Summary
Over the past decade, health care in the United States has been a topic of intense political debate, resulting in dramatic legislative, regulatory, and economic changes. These changes have occurred due to the unsustainable rise of health care costs without accompanying improvement in measured health outcomes when compared to other economically developed countries. In an attempt to contain costs and improve the quality of health care provided, the Center for Medicare and Medicaid Services has implemented 4 distinct incentive-based programs. Data are scarce concerning whether such programs will be successful in accomplishing these goals. Each health care provider will need to weigh the costs of participation against the fines incurred by nonparticipation (up to 10% of annual Medicare payments). Knowledge of the percentage of one's practice dedicated to the care of patients in the Medicare and Medicaid programs will be helpful in arriving at a final decision.
In 2012, US national spending on health care reached $2.8 trillion, or about 18% of all spending on all goods and services.1 This is projected to grow faster than the economy, reaching 25% of the gross domestic product by 2037.1 This high level of spending reduces our ability to invest in other important initiatives in our economy and adds to our unsustainable national debt. This creates an economic burden not only for our government, but on families and businesses.2
Currently, our health care system operates under a flawed fee-for-service payment agreement. This encourages quantity of care (volume) and overutilization of high-cost tests and procedures, and does not incentivize prolonged face-to-face time spent evaluating patients. This system of reimbursement has no connection to the quality of care delivered or the outcome for the patient. To date, the Centers for Medicare and Medicaid Services (CMS) has limited information concerning the quality, safety, efficiency, and appropriateness of health care provided.2 A meaningfully reformed health care system will reorient payment incentives toward services and activities that improve the quality of patient care while slowing the pace of growth in national health care spending.3
Quality care has been defined by the Institute of Medicine and Agency for Healthcare Research and Quality as doing the “right thing at the right time, in the right way, for the right person, and having the best possible results.”4 Efficient care is defined as delivering the highest quality care for the least amount of cost.5
CMS has implemented 4 distinct programs in an attempt to codify quality and efficiency and hopefully reduce costs. They have done this by developing incentive programs that are based on rewarding physicians financially when they successfully demonstrate compliance with the requirements for each of these programs. Initially only incentives are offered for practitioners who meet these requirements; however, over time, every one of these programs will transform from a payment-only program to a penalty-only program if the health care provider does not successfully participate.6
These programs include the Medicare Electronic Prescribing (eRx) Incentive Program, the Physician Quality Reporting System (PQRS), the Electronic Health Records (EHR) Incentive Program/Meaningful Use, and the Physician Value-Based Payment Modifier (Value Modifier), which will be discussed.6,7 Details concerning each of these CMS programs are outlined below.
Medicare electronic prescribing incentive program
eRx is the transmission of prescriptions or prescription-related information through electronic media. Electronic prescribing takes place between the prescriber and the dispenser, pharmacy benefit manager, or health plan. It can take place directly or through an intermediary (eRx network). eRx includes, but is not limited to, 2-way transmissions between point of care and the dispenser. Durable medical equipment and over-the-counter medications may be electronically prescribed for the purpose of this program.
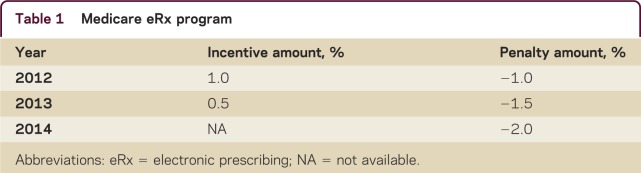
The Medicare eRx Incentive Program is for eligible professionals who are successful electronic prescribers as defined by the Medicare improvements for Patients and Providers Act of 2008. This incentive program began on January 1, 2009, and is a separate program from the PQRS program. Beginning in 2012, eligible professionals who did not meet the requirements for the Medicare eRx Incentive Program were subjected to a payment adjustment (deduction). The adjustment applies to all of the eligible professional's Part B professional services under the Medicare Physician Fee Schedule. The payment adjustment (deduction) will increase with each new reporting period (table 1).
Table 1 Medicare eRx program
For the purposes of the Medicare Electronic Prescribing Incentive Program measure, an eRx event includes all prescriptions electronically prescribed during the patient visit. Note that faxes initiated from the eligible professional's office do not qualify as electronic prescribing for the Medicare eRx Incentive Program.
Participants cannot simultaneously earn incentives in the Medicare EHR Incentive Program and the Medicare eRx Incentive Program. Participants can receive incentives through the Medicaid EHR Incentive Program and the Medicare eRx Incentive Program. However, participation is encouraged in all Medicare Incentive Programs to avoid payment adjustments.
For successfully reporting under the Medicare eRx Incentive Program, neurologists must generate at least one eRx associated with a patient visit on 25 or more unique events during the reporting period. It is to be noted that neurologists who successfully reported during the 2011 period will be exempt from the 2013 payment adjustment, and physicians who successfully reported during the 2012 period will be exempt from the 2014 payment adjustment.
There is no formal way to track your eRx and Medicare does not provide any up-to-date feedback on if an eligible professional is correctly reporting. Hardship exemption categories for the 2013 to 2014 payment adjustments include the following:
The professional or group practice is in a rural area with limited high-speed Internet access
The professional or group practice is in an area with limited available pharmacies for eRx
Inability to eRx due to local, state, or Federal law or regulation
Professionals who prescribe fewer than 100 prescriptions during a 6-month payment adjustment reporting period.
Physician Quality Reporting System
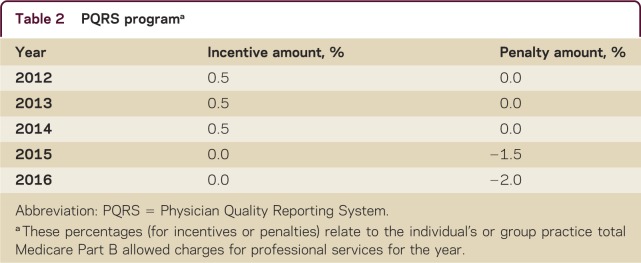
The PQRS provides an incentive payment for eligible professionals who satisfactorily report data on quality measures for services furnished to Medicare beneficiaries. Individual eligible professionals do not need to sign up or preregister in order to begin reporting. To participate in the PQRS, neurologists may choose to report information on individual PQRS quality measures or measure groups 1) to CMS on their Medicare Part B claims, 2) to a qualified PQRS registry, or 3) to CMS via a qualified EHR product. There are individual measures dealing with epilepsy, diabetic neuropathy, smoking cessation, stroke, geriatrics, HIT, depression, medication management, preventive care, and screening, which could be potentially used in a neurologist's practice to fulfill the PQRS requirements. Measure groups include Parkinson disease, dementia, back pain, and sleep apnea. These measures may vary from year to year at the discretion of CMS, so it is important that you are using reporting measures for the correct program year. The simplest way of participating in PQRS may be reporting on 3 measures via CMS claims. To be successful using this method, one must report on at least 50% of the eligible professional's Medicare Part B fee for service patients during the reporting period to which the measure applies.
The incentives and penalties associated with the PQRS program can be found in table 2. In order to avoid the penalties that begin in 2015, one will have to successfully report in the calendar year 2013. Members of the American Academy of Neurology may wish to use an electronic reporting format offered by the American Academy of Neurology (AAN) called the PQRIwizard. This can be accessed through the AAN Web site under the Practice tab, and looking under Incentive Programs, or by contacting AAN staff at ggorvad@aan.com.
Table 2 PQRS programa
A provider can earn additional incentives from the eRx or the EHR/Meaningful Use programs if he or she successfully completes the PQRS program. If you do not participate in the PQRS program, then you cannot receive incentives from both the eRx and the EHR/Meaningful Use programs (if you successfully participate in both, you will by default receive payment for the Meaningful Use program). Specifics concerning successful levels for reporting and the measures for 2013 can be found at the CMS.gov Web site at http://www.cms.gov/PQRSIncentivePrograms/.
Medicare electronic health record incentive program/meaningful use
The American Recovery and Reinvestment Act (Recovery Act) of 2009 provides for incentive payments for Medicare eligible professionals who are meaningful users of certified EHR technology. Incentive payments are allowed if all of the requirements are met for the “meaningful use” of certified EHR technology. Professionals may not receive incentive payments from both the Medicare and Medicaid programs in the same year. The maximum incentive for completing all of the components for the Medicare program over a 5-year period is $44,000 and for completing the Medicaid program over a 6-year period is $63,750. Penalties for nonparticipation will begin in 2015 for the Medicare program, and the last year a provider may initiate the Medicare program is 2014. The last initiation year for the Medicaid program is 2016. There will be no Medicaid payment reductions for nonparticipation by a provider. An outline of how the Medicare Incentive Program Payment Schedule operates can be found in table 3.
Table 3 Medicare electronic health record program
Beginning in 2015, if the provider does not successfully demonstrate meaningful use of certified EHR technology, the covered professional services will be subject to a payment adjustment of 1%. This increases to 2% in 2016, and rises to 3% in 2017 and subsequent years. If it is determined that for 2018 and subsequent years that fewer than 75% of professional providers are meaningful users, then the payment penalty will increase by one percentage point each year until the payment penalty reaches 5%. If you were successful in the Medicare EHR Incentive Program in 2011 or 2012, you must successfully meet the requirements for the full calendar year 2013 to avoid the 2015 penalty. If you are successful in the Medicare EHR Incentive Program in 2013, you must successfully meet the requirements in the 90-day reporting period in 2014 to avoid the 2015 penalty. If you begin the Medicare EHR Incentive Program in 2014, you must successfully meet the requirements for a 90-day reporting period in 2014 within the first 9 months of the 2014 calendar year and attest no later than October 1, 2014, to avoid the 2015 penalty.8
In the Medicaid EHR program, the provider must have a minimum of 30% of his or her practice comprised of Medicaid patients in order to be eligible. The incentive payments (total of $63,750) are distributed over 6 years for successfully participating over the 6 years, and this is a voluntary program for providers and voluntary for states to implement (therefore may not be an option in every state).
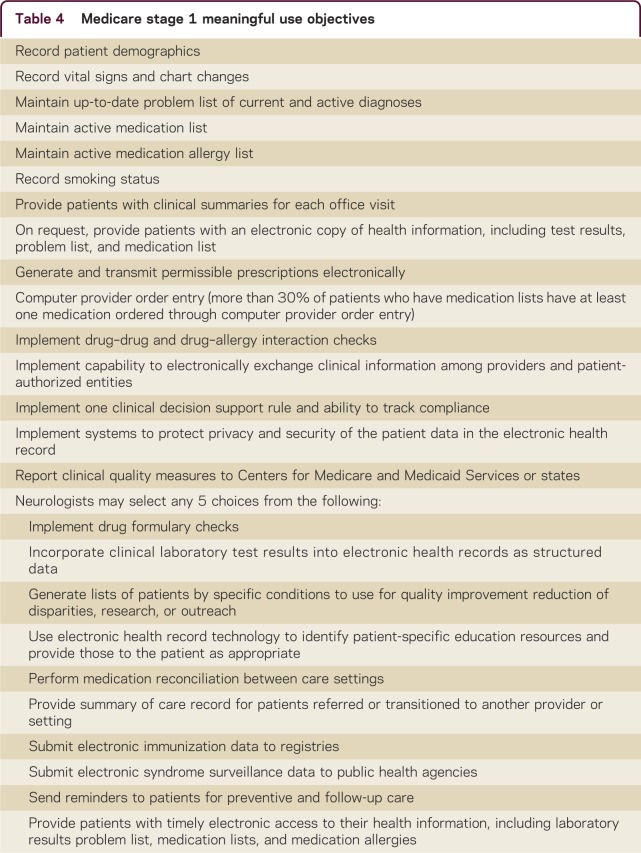
In order to meet the requirements for the stage 1 incentive of the EHR program, neurologists must comply with 15 core objectives and a menu of others, from which physicians can choose 5.9,10 The core objectives and menu of additional objectives are listed in table 4.
Table 4 Medicare stage 1 meaningful use objectives
Physicians must also report on 3 core clinical quality measures (related to blood pressure management, tobacco use, and weight) as well as 3 additional quality measures that they may choose from a list of 38. The purpose of this is to move toward integration of reporting measures under the PQRS with the reporting requirements of the Medicare EHR Incentive Program.
In August 2012, CMS released the stage 2 requirements for its EHR program. Stage 2 of meaningful use will begin in 2014. In the first year of participation (stage 1), eligible professionals must demonstrate meaningful use of their EHR for a 90-day reporting period and for a full calendar year each subsequent year. CMS finalized that for 2014 only, all providers, regardless of their stage of meaningful use, are only required to demonstrate meaningful use for a 90-day reporting period. This was done to align with existing CMS quality measurement programs such as the PQRS and to ensure providers who must upgrade their 2014 Certified EHR Technology have adequate time for implementation.9
In stage 2, physicians are required to meet 17 core measures and an additional 3 measures selected from a menu set of 6 measures; in comparison to stage 1, nearly all core and menu measures are included in stage 2. Due to the delayed onset of stage 2 criteria (2014), the progression from stage 1 to stage 3 has been altered, so that providers who qualified for stage 1 in 2011/2012 will need to continue participation in stage 1 criteria through 2013. For providers who begin stage 1 qualifying in 2013 or later, they are required to demonstrate ability to provide stage 1 capabilities for a 2-year period before proceeding to stage 2 for 2 years, then to stage 3 for 2 years. The specifics concerning stage 2 core and main objectives can accessed at http://www.cms.gov/EHRIcentivePrograms.
The EHR incentive program is an all-or-nothing proposition. You must attest to meeting all of the criteria outlined by CMS in order to qualify for the incentive payments or in the future, receive penalties for failing to meet the thresholds proposed for each step of Meaningful Use. CMS has allocated funds for performance of audits to determine the veracity of your attestation.
Physician value-based payment modifier program (value modifier)
In accordance with Section 3007 of the Affordable Care Act of 2010, all group practices that consist of 100 or more eligible providers (EPs) will be subject to the value modifier effective January 1, 2015. This modifier will apply to all physicians by January 1, 2017.11 For groups of 100 or more that do not self-nominate for the Value Modifier program in 2013, CMS will implement a 1.0% payment reduction for all allowable professional charges for the calendar year 2015. This program will compare physician performance on quality and cost and will divide physicians into quartiles. The top performers are designated as “high-quality, low-cost” providers and poor performers as “low-quality, high-cost” providers. The high-performing providers will receive an increase in payment (1%) and low-performing physicians will receive a decrease in payment (1%). This is a “budget-neutral” program; therefore, colleagues will compete with each other to maintain the same level of reimbursement.
The measures utilized for the program in 2013 include the HHS Million Heart measures, PQRS proficiency in reporting measures via Group Practice Reporting Option (Web interface), registries, or EHR, as well as general medicine measures (14 process, 3outcome measures).12 It is anticipated that CMS will include many of the measures currently housed in the PQRS program for inclusion in the Value-Based modifier program in future years. The current measures may be found in the CY 2013 Medicare Fee Schedule Final Rule at https://www.cms.gov.
Data collection for large group practices concerning cost and quality will begin in 2013. CMS will use data to provide confidential feedback to physicians about the quality of care they are providing. The reports are called Quality and Resource Use Reports. Between 2013 and 2015, the CMS will begin sending the feedback reports to all Medicare physicians in the United States.11 It is important to note that in 2013, neither individuals nor groups <100 EPs will be subject to the value modifier.12
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
J.C. Stevens serves on Scientific Advisory Boards for Biogen Idec, Teva Neurosciences, and Genzyme/Sanofi-Aventis; has served on Speakers' Bureaus for and received speaker honoraria from Biogen Idec and Genzyme; and has received research support from Octagam Pharma, Biogen Idec, Sanofi-Aventis, Teva Neurosciences, and NINDS. Full disclosure form information provided by the author is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0b013e3182a1b8bd.
Correspondence to: jcs@fwnc.com
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the author is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0b013e3182a1b8bd.
Footnotes
Correspondence to: jcs@fwnc.com
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the author is available with the full text of this article at http://cp.neurology.org/lookup/doi/10.1212/CPJ.0b013e3182a1b8bd.
REFERENCES
- 1.Emanuel E, Tanden N, Altman S. A systemic approach to containing health care spending. N Eng J Med. 2012;367:949–954. doi: 10.1056/NEJMsb1205901. [DOI] [PubMed] [Google Scholar]
- 2.Antos J, Paulty M, Wilensky G. Bending the cost Curve through market-based incentives. N Eng J Med. 2012;367:954–958. doi: 10.1056/NEJMsb1207996. [DOI] [PubMed] [Google Scholar]
- 3.Stevens J. Pay for performance and the physician quality reporting initiative in neurologic practice. Neurol Clin. 2010;28:505–516. doi: 10.1016/j.ncl.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality, US Department of Health and Human Services. Your Guide to Choosing Quality Healthcare: A Quick Look at Quality. Available at: www.ahrq.gov/consumer/qnt/qntqlook.htm. Accessed September 12, 2012.
- 5.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed]
- 6.Center for Medicare and Medicaid Services. Pay for Performance Programs. Available at: www.cms.gov/P4Pprograms. Accessed September 12, 2012.
- 7.Schneider ME. Pay for performance deadline bears down on providers. Clin Neurol News. 2012;8:19. [Google Scholar]
- 8.Medicare EHR Incentive Program. Available at: www.aan.com/go/practice/pay/ehr. Accessed September 10, 2012.
- 9.Center for Medicare and Medicaid Services. Medicare electronic health record incentive program for eligible professionals. Available at: www.cms.gov/EHRIncentivePrograms. Accessed September 11, 2012.
- 10.Butcher L. What does “Meaningful Use” Mean? CMS issues final rule for EHR incentives. Neurol Today 2010;pp39–pp40.
- 11.AAN News, Focus on Practice. CMS includes new transitional care management code in proposed 2013 Medicare Physician Fee Schedule. Minneapolis: American Academy of Neurology; 2012:10.
- 12.Center for Medicare and Medicaid Services. CY 2013 final rule for Medicare Physician Fee Schedule (MPFS). Available at: www.cms.gov. Accessed February 8, 2013.