Summary
Acute visual loss in one eye is a common symptom brought to the attention of the practicing neurologist. In this circumstance, it is critical to identify whether visual loss is due to an optic neuropathy or an ocular disorder (especially retinal disease). This review addresses the elements of the history and examination that are useful in evaluating a patient with visual loss, with the goals of correctly localizing the lesion and constructing a likely differential diagnosis.
 |
The evaluation of a patient with acute monocular visual loss begins with a careful history. Details from the patient's description of visual symptoms may offer a preliminary suggestion of whether visual loss results from ocular or optic nerve pathology. Monocular metamorphopsia (wavy, warped images) and positive phenomena such as flashing or colored lights often indicate a retinal lesion. Conversely, visual blurring with a description that colors look “washed out” or “faded” may suggest optic nerve dysfunction. Occasionally, patients who perceive scintillating lights with a hemifield defect will misinterpret the hallucinations as originating in one eye. It is helpful to try to clarify whether the patient covered one eye while symptomatic to determine if the visual phenomena occurred in both eyes or in one eye alone.
The tempo of visual loss gives important clues regarding the potential etiology: for example, in patients with optic neuritis it may quickly evolve and then subsequently improve; in ischemic optic neuropathy it may be sudden and fairly static; in patients with compressive lesions, its discovery may be sudden, but in fact its occurrence is more likely to be insidious and slowly progressive. In addition, it is important to elicit the presence or absence of associated orbital, neurologic, or systemic symptoms. The quality and severity of pain should be characterized; pain is typically present in disorders such as optic neuritis or giant cell arteritis, but is absent in most retinal diseases or nonarteritic ischemic optic neuropathy. Knowledge of a patient's age and medical history, in particular a history of vascular risk factors, cancer, or autoimmune disorders, is essential in establishing a reasonable differential diagnosis.
A detailed examination is critical to the accurate identification of an optic neuropathy or ocular disorder producing acute visual loss (figure 1). Reduced central visual acuity may occur with both optic nerve and ocular conditions, both of which must be considered when acuity cannot be corrected by pinhole or refraction. Color vision (which can be assessed with pseudoisochromatic color plates or by testing for perceived color desaturation) is often disproportionately affected by an optic neuropathy. The Amsler grid, which is a series of horizontal and vertical lines similar to graph paper, may have an abnormal appearance to a patient with macular disease.
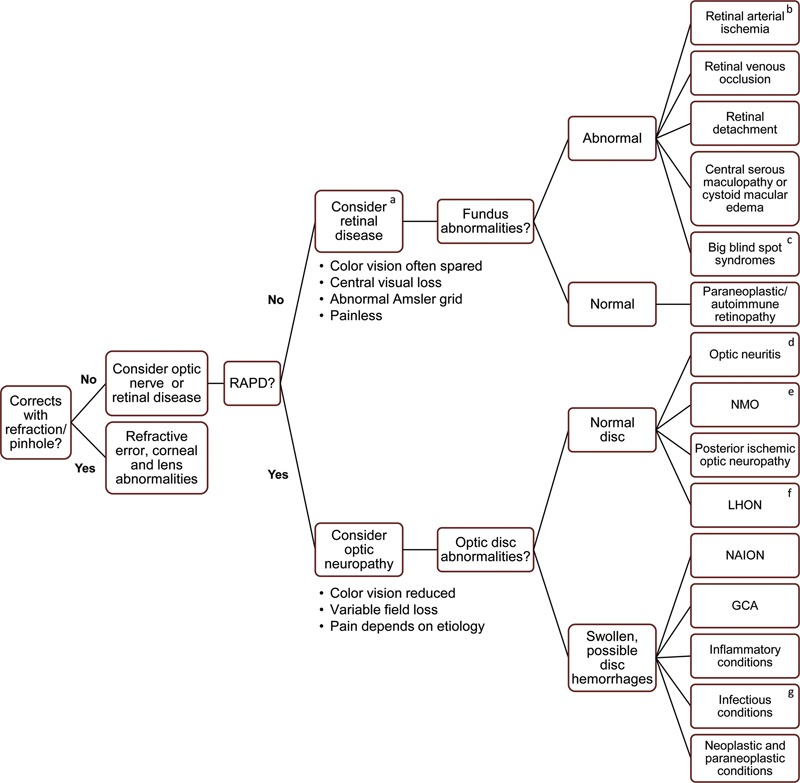
Algorithm for the evaluation of acute monocular visual loss
Figure 1. BRAO = branch retinal artery occlusion; CRAO = central retinal artery occlusion; GCA = giant cell arteritis; LHON = Leber hereditary optic neuropathy; NAION = nonarteritic ischemic optic neuropathy; NMO = neuromyelitis optica; RAPD = relative afferent pupillary defect. (a) With marked retinal diseases, an afferent pupillary defect can be present. (b) CRAO, BRAO, macular ischemia. (c) Retinal abnormalities may not be present. (d) Mild optic disc swelling may be present, typically without peripapillary hemorrhages. (e) Vision loss can be bilateral, recurrent, and often severe. (f) Optic disc pseudoswelling and peripapillary telangiectasias may be present. (g) Some may have macular star.
Visual fields can be assessed through confrontation techniques, but detailed perimetry testing is more sensitive and can reveal patterns of field loss that suggest a specific localization and differential diagnosis. Depression of the central visual field is expected in a maculopathy, but also frequently occurs with optic neuropathy. Conversely, a “nerve fiber bundle field defect” (that originates from the physiologic blind spot and respects the horizontal meridian) is more specific for optic neuropathy. Finally, the assessment of visual fields may identify homonymous field loss owing to a retrochiasmal lesion, despite the patient's misperception that the change in vision is monocular.
Knowledge of a patient's age and medical history, in particular a history of vascular risk factors, cancer, or autoimmune disorders, is essential in establishing a reasonable differential diagnosis.
The hallmark of a unilateral optic neuropathy is the relative afferent pupillary defect (RAPD). The RAPD is determined by the swinging flashlight test, during which light is alternately directed toward each pupil. When light is directed toward the unaffected eye, both pupils should constrict normally. When light is shined into the affected eye, the dilation of both pupils indicates the presence of a RAPD. In a more subtle RAPD, when the affected eye is stimulated the pupils may initially constrict but demonstrate a quicker redilation. While a small RAPD may be observed in the setting of moderate or severe retinal dysfunction, it is often readily apparent with even mild unilateral or asymmetric optic neuropathy.
The appearance of the retina and optic disc provides critical information regarding the likely cause of acute monocular visual loss. A detailed retinal examination following pharmacologic pupillary dilation may reveal evidence of vitreous hemorrhage, retinal arterial or venous infarction, retinal detachment, or other macular pathology. The optic nerve head should be assessed for signs of swelling, pallor, or normal appearance.1 As described below, optic disc swelling in a patient with acute monocular visual loss may indicate ischemia or inflammation of the optic nerve head. A normal optic disc is expected with retrobulbar processes, such as typical optic neuritis. Optic disc pallor would indicate chronic compression or prior optic nerve injury, but these are unlikely to present with acute visual loss unless the patient had unrecognized subclinical injury. When the retina and optic disc appear normal in the setting of acute visual loss, the identification of a retrobulbar optic neuropathy relies heavily on determining the presence of a RAPD.
Some cases of acute monocular visual loss will not have an identifiable organic basis.2 In these cases, abnormal acuity and visual fields will be accompanied by normal-appearing retina and optic disc; importantly, a RAPD will not be present. The reliability indices of automated visual fields may be low and a “cloverleaf” pattern of field constriction is common. On confrontation or tangent screen examination the patient may show nonphysiologic “tubular” constricted fields that do not appropriately expand as the testing distance is increased.
Conducting an appropriate workup
For many causes of acute monocular visual loss, the diagnosis is based solely on the clinical history and physical examination. Characteristic features of these entities are detailed in the following sections. In other cases, once the history and examination suggest a likely localization, an appropriate diagnostic workup can confirm the correct diagnosis. Orbital MRI sequences (including coronal T2-weighted images and fat-saturated postgadolinium images) typically provide excellent views of the prechiasmatic optic nerve. Though not completely specific, MRI can be helpful in separating inflammatory, ischemic, and neoplastic optic neuropathies.3 While increased T2 signal is common to many etiologies of optic neuropathy, pathologic enhancement of the optic nerve reliably distinguishes optic nerve inflammation or demyelination from nonarteritic anterior ischemic optic neuropathy. While imaging characteristics of the optic nerve may not directly distinguish inflammatory and demyelinating causes, there may be evidence of additional involvement of the meninges, pituitary gland, or lacrimal glands pointing to an inflammatory condition.
In some circumstances, additional imaging and electrophysiologic studies prove helpful. Optical coherence tomography (OCT) provides high-resolution cross-sectional images of the retina that aid in distinguishing retinal pathology from optic neuropathy.4 Fluorescein angiography is used in some cases where there is suspicion for an occult maculopathy, such as an ischemic lesion associated with diabetes. Although visual evoked potentials (VEP) are not routinely used in the diagnosis of demyelinating optic neuritis, the finding of a P100 response with prolonged latency provides good evidence for optic nerve demyelination. An electroretinogram can aid in the diagnosis of acute outer retinal dysfunction, particularly when no overt lesions are evident and retinal dysfunction is suspected by history.
Finally, serologic and CSF tests can help diagnose an infectious, inflammatory, or neoplastic illness. Genetic testing can confirm a diagnosis of Leber hereditary optic neuropathy (LHON). These tests are best utilized when the index of suspicion is increased by a suggestive history and examination.
Retinal causes of acute monocular visual loss
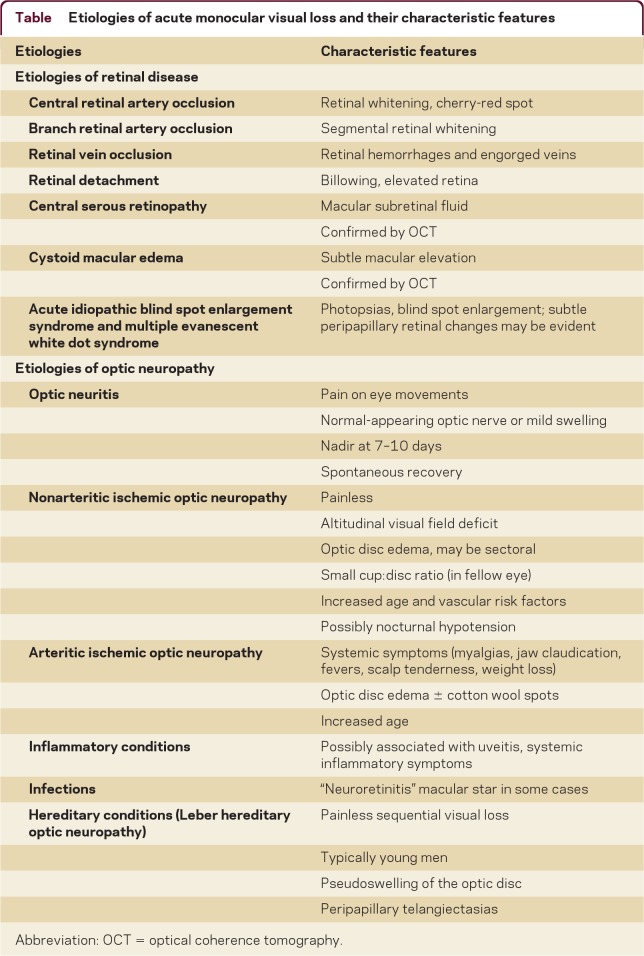
The retinal conditions that cause acute monocular visual loss can typically be distinguished by the history and examination (table). In some cases, abnormalities on fundus examination may be subtle and require the expertise of an ophthalmologist or neuro-ophthalmologist. In this setting, an OCT scan can also be particularly helpful in establishing the diagnosis.
Table Etiologies of acute monocular visual loss and their characteristic features
Retinal artery occlusion is characterized by retinal whitening with a macular cherry-red spot (where intact choroidal circulation is seen most readily) (figure 2A). In the case of a branch retinal artery occlusion, a demarcation between affected and spared areas of retina is apparent (figure 2B). Diabetic macular ischemia often produces macular edema that is apparent on dilated fundus examination, typically in association with retinal microhemorrhages, cotton-wool spots, and attenuated vessels. A retinal vein occlusion produces multiple small retinal hemorrhages and engorgement of retinal veins (figure 2C). Retinal detachment, which produces profound visual loss when the macula is involved, is diagnosed by the observation of abnormal retinal elevation (figure 2D). Central serous retinopathy presents with acute, painless visual loss due to macular subretinal fluid (figure 2E). Cystoid macular edema also causes reduced acuity, with mild thickening or elevation of the macula that may be difficult to appreciate on dilated fundus examination, but readily apparent on OCT. Paraneoplastic retinopathies include cancer-associated retinopathy (most commonly with antibodies to recoverin protein) and melanoma-associated retinopathy (with antibodies to rod bipolar cells); autoimmune retinopathies without underlying cancer also occur.5 Diseases of the outer retina include acute idiopathic blind spot enlargement syndrome and multiple evanescent white-dot syndrome, in which patients may describe sparkling photopsias and missing vision in the region surrounding the physiologic blind spot. The examination may reveal subtle peripapillary pigmentary changes, typically without disc swelling.
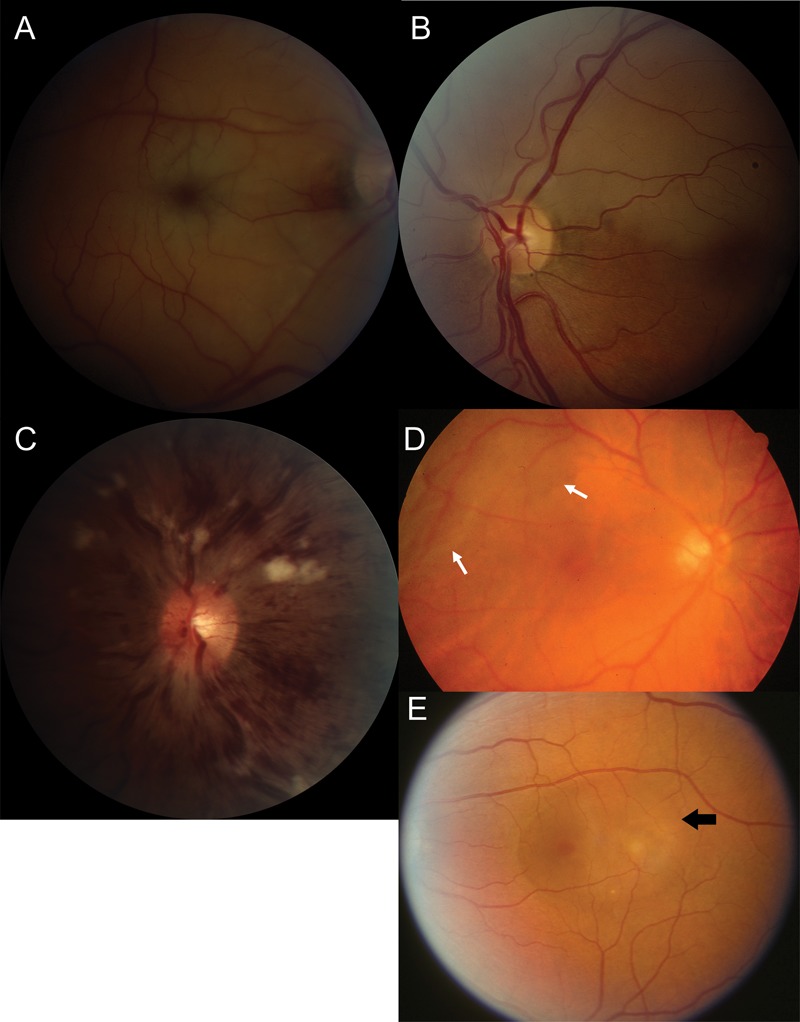
Retinal disorders
Figure 2. (A) Central retinal artery occlusion. Severe retinal pallor and macular cherry-red spot. (B) Branch retinal artery occlusion. Superior retinal pallor with normal retina inferiorly. (C) Central retinal vein occlusion. Mild disc swelling and hyperemia, extensive retinal hemorrhages, dilated retinal veins, and cotton-wool spots. (D) Retinal detachment. Corrugated or folded temporal retina (arrows) (photo courtesy of Nicholas Volpe, MD). (E) Central serous retinopathy. Elevation of the inner retina with underlying fluid in the region of the macula. A and E reprinted with permission from Prasad et al.20
Optic neuropathy: differential diagnosis and clinical clues
When the history and examination suggest an optic neuropathy, several important clinical features help to narrow a broad differential diagnosis. Possibilities include idiopathic demyelinating optic neuritis, ischemic optic neuropathy, inflammatory and infectious conditions, infiltrative or neoplastic processes, and hereditary optic neuropathies (table). Compressive lesions will typically cause slowly progressive, rather than acute visual loss, although on some occasions this symptom comes to attention fairly suddenly. In addition, acute decline in vision may occasionally be superimposed on chronic progression owing to rapid expansion of a mass lesion, as may occur with pituitary apoplexy or an aneurysm.
Optic neuritis
Idiopathic demyelinating optic neuritis most often occurs between the ages of 20 to 50 and is 3 times more frequent in women.6 Visual loss usually occurs rapidly, reaches its nadir within 7–10 days, and begins to recover within 1 month. Retro-orbital pain, particularly with eye movements, occurs in almost all cases; it may precede the visual loss and typically persists for 1–2 weeks. Perimetry testing will most often reveal either a central scotoma or diffuse field loss (figure 3A). One-third of patients have mild optic disc swelling (figure 3B); the remainder have retrobulbar inflammation and the optic nerve head will appear normal. MRI often confirms increased T2 signal and pathologic gadolinium enhancement of the retro-orbital optic nerve. Although the prognosis for recovery of vision is generally good (with a majority of patients returning to 20/20 acuity7), mild residual visual dysfunction is common and may be captured by measures such as contrast sensitivity and stereoacuity.8,9
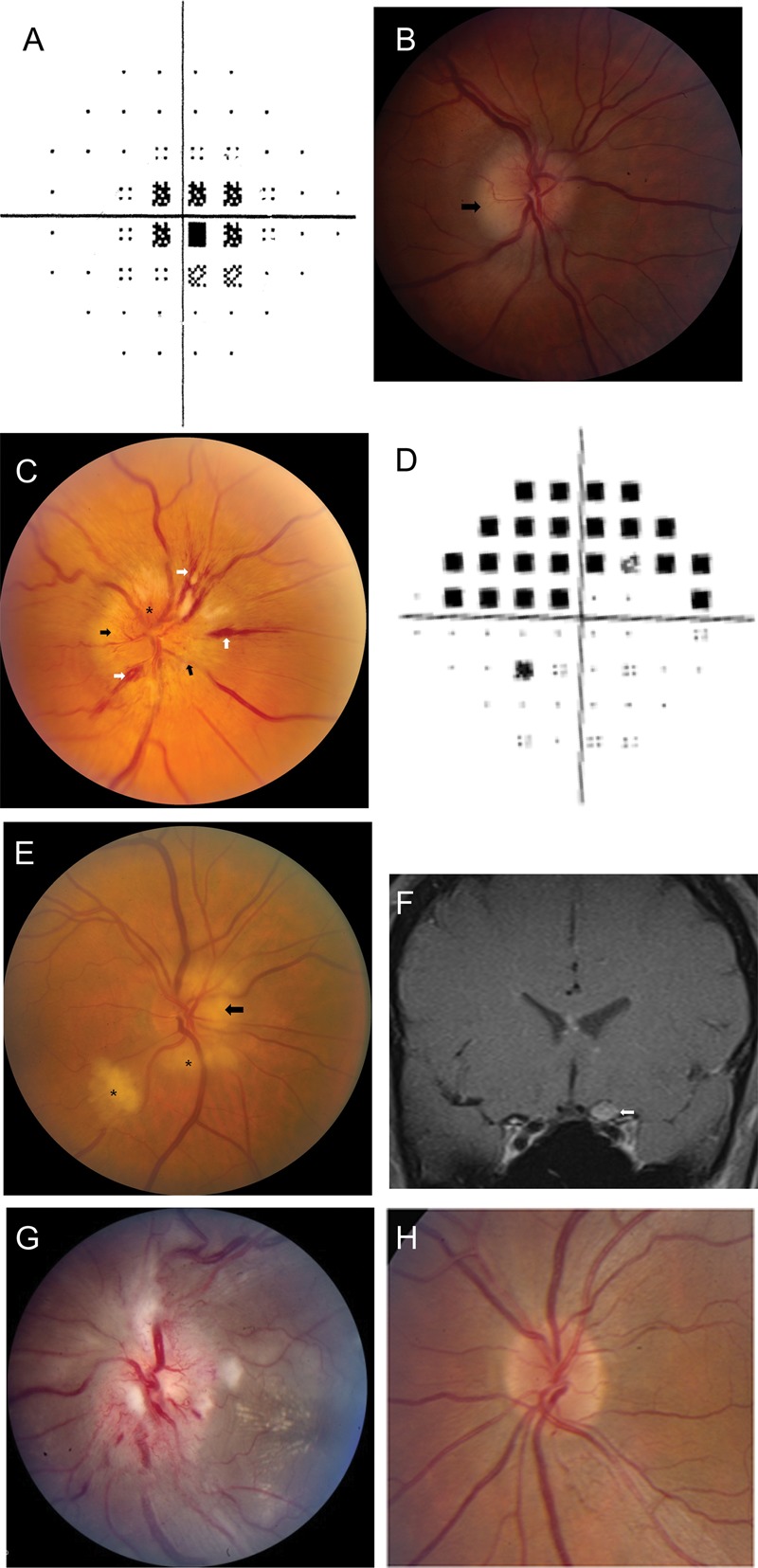
Optic neuropathies
Figure 3. (A) Optic neuritis. Central scotoma on automated perimetry. (B) Optic neuritis. Mild optic disc edema, greatest in the temporal portion (arrow). (C) Nonarteritic ischemic optic neuropathy. Swelling of the optic nerve head (black arrows), splinter hemorrhages (white arrows), and hyperemia of the optic nerve head (asterisk). (D) Nonarteritic ischemic optic neuropathy. Superior arcuate altitudinal field deficit in the right eye. (E) Giant cell arteritis. Pallor and swelling of the optic nerve head (arrow), with retinal cotton wool spots (asterisks). (F) Neurosarcoidosis. Coronal postgadolinum MRI showing enlargement and pathologic enhancement of the left optic nerve (arrow). (G) Neuroretinitis. Marked disc swelling with hyperemia, surrounding cotton-wool spots, and macular exudate in a hemi-star pattern. (H) Leber hereditary optic neuropathy. Peripapillary telangiectasias (at 1 and 5 o'clock). B, C, E, and F reprinted with permission from Prasad et al.20
Features that are atypical for optic neuritis should prompt a rigorous search for other causes.6 These “red flags” include an unusual temporal profile (progression beyond 2 weeks, or lack of recovery within 1 month), absence of pain, an atypical scotoma (such as an altitudinal defect), or an atypical fundus examination (including a nerve that is markedly swollen or atrophic, or retinal abnormalities such as hemorrhages, inflammation, or exudates).
Neuromyelitis optica
Neuromyelitis optica, or Devic disease, typically causes necrotizing demyelinating lesions of the optic nerves and spinal cord. Visual loss may be unilateral, but it is often bilateral, more severe (<20/200 acuity), and more likely to recur than the deficits associated with typical optic neuritis.10 Furthermore, the periorbital pain that is fairly characteristic of optic neuritis may be absent in neuromyelitis optica. Orbital and spinal MRI can reveal extensive regions of signal abnormality and pathologic enhancement. The neuromyelitis optica–immunoglobulin G autoantibody appears to be a useful marker, with reported 76% sensitivity and 91% specificity in a North American population.11 OCT imaging often shows the development of profound loss of retinal nerve fiber layer to less than 60 μm in the affected eye.
Ischemic optic neuropathy
Nonarteritic anterior ischemic optic neuropathy (NAION) is a common cause of unilateral optic neuropathy in adults over age 50. Potential risk factors include diabetes and hypertension, nocturnal hypotension (possibly precipitated by antihypertensive therapy),12 sleep apnea, and the use of phosphodiesterase inhibitors.13 NAION is a clinical diagnosis, relying heavily on the findings of moderate to severe disc edema (often in a wedge-shaped distribution), typically with nerve fiber hemorrhages (figure 3C). Altitudinal visual field loss is common (figure 3D) and pain is virtually universally absent. Inspection of the fellow eye often demonstrates a crowded optic nerve head (with small cup-to-disc ratio). The clinical profile of NAION and optic neuritis may occasionally overlap, and care must be taken to distinguish the two.14 Often, a reliable way to distinguish these entities is by observation, since visual recovery is markedly better for optic neuritis than for NAION. Many patients with NAION will have a stable visual deficit; there can be spontaneous improvement in the first 6 months, although in many patients this reflects improved ability with eccentric fixation.15 OCT imaging may show segmental loss of the retinal nerve fiber layer.
Arteritic anterior ischemic optic neuropathy (AAION) is usually related to giant cell arteritis (GCA), and may cause severe visual loss without early diagnosis and treatment. The prevalence of GCA increases with age, and is rare under the age of 60. The condition is associated with polymyalgia rheumatica, consisting of proximal myalgia and arthralgia, as well as with jaw claudication, fever, malaise, and scalp tenderness. When severe visual loss is present due to GCA, the disc typically appears chalky-white and edematous (figure 3E). The coexistence of retinal ischemia (cotton-wool spots) and disc swelling is highly suggestive of AAION. The diagnosis of GCA is suggested by an elevated erythrocyte sedimentation rate and C-reactive protein, and confirmed by evidence of giant cells and endovascular inflammation on temporal artery biopsy. In suspected cases, treatment with corticosteroids should be initiated promptly, without delay for a biopsy to be obtained.
Posterior ischemic optic neuropathy (PION) is a rare entity presenting with acute, severe optic nerve dysfunction without nerve swelling. In the correct clinical context, posterior ischemic optic neuropathy may be the result of severe blood loss or prolonged surgical procedures (notably spinal surgery). Giant cell arteritis is another important consideration. Nonarteritic posterior ischemic optic neuropathy can occur but is rare.
Other conditions
Inflammatory conditions are an important cause of subacute optic neuropathy, but can occasionally have an acute presentation. Optic nerve involvement occurs in neurosarcoidosis, systemic lupus erythematosus, and Sjögren disease,16 and may be accompanied by anterior uveitis or posterior segment vitritis (figure 3F). Visual loss due to these conditions often is not only steroid-responsive, but also steroid-dependent, with recurrence of visual loss coinciding with withdrawal of steroids.17
Infectious conditions are another frequent cause of optic neuropathy.18 Neuroretinitis, in which optic neuropathy coexists with characteristic peripapillary or macular exudates, is often due to cat scratch disease (Bartonella henselae) (figure 3G). The retinal exudates characteristic of neuroretinitis may form either a complete or partial star pattern. Patients may recognize a history of cat scratches as well as preceding fever and lymphadenopathy. Other infectious optic neuropathies include late syphilis (Treponema pallidum), varicella zoster, Lyme disease (Borrelia burgdorferi), HIV, and opportunistic infections including toxoplasmosis, cytomegalovirus, cryptococcus, mucormycosis, and aspergillosis. Patients with secondary syphilis may not recall the chancres accompanying the primary infection; since this is a treatable condition, serologies should be checked when there is any suspicion. Lyme-associated optic neuritis is relatively rare, but may be considered in a patient with a history of tick exposure, erythema migrans, arthralgias, or positive serologies (typically confirmed by Western blot). Zoster-associated optic neuropathy is also rare but occasionally occurs following zoster ophthalmicus (a vesicular eruption in the V1 distribution). Paranasal sinusitis or mucocele may lead to either compressive or inflammatory optic neuropathy. Suspicion should be higher in elderly patients, those with a history of severe sinus disease, and those with associated fever and ophthalmoparesis.
For many causes of acute monocular visual loss, the diagnosis is based solely on the clinical history and physical examination.
Among neoplastic causes of acute visual loss, primary malignant glioblastoma in adults occasionally originates in the optic nerve and may mimic optic neuritis early in its clinical course. Other neoplastic causes of optic neuropathy include disseminated lymphoma or leukemia, carcinomatous meningitis, and direct optic nerve metastasis (of which breast and lung tumors are most common). Paraneoplastic optic neuropathy is more likely to cause bilateral than unilateral visual loss, but both have been reported. It may precede the manifestation of systemic malignancy, and may present with coexisting retinitis, vitritis, limbic encephalitis, peripheral neuropathy, or ataxia. The antibody most commonly identified is directed toward collapsin response mediated protein-5 (CRMP 5).
LHON presents with acute to subacute visual loss, typically in the second or third decade of life.19 The condition arises from mitochondrial DNA mutations causing dysfunction of the electron transport chain. There is maternal inheritance, with incomplete penetrance within families. Approximately 90% of patients with LHON are men. Loss of vision is bilateral at onset in about 50% of cases, and in the remainder the fellow eye will become affected within 9 months. Although there is no true disc edema in LHON, the optic disc may appear hyperemic and mildly swollen in the acute phase. Circumpapillary telangiectatic vessels are quite characteristic, though not always present (figure 3H). Most patients have permanent vision loss, although the prognosis depends upon the specific mutation harbored; patients with mtDNA mutation T14484C are more likely to have spontaneous recovery than patients with mutations G11778A or G3460A.19 Genetic testing for LHON should be considered in any patient with unexplained sequential or simultaneous bilateral severe optic neuropathies.
Angle closure glaucoma is an important consideration in a patient with painful acute visual loss. It is often distinguished from entities such as optic neuritis by the severity of pain (which can be excruciating) and a red eye with an enlarged, nonreactive pupil.
It is not uncommon for a neurologist to encounter the problem of acute monocular visual loss. In this review, we emphasize the characteristic features that narrow a broad differential diagnosis of retinal and optic nerve diseases, allowing the clinician to execute an efficient, targeted evaluation.
Correspondence to: sprasad2@partners.org
Footnotes
Correspondence to: sprasad2@partners.org
REFERENCES
- 1. O'Neill EC, Danesh-Meyer HV, Connell PP, et al.. The optic nerve head in acquired optic neuropathies. Nat Rev Neurol 2010;6:221–236. [DOI] [PubMed]
- 2. Bruce BB, Newman NJ. Functional visual loss. Neurol Clin 2010;28:789–802. [DOI] [PMC free article] [PubMed]
- 3. Becker M, Masterson K, Delavelle J, Viallon M, Vargas MI, Becker CD. Imaging of the optic nerve. Eur J Radiol 2010;74:299–313. [DOI] [PubMed]
- 4. Mirza RG, Johnson MW, Jampol LM. Optical coherence tomography use in evaluation of the vitreoretinal interface: a review. Surv Ophthalmol 2007;52:397–421. [DOI] [PubMed]
- 5. Damek DM. Paraneoplastic retinopathy/optic neuropathy. Curr Treat Options Neurol 2005;7:57–67. [DOI] [PubMed]
- 6. Balcer LJ. Clinical practice: optic neuritis. N Engl J Med 2006;354:1273–1280. [DOI] [PubMed]
- 7. Group ONS. Visual function 15 years after optic neuritis: a final follow-up report from the Optic Neuritis Treatment Trial. Ophthalmology 2008;115:1079–1082. [DOI] [PubMed]
- 8. Fleishman JA, Beck RW, Linares OA, Klein JW. Deficits in visual function after resolution of optic neuritis. Ophthalmology 1987;94:1029–1035. [DOI] [PubMed]
- 9. Cleary PA, Beck RW, Bourque LB, Backlund JC, Miskala PH. Visual symptoms after optic neuritis: results from the Optic Neuritis Treatment Trial. J Neuroophthalmol 1997;17:18–23; quiz 24–18. [DOI] [PubMed]
- 10. Merle H, Olindo S, Bonnan M, et al.. Natural history of the visual impairment of relapsing neuromyelitis optica. Ophthalmology 2007;114:810–815. [DOI] [PubMed]
- 11. Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology 2006;66:1485–1489. [DOI] [PubMed]
- 12. Hayreh SS, Podhajsky P, Zimmerman MB. Role of nocturnal arterial hypotension in optic nerve head ischemic disorders. Ophthalmologica 1999;213:76–96. [DOI] [PubMed]
- 13. Fontal MR, Kerrison JB, Garcia R, Oria V. Ischemic optic neuropathy. Semin Neurol 2007;27:221–232. [DOI] [PubMed]
- 14. Rizzo JF 3rd, Lessell S. Optic neuritis and ischemic optic neuropathy. Overlapping clinical profiles. Arch Ophthalmol 1991;109:1668–1672. [DOI] [PubMed]
- 15. Hayreh SS, Zimmerman MB. Nonarteritic anterior ischemic optic neuropathy: natural history of visual outcome. Ophthalmology 2008;115:298–305. [DOI] [PMC free article] [PubMed]
- 16. Delalande S, de Seze J, Fauchais AL, et al.. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine 2004;83:280–291. [DOI] [PubMed]
- 17. Kidd D, Burton B, Plant GT, Graham EM. Chronic relapsing inflammatory optic neuropathy (CRION). Brain 2003;126:276–284. [DOI] [PubMed]
- 18. March GA Jr, Lessell S. Infectious optic neuropathy. Int Ophthalmol Clin 1996;36:197–205. [DOI] [PubMed]
- 19. Newman NJ. Hereditary optic neuropathies: from the mitochondria to the optic nerve. Am J Ophthalmol 2005;140:517–523. [DOI] [PubMed]
- 20. Prasad S, Volpe NJ, Balcer LJ. Approach to optic neuropathies: clinical update. Neurologist 2010;16:23–34. [DOI] [PubMed]