Abstract
Objective
Anxiety is a risk factor for disordered eating, but the mechanisms by which anxiety promotes disordered eating are poorly understood. One possibility is local versus global cognitive processing style, defined as a relative tendency to attend to details at the expense of the “big picture.” Anxiety may narrow attention, in turn, enhancing local and/or compromising global processing. We examined relationships between global/local processing style, anxiety, and disordered eating behaviors in a transdiagnostic outpatient clinical sample. We hypothesized that local (vs. global) processing bias would mediate the relationship between anxiety and disordered eating behaviors.
Method
Ninety-three participants completed the eating disorder examination—questionnaire (EDE-Q), State-Trait Anxiety Inventory (STAI)—trait subscale, and the Navon task (a test of processing style in which large letters are composed of smaller letters both congruent and incongruent with the large letter). The sample was predominantly female (95%) with a mean age of 27.4 years (SD = 12.1 years).
Results
Binge eating, but not fasting, purging, or excessive exercise, was correlated with lower levels of global processing style. There was a significant indirect effect between anxiety and binge eating via reduced global level global/local processing.
Discussion
In individuals with disordered eating, being more generally anxious may encourage a detailed-oriented bias, preventing individuals from maintaining the bigger picture and making them more likely to engage in maladaptive behaviors (e.g., binge eating).
Keywords: anxiety, binge eating, eating disorder, global/local processing
1. Introduction
The prevalence of disordered eating behaviors rises throughout adolescence and young adulthood (Hudson, Hiripi, Pope, & Kessler, 2007), and estimations of engagement in at least one pathological eating behavior are as high as 60% for adolescents and adults (Berg, Frazier, & Sherr, 2009; Krahn, Kurth, Gomberg, & Drewnowski, 2005; Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). Dietary restraint, fasting, binge eating, maladaptive weight control behaviors (i.e., excessive exercise, inappropriate diet pill and laxative use, vomiting), low appetite, and dietary restriction are common problematic behaviors in adolescence and adulthood (Field et al., 2001; Solmi, Hatch, Hotopf, Treasure, & Micali, 2014; Stice, Marti, & Rohde, 2013). Further, these behaviors occur transdiagnostically and increase risk for negative health outcomes (e.g., obesity), mood disorders, substance use disorders, and eating disorders (Field et al., 2012; Kotler, Cohen, Davies, Pine, & Walsh, 2001; Krahn et al., 2005; Micali, Ploubidis, De Stavola, Simonoff, & Treasure, 2014; Stice, Davis, Miller, & Marti, 2008). Shared symptoms across eating disorders coupled with high rates of longitudinal diagnostic crossover (Castellini et al., 2011; Eddy et al., 2008) argue for the likelihood of common underlying factors that contribute to the initiation and maintenance of disordered eating behaviors.
One factor frequently associated with disordered eating is high levels of negative affect and, in particular, difficulty managing anxiety (Bulik, Sullivan, Fear, & Joyce, 1997; Deep, Nagy, Weltzin, Rao, & Kaye, 1995; Fisher et al., 2014; Kaye, Bulik, Thornton, Barbarich, & Masters, 2004; Klump, Bulik, Kaye, Treasure, & Tyson, 2009; Pallister & Waller, 2008; Pollice, Kaye, Greeno, & Weltzin, 1997; Raney et al., 2008). The prevalence of anxiety disorders is higher than in the general population for all eating and feeding disorders (Bulik et al., 1997; Fisher et al., 2014; Kaye et al., 2004; Klump et al., 2009; Pallister & Waller 2008); anxiety disorders often predate the onset of disordered eating (Bulik et al., 1997; Deep et al., 1995; Kaye et al., 2004; Klump et al., 2009; Pallister & Waller, 2008; Raney et al., 2008); and clinically significant anxiety frequently persists following treatment for eating pathology (Klump et al., 2009; Pollice et al., 1997). Furthermore, higher levels of trait anxiety are associated with lower body mass index (BMI), longer duration of symptoms, and increased rates of compensatory behaviors, binge eating, body dissatisfaction, and drive for thinness (Dellava et al., 2010; Raney et al., 2008; Rosenbaum & White, 2015; Thornton, Dellava, Root, Lichtenstein, & Bulik, 2011). However, the mechanisms by which anxiety is specifically involved in the maintenance of different disordered eating behaviors are poorly understood.
The way we process incoming multilevel visual information, referred to as global/local processing style, represents a potential mediating mechanism that may explain the relationship between anxiety and eating disorder symptoms. When presented with a visual input consisting of several smaller components, individuals typically respond faster to the larger figure's properties (e.g., overall contour or shape; global processing) than to more detailed features (local processing; Navon, 1977). This so-called “global precedence effect” is assumed to result from processing information holistically in the context in which it appears before attending to the figure's elements. While the human cognitive system typically favors global processing over local processing, the experience of emotions has been found to alter an individual's information processing style. Emotions are theorized to have evolved to prepare the body for specific actions and consequently are associated with shifts in attention, thoughts, behavioral urges, and physiology (Linehan, 2014). With regard to global versus local processing, positive affect has been shown to broaden the attentional focus (Dreisbach & Goschke, 2004; Fredrickson & Branigan, 2005) and increase perceptual flexibility, overcoming trait preferences to global or local features (Baumann & Kuhl, 2005). In contrast, negative affect was found to reduce attentional flexibility and increase local level processing (Fredrickson & Branigan, 2005; Gasper & Clore, 2002). Similar to general negative mood, anxiety promotes narrowing of attentional resources toward the encoding of threat stimuli (de Fockert & Cooper, 2014; Mogg & Bradley, 1998, 2005) and may limit cognitive resources to processing threatening and other information on a more detailed, local level. This might manifest in individuals with disordered eating behavior in a stronger focus on calories, body weight, and body shape, preventing them from meeting their nutritional needs.
Accumulating evidence indeed suggests a more detailed information processing style in patients with eating disorders (and anorexia nervosa [AN] in particular), which has also been associated with a poorer organizational strategy and difficulties in problem solving because of a lack of taking into account the bigger picture (Lang, Lopez, Stahl, Tchanturia, & Treasure, 2014; Moynihan, Rose, van Velzen, & de Fockert, 2016). However, to our knowledge, no investigation has yet utilized a transdiagnostic sample to examine potential links between information processing and different specific disordered eating behaviors. This is important because these behaviors may be at least partially maintained via a local-level processing bias or limited access to “big picture” thinking that is essential for adaptive problem-solving.
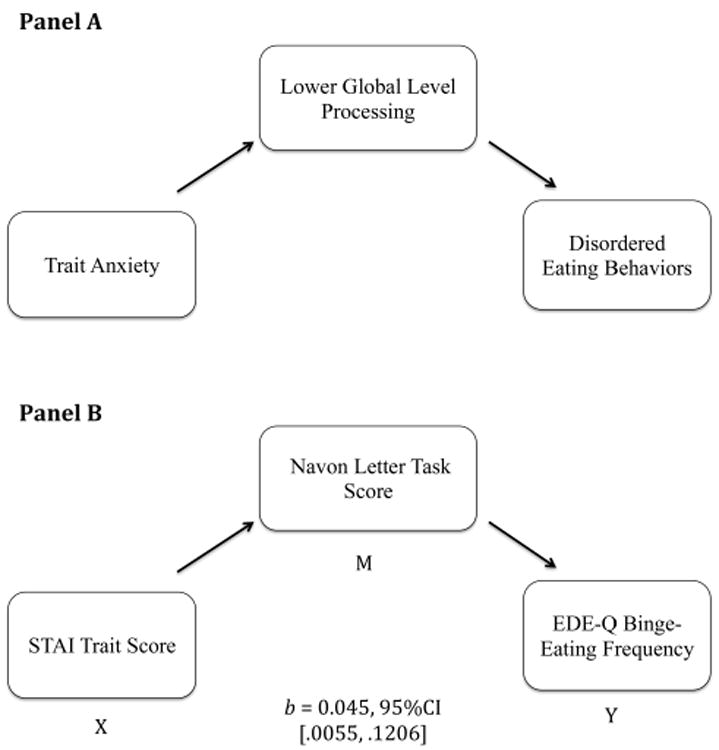
To address this gap in the literature, we examined whether the observed relationship between trait anxiety and disordered eating behaviors is mediated by a tendency for local-level processing of incoming information, thus allowing for enhanced detection of anticipated negative or threatening information and encouraging withdrawal behaviors such as maladaptive eating. In this study, we chose to examine disordered eating behaviors rather than global eating pathology, as we wanted to investigate a possible pathway via which increased anxiety could maintain disordered eating by influencing behaviors. Furthermore, because this is a transdiagnostic sample, some classifications of disordered eating score traditionally lower on features of global measures of eating pathology, such as weight and shape concerns, (e.g., ARFID) but may still report similar behaviors (e.g., restrictive eating). Therefore, because our focus was on mechanisms of transdiagnostic behaviors, independent of reported weight and shape concerns, we chose not to examine our indirect model using beliefs and attitudes. Using standard measures of trait anxiety and disordered eating (fasting, binge eating, purging, and excessive exercise) together with a well-established experimental paradigm for assessing an individual's global/local processing style, we examined the relationship between anxiety, information processing style, and problematic eating behaviors in a transdiagnostic sample of individuals seeking treatment at an outpatient eating disorder clinic. We theorized that higher levels of trait anxiety narrow attention and increase local processing at the cost of attending to the big picture, increasing the likelihood of engaging in disordered eating (i.e., reducing the likelihood of considering and using behavioral alternatives to disordered eating). Accordingly, we hypothesized that there would be a significant indirect relationship between levels of trait anxiety and disordered eating behaviors through global/local processing style, such that lower levels of global-level processing (i.e., higher reliance on local-level processing) would be associated with increased engagement in disordered eating for those with higher trait levels of anxiety (see Figure 1, Panel A).
Figure 1. Global processing as mediator between trait anxiety and disordered eating behaviors.
2. Method
2.1. Participants
Participants were individuals (N = 93) who presented to an outpatient eating disorder clinic requesting an initial evaluation (Table 1). Following a standard clinic phone intake, as part of routine clinical practice, all participants were emailed a link for the completion of several cognitive tasks and questionnaires. All individuals completed the battery in the time period between intake and first evaluation appointment (typically approximately 4 weeks). Participants included in this study sample were clinic patients who completed the diagnostic evaluation by a clinician (n = 75) as well as those who did not attend their scheduled appointment but nonetheless completed the online assessment battery (n = 18). We chose to include individuals who did not attend an intake appointment in the analysis because we were specifically interested in examining relationships between cognitive processing style, self-reported disordered eating behaviors, and anxiety across the spectrum of eating pathology—all assessed in the aforementioned test battery. DSM-5 eating disorder diagnosis was assigned by a clinician at intake evaluation based on clinical interview and review of DSM-5 symptoms. Of the 75 individuals who were evaluated, 72 received a DSM-5 diagnosis, while three individuals displayed subclinical eating pathology. The most common diagnosis was bulimia nervosa (BN; 20.0%) followed by AN—restricting type (AN-R: 17.3%), other specified feeding and eating disorder—atypical anorexia nervosa (OSFED-AA; 13.3%), binge-eating disorder (BED; 10.7%), AN—binge purge type (AN-BP; 10.7%), and avoidant/restrictive food intake disorder (ARFID; 9.3%). Participants provided consent for their responses to be used for research purposes prior to completing the measures. The Partners Human Research Committee reviewed and approved this study.
Table 1. Demographic sample characteristics.
| Mean age (SD) | 27.4 (12.1) |
|
| |
| Adolescents <18 years old, n (%) | 14 (15.1) |
|
| |
| Mean BMI percentile (SD) | 61.2 (35.0) |
|
| |
| Adults ≥ 18 years old, n (%) | 79 (84.9) |
|
| |
| Mean BMI (SD) | 24.6 (9.5) |
| Male, n (%) | 5 (5.4) |
| Female, n (%) | 88 (94.6) |
|
| |
| DSM-5 diagnosisa, n (%) | |
| AN-R | 13 (17.3) |
| AN-BP | 8 (10.7) |
| BN | 15 (20.0) |
| BED | 8 (10.7) |
| ARFID | 7 (9.3) |
| Rumination disorder | 1 (1.3) |
| OSFED—atypical AN | 10 (13.3) |
| OSFED—subthreshold BN | 4 (5.4) |
| OSFED—subthreshold BED | 2 (2.7) |
| OSFED—night eating syndrome | 1 (1.3) |
| OSFED—other | 3 (4.0) |
| Subclinical eating pathology | 3 (4.0) |
|
| |
| Ethnicity, n (%) | |
| Hispanic/Latino | 3 (3.2) |
| Not Hispanic/Latino | 90 (96.8) |
|
| |
| Raceb, n (%) | |
| American Indian/Alaska native | 0 (0) |
| Black/African American | 4 (4.3) |
| Asian | 6 (6.5) |
| Native Hawaiian/other Pacific Islander | 0 (0) |
| White | 87 (93.5) |
|
| |
| Sexual orientationb, n (%) | |
| Heterosexual | 83 (89.2) |
| Homosexual | 5 (5.4) |
| Bisexual | 2 (2.2) |
| Other | 3 (3.2) |
|
| |
| Level of educationb, n (%) | |
| High school graduate (or less) | 23 (24.7) |
| College student (currently) | 26 (28.0) |
| College graduate | 45 (48.4) |
|
| |
| Global/local processingc | |
| Global/local score | 81.5 (113.6) |
|
| |
| Anxietyc | |
| STAI trait | 56.2 (12.7) |
|
| |
| Eating behaviorc | |
| EDE-Q restraint | 2.7 (1.8) |
| EDE-Q eating concern | 2.8 (1.7) |
| EDE-Q shape concern | 3.8 (1.8) |
| EDE-Q weight concern | 3.4 (1.7) |
| EDE-Q global score | 3.2 (1.6) |
| EDE-Q fasting frequency | 1.0 (1.6) |
| EDE-Q binge-eating frequency | 7.0 (9.0) |
| EDE-Q purging frequency | 4.3 (10.7) |
| EDE-Q excessive exercise days | 6.5 (10.1) |
Note. AN = anorexia nervosa; ARFID = avoidant/restrictive food intake disorder; BED = binge-eating disorder; BN = bulimia nervosa; OSFED = other specified feeding and eating disorder. N = 93.
This includes only participants who underwent clinical evaluation, and thus were able to receive a diagnosis, prior to manuscript submission (N = 75).
Individuals were given the option to select more than one category for race, sexual orientation, and level of education.
Data are presented as mean (SD). EDE-Q = eating disorder examination questionnaire. STAI = state-trait anxiety inventory.
2.2. Measures
2.2.1. Demographics questionnaire
Participants self-reported their sex, age, sexual orientation, race, and ethnicity.
The eating disorders examination—questionnaire (EDE-Q) (Fairburn & Beglin, 2008) is a measure of pathological eating behaviors and related attitudes and cognitions. Participants rate the number of days over the past 28 days in which they engaged in behaviors. For this study, we used the binge eating, purging, and excessive exercise frequency counts as well as the fasting item (i.e., frequency of periods of 8 hr or longer without eating for the reason of influencing shape and weight).
The State-Trait Anxiety Inventory (STAI)—trait form (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) is a 20-item measure (range of scores between 20 and 80) that assesses levels of anxiety regardless of context (e.g., how a person generally feels). Participants rate their level of agreement with statements such as “I feel nervous and restless” on a 4-point Likert-like scale ranging from 1 (“almost never”) to 4 (“almost always”). STAI-Trait reliability was α = .94 in this study.
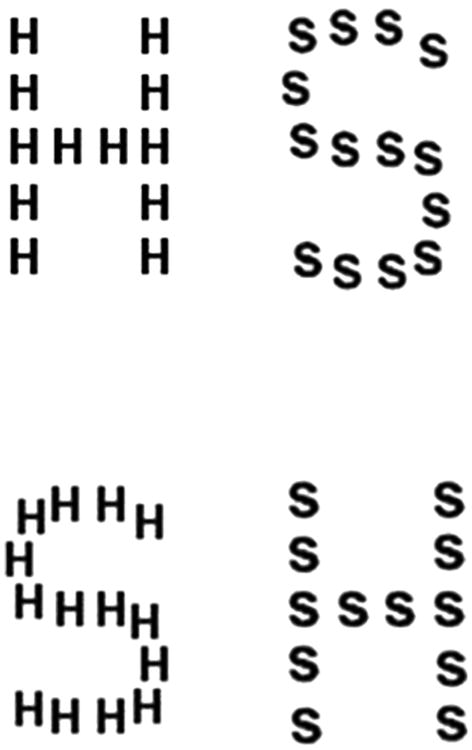
The Navon task (Navon, 1977) is a cognitive task that assesses information processing. Participants completed a web-based version of the test designed for self-administration and validated on a sample of over 7,000 people. Scores on similar reaction time-based tests administered through testmybrain.org have been shown to give comparable results to lab-based tests using the same methods, in participants ages 10–70 years (Germine et al., 2012). In this Navon task, visual stimuli composed of either Hs or Ss forming larger shapes of either Hs or Ss were presented to participants (see Figure 2). Each compound letter was approximately 200 pixels wide by 300 pixels high, with each smaller single letter approximately 50 pixels wide by 50 pixels high. Participants were instructed to categorize either the compound (global) letter (global processing blocks) or single (local) letter (local processing blocks) by pressing “h” or “s” on their keyboards. Each letter was visible until a response was provided, followed by an intertrial interval of 500 ms. All images were preloaded into the browser to prevent any timing delays that would impact stimulus presentation accuracy. Participants first completed five practice trials (with feedback) of judging the local (small) letter, followed by 24 test trials (no feedback). Next, participants completed five practice trials judging the global letter, followed by 24 global test trials. This was followed by a third block of 24 global trials and a final fourth block of 24 local trials (ABBA design). In each test block, local and global judgments were congruent in half of the trials and incongruent in the other half of trials. For each individual, performance difference between global and local processing blocks was calculated based on response times in correct trials as a measure of the global precedence effect, with values below zero indicating a stronger tendency for local processing and values above zero signifying more reliance on global processing. As an additional experimental manipulation, we varied the vertical position of the compound stimulus from trial to trial between 0 and 200 pixels from the center of the screen to prevent participants from focusing on a tiny area of the screen during local blocks and through that lessen the impact of global perceptual information on local discrimination (Duchaine, Yovel, & Nakayama, 2007).
Figure 2. Navon latter task example.
2.3. Statistical data analysis
We used SPSS Version 23 to conduct all analyses (with the exception of the zero inflated Poisson regression analysis, which we conducted in MPlus version 7). We evaluated indirect effects using the INDIRECT Macro for SPSS (Preacher & Hayes, 2008). Prior to analysis, we examined all variables for outliers, resulting in the removal of two participants because of response times that deviated >3 SDs from the sample mean on the Navon task. Bivariate correlations between variables of interest were examined to determine relationships between behaviors and global/local processing style. Following our theoretical assumption of an explanatory link between anxiety and disordered eating behaviors via information processing style, only behaviors that were significantly correlated with information processing style were examined further via indirect analyses.
Indirect effect analysis is a bootstrapping method for examining indirect relationships between two or more variables. Although procedural temporal precedence (i.e., prospective data) is required, to reasonably suggest causality between variables, indirect effect analysis can be appropriate if theoretical temporal precedence can be established. In addition, unlike more traditional methods (i.e., causal steps analysis), indirect effect analysis does not assume that all paths in a proposed model need be statistically significant, as this requirement reduces power to detect meaningful relationships (type II error). Instead, indirect effect analysis calculates the magnitude of the indirect effect and evaluates the statistical significance of the indirect effect using the bias-corrected bootstrapped 95% confidence interval. Bootstrapping allows for better control of type I error compared to traditional p values because the indirect effect is seldom normally distributed (Fritz & Mackinnon, 2007; Hayes, 2013). Indeed, bootstrapping is a resampling procedure in which multiple estimates of the indirect effect are generated by repeatedly resampling with replacement from the sample data. The generated indirect effect distribution can be considered an empirical approximation of the sampling distribution when samples of the specified size (n) are taken from the original population (Hayes, 2009; Preacher & Hayes, 2004, 2008). We selected indirect effect analysis because we expected cognitive processing style would help explain why trait anxiety is linked to engagement in disordered eating, while not hypothesizing that this is the only pathway by which anxiety and disordered eating may be related (e.g., Bollen & Stine, 1990; Preacher & Hayes, 2004, 2008; Shrout & Bolger, 2002). In our model, we included trait levels of anxiety as the independent variable (X), frequency of a disordered eating behavior as the dependent variable (Y), and global/local processing score as the indirect variable (M; see Figure 1, Panel B). The statistical significance of the indirect effect was evaluated using the 95% bias-corrected bootstrapped confidence interval with 5,000 resamples.
3. Results
Data collection took place between May 2014 and November 2015. Sample characteristics for the 93 participants are presented in Table 1. The majority of our sample was Caucasian (94%), female (95%), and over 18 years of age (85%; mean age of entire sample: 27.4 years).
Cognitive processing style, anxiety, and eating disorder pathology scores are presented in Table 1. On average, participants reported higher levels of trait anxiety on the STAI-Trait (M = 56.2; SD = 12.7) compared to norms for working adults (M = 35.2; SD = 10.6) and college students (M = 38.8; SD = 11.9) (Spielberger et al., 1983). Participants also reported moderate levels of general eating pathology (EDE-Q global: M = 3.2; SD = 1.6), compared to norms for adult women (M = 1.5; SD = 1.2) (Mond, Hay, Rodgers, & Owen, 2006) and college students (M = 1.7; SD = 1.3) (Luce, Crowther, & Pole, 2008). Finally, our sample demonstrated a wide range of scores on the Navon task with values ranging from −245 (indicating a strong reliance on local processing) to 478 (signifying a strong reliance on global processing).
We completed bivariate correlations between all study variables (see Table 2). STAI-Trait scores were negatively related to global/local processing score such that, as hypothesized, higher levels of trait anxiety corresponded to reduced global-level and increased local-level processing. In addition, binge eating, captured by the EDE-Q, was negatively correlated with global/local processing score. Neither purging, nor fasting, nor excessive exercise was related to global/local processing scores. Therefore, we only conducted indirect effect analyses between trait anxiety and binge-eating frequency. The indirect effect analysis revealed a statistically significant indirect coefficient (b = 0.045, SE = 0.0278, 95% CI [.0055,.1206]), indicating that higher trait anxiety indirectly influenced engagement in binge eating via an increased tendency for local processing (see Figure 1 Panel B). This model explained close to 7% of the variance in global/local processing (R2 = .067) and close to 8% of the variance in binge-eating frequency (R2 = .075).
Table 2. Correlation matrix of age, global/local score, trait anxiety, and eating psychopathology in a sample of 93 individuals.
| Age | Global-local score | STAI trait | EDE-Q fasting frequency | EDE-Q binge-eating frequency | EDE-Q purge frequency | EDE-Q excessive exercise days | |
|---|---|---|---|---|---|---|---|
| Age | 1.0 | ||||||
| Global-local score | −.13 | 1.0 | |||||
| STAI trait | −.06 | −.26* | 1.0 | ||||
| EDE-Q fasting frequency | −.08 | −.05 | .32** | 1.0 | |||
| EDE-Q binge-eating frequency | .15 | −.28** | .17 | .25* | 1.0 | ||
| EDE-Q purge frequency | .14 | −.08 | .13 | .25* | .21* | 1.0 | |
| EDE-Q excessive exercise days | −.004 | −.02 | .34** | .40** | .02 | .17 | 1.0 |
Note. EDE-Q = eating disorder examination questionnaire; STAI = state-trait anxiety inventory. N = 93.
p <.05,
p < .01.
In order to further understand whether global/local processing is related to the presence or absence of binge-eating behavior, the frequency of engaging in eating behaviors (if present), or both, we conducted a follow-up zero-inflated (ZIP) Poisson regression analysis. With the aim of building further confidence in our indirect effect analysis findings, we included age, gender, and BMI as additional factors that might be related to trait anxiety, cognitive functioning, and/or binge eating (e.g., Jarmolowicz et al., 2014; Muller-Oehring, Schulte, Raassi, Pfefferbaum, & Sullivan, 2007; Smith et al., 2017). The ZIP model involves estimating two regression equations. The first regression is the Poisson portion of the model in which the BMI and global/local processing are predictors of binge-eating frequency. The second regression is the zero-inflated portion in which BMI and global/local processing are predictors of whether or not participants engaged in binge eating. In this analysis, an observed score of zero (i.e. did not engage in binge eating) was coded as 1 and an observed score that is not zero (i.e. engaged in binge eating) was coded as zero. Results from the Poisson portion of the ZIP model show that only global/local scores were negatively associated with engagement in binge-eating behavior (b = −0.002, SE = 0.001, b/SE = −1.993, p = .046). BMI emerged as a trend (b = 0.012, SE = 0.006, b/SE = 1.917, p = .055). No other factors were statistically significant in the Poisson portion of the model (p's ≥ .198). For the zero-inflated portion of the ZIP model, greater BMI was associated with a greater likelihood of having engaged in binge eating versus not having engaged in binge eating (b = −0.129, SE = 0.053, b/SE = −2.414, p = .016). No other factors were statistically significant (p's ≥ .148).
4. Discussion
The purpose of this study was to investigate a theoretical model in which we predicted that increased reliance on local-level cognitive processing over global-level processing would partially explain the relationship between anxiety and disordered eating behaviors. Although prior work has identified deficits in global-level processing in restrictive eating disorders and BN, this study is novel in identifying a specific relationship between reduced global processing and binge-eating behavior. Our findings indicated that a reduced global precedence effect, indicative of a stronger bias toward local processing of visual details, was related to binge eating across eating disorder diagnoses and subclinical levels of eating pathology. Furthermore, indirect effect analyses revealed that global/local information processing style may be important for understanding the relationship between trait anxiety and binge eating. That is, levels of trait anxiety were associated with binge eating in part because of a local processing bias (at the cost of global processing). Importantly, we do not suggest that either global or local processing style represents superior cognitive functioning, as adaptive functioning is related to a balanced use of both. While extreme levels of either global or local processing style could be problematic to effective responding, in this study we demonstrate specifically that the cognitive system's way of processing complex information by retracting from the big picture toward perceptual details may be related to disordered eating and binge eating in particular.
Follow-up analyses indicated that global/local processing was related to binge-eating frequency, but is not indicative of whether or not an individual engages in binge eating. However, because this study is based on a transdiagnostic sample, a substantial portion of the participants (n = 37) did not report binge eating. Larger prospective studies are required to further examine the relationships between the discussed factors.
Although the cross-sectional design of our study does not allow for drawing conclusions about causality, our results provide some evidence that struggling to perceive the bigger picture in those with eating disorders may be related to higher rates of anxiety and depression. Further, identifying that reduced global information processing at the benefit of local processing is associated with binge eating is supported by previous research reporting that those with BN or BED show a similar disorganized performance on cognitive processing tasks (Roberts, Tchanturia, & Treasure, 2013). Although a small effect, our results are notable given the heterogeneity of clinical presentations in our sample. Thus, those with eating pathology who also tend to be more anxious might be the most likely to engage in binge eating, even with only a slight bias toward local information processing. Our findings emphasize the importance of including measures of anxiety in future studies of cognitive processing in eating disorders.
Interestingly, and in contrast to our predictions, no relationships between processing style and other aberrant eating behaviors emerged. However, trait anxiety levels in our sample were consistent with those reported for individuals with anxiety disorders (Bieling, Antony, & Swinson, 1998), and significant relationships emerged between trait anxiety and excessive exercise and fasting in our sample. Thus, anxiety might be related to dietary restriction and excessive exercise via other identified deficits in cognitive functioning, such as cognitive inflexibility, observed in individuals with eating disorders (Roberts, Tchanturia, Stahl, Southgate, & Treasure, 2007). Importantly, purging behaviors were not correlated with trait anxiety and global/local processing style in our sample. However, it may be that some behaviors have stronger relationships with momentary emotions and may therefore be most strongly motivated by other emotions such as guilt (Berg et al., 2013).
We believe that these results uniquely contribute to the field by providing one way of understanding of how anxiety may be related to binge eating, generating testable hypotheses for future studies. Anxiety is a high-arousal negative emotion that promotes avoidance and withdrawal behaviors by narrowing attention to threatening stimuli (Davis & Fischer, 2013). Escape Theory posits that eating pathology (and binge eating in particular) emerges as a coping strategy for avoiding uncomfortable self-awareness and aversive mood states (Heatherton & Baumeister, 1991; Pallister & Waller, 2008). Individuals who generally tend to be more anxious (i.e., display high levels of trait anxiety) may experience a wider range of cues and environments as threatening and therefore engage in more local, detailed processing more frequently (Mogg & Bradley, 1998, 2005). It is important to note that bias toward more global processing in this study was tested for non-threatening, neutral stimuli and found to provide an indirect effect pathway between trait anxiety and binge eating. This indicates that frequent high levels of anxiety may prevent individuals from balanced practice with global processing style on a threat-independent, more global level and thus limit information integration and consequently reduce problem-solving abilities and increase reliance on maladaptive behaviors (e.g., binge eating) on a broader scale (Hawkins & Clement, 1984).
Our study is unique in that we examined the effect of anxiety and information processing style on specific disordered eating behaviors rather than comparing individuals with and without an eating disorder or with different eating disorder diagnoses. This transdiagnostic approach also mirrors cognitive behavioral therapy for eating disorders which adopts a transdiagnostic approach to treatment, theoretically indicating that shared characteristics, such as relationships between mood and cognitive processing, may help explain engagement in those behaviors that span diagnoses (Eddy et al., 2008; Fairburn, Cooper, & Shafran, 2003; Plessow & Eddy, 2017).
4.1. Future directions
To our knowledge, this is the first study to explore global/local processing style, anxiety, and specific disordered eating behaviors in a clinical sample; therefore, there are many ways to expand upon our findings. While indirect effects analysis allows for the examination of potential mediators between variables, it cannot describe causal relationships in cross-sectional data. This study rather serves as a hypothesis-generating tool to guide subsequent research efforts. Future studies could employ path analysis in the context of prospective designs to further test the revealed indirect effect that high trait anxiety is related to binge eating via local processing, establishing causal relationships. Additionally, relationships between anxiety and behavior are complex, and our observed relationship between trait anxiety and disordered eating behaviors may be different for state and momentary anxiety levels. Furthermore, anxiety is only one of many emotions studied in relation to disordered eating. For example, depression is also elevated in those with binge eating (Bulik, 2005), and sadness has been shown to reduce cognitive flexibility and increase local-level processing (Fredrickson & Branigan, 2005; Gasper & Clore, 2002). Relationships between various emotions and state, trait, or momentary levels of emotions may differentially impact cognitive processing and, therefore, may help to explain engagement in compensatory behaviors as well as binge eating. Although these were not the questions we were able to explore in this study, they may be exciting avenues for future research.
All of our participants completed the Navon task using their home computer, thus, it is important to replicate these results across various tasks in a more standardized lab environment. Our assessment of disordered eating behaviors relied on self-report and there is evidence that discrepancy exists between interview and self-report assessments of eating disordered behaviors (Carter, Aime, & Mills, 2001; Fairburn & Beglin, 1994). Specifically, the EDE-Q may either underestimate or overestimate certain behaviors such as objective binge eating and self-induced vomiting in clinical and community samples (Carter et al., 2001; Fairburn & Beglin, 1994; Mond, Hay, Rodgers, Owen, & Beu-mont, 2004). For other behaviors such as laxative use and restriction, the interview and self-report version appear to perform similarly (Carter et al., 2001; Fairburn & Beglin, 1994). This literature suggests that these findings should be corroborated in future studies using interview assessment of disordered eating behaviors. Finally, our sample is composed of mostly Caucasian female participants, and the majority of participants reported clinically significant eating disorder pathology, and therefore future tests of further generalizability are warranted.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under F32MH111127 awarded to K.R.B. and by the Charles A. King Trust Postdoctoral Research Fellowship Program, Bank of America, N.A., Co-Trustees under a Charles A. King Trust Fellowship awarded to F.P. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Charles A. King Trust Postdoctoral Research Fellowship Program.
Funding information: National Institutes of Health, Grant Number: F32MH111127 (K.R.B.); Charles A. King Trust Postdoctoral Research Fellowship Program (F.P.)
Footnotes
Conflict of Interest: Dr. Thomas has received honoraria originating from John Wiley & Sons, Inc. for service as associate editors for the International Journal of Eating Disorders. She has received also travel reimbursement from the Academy for Eating Disorders.
Orcid: Kendra R. Becker, http://orcid.org/0000-0002-8946-9977
Franziska Plessow, http://orcid.org/0000-0002-9721-7817
Kathryn A. Coniglio, http://orcid.org/0000-0002-8549-2790
Jennifer Thomas, http://orcid.org/0000-0003-2601-581X
Supporting Information: Additional Supporting Information may be found online in the supporting information tab for this article.
References
- Baumann N, Kuhl J. Positive affect and flexibility: Overcoming the precedence of global over local processing of visual information. Motivation and Emotion. 2005;29(2):123–134. [Google Scholar]
- Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, Wonderlich SA. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology. 2013;122(1):111–118. doi: 10.1037/a0029703. https://doi.org/10.1037/a0029703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Frazier P, Sherr L. Change in eating disorder attitudes and behavior in college women: Prevalence and predictors. Eating Behaviors. 2009;10(3):137–142. doi: 10.1016/j.eatbeh.2009.03.003. https://doi.org/10.1016/j.eatbeh.2009.03.003. [DOI] [PubMed] [Google Scholar]
- Bieling PJ, Antony MM, Swinson RP. The State-Trait Anxiety Inventory, trait version: Structure and content re-examined. Behaviour Research and Therapy. 1998;36(7-8):777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Stine R. Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology. 1990;20(1):15–140. [Google Scholar]
- Bulik CM. Anxiety, depression and eating disorders. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: A comprehensive handbook. 2nd. New York, NY: Guilford Press; 2005. [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatrica Scandinavica. 1997;96(2):101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Carter JC, Aime AA, Mills JS. Assessment of bulimia nervosa: A comparison of interview and self-report questionnaire methods. International Journal of Eating Disorders. 2001;30(2):187–192. doi: 10.1002/eat.1071. [DOI] [PubMed] [Google Scholar]
- Castellini G, Lo Sauro C, Mannucci E, Ravaldi C, Rotella CM, Faravelli C, Ricca V. Diagnostic crossover and outcome predictors in eating disorders according to DSM-IV and DSM-V proposed criteria: A 6-year follow-up study. Psychosomatic Medicine. 2011;73(3):270–279. doi: 10.1097/PSY.0b013e31820a1838. https://doi.org/10.1097/PSY.0b013e31820a1838. [DOI] [PubMed] [Google Scholar]
- Davis K, Fischer S. The influence of trait anger, trait anxiety and negative urgency on disordered eating. Personality and Individual Differences. 2013;54(2):307–310. https://doi.org/10.1016/j.paid.2012.08.036. [Google Scholar]
- de Fockert JW, Cooper A. Higher levels of depression are associated with reduced global bias in visual processing. Cognition and Emotion. 2014;28(3):541–549. doi: 10.1080/02699931.2013.839939. https://doi.org/10.1080/02699931.2013.839939. [DOI] [PubMed] [Google Scholar]
- Deep AL, Nagy LM, Weltzin TE, Rao R, Kaye WH. Premorbid onset of psychopathology in long-term recovered anorexia nervosa. The International Journal of Eating Disorders. 1995;17(3):291–297. [PubMed] [Google Scholar]
- Dellava JE, Thornton LM, Hamer RM, Strober M, Plotnicov K, Klump KL, et al. Bulik CM. Childhood anxiety associated with low BMI in women with anorexia nervosa. Behaviour Research and Therapy. 2010;48(1):60–67. doi: 10.1016/j.brat.2009.09.009. https://doi.org/10.1016/j.brat.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreisbach G, Goschke T. How positive affect modulates cognitive control: Reduced perseveration at the cost of increased distractibility. The Journal of Experimental Psychology: Learning, Memory, and Cognition. 2004;30(2):343–353. doi: 10.1037/0278-7393.30.2.343. https://doi.org/10.1037/0278-7393.30.2.343. [DOI] [PubMed] [Google Scholar]
- Duchaine B, Yovel G, Nakayama K. No global processing deficit in the Navon task in 14 developmental prosopagnosics. Social Cognitive and Affective Neuroscience. 2007;2(2):104–113. doi: 10.1093/scan/nsm003. https://doi.org/10.1093/scan/nsm003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Diagnostic crossover in anorexia nervosa and bulimia nervosa: Implications for DSM-V. American Journal of Psychiatry. 2008;165(2):245–250. doi: 10.1176/appi.ajp.2007.07060951. https://doi.org/10.1176/appi.ajp.2007.07060951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? The International Journal of Eating Disorders. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Eating disorder examination questionnaire (6.0) New York, NY: Guilford Press; 2008. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Field AE, Camargo CA, Jr, Taylor CB, Berkey CS, Roberts SB, Colditz GA. Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics. 2001;107(1):54–60. doi: 10.1542/peds.107.1.54. [DOI] [PubMed] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, et al. Horton NJ. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130(2):e289–e295. doi: 10.1542/peds.2011-3663. https://doi.org/10.1542/peds.2011-3663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher MM, Rosen DS, Ornstein RM, Mammel KA, Katzman DK, Rome ES, et al. Walsh BT. Characteristics of avoidant/restrictive food intake disorder in children and adolescents: A “new disorder” in DSM-5. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2014;55(1):49–52. doi: 10.1016/j.jadohealth.2013.11.013. https://doi.org/10.1016/j.jadohealth.2013.11.013. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Branigan C. Positive emotions broaden the scope of attention and thought-action repertoires. Cognition and Emotion. 2005;19(3):313–332. doi: 10.1080/02699930441000238. https://doi.org/10.1080/02699930441000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. https://doi.org/10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasper K, Clore GL. Attending to the big picture: Mood and global versus local processing of visual information. Psychological Science. 2002;13(1):34–40. doi: 10.1111/1467-9280.00406. [DOI] [PubMed] [Google Scholar]
- Germine L, Nakayama K, Duchaine BC, Chabris CF, Chatterjee G, Wilmer JB. Is the Web as good as the lab? Comparable performance from Web and lab in cognitive/perceptual experiments. Psychonomic Bulletin and Review. 2012;19(5):847–857. doi: 10.3758/s13423-012-0296-9. https://doi.org/10.3758/s13423-012-0296-9. [DOI] [PubMed] [Google Scholar]
- Hawkins RC, Clement PF. Binge eating: Measurement problems and a conceptual model. In: Hawkins RC, Fremouw WJ, Clement PF, editors. The binge purge syndrome: Diagnosis, treatment and research. New York, NY: Springer; 1984. pp. 229–251. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York, NY: Guilford Press; 2013. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. https://doi.org/10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarmolowicz DP, Cherry JB, Reed DD, Bruce JM, Crespi JM, Lusk JL, Bruce AS. Robust relation between temporal discounting rates and body mass. Appetite. 2014;78:63–67. doi: 10.1016/j.appet.2014.02.013. https://doi.org/10.1016/j.appet.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. The American Journal of Psychiatry. 2004;161(12):2215–2221. doi: 10.1176/appi.ajp.161.12.2215. https://doi.org/10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for eating disorders position paper: Eating disorders are serious mental illnesses. International Journal of Eating Disorders. 2009;42(2):97–103. doi: 10.1002/eat.20589. https://doi.org/10.1002/eat.20589. [DOI] [PubMed] [Google Scholar]
- Kotler LA, Cohen P, Davies M, Pine DS, Walsh BT. Longitudinal relationships between childhood, adolescent, and adult eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(12):1434–1440. doi: 10.1097/00004583-200112000-00014. https://doi.org/10.1097/00004583-200112000-00014. [DOI] [PubMed] [Google Scholar]
- Krahn DD, Kurth CL, Gomberg E, Drewnowski A. Pathological dieting and alcohol use in college women—A continuum of behaviors. Eating Behaviors. 2005;6(1):43–52. doi: 10.1016/j.eatbeh.2004.08.004. https://doi.org/10.1016/j.eatbeh.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Lang K, Lopez C, Stahl D, Tchanturia K, Treasure J. Central coherence in eating disorders: An updated systematic review and meta-analysis. World Journal of Biological Psychiatry. 2014;15(8):586–598. doi: 10.3109/15622975.2014.909606. https://doi.org/10.3109/15622975.2014.909606. [DOI] [PubMed] [Google Scholar]
- Linehan MM. DBT® skills training manual. New York: Guilford Publications; 2014. [Google Scholar]
- Luce KH, Crowther JH, Pole M. Eating disorder examination questionnaire (EDE-Q): Norms for undergraduate women. The International Journal of Eating Disorders. 2008;41(3):273–276. doi: 10.1002/eat.20504. https://doi.org/10.1002/eat.20504. [DOI] [PubMed] [Google Scholar]
- Micali N, Ploubidis G, De Stavola B, Simonoff E, Treasure J. Frequency and patterns of eating disorder symptoms in early adolescence. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2014;54(5):574–581. doi: 10.1016/j.jadohealth.2013.10.200. https://doi.org/10.1016/j.jadohealth.2013.10.200. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP. A cognitive-motivational analysis of anxiety. Behaviour Research and Therapy. 1998;36(9):809–848. doi: 10.1016/s0005-7967(98)00063-1. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP. Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive Therapy and Research. 2005;29(1):29–45. [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C. Eating disorder examination questionnaire (EDE-Q): Norms for young adult women. Behaviour Research and Therapy. 2006;44(1):53–62. doi: 10.1016/j.brat.2004.12.003. https://doi.org/10.1016/j.brat.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Validity of the Eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy. 2004;42(5):551–567. doi: 10.1016/S0005-7967(03)00161-X. https://doi.org/10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- Moynihan J, Rose M, van Velzen J, de Fockert J. Local and global visual processing and eating disorder traits: An event-related potential study. Biological Psychology. 2016;115:27–34. doi: 10.1016/j.biopsycho.2016.01.002. https://doi.org/10.1016/j.biopsycho.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Muller-Oehring EM, Schulte T, Raassi C, Pfefferbaum A, Sullivan EV. Local-global interference is modulated by age, sex and anterior corpus callosum size. Brain Research. 2007;1142:189–205. doi: 10.1016/j.brainres.2007.01.062. https://doi.org/10.1016/j.brainres.2007.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navon D. Forest before trees: The precedence of global features in visual perception. Cognition Psychology. 1977;9(3):353–383. https://doi.org/10.1016/0010-0285(77)90012-3. [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of American Dietetic Association. 2011;111(7):1004–1011. doi: 10.1016/j.jada.2011.04.012. https://doi.org/10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: Understanding the overlap. Clinical Psychology Review. 2008;28(3):366–386. doi: 10.1016/j.cpr.2007.07.001. https://doi.org/10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Plessow F, Eddy KT. Diagnostic crossover. In: Wade T, editor. Encyclopedia of feeding and eating disorders. New York, NY: Springer; 2017. pp. 1–5. [Google Scholar]
- Pollice C, Kaye WH, Greeno CG, Weltzin TE. Relationship of depression, anxiety, and obsessionality to state of illness in anorexia nervosa. The International Journal of Eating Disorders. 1997;21(4):367–376. doi: 10.1002/(sici)1098-108x(1997)21:4<367::aid-eat10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behaviour Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Raney TJ, Thornton LM, Berrettini W, Brandt H, Crawford S, Fichter MM, et al. Bulik CM. Influence of overanxious disorder of childhood on the expression of anorexia nervosa. The International Journal of Eating Disorders. 2008;41(4):326–332. doi: 10.1002/eat.20508. https://doi.org/10.1002/eat.20508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychological Medicine. 2007;37(8):1075–1084. doi: 10.1017/S0033291707009877. https://doi.org/10.1017/S0033291707009877. [DOI] [PubMed] [Google Scholar]
- Roberts ME, Tchanturia K, Treasure JL. Is attention to detail a similarly strong candidate endophenotype for anorexia nervosa and bulimia nervosa? World Journal of Biological Psychiatry. 2013;14(6):452–463. doi: 10.3109/15622975.2011.639804. https://doi.org/10.3109/15622975.2011.639804. [DOI] [PubMed] [Google Scholar]
- Rosenbaum DL, White KS. The relation of anxiety, depression, and stress to binge eating behavior. Journal of Health Psychology. 2015;20(6):887–898. doi: 10.1177/1359105315580212. https://doi.org/10.1177/1359105315580212. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7(4):422–445. [PubMed] [Google Scholar]
- Smith KE, Mason TB, Murray SB, Griffiths S, Leonard RC, Wetterneck CT, et al. Lavender JM. Male clinical norms and sex differences on the Eating Disorder Inventory (EDI) and Eating disorder examination questionnaire (EDE-Q) International Journal of Eating Disorders. 2017;50:769–775. doi: 10.1002/eat.22716. https://doi.org/10.1002/eat.22716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi F, Hatch SL, Hotopf M, Treasure J, Micali N. Prevalence and correlates of disordered eating in a general population sample: The South East London Community Health (SELCoH) study. Social Psychiatry and Psychiatric Epidemiology. 2014;49(8):1335–1346. doi: 10.1007/s00127-014-0822-3. https://doi.org/10.1007/s00127-014-0822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the Stait-Trait Anxiety Scale. Palo Alto, CA: Consulting Psychologists; 1983. [Google Scholar]
- Stice E, Davis K, Miller NP, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: A 5-year prospective study. Journal of Abnormal Psychology. 2008;117(4):941–946. doi: 10.1037/a0013644. https://doi.org/10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology. 2013;122(2):445–457. doi: 10.1037/a0030679. https://doi.org/10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton LM, Dellava JE, Root TL, Lichtenstein P, Bulik CM. Anorexia nervosa and generalized anxiety disorder: Further explorations of the relation between anxiety and body mass index. Journal of Anxiety Disorders. 2011;25(5):727–730. doi: 10.1016/j.janxdis.2011.03.010. https://doi.org/10.1016/j.janxdis.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


