Abstract
Meniscal injuries and meniscal loss are associated with changes in knee kinematics and loading, ultimately leading to poor functional outcomes and increased risk of progression to osteoarthritis. Biomechanical studies have shown restored knee function, and clinical studies have reported improved outcomes and decreased risk of osteoarthritis after meniscal repair. This has led orthopaedic surgeons to try and save the meniscus by repair whenever possible, as shown by increasing incidence of meniscal repair surgeries. Historically, meniscal lesions, particularly those greater in size and located in the white-white region of the meniscus, have been shown to have poor healing. In recent years, there has been an increasing interest in the use of biologic agents to help stimulate and expedite healing in traditionally more avascular tissue. Preliminary results for biologic therapeutic agents, such as platelet rich plasma and bone marrow aspirate concentrate, have been encouraging. However, these options are more demanding in regard to time, financial burden, resources, and regulations than some more classic agents such as fibrin clots. Fibrin clot is readily available, easy to use, affordable, and minimally invasive. This Technical Note describes a step-by-step and reproducible technique for harvesting, preparation, and using a fibrin clot to augment healing of meniscal repairs.
Meniscal damage has long been known to lead to expedited onset of osteoarthritis (OA) and long-term pain and debilitation of the tibiofemoral joint.1, 2 More recently, there has been a push toward more aggressive repair of acute meniscal lesions.3 Follow-up has shown repair to significantly improve patient outcomes as well as delaying the onset of OA when compared with meniscectomy.4, 5 There is still some disagreement when deciding to attempt a meniscal repair due to contradicting outcomes involving the ability for a meniscus to heal, even with repair.6, 7 Of particular concern is the “white-white” region of the meniscus that is known to be highly avascular and therefore does not have great healing potential.8 With this in mind, techniques to improve healing of the meniscus have long been used, including fibrin clots.9
More recently there has been increased usage of more advanced healing stimulators including platelet rich plasma (PRP) and bone marrow aspirate concentrate (BMAC).10, 11, 12 However, although early studies have shown some advantages to these techniques, they are technically challenging, time consuming, invasive, and very expensive for the patient. The recent attention on healing stimulators has led to renewed interest in the use of fibrin clots due to ease of preparation, low cost, and minimal invasiveness. Fibrin clots are formed by an intrinsic clotting process and by stirring of the patient's blood. Furthermore, fibrin clots allow surgeons to more precisely localize desired biologic factors at the site of repair. The purpose of this technique is to describe a reproducible and simplistic way to harvest, create, and use a fibrin clot, as well as provide step-by-step instructions via video and text on how to place the clot arthroscopically.
Surgical Technique
Patient Positioning
The patient is placed in the supine position on the operating table (Fig 1). After the induction of general anesthesia, a bilateral knee examination is performed to assess range of motion and evaluate for any concurrent ligamentous instability. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, which is positioned into a leg holder (Mizuho OSI, Union City, CA). The contralateral knee remains in an abduction stirrup (Birkova Product LLC, Gothenburg, NE) with a pneumatic compression device.
Fig 1.
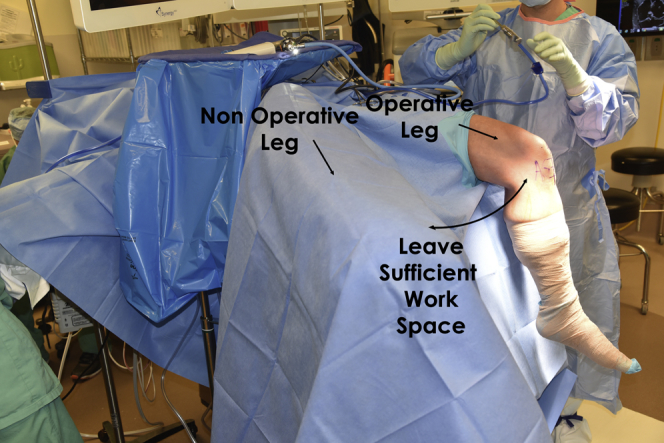
Patient positioning. The operative (left) leg is sterilized in the standard fashion. Coband is wrapped around the calf and extended distally around the patient's left foot. The surgeon should ensure that sufficient work space is exposed around the patient's knee.
The anterolateral portal is created first in a vertical fashion adjacent to the patellar tendon and the joint is initially inspected. With the aid of a spinal needle to assess location, the anteromedial portal is created next in a similar manner. The meniscal margins are probed and any unstable peripheral meniscal tears are considered for repair.
Surgical Approach
Common approaches for inside-out meniscal repair techniques, including posteromedial and posterolateral, are performed as previously described.13 Briefly, for a posteromedial approach, an arthroscopic probe is placed inside the joint to help locate the planned incision and identify the joint line. An oblique vertical incision is performed posterior to the medial collateral ligament extending from the adductor tubercle to the posterior aspect of the tibial plateau (2 cm distal to the joint line). Because of the proximity of the saphenous nerve, care must be taken to ensure that the incision is not placed too far posterior.
After sharp and then blunt dissection of the sartorius fascia, an anatomic triangle composed of the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly, and the semimembranosus inferiorly is identified. Careful dissection of the posteromedial joint capsule away from adhesions to the medial gastrocnemius complex is performed to allow for improved visualization and to permit passage of a neurovascular protector. Furthermore, a Cobb elevator is then used to separate the medial gastrocnemius tendon and muscle from any posterior capsular adhesions. A tablespoon or other device can be placed in this interval to act as a retractor, protecting the popliteal vessels. Similarly, for the posterolateral approach, a vertical skin incision is made posterior to the fibular collateral ligament. A transverse oblique incision is performed after the posterior border of the iliotibial band down to Gerdy's tubercle, centered over the lateral joint line. Care must be taken to avoid the common peroneal nerve that is located posteromedial to the biceps femoris tendon. Next, blunt dissection is performed toward the fibular head, and an interval is created with the lateral head of the gastrocnemius superiorly and posterolateral joint capsule anteriorly. The muscle of the gastrocnemius can be bluntly dissected off the capsule in a similar fashion as the medial approach. Again, a tablespoon or other device can be placed in this interval to act as a retractor for the neurovascular structures.
Meniscal Suture
Before the repair, the lesion should be identified and characterized based on its location, size, stability, and overall quality. The tear should be anatomically reduced and the sutures should be placed perpendicularly to the lesion to restore its anatomic position. In this case, the patient had a vertical undersurface tear that was found to be extremely unstable when probed.
The authors prefer an inside-out repair technique because of the ability to confer greater stability to the lesion via increased number of sutures, and not having to use a large intra-articular device that allows for greater versatility. Double-loaded nonabsorbable No. 2.0 Fiberwire sutures (Arthrex, Naples, FL) are placed via a self-delivery gun fitted with a cannula (Sharpshooter, ConMed Linvatec, Largo, FL) into the meniscus. Vertical mattress sutures were passed via a previously described technique.1 In total 6 vertical mattress sutures were needed to repair the lesion for stronger construct (unpublished data).
Fibrin Clot Preparation and Usage
Pearls and risk/pitfalls and how to avoid them are listed in Tables 1 and 2, respectively. Video 1 shows the technique in detail. Although the meniscal repair is being undertaken, 60 mL of blood can be drawn from a peripheral site (Figs 2 and 3), in this case, via subcutaneous veins on the dorsum of the hand. Approximately 60 cc of blood is collected and then placed in a basin. An assistant can stir the blood with a glass syringe for approximately 15 minutes to assure adequate clot formation around the glass syringe (Fig 4).
Table 1.
Pearls for A Successful Fibrin Clot Augmentation for Meniscus Repair
|
Table 2.
Risk and Pitfalls for A Successful Fibrin Clot–Augmented Meniscus Repair
| Risks/Pitfalls | How to Avoid Them |
|---|---|
| Injury to the popliteal artery and its branches | Careful dissection and use the heads of the gastrocnemius to protect vascular structures/Use a spoon or other retractor to protect the exit of the needles |
| Injury to the saphenous nerve | Attention should be paid to avoid placing the medial incision too posterior |
| Flexion contracture/stiffness | Do not overtight the sutures Early mobilization (0° to 90°) with an experienced physical therapist |
| Deep venous thrombosis (DVT) | Use of intra- and postoperative DVT prophylaxis |
Fig 2.
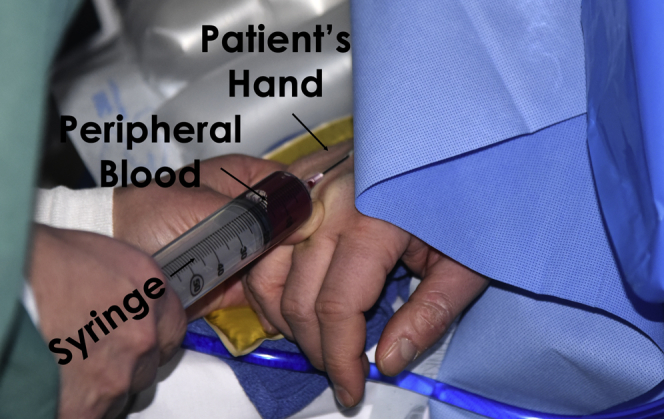
Peripheral blood draw being performed to prepare a fibrin clot. A 60 cc syringe is used to draw up blood from a peripheral vein on the dorsal aspect of the patient's right hand. Approximately 60 cc of patient blood should be drawn to prepare the fibrin clot.
Fig 3.
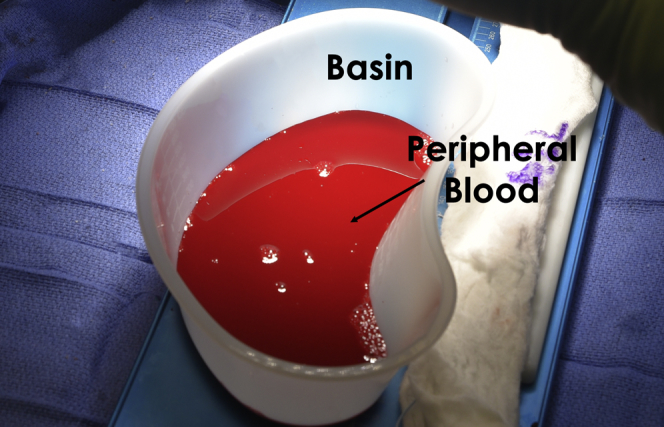
Sixty cubic centimeters of blood is collected from the patient and then placed in a basin on the surgical field.
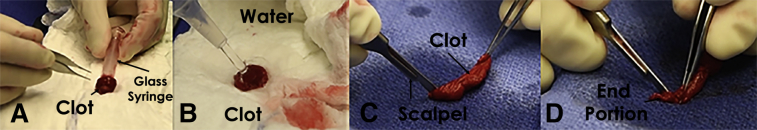
Fig 4.
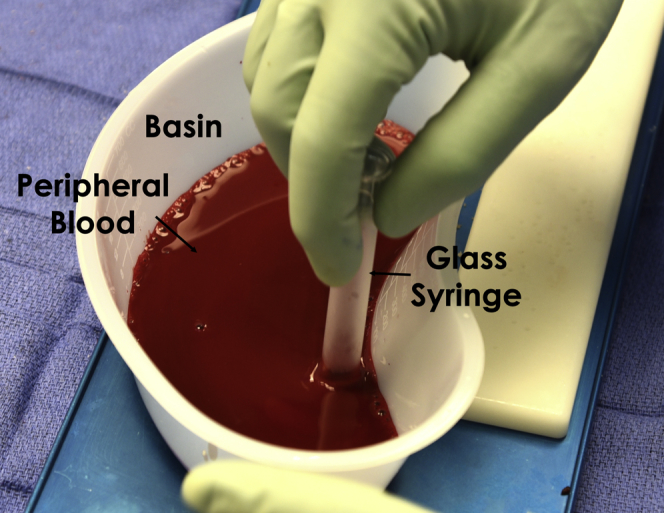
After placing approximately 60 cc of blood into the basin, a surgical assistant then stirs the blood with a glass syringe for approximately 15 minutes to assure adequate clot formation around the glass syringe.
Once an adequate clot has formed on the distal aspect of the syringe, it can be transferred to a sterile surgical sponge. Water is then applied to help further condense the clot and to help improve its visibility arthroscopically. A scalpel and pickups can then be used to shape the clot to best fit the meniscal lesion (Fig 5).
Fig 5.
Clot preparation steps. (A) After approximately 15 minutes of stirring, the fibrin clot is carefully removed from the glass syringe onto a sterile surgical pad. (B) A baster is used to add 2 to 3 drops of water to enhance clot formation, which allows for improved clot visualization during arthroscopy. (C) A scalpel and pickups can then be used to shape the clot to best fit the meniscal lesion. (D) Final fibrin clot product, ready to arthroscopic implantation into the surgical site.
A grasper is then used to introduce the clot through the anterolateral arthroscopic portal. The meniscal sutures previously placed were loosened so that the clot can fit underneath the meniscus and have the best contact area with the lesion. The knee was then taken to 90° of flexion and the sutures were fastened down and then tied (Figs 6 and 7).
Fig 6.
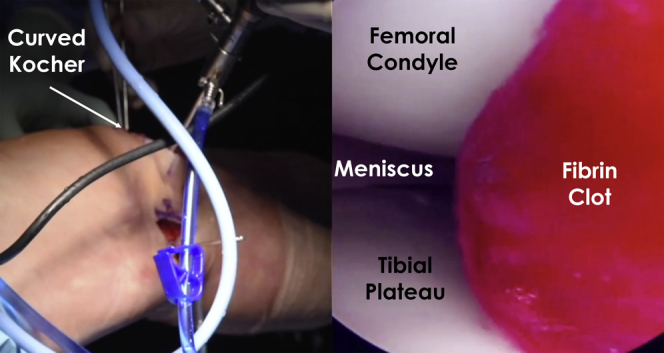
Intraoperative image showing the insertion of the fibrin clot with a curved Kocher forceps (on the left) and arthroscopic picture (as viewed from the anteromedial portal) of the clot entering the joint on a right knee (image on the right).
Fig 7.
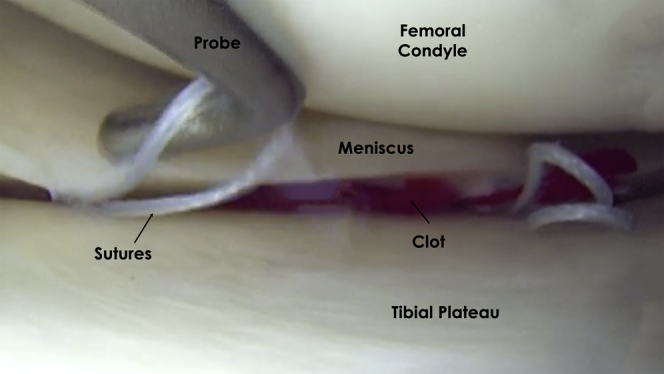
Arthroscopic view (anterolateral portal) demonstrating the sutures and the fibrin clot underneath the meniscus. After the clot is stabilized by the sutures, the knee was flexed to 90° of flexion and the sutures were fastened down and then tied over the posteromedial capsule.
Postoperative Rehabilitation for Isolated Meniscal Repairs
Postoperatively, all patients with an isolated meniscus tear remain non-weight-bearing for 6 weeks. Physical therapy emphasizes early quadriceps muscle activation and knee flexion from 0° to 90° restricted for the first 2 weeks and progressed thereafter. Six weeks postoperatively, weight-bearing is initiated. Also at this time, patients may begin the use of a stationary bike with low resistance settings and 25% body weight leg presses to a maximum of 70° of knee flexion. All increases in low-impact knee exercises are permitted as tolerated starting at 12 weeks postoperatively. Patients are recommended to avoid deep squatting, sitting cross-legged, or performing any heavy lifting or squatting activities for a minimum of 4 months after surgery. After 4 months, full flexion, squatting, and return to full activities or sports is allowed.
Discussion
Meniscal repairs are increasing in prevalence because of outcome studies showing improved International Knee Documentation Committee scores and decreased incidence and delayed onset of OA when compared with meniscectomy. That being said, because of the vascular supply of the meniscus being somewhat restricted, outcomes of meniscal repairs are currently limited by the menisci's ability to heal. Early results have been promising regarding the healing properties of biologics; however, much more research and long-term follow-up is needed. Preparation of BMAC and PRP requires additional preparation and costs related to the machinery required for preparation. On the contrary, preparation of a fibrin clots does not require additional machinery or laboratory assistants, thereby lowering the cost of treatment.
While these biologics approaches are seemingly viable options for improving healing, many are too expensive and time consuming to be utilized by the general public. With this in mind, more simple and less expensive options such as the fibrin clot are a good alternative for patients.
Fibrin clots have been used in the treatment of meniscal pathology for some time. Arnoczky and Warren8 helped to show how the fibrin clot works histologically. They showed that areas of a meniscal tear that had been filled with fibrin clot healed through proliferation of fibrous connective tissue that eventually became fibrocartilaginous tissue.8 Clinical studies also have shown promising results with high rates of meniscal healing after repair with a fibrin clot.13, 14, 15
In conclusion, the use of a fibrin clot is a worthwhile strategy to be used, especially in radial tears, to help with healing of meniscal repairs. We recommend using our described technique for the harvest, formation, and placement of the fibrin clot. We feel that our technique is not only very reproducible but also less technically challenging and financially costly than some other alternatives. In the future, more studies should be performed regarding fibrin clots and other biologics and their benefit on more complex meniscal tears with historically worse outcomes. Also more long-term studies should be undertaken to see if this positive effect on meniscal healing after repair leads to improved long-term subjective and objective outcomes.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives support and consultancy fees from Arthrex, Ossur, and Smith & Nephew; has grants/grants pending from Health East, Norway; NIH R-13 grant for biologics; has patents (planned, pending or issued) from Ossur and Smith & Nephew; receives royalties from Arthrex, Ossur, and Smith & Nephew; and has board membership in American Journal of Sports Medicine and Knee Surgery Sports Traumatology and Arthroscopy. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess for range of motion and evaluate for any concurrent ligament instability. A well-padded high-thigh tourniquet is subsequently placed on the right knee, which is positioned into a leg holder. The leg is prepared and draped in a sterile fashion. A standard anterolateral portal is created, and the anteromedial portal is created arthroscopically guided. A diagnostic arthroscopy is then performed. The menisci are probed and the tears are evaluated for repair. To perform an inside-out meniscal repair, a posteromedial approach is then performed as previously described by Chahla et al.13 An oblique vertical incision is performed from the adductor tubercle to the posterior aspect of the tibial plateau. An anatomic triangle composed of the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly, and the semimembranosus inferiorly is identified. A tablespoon is then placed in this interval to act as a retractor, protecting the popliteal vessels. Attention is then drawn to the meniscal repair. The tear is anatomically reduced and the sutures are placed perpendicularly to the lesion to restore its anatomic position. Double-loaded nonabsorbable No. 2.0 Fiberwire sutures are placed via a self-delivery gun fitted with a cannula into the meniscus. Vertical mattress sutures are placed for a strong construct. While the meniscal repair is being performed, 60 mL of blood is drawn from a peripheral site, in this case via subcutaneous veins on the dorsum of the hand. The blood is then placed in a basin. An assistant stirs the blood with a glass syringe for approximately 15 minutes to assure adequate clot formation. Once an adequate clot has formed on the distal aspect of the syringe, it is transferred to sterile surgical sponge. Temperate normal saline is then gently applied to help further condense the clot and to help improve its visibility arthroscopically. A scalpel and pickups are used to shape the clot to best fit the meniscal lesion. A grasper is then used to gently introduce the clot through the anterolateral portal. The meniscal sutures previously placed are loosened so that the clot could fit underneath the meniscus and have the best contact area with the lesion. After placing the fibrin clot, the knee is taken to 90° of flexion and the sutures are fastened down and then tied. The portals and the incision are then closed.
References
- 1.Hede A., Larsen E., Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16:122–125. doi: 10.1007/BF00180200. [DOI] [PubMed] [Google Scholar]
- 2.Verdonk R., Madry H., Shabshin N. The role of meniscal tissue in joint protection in early osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24:1763–1774. doi: 10.1007/s00167-016-4069-2. [DOI] [PubMed] [Google Scholar]
- 3.Parker B.R., Hurwitz S., Spang J., Creighton R., Kamath G. Surgical trends in the treatment of meniscal tears: Analysis of data from the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2016;44:1717–1723. doi: 10.1177/0363546516638082. [DOI] [PubMed] [Google Scholar]
- 4.Xu C., Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: The more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164–170. doi: 10.1007/s00167-013-2528-6. [DOI] [PubMed] [Google Scholar]
- 5.Lutz C., Dalmay F., Ehkirch F.P., French Arthroscopy Society Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res. 2015;101(suppl):S327–S331. doi: 10.1016/j.otsr.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Krych A.J., Reardon P., Sousa P., Levy B.A., Dahm D.L., Stuart M.J. Clinical outcomes after revision meniscus repair. Arthroscopy. 2016;32:1831–1837. doi: 10.1016/j.arthro.2016.01.070. [DOI] [PubMed] [Google Scholar]
- 7.Barber-Westin S.D., Noyes F.R. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30:134–146. doi: 10.1016/j.arthro.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Arnoczky S.P., Warren R.F. The microvasculature of the meniscus and its response to injury: An experimental study in the dog. Am J Sports Med. 1983;11:131–141. doi: 10.1177/036354658301100305. [DOI] [PubMed] [Google Scholar]
- 9.Van Trommel M.F., Simonian P.T., Potter H.G., Wickiewicz T.L. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy. 1998;14:360–365. doi: 10.1016/s0749-8063(98)70002-7. [DOI] [PubMed] [Google Scholar]
- 10.Lee H.R., Shon O.J., Park S.I. Platelet-rich plasma increases the levels of catabolic molecules and cellular dedifferentiation in the meniscus of a rabbit model. Int J Mol Sci. 2016;17:E120. doi: 10.3390/ijms17010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Desando G., Giavaresi G., Cavallo C. Autologous bone marrow concentrate in a sheep model of osteoarthritis: New perspectives for cartilage and meniscus repair. Tissue Eng Part C Methods. 2016;22:608–619. doi: 10.1089/ten.TEC.2016.0033. [DOI] [PubMed] [Google Scholar]
- 12.Longo U.G., Campi S., Romeo G., Spiezia F., Maffulli N., Denaro V. Biological strategies to enhance healing of the avascular area of the meniscus. Stem Cells Int. 2012;2012:528359. doi: 10.1155/2012/528359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chahla J., Serra Cruz R., Cram T.R., Dean C.S., LaPrade R.F. Inside-out meniscal repair: Medial and lateral approach. Arthrosc Tech. 2016;5:e163–e168. doi: 10.1016/j.eats.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ra H.J., Ha J.K., Jang S.H., Lee D.W., Kim J.G. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130. doi: 10.1007/s00167-012-2191-3. [DOI] [PubMed] [Google Scholar]
- 15.Henning C.E., Lynch M.A., Yearout K.M., Vequist S.W., Stallbaumer R.J., Decker K.A. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res. 1990;(252):64–72. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess for range of motion and evaluate for any concurrent ligament instability. A well-padded high-thigh tourniquet is subsequently placed on the right knee, which is positioned into a leg holder. The leg is prepared and draped in a sterile fashion. A standard anterolateral portal is created, and the anteromedial portal is created arthroscopically guided. A diagnostic arthroscopy is then performed. The menisci are probed and the tears are evaluated for repair. To perform an inside-out meniscal repair, a posteromedial approach is then performed as previously described by Chahla et al.13 An oblique vertical incision is performed from the adductor tubercle to the posterior aspect of the tibial plateau. An anatomic triangle composed of the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly, and the semimembranosus inferiorly is identified. A tablespoon is then placed in this interval to act as a retractor, protecting the popliteal vessels. Attention is then drawn to the meniscal repair. The tear is anatomically reduced and the sutures are placed perpendicularly to the lesion to restore its anatomic position. Double-loaded nonabsorbable No. 2.0 Fiberwire sutures are placed via a self-delivery gun fitted with a cannula into the meniscus. Vertical mattress sutures are placed for a strong construct. While the meniscal repair is being performed, 60 mL of blood is drawn from a peripheral site, in this case via subcutaneous veins on the dorsum of the hand. The blood is then placed in a basin. An assistant stirs the blood with a glass syringe for approximately 15 minutes to assure adequate clot formation. Once an adequate clot has formed on the distal aspect of the syringe, it is transferred to sterile surgical sponge. Temperate normal saline is then gently applied to help further condense the clot and to help improve its visibility arthroscopically. A scalpel and pickups are used to shape the clot to best fit the meniscal lesion. A grasper is then used to gently introduce the clot through the anterolateral portal. The meniscal sutures previously placed are loosened so that the clot could fit underneath the meniscus and have the best contact area with the lesion. After placing the fibrin clot, the knee is taken to 90° of flexion and the sutures are fastened down and then tied. The portals and the incision are then closed.