Abstract
Quadriceps tendinopathy in an increasingly recognized diagnosis can lead to quadriceps tendon rupture, especially in the older population. It can be caused by repeated micro trauma or also predisposed by systemic diseases such as diabetes mellitus and connective tissue disorders that can in turn lead to extensor mechanism deficits. Although a trial of conservative treatment is advocated, operative treatment should be performed in cases of persistent pain, extension deficit, or complete rupture of the tendon. The purpose of this Technical Note is to describe in detail a procedure for open repair of a quadriceps tendon, with significant degeneration due to quadriceps tendinopathy, using suture anchors and semitendinosus tendon allograft augmentation.
The extensor mechanism in the knee comprises a synergistic pair of muscle/tendon relations: the quadriceps muscles and tendon and the patellar tendon and its supporting retinaculum.1 Quadriceps tendon tendinopathy is less commonly seen than patellar tendinopathy,2 but has become increasingly common as older patients remain active at increasingly older ages. Quadriceps tendon tendinopathy can lead to quadriceps tendon rupture, especially in the older population.3, 4 Furthermore, systemic diseases such as diabetes mellitus and connective tissue disorders can lead to quadriceps tendon tendinopathy and, in turn, extensor mechanism deficits.3 The conservative treatment of these injuries is indicated if there is only a partial tear of the quadriceps tendon, with an intact extensor mechanism.3
However, when patients have persistent quadriceps tendon tendinopathy pain, pain with ambulation or have extension deficits, and have failed conservative treatment, a surgical approach is advocated. Although several techniques have been described including end-to-end suture, transosseous patellar tunnels or anchor fixation, and graft augmentation for complete quadriceps tendon tears, there is a paucity of literature on the treatment of high-grade partial quadriceps tendon tears. The purpose of this Technical Note is to describe in detail a procedure for open repair of a quadriceps tendon, with significant degeneration due to quadriceps tendinopathy, using suture anchors and semitendinosus tendon allograft augmentation.
Surgical Technique
A detailed accompanying video is presented with this Technical Note (Video 1). Pears and pitfalls and advantages and disadvantages of this procedure are listed in Tables 1 and 2, respectively.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Care should be taken to place the leg holder as proximal as possible. | Placement of the leg holder too distal can limit visualization of the entire quadriceps tendon. |
| The quadriceps tendon should be divided longitudinally overlying the area of the tendinopathy based on preoperative imaging. | The superficial tendon overlying the diseased tissue will often have a normal appearance. |
| The guide pin should be drilled from lateral to medial at approximately the junction of the superior one-third and inferior two-thirds of the patellar distance. | Care should be taken not to injure the medial patellofemoral ligament attaching to the medial aspect of the patella. |
| Place two double-loaded suture anchors at the superior pole of the patella to cerclage the allograft limbs and the adjacent retinaculum to secure the grafts to the superior pole of the patella. | Improper orientation of the suture anchors can lead to damage of the articular surface of the patella. |
| Before skin closure, the knee should be taken through gentle passive range of motion to 90° of flexion to ensure that postoperative rehabilitation can be started on day 1 postoperatively. | Avoid overconstraining with the incorporation of the allografts in the quadriceps tendon reconstruction. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| This technique allows for complete visualization of the degenerative, native quadriceps tendon. | The patient remains non-weight-bearing for 6 weeks, with an immobilizer. |
| Easily replicable technique. | Rate of subsequent rupture is still unknown. |
| Help to maintain proper function of the extensor mechanism. | Long-term outcomes, particularly in regard to the extensor mechanism strength, is still unknown. |
Preoperative Imaging
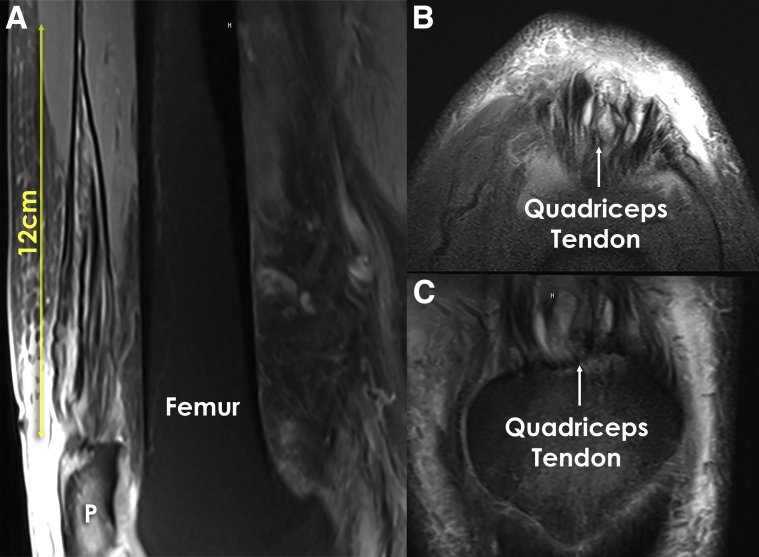
Preoperative magnetic resonance imaging is key not only to confirm the presence of this pathology (the diagnosis has to be performed clinically) but also to measure the extent of the pathology. This will allow us to plan the approach to gain access to the pathologic tendon. Also it is important to rule out concomitant pathology (Fig 1).
Fig 1.
Magnetic resonance imaging of the left knee showing quadriceps tendinopathy. (A) Sagittal view of the left knee showing tendinopathy. It is important to measure the length of the lesion to determine the length of the skin incision. (B) An axial view of the left knee showing changes in the quadriceps tendon. (C) Coronal view of the left quadriceps tendon attaching to the patella. The high signal changes consistent with tendinopathy can be seen. (P, patella.)
Patient Positioning and Anesthesia
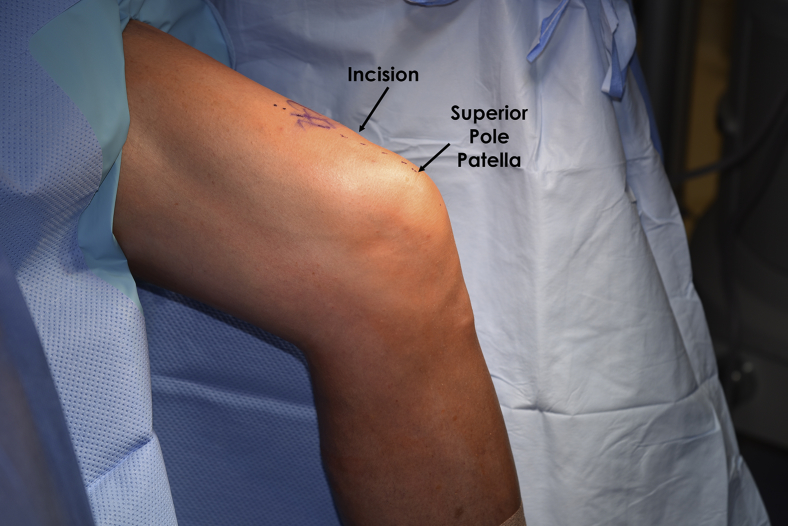
The patient is positioned supine on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to assess knee range of motion and evaluate for concurrent ligamentous laxity. A well-padded thigh tourniquet is placed on the operative extremity, which is then secured in a leg holder (Mizuho OSI, Union City, CA), whereas the contralateral knee is padded and placed into an abduction stirrup (Birkova Product LLC, Gothenburg, NE). The leg holder should be placed proximal enough to allow visualization of the entire quadriceps tendon during the approach for an augmented quadriceps reconstruction. The foot of the operating table is then lowered, allowing the surgeon to freely manipulate the knee (Fig 2).
Fig 2.
A picture of the left knee showing patient position with the knee hanging. This allows for easy access to the operation field, and the leg can be moved as desired during surgery. The skin incision site is marked corresponding with the length of the changes on the sagittal view on magnetic resonance imaging.
Operative Procedure
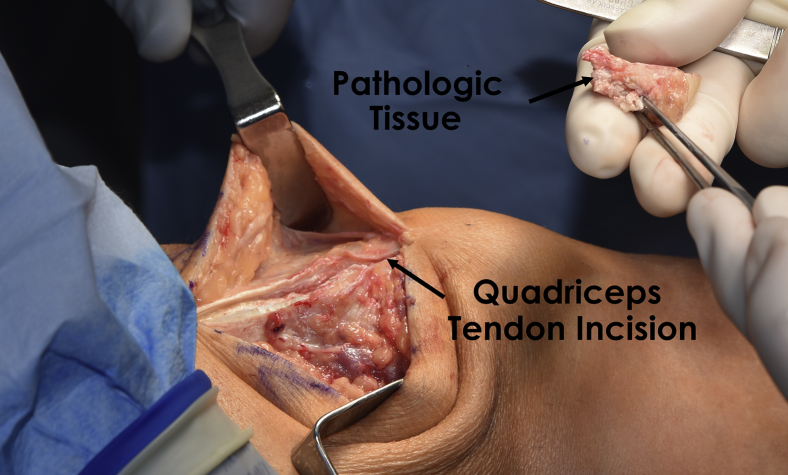
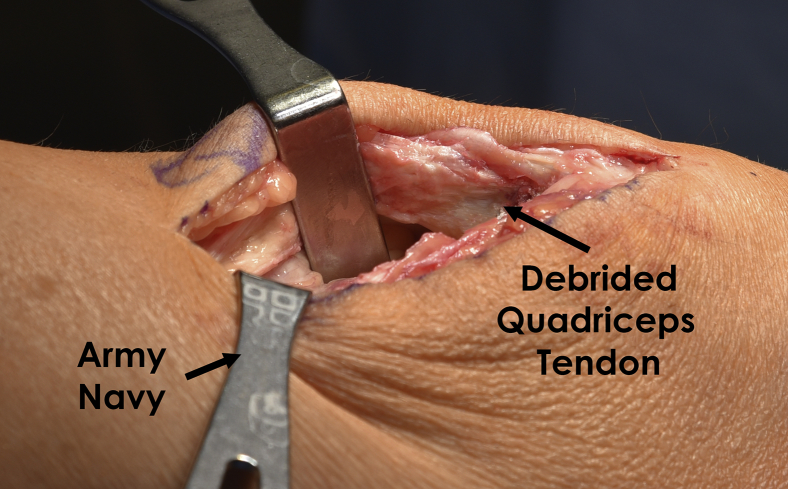
The operative leg is exsanguinated and a tourniquet is elevated. An anterior incision is made midline from the proximal pole of the patella extending as far proximally as necessary to address the extent of the quadriceps tendinopathy based on preoperative imaging. Dissection is carried down through the subcutaneous tissue sharply to the level of the fascia overlying the quadriceps tendon, and full-thickness flaps are elevated medially and laterally to expose the extent of the tendon. At this point, the quadriceps tendon is divided longitudinally overlying the area of the tendinopathy based on preoperative imaging. The superficial tendon overlying the diseased tissue will often have a normal appearance. The tendon is fully divided, and an arthrotomy is created. The area of tendinopathy is then exposed and subsequently debrided sharply with a knife and a rongeur. If present, any hypertrophic pathological tissue should be excised at this point (Fig 3).
Fig 3.
After a skin incision on the left knee, a sharp dissection through the subcutaneous tissue is performed. The quadriceps tendon is incised along the fibers and the pathologic tissue is excised.
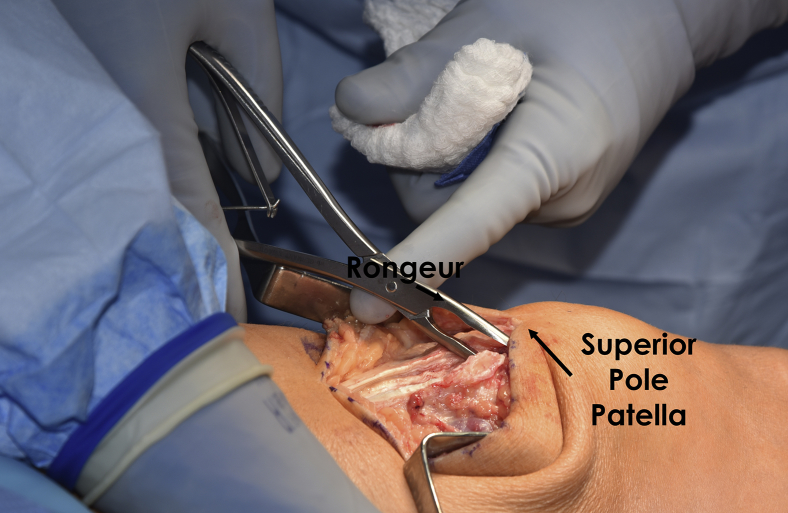
After excision of the diseased tissue, the exposed portion of the superior pole of the patella is debrided down to a bleeding bony bed to allow for healing after reconstruction (Figs 4 and 5).
Fig 4.
An intraoperative view showing removal of the pathologic tissue on the left proximal patella with a rongeur. It is important to remove the pathologic tissue and come to the bleeding surface on the proximal patella to stimulate healing.
Fig 5.
The quadriceps tendon on the left extremity showing the healthy tissue after debridement. Excising the pathologic tissue and getting to the healthy tissue is important for healing and symptom relief. The whole tendon thickness can be visualized and the margins are inspected.
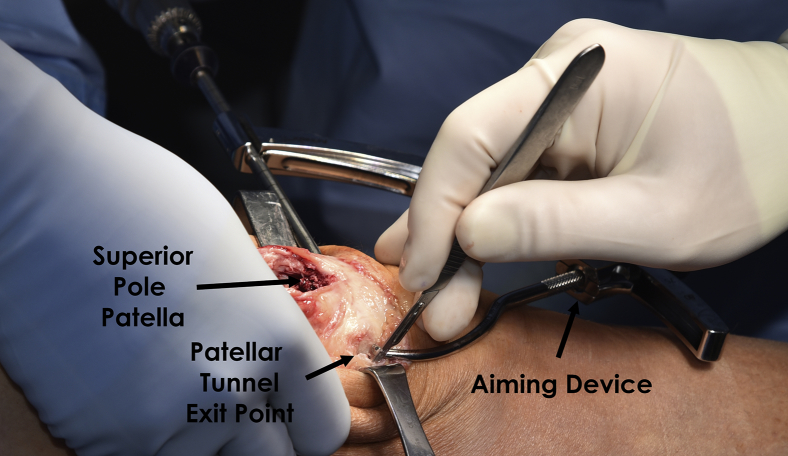
With all the diseased tissue removed, the quadriceps reconstruction is performed by creating a transverse tunnel through the proximal portion of the patella. With the use of an aiming device, a guide pin is drilled from lateral to medial at approximately the junction of the superior one-third and inferior two-thirds of the patellar distance taking care not to injure the medial patellofemoral ligament attaching to the medial aspect of the patella (Fig 6).
Fig 6.
An aiming device is used to ream a tunnel in the left proximal patella for the reconstruction graft. A beath pin is drilled first in the desired position and a reamer is then used to create a tunnel. Before reaming the tunnel, it is important to confirm the position of the pin to minimize the risk of fracture, and patellar articular cartilage violation. The position can easily be confirmed by visualizing the entry and exit points of the pin relative to the patellar thickness. If in doubt, a mini C-arm can be used to confirm position.
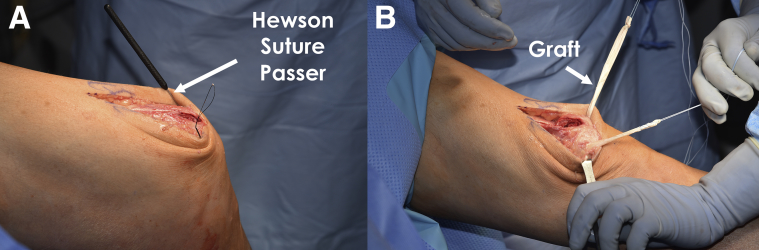
After guide pin placement, a 5-mm cannulated reamer is used to create a tunnel along the path of the guide pin for allograft passage. The allograft is then prepared. A semitendinosus graft is used and both ends of the graft are whipstitched with nonabsorable suture. With the aid of a Hewson suture passer, the allograft is subsequently passed through the transverse patellar tunnel (Fig 7).
Fig 7.
After tunnel reaming on the left patella, a Hewson suture passer is used to facilitate graft passage (A), and (B) the graft is pulled through the tunnel with a limb on each side. The free limbs of the graft will be used to repair the quadriceps tendon.
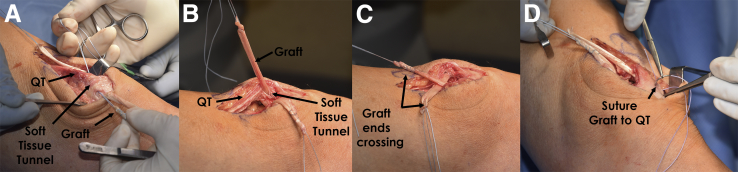
The graft is pulled through the tunnel to the extent that an equal length of graft limb is present on both the medial and lateral aspects of the patella. The ends of the graft are sewed to the periosteum at the exit points of the tunnel. Medial and lateral soft tissue tunnels are then created from each aperture of the patellar tunnel deep to the retinaculum and native quadriceps tendon to the superior pole of the patella. The medial and lateral limbs of the graft are then passed through these soft tissue tunnels such that both are passing through the defect in the debrided quadriceps tendon. A figure-of-8 stitch is placed through the retinaculum and through the allograft at the medial and lateral apertures of the patellar tunnel to fix the graft in place in the soft tissue tunnels (Fig 8).
Fig 8.
(A) To facilitate the repair with a graft, a soft tissue tunnel is created on both the medial and the lateral sides and the graft is passed through the tunnel with the aid of passing sutures. (B) The quadriceps (QT) tendon can be visualized and the length of the graft limbs on the medial and lateral sides is checked to ensure that they correspond to the length of the defect to be repaired. (C) The limbs of the graft are crossed over the proximal pole of the patella and (D) the graft is sutured to the native healthy quadriceps tendon using a No. 2 nonabsorbable suture.
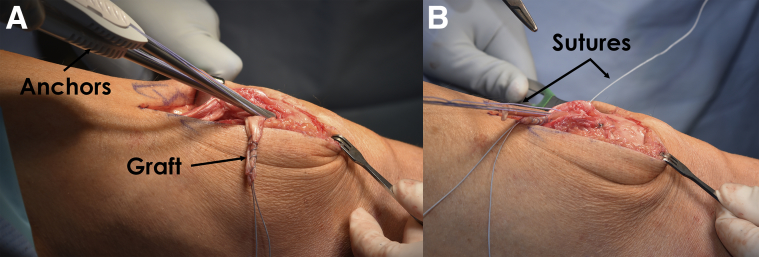
At this point, 2 double-loaded suture anchors are placed at the superior pole of the patella. Care is taken to orient the suture anchors such that they do not violate the articular surface of the patella. The sutures from each anchor are then used to cerclage the allograft limbs and the adjacent retinaculum to secure the grafts to the superior pole of the patella (Fig 9).
Fig 9.
Suture anchors are placed in the left proximal patella (A) and the graft is sutured to the left proximal patella (B). This ensures that the graft is also firmly fixed to the proximal patella before repairing the defect.
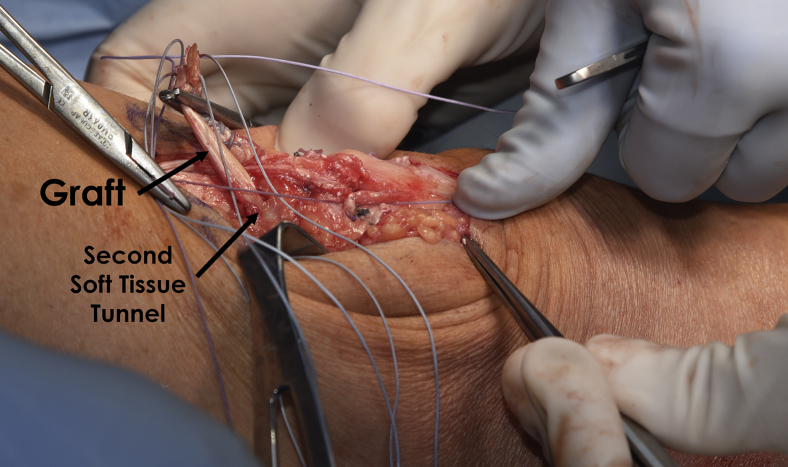
Finally, with the allograft limbs secured in the patellar tunnel, to the superior pole of the patella, and to the retinaculum, the limbs are crossed and tunneled through the quadriceps tendon more proximally at a second series of medial and lateral soft tissue tunnels (Fig 10).
Fig 10.
After suturing the grafts to the left proximal patella with suture anchors, soft tissue tunnels are created on the medial and lateral sides of the quadriceps tendon and the free limbs of the graft. At this point, the graft limb that was on the lateral side is on the medial side, and the one that exited the patella on the medial side is lateral. It is important to put tension on the graft to ensure that it is not caught in the soft tissue. The goal is to have the same tension as the native quadriceps tendon.
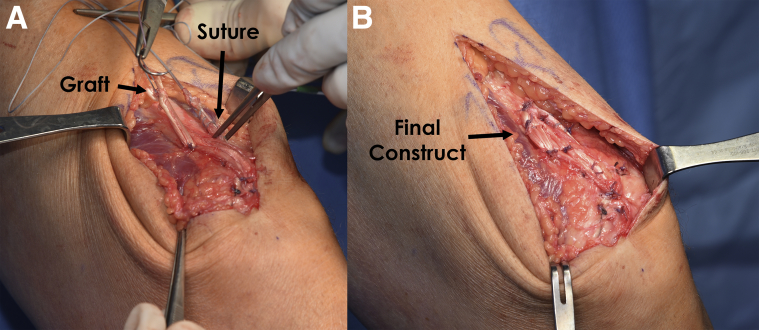
The grafts and the native quadriceps tendon are then secured with additional nonabsorbable suture as the arthrotomy and overlying native quadriceps tendon are closed securely with incorporation of the grafts (Fig 11). The knee is then taken through a gentle passive range of motion to 90° of flexion to ensure that there is no overconstraint with the incorporation of the allografts in the quadriceps tendon reconstruction.
Fig 11.
To repair the defect, the graft is sutured to the native quadriceps tendon using nonabsorbable sutures while maintaining adequate tension on the graft (A). After completing the repair, the quadriceps tendon is inspected and the tension checked (B). In addition, the knee is flexed and extended to check the tension on the repair during range on motion. It is important to check the tension on the repair to ensure that it is not too tight and to guide rehabilitation.
Postoperative Rehabilitation
After surgery, the patient uses a knee immobilizer and remains non-weight-bearing for 6 weeks. Passive range of motion is initiated on the first day postoperatively and is gradually progressed to full range of motion as tolerated, with the goal of attaining at least 90° of knee flexion by 2 weeks postoperatively. During the first 6 weeks, the patient's primary exercises are patella and quadriceps tendon mobilizations, active and passive knee range of motion, and quadriceps activation exercises. At 6 weeks, patients are permitted to initiate weight-bearing and to gradually wean off crutches and begin spinning on a stationary bike with no resistance. The patients are cleared to be off crutches once they can fully ambulate without a limp and demonstrate adequate muscular control of their quadriceps.
Once they are full weight-bearing, patients begin closed chain strengthening exercises with training periodization focused on developing muscular endurance first, followed by strength and power. Strengthening exercises with weight-bearing status begin at 8 weeks postoperatively, with limited leg press to 70° of knee flexion allowed at 10 weeks. Patients may begin running exercises at 6 months with the initiation of speed and agility drills at this time. A gradual return to play progression is initiated at 7 months postoperatively after completion of a functional sports examination. Return to sports or activity is allowed when normal strength, stability, and knee range of motion comparable to the contralateral side have been achieved (usually 6-9 months postoperatively).
Discussion
Chronic tendinopathy is a painful and disabling condition that can ultimately lead to sequelae such as tendon rupture. In this technique, we describe our approach to the treatment of chronic degenerative tendinopathy. The treatment of chronic tendinopathy is challenging due to a poor healing response. Bruns et al.5 helped explain why this is the case in a sheep model. They transected sheep Achilles tendons and allowed spontaneous healing and tested rupture force and found that it was only 56.7% of the native Achilles tendons.5 This helps also to explain why those undergoing chronic tendinopathy never regain full biomechanical function, and are more prone to traumatic rupture.
Tendinopathy is commonly treated with conservative means such as rest, ice, and physical therapy. An eccentric exercise program is a specific therapeutic protocol that has been shown to be effective in the treatment of tendinopathy.6 Corticosteroid injections have also been reported to decrease pain and inflammation associated with tendinopathy; however, they are also associated with an increased risk of tendon rupture.7 Aside from therapy, other current treatment modalities are largely experimental. New biologic healing agents are currently being evaluated for efficacy in treating tendinopathy. Early results and in vivo studies have showed some promise from platelet-rich plasma, interleukin-6, and scaffolds with stem cells in regard to improving tendinous healing.8, 9 However, more clinical studies are needed in the future to help elucidate the effects of biologic agents.
When conservative treat fails to improve symptoms or a complete rupture occurs, operative treatment should be performed. Repair can be achieved both arthroscopically and via an open procedure with good results.10, 11 Surgical repair techniques described include simple running sutures, suture anchor fixation, transosseous suture repair, and graft augmentation. All of these repair techniques have been reported to have good clinical results.12 Although results have been varied,13 more recent biomechanical studies have shown suture anchor fixation to be superior to transosseous fixation in regard to gapping with cyclic loading,14, 15, 16 and higher ultimate failure loads.14, 16 This technique has been shown to have positive clinical outcomes in regard to subjective scores, and return to sport.10, 17, 18
In conclusion, we recommend this augmented repair technique, using a semitendinosus allograft, to help strengthen the degenerative, native quadriceps tendon and decrease the risk of further complications such as complete quadriceps tendon rupture. This technique is easily replicable and one that can be used to treat this chronic condition, and help to maintain proper function of the extensor mechanism. Furthermore, given the success of quadriceps repair techniques in a similar manner, it stands to reason that these patients would have good subjective and objective outcomes. However, further follow-up studies are needed to determine the long-term outcomes of these patients, particularly in regard to their extensor mechanism strength, and their rate of subsequent rupture when compared with those treated with more traditional, conservative means.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives support from Arthrex, Ossur, Siemans, and Smith & Nephew; receives consultancy fees from Arthrex, Smith & Nephew, and Ossur; has grants/grants pending from Health East, Norway, and NIH R-13 grant for biologics; has patents (planned, pending, or issued) from Ossur and Smith & Nephew; and receives royalties from Arthrex, Ossur, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned supine on the operating table and the operative leg (left knee in this video) is exsanguinated and a tourniquet is elevated. An anterior incision is made midline from the proximal pole of the patella extending. Dissection is carried down through the subcutaneous tissue sharply to the level of the fascia overlying the quadriceps tendon. The quadriceps tendon is divided longitudinally and the area of tendinopathy is then exposed and subsequently debrided sharply with a knife and a rongeur. After excision of the diseased tissue, the exposed portion of the superior pole of the patella is debrided down to a bleeding bony bed to allow for healing after reconstruction. The quadriceps reconstruction is performed by creating a transverse tunnel through the proximal portion of the patella. With the use of an aiming device, a guide pin is drilled from lateral to medial proximally and a 5-mm cannulated reamer is used to create a tunnel along the path of the guide pin for allograft passage. With the aid of a Hewson suture passer, the allograft is subsequently passed through the transverse patellar tunnel. Medial and lateral soft tissue tunnels are then created from each aperture of the patellar tunnel deep to the retinaculum and native quadriceps tendon to the superior pole of the patella. The medial and lateral limbs of the graft are then passed through these soft tissue tunnels such that both are passing through the defect in the debrided quadriceps tendon. A figure-of-8 stitch is placed through the retinaculum and through the allograft at the medial and lateral apertures of the patellar tunnel to fix the graft in place in the soft tissue tunnels. Then, 2 double-loaded suture anchors are placed at the superior pole of the patella. The sutures from each anchor are then used to cerclage the allograft limbs and the adjacent retinaculum to secure the grafts to the superior pole of the patella. With the allograft limbs secured in the patellar tunnel, to the superior pole of the patella, and to the retinaculum, the limbs are crossed and tunneled through the quadriceps tendon more proximally at a second series of medial and lateral soft tissue tunnels. The grafts and the native quadriceps tendon are then secured with additional nonabsorable suture as the arthrotomy and overlying native quadriceps tendon are closed securely with incorporation of the grafts.
References
- 1.Tuong B., White J., Louis L., Cairns R., Andrews G., Forster B.B. Get a kick out of this: The spectrum of knee extensor mechanism injuries. Br J Sports Med. 2011;45:140–146. doi: 10.1136/bjsm.2010.076695. [DOI] [PubMed] [Google Scholar]
- 2.Pfirrmann C.W., Jost B., Pirkl C., Aitzetmuller G., Lajtai G. Quadriceps tendinosis and patellar tendinosis in professional beach volleyball players: Sonographic findings in correlation with clinical symptoms. Eur Radiol. 2008;18:1703–1709. doi: 10.1007/s00330-008-0926-9. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N., Papalia R., Torre G., Denaro V. Surgical treatment for failure of repair of patellar and quadriceps tendon rupture with ipsilateral hamstring tendon graft. Sports Med Arthrosc. 2017;25:51–55. doi: 10.1097/JSA.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 4.Ker R.F. The implications of the adaptable fatigue quality of tendons for their construction, repair and function. Comp Biochem Physiol A Mol Integr Physiol. 2002;133:987–1000. doi: 10.1016/s1095-6433(02)00171-x. [DOI] [PubMed] [Google Scholar]
- 5.Bruns J., Kampen J., Kahrs J., Plitz W. Achilles tendon rupture: Experimental results on spontaneous repair in a sheep-model. Knee Surg Sports Traumatol Arthrosc. 2000;8:364–369. doi: 10.1007/s001670000149. [DOI] [PubMed] [Google Scholar]
- 6.Murtaugh B., Ihm J.M. Eccentric training for the treatment of tendinopathies. Curr Sports Med Rep. 2013;12:175–182. doi: 10.1249/JSR.0b013e3182933761. [DOI] [PubMed] [Google Scholar]
- 7.Nepple J.J., Matava M.J. Soft tissue injections in the athlete. Sports Health. 2009;1:396–404. doi: 10.1177/1941738109343159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou Y., Wang J.H. PRP treatment efficacy for tendinopathy: A review of basic science studies. Biomed Res Int. 2016;2016:9103792. doi: 10.1155/2016/9103792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro E., Grande D., Drakos M. Biologics in Achilles tendon healing and repair: A review. Curr Rev Musculoskelet Med. 2015;8:9–17. doi: 10.1007/s12178-015-9257-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rehman H., Kovacs P. Quadriceps tendon repair using hamstring, prolene mesh and autologous conditioned plasma augmentation. A novel technique for repair of chronic quadriceps tendon rupture. Knee. 2015;22:664–668. doi: 10.1016/j.knee.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Saito H., Shimada Y., Yamamura T. Arthroscopic quadriceps tendon repair: Two case reports. Case Rep Orthop. 2015;2015:937581. doi: 10.1155/2015/937581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ciriello V., Gudipati S., Tosounidis T., Soucacos P.N., Giannoudis P.V. Clinical outcomes after repair of quadriceps tendon rupture: A systematic review. Injury. 2012;43:1931–1938. doi: 10.1016/j.injury.2012.08.044. [DOI] [PubMed] [Google Scholar]
- 13.Hart N.D., Wallace M.K., Scovell J.F., Krupp R.J., Cook C., Wyland D.J. Quadriceps tendon rupture: A biomechanical comparison of transosseous equivalent double-row suture anchor versus transosseous tunnel repair. J Knee Surg. 2012;25:335–339. doi: 10.1055/s-0031-1299656. [DOI] [PubMed] [Google Scholar]
- 14.Ettinger M., Dratzidis A., Hurschler C. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: a cadaveric study. Am J Sports Med. 2013;41:2540–2544. doi: 10.1177/0363546513500633. [DOI] [PubMed] [Google Scholar]
- 15.Sherman S.L., Copeland M.E., Milles J.L., Flood D.A., Pfeiffer F.M. Biomechanical evaluation of suture anchor versus transosseous tunnel quadriceps tendon repair techniques. Arthroscopy. 2016;32:1117–1124. doi: 10.1016/j.arthro.2015.11.038. [DOI] [PubMed] [Google Scholar]
- 16.Petri M., Dratzidis A., Brand S. Suture anchor repair yields better biomechanical properties than transosseous sutures in ruptured quadriceps tendons. Knee Surg Sports Traumatol Arthrosc. 2015;23:1039–1045. doi: 10.1007/s00167-014-2854-3. [DOI] [PubMed] [Google Scholar]
- 17.McCormick F., Nwachukwu B.U., Kim J., Martin S.D. Autologous hamstring tendon used for revision of quadriceps tendon tears. Orthopedics. 2013;36:e529–e532. doi: 10.3928/01477447-20130327-36. [DOI] [PubMed] [Google Scholar]
- 18.Gomes J.L., de Oliveira Alves J.A., Zimmermann J.M., Jr. Reconstruction of neglected patellar tendon ruptures using the quadriceps graft. Orthopedics. 2014;37:527–529. doi: 10.3928/01477447-20140728-04. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned supine on the operating table and the operative leg (left knee in this video) is exsanguinated and a tourniquet is elevated. An anterior incision is made midline from the proximal pole of the patella extending. Dissection is carried down through the subcutaneous tissue sharply to the level of the fascia overlying the quadriceps tendon. The quadriceps tendon is divided longitudinally and the area of tendinopathy is then exposed and subsequently debrided sharply with a knife and a rongeur. After excision of the diseased tissue, the exposed portion of the superior pole of the patella is debrided down to a bleeding bony bed to allow for healing after reconstruction. The quadriceps reconstruction is performed by creating a transverse tunnel through the proximal portion of the patella. With the use of an aiming device, a guide pin is drilled from lateral to medial proximally and a 5-mm cannulated reamer is used to create a tunnel along the path of the guide pin for allograft passage. With the aid of a Hewson suture passer, the allograft is subsequently passed through the transverse patellar tunnel. Medial and lateral soft tissue tunnels are then created from each aperture of the patellar tunnel deep to the retinaculum and native quadriceps tendon to the superior pole of the patella. The medial and lateral limbs of the graft are then passed through these soft tissue tunnels such that both are passing through the defect in the debrided quadriceps tendon. A figure-of-8 stitch is placed through the retinaculum and through the allograft at the medial and lateral apertures of the patellar tunnel to fix the graft in place in the soft tissue tunnels. Then, 2 double-loaded suture anchors are placed at the superior pole of the patella. The sutures from each anchor are then used to cerclage the allograft limbs and the adjacent retinaculum to secure the grafts to the superior pole of the patella. With the allograft limbs secured in the patellar tunnel, to the superior pole of the patella, and to the retinaculum, the limbs are crossed and tunneled through the quadriceps tendon more proximally at a second series of medial and lateral soft tissue tunnels. The grafts and the native quadriceps tendon are then secured with additional nonabsorable suture as the arthrotomy and overlying native quadriceps tendon are closed securely with incorporation of the grafts.