Abstract
Microfracture of hip chondral lesions has been performed for more than a decade with modified treatment principles and techniques from knee arthroscopy. This note and accompanying video review the pertinent techniques, pearls, and pitfalls of the microfracture procedure in the treatment of hip chondral lesions. After debridement of damaged chondral tissue, the size of the lesion is approximated to determine the number of microfracture holes to create. The working portal may be adjusted based on the site of the lesion. Microfracture picks of different angles are used to ensure perpendicular advancement to a depth of 3 to 4 mm in the subchondral bone. The holes are placed at a gap of approximately 3 to 4 mm. The debris is washed out to obtain open holes connecting the marrow with the articular surface. The microfracture procedure should be performed near the end of the overall procedure to secure the bleeding bone marrow within the joint and prevent washout.
Microfracture is a popular and well-established marrow-stimulating procedure in the treatment of articular cartilage defects in the knee. Indications for the use of microfracture in arthroscopic management of chondral defects in the hip, however, remain a topic of debate and are poorly defined in the literature. The principles and techniques for treating chondral defects in the hip are primarily derived from knee arthroscopy. Although microfracture of hip chondral defects continues to grow in popularity, there have been few resources that describe and address the technical aspects of the procedure.1 In this Technical Note and accompanying video, we describe microfracture of the hip, including various tips, pearls, and pitfalls of the procedure.
Surgical Technique
In the supine position, the anterolateral and modified anterior portals are initiated with 2 separate limited capsulotomies as previously described (Video 1).2
-
1.
After localizing the pathologic defect, the chondral lesion is examined using an arthroscopic probe (Fig 1). The size of the lesion is measured using an arthroscopic ruler or a shaver. Debridement of chondral flaps or chondral tissue remnants is performed with straight and curved 4.5- and/or 5.5-mm full radius shavers (Smith & Nephew, Andover, MA) (Fig 2). Margins of the lesion are determined and prepared sharply and perpendicularly with a 45° open arthroscopic curette (Smith & Nephew) (Fig 3). Calcified cartilage is removed gently without violating the subchondral bone underneath, via a 45° open arthroscopic rectangular ring curette (Smith & Nephew) (Fig 4). The tissue debris is washed out using shaver suction. The final lesion is examined globally to determine where and how many holes to create (Fig 5).
-
2.
Rim trimming and labral repair are performed as needed. If a femoroplasty needs to be performed, traction is relaxed to facilitate the procedure. Afterwards, traction is reapplied to perform the microfracture procedure.
-
3.
For acetabular lesions, a 90° double-angled arthroscopic microfracture pick (Smith & Nephew) is used. The working portal is chosen based on the lesion site: anterior-based portals for anterior acetabular lesions, anterolateral portal for superior acetabular lesions, and posterolateral portal for posterior acetabular wall lesions.
-
4.
For femoral head lesions, a 45° arthroscopic solid pick (Smith & Nephew) is used, and the portals are again changed based on the site of the lesion. Rotation of the lower extremity can be used to achieve a perpendicular insertion of the pick. For certain lesions, 90° solid picks can also be used (Table 1).
-
5.
The microfracture pick is inserted in a perpendicular fashion to a depth of 3 to 4 mm, while observing for the fatty yellow bone marrow to exit from the opened hole (Fig 6). Approximately 3- to 4-mm gaps are maintained from one hole to the next to avoid combining the holes (Fig 7). After establishing the holes with the microfracture pick, the debris is washed out to obtain open holes, connecting the marrow with the articular surface (Fig 8). After suctioning out the irrigation fluid, dense fatty marrow bleeding from the microfracture holes can be observed (Fig 9).
Fig 1.
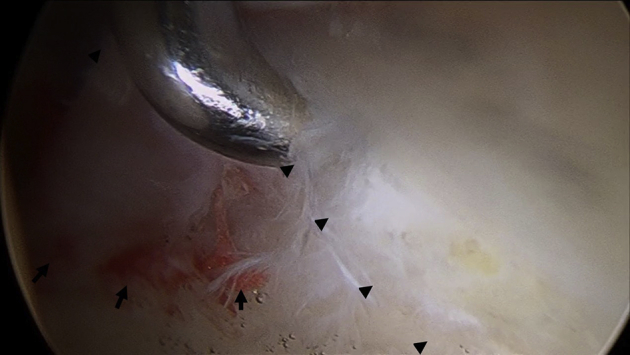
Examination of the lesion with an arthroscopic probe. Arrow heads indicate the chondrolabral junction. Black arrows indicate the articular cartilage delamination. Lesion extends from 11- to 1-o'clock position in the left hip. The arthroscopic probe is introduced from the modified anterior portal and the camera is introduced from the anterolateral portal. The probe penetrates into the chondrolabral delamination.
Fig 2.
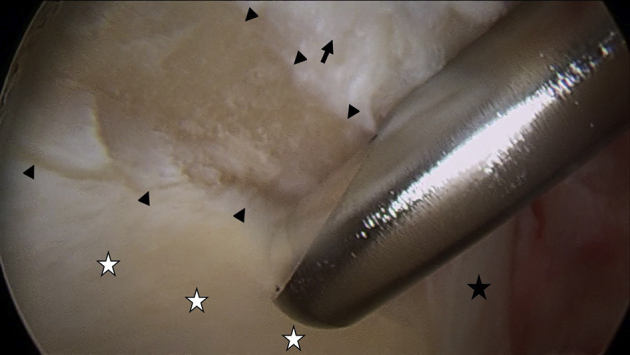
Debridement of the chondral flap or chondral tissue remnants. Black arrow heads indicate the border of the articular cartilage defect. The black star is on the healthy labral tissue and the white stars are on the healthy articular cartilage. The black arrow shows the injured labrum. A straight 4.5-mm full-radius shaver (Smith & Nephew), which is introduced from the anterolateral portal, debrides the injured chondral flaps. The camera is introduced from the modified anterior portal.
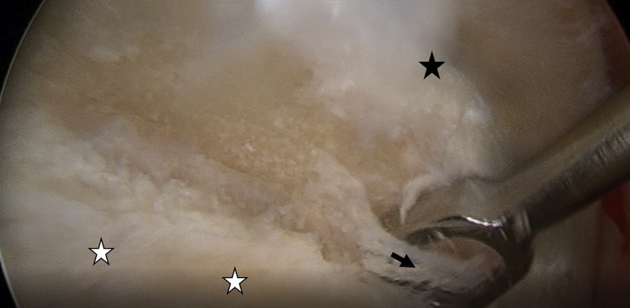
Fig 3.

Preparation of the margins of the lesion. Black arrow heads indicate the border of the articular cartilage defect. The black star is on the healthy labral tissue and the white stars are on the healthy articular cartilage. Margins of the lesion are determined and prepared sharply and perpendicularly by a 45° open arthroscopic curette (Smith & Nephew), which is introduced from the anterolateral portal. The camera is introduced from the modified anterior portal in the left hip.
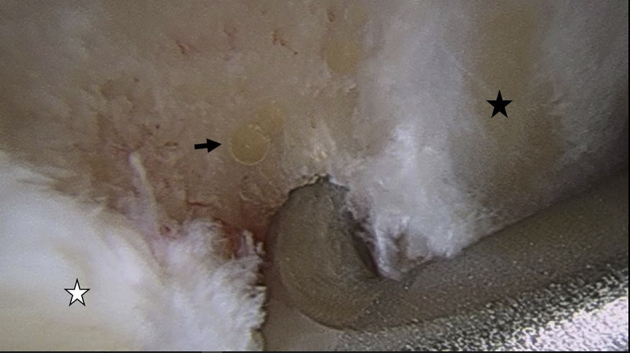
Fig 4.
Removal of the calcified cartilage over the subchondral bone. A 45° open arthroscopic rectangular curette (Smith & Nephew) removes the calcified cartilage (black arrow) over the subchondral bone. White stars are on the healthy cartilage and the black star is on the labral tissue. The curette is introduced from the anterolateral portal and the camera from the modified anterior portal in the left hip.
Fig 5.

Determination of the possible hole locations. The final lesion is examined globally to determine where and how many holes to create. The microfracture pick is introduced from the anterolateral portal and the camera from the modified anterior portal in the left hip. The white star is on the healthy cartilage and the black star is on the labral tissue.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
Fig 6.
The microfracture pick is inserted in a perpendicular fashion to a depth of 3-4 mm, while observing for the fatty yellow bone marrow (black arrow) to exit from the opened hole. The microfracture pick is introduced from the anterolateral portal and the camera from the modified anterior portal in left hip. The white star is on the healthy cartilage and the black star is on the labral tissue.
Fig 7.
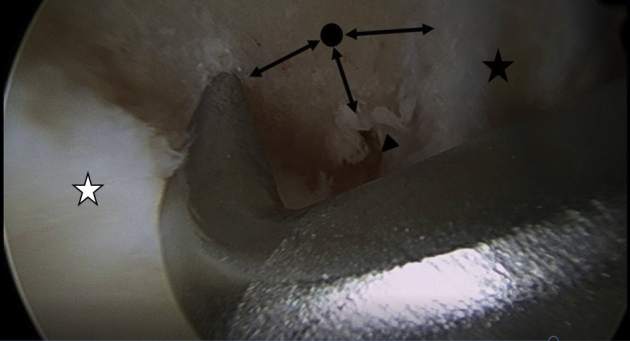
The microfracture sites should be created approximately 3-4 mm apart to prevent combining the holes. The black arrow head shows the first opened hole. The pick is on the next hole and black point is on the following hole. Each double-headed arrow indicates the 3-4 mm distances between microfracture holes. The white star is on the healthy cartilage and the black star is on the labral tissue. The microfracture pick is introduced from the anterolateral portal and the camera from the modified anterior portal in the left hip.
Fig 8.
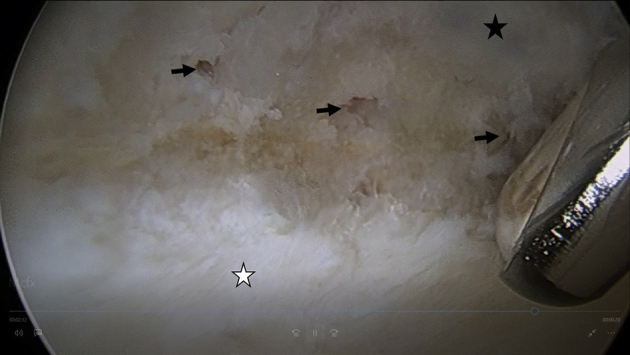
After creating all the holes, the debris is removed by a shaver to obtain open clear holes (black arrows). The white star is on the healthy cartilage and the black star is on the labral tissue. The shaver is introduced from the anterolateral portal and the camera from the modified anterior portal in the left hip.
Fig 9.
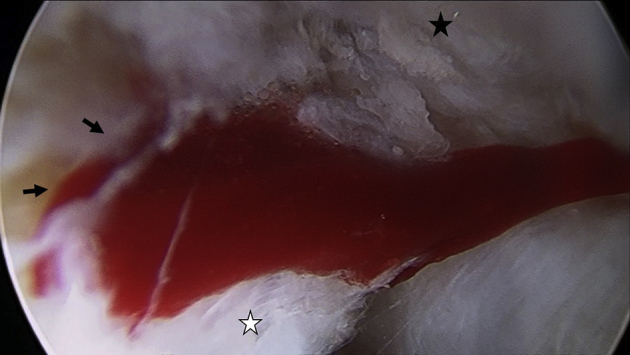
Dense fatty marrow bleeding from the microfracture site (black arrows) was observed after sucking out the irrigation fluid. The camera is introduced from the modified anterior portal in the left hip. The white star is on the healthy cartilage and the black star is on the labral tissue.
Rehabilitation Program After Hip Microfracture
-
1.
Cryotherapy packs are used immediately in the recovery room to decrease pain and inflammation. An antirotation splint can be used while sleeping to protect against shear forces.
-
2.
Continuous passive motion machines are employed for 8 hours per day for 8 weeks.
-
3.
Assisted passive range-of-motion exercises are started on postoperative day 1. Active assisted range-of-motion exercises are started on postoperative day 4. Strengthening exercises start after the 12th week.
-
4.
The patient is made to weight-bear 20 pounds flat-foot for 8 weeks, before gradually returning to full weight-bearing as tolerated (Table 1).
-
5.
Upper extremity, core, and thigh muscle strengthening can be started just hours after the operation. If all rehabilitation milestones are reached, return to competitive sports can be advised after 16 weeks.
Discussion
The indication for microfracture of the hip is focal, full-thickness (Outerbridge grade IV), and contained lesions typically less than 2 cm2 in area. Further, those defects in weight-bearing areas, unstable lesions with intact subchondral bone, and focal lesions without evidence of surrounding chondromalacia in patients younger than 50 years should be considered as well.4 Conversely, some studies have demonstrated promising results even for larger-sized lesions and in the elderly population (Table 2).5 Contraindications to microfracture of the hip include partial-thickness chondral lesions accompanied by bony defects and patients who are not able to comply with the rehabilitation protocol, including patients who are unable to use their other leg for weight-bearing.
Table 2.
Advantages and Disadvantages of the Microfracture in Hip Chondral Lesions
| Advantages | Disadvantages |
|---|---|
|
|
Some authors do not recommend microfracture because of the potential formation of subchondral cysts created by destruction of subchondral anatomy (Table 2).6 Various techniques have been described for hip microfracture procedures. Drilling has some advantages, including creating less debris with a better-shaped hole that facilitates bone marrow migration to the defect.7 Some published reports, however, have raised concerns regarding thermal necrosis with drilling of the bone.8 More recently, nanofracture with small diameter and deeper subchondral penetration have demonstrated better outcomes when compared with standard awls.6
In the knee, ease of access to the joint may allow for conversion to open or mini-open techniques for grafting procedures. In the hip, however, open management of chondral lesions requires an extensile approach, which includes surgical dislocation of the hip with trochanteric osteotomy (Table 2). Although debate persists over the indications for microfracture and its use in the hip, the procedure remains the best option currently, even for large chondral lesions and in older patients.5 Continued research on this topic and long-term outcomes are required to more clearly define the indications for microfracture of the hip.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.J.S. is a board member of the Journal of Hip Preservation Surgery (no financial support) and the International Society of Hip Arthroscopy (no financial support); a paid consultant for Smith & Nephew; employed as an attending surgeon at Wake Forest Baptist Health and as an Associate Professor at Wake Forest School of Medicine; receives research grant support from Bauerfeind; stock holder at Johnson & Johnson; received travel expenses from the Arthroscopy Association of North America; and received unrestricted educational grants to department from Arthrex, DePuy-Mitek, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This technical video explains the basic principles of arthroscopic microfracture of hip chondral lesions. A camera is introduced from the modified anterior portal in the left hip, and instruments from the anterolateral portal. The first step is the arthroscopic examination of the joint and identification and grading of the chondral lesion. Debridement of the delaminated chondral tissue is performed. To obtain perpendicular healthy chondral borders, an open rectangular ring curette is used. Abrasion of the calcified layer is performed without violating the subchondral bone. All debris is washed out and cleaned up using a suction shaver. Rim trimming and labral repair are performed as needed. Traction is released to perform a femoroplasty procedure. Contact-free relation between the femoral neck and the lesion side is obtained by gradual femoroplasty. After observing the lesion globally and approximating the possible hole locations, an arthroscopic microfracture pick is introduced and inserted into the subchondral bone to a depth of 3-4 mm at a perpendicular angle. The extraction of the yellow fatty marrow is visualized for confirmation of the penetration depth. It is important to leave 3-4 mm of space between the holes. Debris created by microfracture is washed out to obtain clean holes. After suctioning out the irrigation fluid, the marrow bleeding can be visualized.
References
- 1.McCarthy J.C. The diagnosis and treatment of labral and chondral injuries. Instr Course Lect. 2004;53:573–577. [PubMed] [Google Scholar]
- 2.Howse E.A., Botros D.B., Mannava S., Stone A.V., Stubbs A.J. Basic hip arthroscopy: anatomic establishment of arthroscopic portals without fluoroscopic guidance. Arthrosc Tech. 2016;5:e247–e250. doi: 10.1016/j.eats.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck A., Murphy D.J., Carey-Smith R., Wood D.J., Zheng M.H. Treatment of articular cartilage defects with microfracture and autologous matrix-induced chondrogenesis leads to extensive subchondral bone cyst formation in a sheep model. Am J Sports Med. 2016;44:2629–2643. doi: 10.1177/0363546516652619. [DOI] [PubMed] [Google Scholar]
- 4.McGill K.C., Bush-Joseph C.A., Nho S.J. Hip microfracture: Indications, technique, and outcomes. Cartilage. 2010;1:127–136. doi: 10.1177/1947603510366028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trask D.J., Keene J.S. Analysis of the current indications for microfracture of chondral lesions in the hip joint. Am J Sports Med. 2016;44:3070–3076. doi: 10.1177/0363546516655141. [DOI] [PubMed] [Google Scholar]
- 6.Zedde P., Cudoni S., Giachetti G. Subchondral bone remodeling: Comparing nanofracture with microfracture. An ovine in vivo study. Joints. 2016;4:87–93. doi: 10.11138/jts/2016.4.2.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen H., Sun J., Hoemann C.D. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res. 2009;27:1432–1438. doi: 10.1002/jor.20905. [DOI] [PubMed] [Google Scholar]
- 8.Steadman J.R., Rodkey W.G., Rodrigo J.J. Microfracture: Surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001:S362–S369. doi: 10.1097/00003086-200110001-00033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This technical video explains the basic principles of arthroscopic microfracture of hip chondral lesions. A camera is introduced from the modified anterior portal in the left hip, and instruments from the anterolateral portal. The first step is the arthroscopic examination of the joint and identification and grading of the chondral lesion. Debridement of the delaminated chondral tissue is performed. To obtain perpendicular healthy chondral borders, an open rectangular ring curette is used. Abrasion of the calcified layer is performed without violating the subchondral bone. All debris is washed out and cleaned up using a suction shaver. Rim trimming and labral repair are performed as needed. Traction is released to perform a femoroplasty procedure. Contact-free relation between the femoral neck and the lesion side is obtained by gradual femoroplasty. After observing the lesion globally and approximating the possible hole locations, an arthroscopic microfracture pick is introduced and inserted into the subchondral bone to a depth of 3-4 mm at a perpendicular angle. The extraction of the yellow fatty marrow is visualized for confirmation of the penetration depth. It is important to leave 3-4 mm of space between the holes. Debris created by microfracture is washed out to obtain clean holes. After suctioning out the irrigation fluid, the marrow bleeding can be visualized.


