Summary
The relationship between head trauma and parkinsonism has been debated since James Parkinson's first description of the shaking palsy in the late 19th century. We observed in our outpatient clinic a young woman in whom hemiparkinsonism developed within 3 weeks of sustaining closed head trauma with loss of consciousness. The patient had a discrete unilateral midbrain hemorrhage on head MRI which involved the contralateral substantia nigra. The condition responded well to carbidopa/levodopa. This patient is a convincing example of posttraumatic midbrain hemorrhage causing parkinsonism.
In our outpatient neurology clinic, we encountered a young woman with hemiparkinsonism that developed shortly after a car wreck that caused major head and body trauma. Head MRI showed a discrete unilateral midbrain lesion, consistent with posttraumatic parenchymal hemorrhage. This observation provided a convincing cause-and-effect relationship between a midbrain lesion and contralateral hemiparkinsonism.
Patient
A 23-year-old woman was healthy until she was involved in a major car wreck 14 years ago. She had head trauma; multiple fractures including a clavicle, several ribs, and pelvis; splenic rupture; and liver contusions. She lost consciousness for about 1 hour and was obtunded at the time she was admitted to hospital, where she underwent emergency splenectomy. Head CT without contrast reportedly showed swelling of the scalp in the left frontoparietal region, but no intracranial abnormalities. After surgery, she was in the intensive care unit for several days with an altered state of consciousness. She was transferred to our hospital about 2 weeks after the accident for management of an unstable pelvic fracture by orthopedic surgery. Upon discharge about 3 weeks after trauma, she was noted to have a left "foot drop" and difficulties with motor control of the left limbs.
When evaluated in the outpatient neurology clinic about 4 months later, the patient complained of difficulty in performing movements with the left side of her body, including her face, which she had noted within weeks after the accident. She had rest tremor, mostly in the left lower extremity, in addition to rigidity and bradykinesia. The right side had normal mobility. The clinical diagnosis of posttraumatic hemiparkinsonism was considered. She responded well to carbidopa/levodopa (CD/LD), initially in a dose of 25/100 mg, thrice daily. Thereafter, she needed higher doses to maintain mobility. Although left-sided drug-induced dyskinesias developed after several years, she did not mind these movements because of substantial benefits that she derived in alleviating the rigidity and bradykinesia.
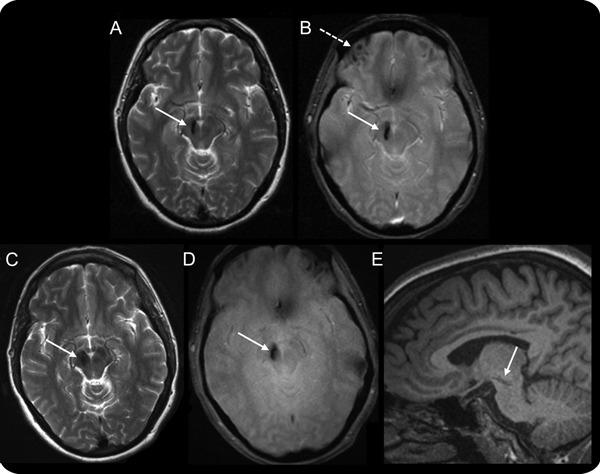
The earliest head MRI, performed about 5 months after trauma, showed a right ventral midbrain hemorrhage in the region of the substantia nigra (figure, A and B). In addition, there were multiple small hemorrhages in the supraorbital frontal lobes, particularly the right. Repeat head MRI about 8 years later showed no appreciable changes (figure, C–E).
Head MRI
Figure. (A) Axial T2-weighted sequence shows focal hypointensity (arrow) in the right ventral midbrain just lateral to the red nucleus and extending rostrally into the substantia nigra. (B) Axial T2* gradient echo sequence shows focal hypointensity in the right midbrain (solid arrow) and right frontal lobe (dashed arrow). There are similar hypointensities involving the left frontal lobe. These susceptibility artifacts are indicative of hemorrhagic lesions. (A, B) About 5 months after head trauma. (C–E) Axial T2-weighted, axial T2* gradient echo, and sagittal T1-weighted sequences that were obtained about 8 years after head trauma. (C, D) No appreciable evolvement of the right midbrain lesion. (E) The rostro-caudal extent of the lesion and its involvement of the substantia nigra.
The patient had relatively stable hemiparkinsonism for the past 14 years. She currently takes CD/LD, CR, 50/200 mg tablets, 4 tablets/day, supplemented with CD/LD, 25/100 mg tablets, 4 to 5 tablets/day. She developed left dystonic features over the years. Unified Parkinson’s Disease Rating Scale (UPDRS) motor examination was performed in the “off” and “on” states. The “off” state was achieved by withdrawal of CD/LD for 36 hours. The “off” UPDRS motor score was 17. The patient had rest tremor of the left lower extremity and rigidity with dystonia and bradykinesia of the left face and body. The patient was then given 1 tablet of CD/LD, CR, 50/200 mg, and 1 tablet of regular CD/LD, 25/100 mg, and re-examined 1 hour later in the “on” state. The UPDRS motor score decreased to 2.5.
DISCUSSION
Theoretically, any lesion that destroys the substantia nigra or its dopaminergic output to the striatum can cause parkinsonism. Thus, ischemic strokes, hemorrhages, abscesses, and tumors are all capable of causing parkinsonism. In clinical practice, these entities are rarely encountered as causes of parkinsonism, probably because the midbrain lesions caused by these entities usually involve much more than the nigrostriatal dopaminergic system. Thus, their clinical manifestations are devastating and parkinsonism is often overlooked.
Because of the proximity of the midbrain to the incisura of the tentorium cerebelli, discrete midbrain hemorrhagic lesions occur in patients with closed head injuries, especially those that cause rostrocaudal brain displacement. Long before the era of modern neuroimaging, the relationship between trauma and parkinsonism was extensively debated, starting with James Parkinson in his original essay on the shaking palsy.1 In these debates, trauma was sometimes used in its widest context, including limb soft tissue injuries and psychological painful experiences.2,3 In 1929, Crouzon and Justin-Besançon4 reviewed the subject of “traumatic parkinsonism.” They considered head trauma to be a rare but definite cause of parkinsonism and suggested strict criteria to justify causal association. Such criteria included 1) “severe head trauma” in a person without prior symptoms, severe enough to cause commotio cerebri, with loss of consciousness; 2) the time interval between trauma and clinical parkinsonism should be “definite,” not too short or too long; and 3) there should be definite progression from symptoms of cerebral commotion to parkinsonism. A similar review arrived at similar conclusions 3 years later.5
For the next 5 decades, postmortem findings of considerable brain destruction, usually of the midbrain and basal ganglia, was considered essential for the definitive diagnosis of posttraumatic parkinsonism.2,3 In the era of computerized brain imaging, most published reports of posttraumatic parkinsonism were associated with hemorrhages in the midbrain and basal ganglia.2,3 Not included in this discussion is another form of posttraumatic parkinsonism that is observed in boxers and other athletes where there is propensity for repeated but less severe episodes of blunt head trauma.
The patient we report satisfied all the criteria listed above. Before the traumatic accident, she was young and healthy. She lost consciousness for about 1 hour and for several days thereafter she was in an altered state of consciousness. The patient recalled having neurologic symptoms that were consistent with left hemiparkinsonism soon after she regained full consciousness several days after head trauma. The orthopedic surgeon noted left “foot drop” in the discharge summary 3 weeks following the car wreck. The diagnosis of hemiparkinsonism was made by neurologists 4 months after head trauma and she responded well to CD/LD treatment. Head MRI revealed a discreet bleed in the right midbrain, which involved the substantia nigra, in addition to relatively minor frontal contusions (figure).
Other points regarding this patient's presentation deserve emphasis. Her hemiparkinsonism remained stable, with no evidence of progression to the right side during 14 years of follow-up. In addition, her condition remained responsive to CD/LD, albeit in increasing doses. The maximal levodopa-induced improvement in the motor functions of the left limbs remained stable, but required increasing doses of CD/LD. Whether this represents “progression” of hemiparkinsonism or “tolerance” to the medication over time remains unclear. The patient developed dystonic features affecting the left side of her body in the “off” state, in addition to LD-induced dyskinesias in the “on” state. Many patients with posttraumatic parkinsonism do not respond to LD. This is usually blamed on more extensive lesions affecting the basal ganglia and brain regions other than the substantia nigra.6
This patient is an excellent illustration of posttraumatic hemiparkinsonism and the natural history of a limited unilateral lesion of the substantia nigra in humans.
STUDY FUNDING
Department of Neurology funds.
DISCLOSURES
The authors report no disclosures relevant to the manuscript. Go to http://neurology.org/cp for full disclosures.
Correspondence to: siharik@gmail.com
Footnotes
Correspondence to: siharik@gmail.com
REFERENCES
- 1.Parkinson J. Essay on the Shaking Palsy. London: Whittingham and Rowland; 1817.
- 2.Factor SA, Sanchez-Ramos J, Weiner WJ. Trauma as an etiology of parkinsonism: a historical review of the concept. Mov Disord. 1988;3:30–36. doi: 10.1002/mds.870030105. [DOI] [PubMed] [Google Scholar]
- 3.Jankovic J. Post-traumatic movement disorders: central and peripheral mechanisms. Neurology. 1994;44:2006–2014. doi: 10.1212/wnl.44.11.2006. [DOI] [PubMed] [Google Scholar]
- 4.Crouzon O, Justin-Besançon L. Le parkinsonisme traumatique. Presse Med. 1929;37:1325–1327. [Google Scholar]
- 5.Kulkov AE. On the problem of traumatic parkinsonism. J Nerv Ment Dis. 1932;75:361–373. [Google Scholar]
- 6.Doder M, Jahanshahi M, Turjanski N, Moseley IF, Lees AJ. Parkinson’s syndrome after closed head injury: a single case report. J Neurol Neurosurg Psychiatry. 1999;66:380–385. doi: 10.1136/jnnp.66.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]


