrast CT | Not present, chest CT 1 week prior | N/A | N/A | N/A | N/A | Not present, subsequent CT procedure planning images 1 month later, or CT of PET-CT 8 months prior | N/A |
CTM, computed tomography myelogram; SIH, spontaneous intracranial hypotension; HU, Hounsfield units; N/A, not available; PET-CT, positron emission tomography – computed tomography.
Additional patient and CTM characteristics of the 7 cases positive for the hyperdense paraspinal vein sign are listed in Table 2. The mean patient age was 53 years (range, 36–84 years) and 57% (4/7) were female. Headache was a presenting symptom in all 7 patients. Additional presenting symptoms included nausea and/or vomiting, cognitive changes, fatigue, imbalance, vision changes and back discomfort. Mean duration of symptoms was 1.7 years (range, 2 months to 4 years). Each hyperdense paraspinal vein sign occurred at a thoracic level. Of the hyperdense paraspinal veins, 86% (6/7) occurred on the right. No patient had more than one site demonstrating the sign. The sign was seen on early images and not on delayed images in 43% of the cases (3/7), and on both early and delayed images in 57% of cases (4/7).
Fluoroscopic myelography images did not demonstrate a correlative hyperdense paraspinal vein in any patient from any of the three groups. In only one case did the original radiology report describe “a thin curvilinear area of extradural contrast material” (at the same side and level as the hyperdense paraspinal vein found by the study reviewers), but the finding was described to be of uncertain clinical significance.
Discussion
SIH is an often debilitating condition caused most commonly by a spinal dural CSF leak. In some cases, however, such a leak cannot be demonstrated on CTM and nontargeted minimally invasive therapy such as large volume single site or multilevel blood patches may not be effective. A recently discovered entity responsible for SIH in some such standard CTM dural CSF leak-negative patients is CVF. This entity can be evident on myelographic imaging, and if discovered, targeted therapy can be pursued, including directed blood patch and/or surgery. For example, identification of the hyperdense paraspinal vein sign on CTM can help guide surgical ligation of the fistula site.
Our study suggests that the hyperdense paraspinal vein sign has a prevalence of at least 7% in patients with SIH who have a dural CSF leak-negative standard CTM. The sign was not seen in control patients, with the difference in prevalence statistically significant. The sign is highly compatible with the presence of a CVF. This result is relevant because it warrants that this sign be specifically sought on routine CTM, which is typically the first myelographic modality used to evaluate the spine in SIH patients. The sign should specifically be sought on standard CTM when this study does not demonstrate a typical dural CSF leak. While more work is required to define the operating characteristic of the sign, given present knowledge, if unequivocal CTM evidence for this sign is found, further dedicated imaging (e.g., DSM) may be obviated. Meanwhile, in a case where the CTM evidence is equivocal, dedicated imaging with DSM may be warranted. In either case nondiagnosis and nontargeted therapies may be obviated. In our series, the early (initial) CTM series more often demonstrated the sign than the delayed series, although in several cases it was visualized on both. We emphasize that we do not advocate standard CTM as a dedicated technique for specifically evaluating CVF at a given level (dedicated studies such as DSM are better-suited). However, standard CTM remains the optimal initial myelographic modality for evaluating SIH patients, and the hyperdense paraspinal vein sign should be sought on such standard CTM, especially in dural-leak negative examinations.
Although the hyperdense paraspinal vein sign is not absolute proof of the presence of CVF, there were no positives in the control groups in the current study, nor are we aware of false positives in our anecdotal experience or in the published literature. Several observations about this recently described condition are relevant. CVF first appeared in the literature in 2014 (4), and is thus at present still an underrecognized cause of SIH. The clinical results of the small number of reported surgically confirmed cases suggest that most patients with CVF (17 of 18 with available follow-up) can respond successfully to treatment, typically surgical obliteration or nerve root ligation (4, 5, 7). This implies that making a diagnosis of CVF has important therapeutic implications. The actual prevalence of CVF in SIH patients with dural CSF leak-negative standard CTMs is likely even higher than the 7% suggested by our study, as our CTMs were not performed specifically for the detection of CVF. Indeed, routine CTM is likely not the optimal imaging modality for this condition. CVF is almost certainly better detected by dynamic techniques like DSM. In 2016, Schievink et al. (7) reported a series of patients with SIH and no dural CSF leak detected at CTM, 19% of whom (10/53) were found to have a CVF on DSM. Their study’s prevalence of 19% confirms our suspicion that the current study’s 7% prevalence of visualizing a hyperdense paraspinal vein on CTM is probably an underestimate. The overall prevalence of CVF in the SIH population is lower; in a recent large series of 568 SIH patients, the prevalence of CVF was 2.5% among all patients and 5% among patients without an extradural CSF collection (3).
The thoracic location (4–7) and female predominance (4, 5, 7) of the hyperdense paraspinal vein is in keeping with others’ results of reported CVF (4, 5, 7). When including our 7 cases strongly suggestive of CVF and the other 19 published cases, all have occurred at thoracic levels, 69% (18 of 26) on the right, and 69% (18 of 26) in females. Cervical and lumbar CVF have not been reported, nor have multisite CVFs.
There are several limitations of our study, including the retrospective nature. Some unblinding of the reviewing radiologists to the CTM indication may have occurred. Specifically, due to the existence of standard imaging protocols for a variety of indications at our institution, the reviewing radiologist could have deduced the initial indication simply by noticing which series were obtained. In addition, although there was concordance among three experienced neuroradiologists regarding the presence of a hyperdense paraspinal vein in the 7 positive cases, there was neither surgical proof, nor proof with a dedicated myelographic study such as DSM. Our group has contacted the referring clinical provider about the presence of a hyperdense paraspinal vein in these 7 cases and we anticipate seeing some of these patients back in follow-up. We hope in the future to report on the follow-up imaging and/or treatment of these patients, but none thus far have been re-imaged with CTM. The unbalanced relatively small size of the control groups, especially the delayed control groups, is also a limitation. However, the primary goal of the study was to assess the prevalence of the hyperdense paraspinal vein sign in SIH patients, with control group analysis performed as a secondary goal in order to assess if the sign occurs in non-SIH patients. The use of only the most recent CTM in the SIH group could potentially decrease the prevalence of the hyperdense paraspinal vein sign, as prior treatments such as blood patches could theoretically cause a previously present sign to be absent on the most recent study. Excluding patients with prior dural CSF leak could result in missing cases of the hyperdense paraspinal vein sign, as some of the reported cases had such prior leaks; however, our goal was to specifically study the population of patients in whom no typical dural CSF leak was ever present.
In conclusion, the hyperdense paraspinal vein has recently been described and is highly compatible with a CVF, which is a newly identified and important cause of SIH. The prevalence of the hyperdense paraspinal vein sign in patients with dural CSF leak-negative standard CTM in our study was 7%, which likely underestimates the true prevalence. This sign should be specifically sought on routine CTM, which is typically the first myelographic modality used to evaluate the spine in SIH patients.
Main points.
A recently discovered cause of spontaneous intracranial hypotension (SIH) in some patients is a cerebrospinal fluid (CSF)-venous fistula, and the hyperdense paraspinal vein sign on CT myelography (CTM) is a recently described sign strongly suggestive of this entity.
In this retrospective review, the prevalence of the sign on standard CTM in patients with SIH who lacked traditional dural CSF leak was 7%. The sign was not found in non-SIH patient control groups, and this difference was statistically significant.
The hyperdense paraspinal vein sign should be sought on standard CTM, which is often the initial myelographic study performed in SIH patients.
The presence of the hyperdense paraspinal vein sign may help avoid nondiagnosis and nontargeted therapies, as well as obviate or direct further myelographic studies, such as digital subtraction myelography.
Acknowledgements
The authors thank Vicki C. Schmidt for her assistance in searching the electronic database for research subjects and Andrea Moran and Sonia Watson for their assistance in editing the manuscript.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Mokri B. Spontaneous low pressure, low CSF volume headaches: spontaneous CSF leaks. Headache. 2013;53:1034–1053. doi: 10.1111/head.12149. https://doi.org/10.1111/head.12149. [DOI] [PubMed] [Google Scholar]
- 2.Kranz PG, Luetmer PH, Diehn FE, Amrhein TJ, Tanpitukpongse TP, Gray L. Myelographic techniques for the detection of spinal CSF leaks in spontaneous intracranial hypotension. AJR Am J Roentgenol. 2016;206:8–19. doi: 10.2214/AJR.15.14884. https://doi.org/10.2214/AJR.15.14884. [DOI] [PubMed] [Google Scholar]
- 3.Schievink WI, Maya MM, Jean-Pierre S, Nuno M, Prasad RS, Moser FG. A classification system of spontaneous spinal CSF leaks. Neurology. 2016;87:673–679. doi: 10.1212/WNL.0000000000002986. https://doi.org/10.1212/WNL.0000000000002986. [DOI] [PubMed] [Google Scholar]
- 4.Schievink WI, Moser FG, Maya MM. CSF-venous fistula in spontaneous intracranial hypotension. Neurology. 2014;83:472–473. doi: 10.1212/WNL.0000000000000639. https://doi.org/10.1212/WNL.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 5.Kranz PG, Amrhein TJ, Schievink WI, Karikari IO, Gray L. The “hyperdense paraspinal vein” sign: a marker of CSF-venous fistula. AJNR Am J Neuroradiol. 2016;37:1379–1381. doi: 10.3174/ajnr.A4682. https://doi.org/10.3174/ajnr.A4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar N, Diehn FE, Carr CM, et al. Spinal CSF venous fistula: A treatable etiology for CSF leaks in craniospinal hypovolemia. Neurology. 2016;86:2310–2312. doi: 10.1212/WNL.0000000000002776. https://doi.org/10.1212/WNL.0000000000002776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schievink WI, Moser FG, Maya MM, Prasad RS. Digital subtraction myelography for the identification of spontaneous spinal CSF-venous fistulas. J Neurosurg Spine. 2016;24:960–964. doi: 10.3171/2015.10.SPINE15855. https://doi.org/10.3171/2015.10.SPINE15855. [DOI] [PubMed] [Google Scholar]