Abstract
Arthroscopic SLAP tear repair has become an increasingly used treatment for patients presenting with symptomatic SLAP tears after failed nonoperative management. Debridement, SLAP repair, and open or arthroscopic biceps tenodesis or tenotomy have been used for the treatment of SLAP tears. Various techniques for repair have been described, and furthermore, there is a high incidence of concomitant pathology of the shoulder. Repair remains an excellent option in isolated SLAP tears amenable to repair, with excellent outcomes in well-indicated patients. We present a method for repairing a SLAP tear using standard suture anchor fixation, anterior and posterior portals, and an accessory portal of Wilmington. Adequate labral repair can be achieved with this technique in patients with no concomitant biceps pathology. This report highlights this technique for SLAP repair in patients with isolated symptomatic SLAP tears that have failed conservative management.
The glenoid labrum is a fibrocartilaginous structure that functionally deepens the glenoid, resisting translation of the humeral head relative to the glenoid. In addition, it serves as an attachment site for the glenohumeral ligaments and long head of the biceps tendon. Andrews et al.1 were the first authors to describe superior labral pathology in throwing athletes. Snyder et al.2, 3 subsequently coined the term “superior labrum anterior posterior” (SLAP) and established the most widespread classification system (Table 1). Type II tears are of particular interest because they are characterized by labral and biceps anchor detachment from the glenoid rim. This is the most common morphology for tears, as well as a surgical indication for repair.2, 3
Table 1.
SLAP Tear Classification
| Type | Description |
|---|---|
| I | Fraying of superior labrum and biceps; both remain intact and attached to glenoid; patients may often be asymptomatic |
| II | Both superior labrum and biceps anchor are detached from glenoid; most common type |
| III | Bucket-handle tear of superior labrum; biceps anchor intact, however |
| IV | Bucket-handle tear of superior labrum that extends into fibers of biceps, often creating split appearance of tendon |
| V | Anteroinferior Bankart lesion that continues superiorly to include separation of biceps tendon |
| VI | Unstable flap tear of labrum with biceps tendon separation |
| VII | SLAP lesion that extends anteroinferiorly along labrum to below MGHL |
MGHL, middle glenohumeral ligament.
Most tears can initially be treated with nonoperative management including physical therapy and nonsteroidal anti-inflammatories. The criteria for operative management include painful and symptomatic SLAP tears that have failed to respond to conservative management, as well as acute traumatic tears in high-demand patients, such as competitive athletes. These tears must be examined arthroscopically before a decision can be made whether to repair, debride, or perform a biceps tenodesis or tenotomy. Although most patients enjoy good to excellent clinical outcomes, identifying isolated SLAP tears can be challenging because of the lack of specificity and sensitivity of diagnostic tests, as well as the high rate of concomitant shoulder pathology. Accordingly, various technological and technical advancements have sought to improve outcomes. Suture anchor fixation with simple or mattress sutures offers a straightforward approach to restoring the glenolabral relation in isolated SLAP tears.
We present a method for repairing a type II SLAP tear using a 2-anchor horizontal mattress suture technique. This method effectively re-creates the anatomic relation between the glenoid and the labrum with technical ease. This report highlights the technique for SLAP repair in an adult by using a suture anchor technique and strategic use of an accessory portal.
Surgical Technique
Setup
A step-by-step video of the procedure can be seen in Video 1. The patient is placed in the lateral decubitus position using a support such as a beanbag with all bony prominences well padded. The operative arm is placed in traction by use of a foam sleeve, and approximately 10 lb of traction is used to distract the joint. The arm is placed in 40° to 50° of abduction and approximately 15° of forward flexion. Bony landmarks, including the coracoid process, acromion, scapular spine, and clavicle, are drawn.
Portal Placement
First, we make a standard posterior viewing portal 2 cm inferior and medial to the posterolateral corner of the acromion. The arthroscope is inserted into the glenohumeral joint. An anterior working portal is made by an outside-in technique with an 18-gauge spinal needle approximately 1 to 2 cm inferior and medial to the anterolateral corner of the acromion through the rotator interval; care is taken to remain lateral and superior to the coracoid to avoid neurovascular injury.
Site Preparation
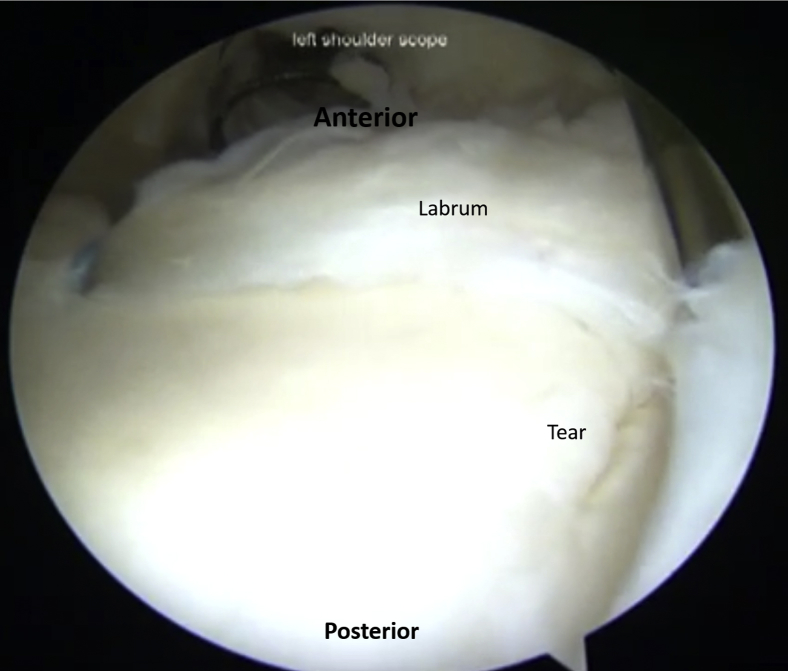
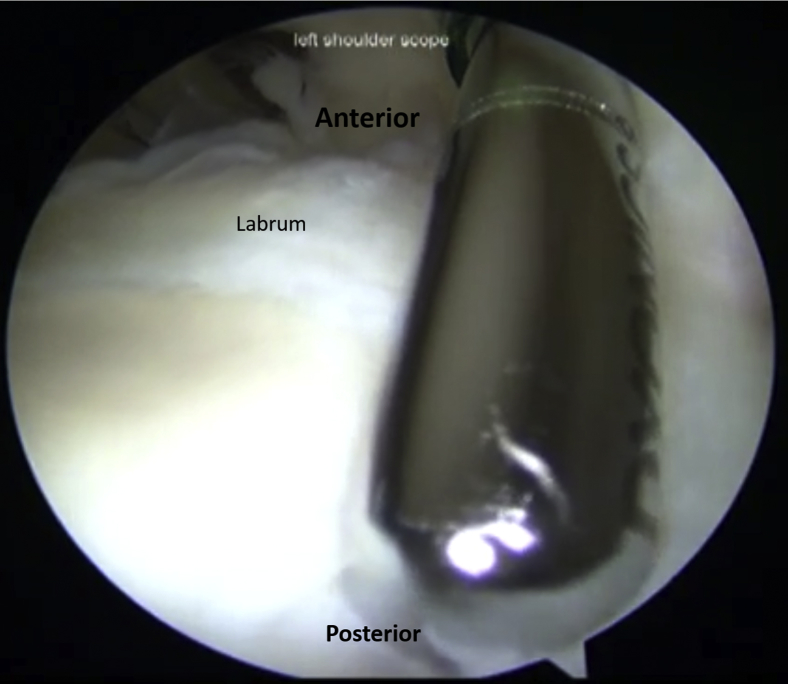
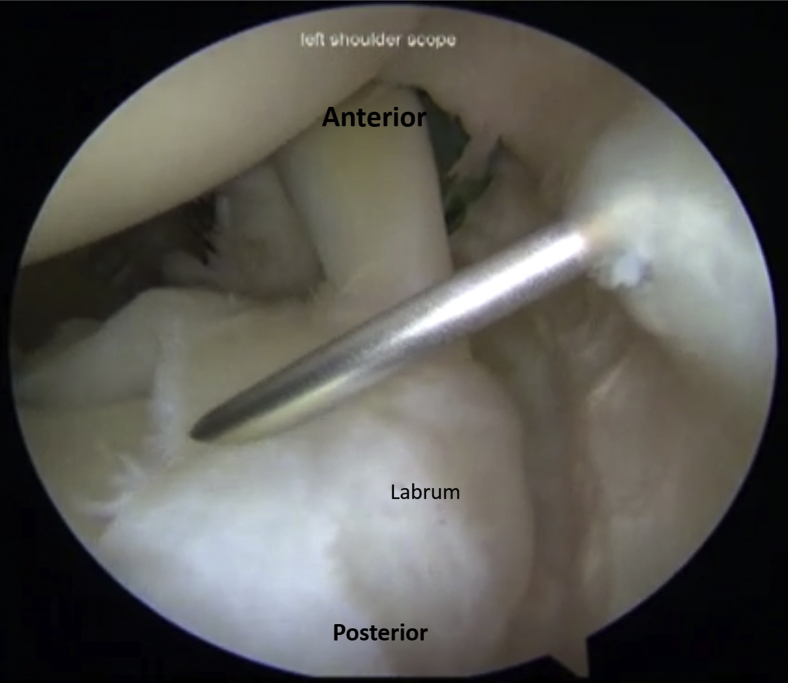
While viewing posteriorly, the surgeon uses an arthroscopic probe (Stryker, Kalamazoo, MI) to carefully inspect the superior labrum and a type II SLAP lesion is identified (Fig 1). An arthroscopic rasp and a shaver (Synthes, West Chester, PA) are used to prepare the glenoid rim for repair (Fig 2). An accessory portal of Wilmington is used, approximately 1 cm anterior and lateral to the posterolateral corner of the acromion (Fig 3). This is a trans-cuff portal through the musculotendinous portion of the rotator cuff to aid in anchor placement.
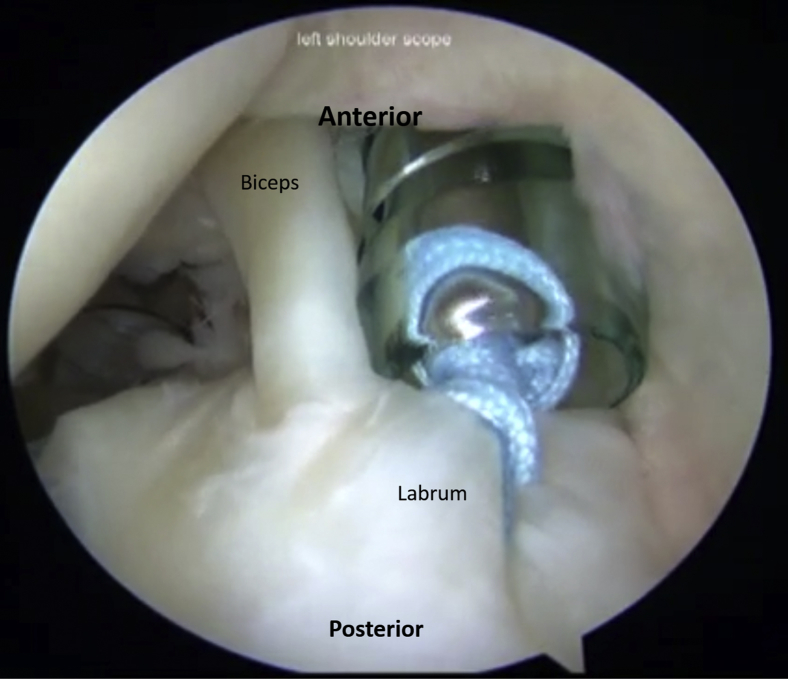
Fig 1.
With the patient in the lateral decubitus position, viewing from the posterior portal, the extent of the SLAP tear can be appreciated as it is probed. The tear in this case is considered a type II SLAP tear.
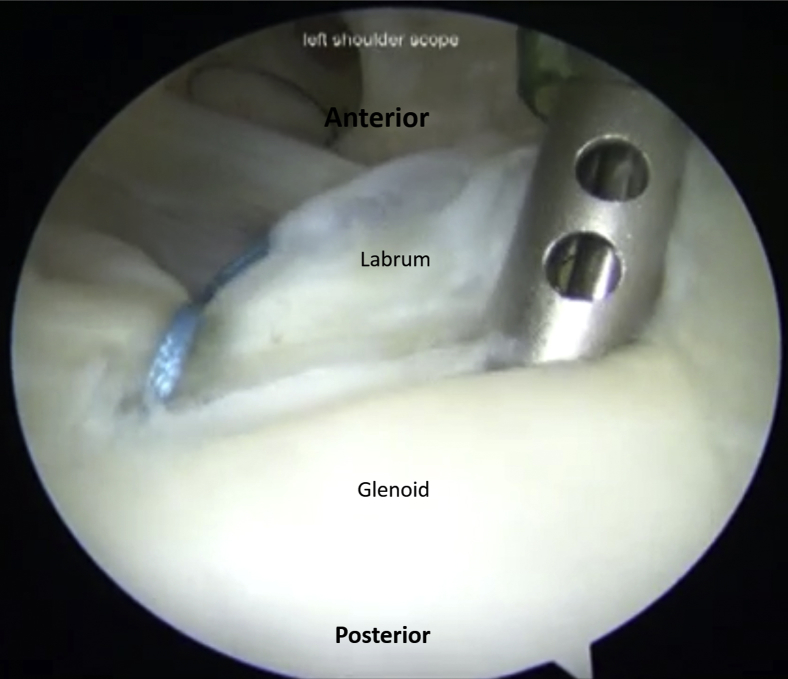
Fig 2.
With the patient in the lateral decubitus position, viewing from the posterior portal, an arthroscopic rasp and a shaver are used to prepare the glenoid rim for repair.
Fig 3.
With the patient in the lateral decubitus position, viewing from the posterior portal, an accessory portal of Wilmington is used, approximately 1 cm anterior and lateral to the posterolateral corner of the acromion. This is a trans-cuff portal through the musculotendinous portion of the rotator cuff to aid in anchor placement.
Anchor Placement
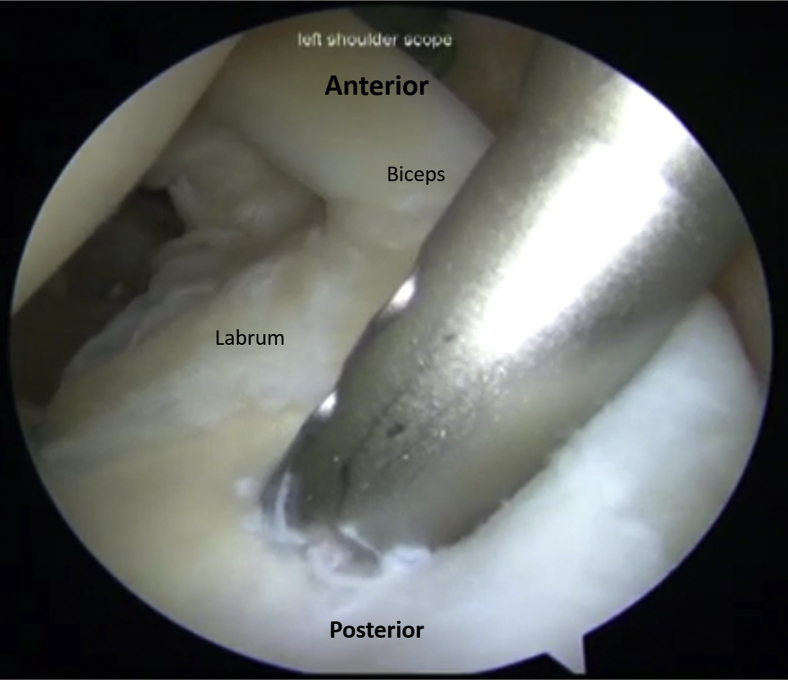
Next, the surgeon places an anchor (Arthrex, Naples, FL) adjacent to the detached labrum through the port of Wilmington at a 45° angle with respect to the posterior-superior glenoid rim after drilling through a drill sleeve or trocar (Fig 4). The anchor is then tested for stability before the sutures are passed through the anterior portal cannula that is placed superior to the biceps tendon. Each suture limb is shuttled through the labrum back through the port of Wilmington by use of a suture-passing device. Once the limbs are passed, they are brought through the anterior working portal and an arthroscopic knot is tied (Fig 5). Excess suture limbs are cut arthroscopically. Knots should be placed superiorly and medially, away from the articular surfaces. Alternatively, knotless devices can be used. In this case the decision is made to place a horizontal mattress suture to obtain repair of the labral tear. A second anchor is placed anterior to the biceps tendon in this case. An adjacent anterior portal can be placed to assist in passage of the suture for an anteriorly placed anchor (Fig 6, Fig 7, Fig 8). The biceps anchor is probed to verify stability after the labrum is repaired. Pearls and pitfalls can be found in Table 2.
Fig 4.
With the patient in the lateral decubitus position, viewing from the posterior portal, an anchor is placed adjacent to the detached labrum through the port of Wilmington at a 45° angle with respect to the posterior-superior glenoid rim after drilling through a drill sleeve or trocar. The anchor is then tested for stability before the sutures are passed through the anterior portal cannula that is placed superior to the biceps tendon.
Fig 5.
With the patient in the lateral decubitus position, viewing from the posterior portal, after limb passage, the limbs are brought through the anterior working portal and an arthroscopic knot is tied. Excess suture limbs are cut arthroscopically. Knots should be placed superiorly and medially, away from the articular surfaces.
Fig 6.
With the patient in the lateral decubitus position, viewing from the posterior portal, an adjacent anterior portal can be placed to assist in passage of the suture for an anteriorly placed anchor.
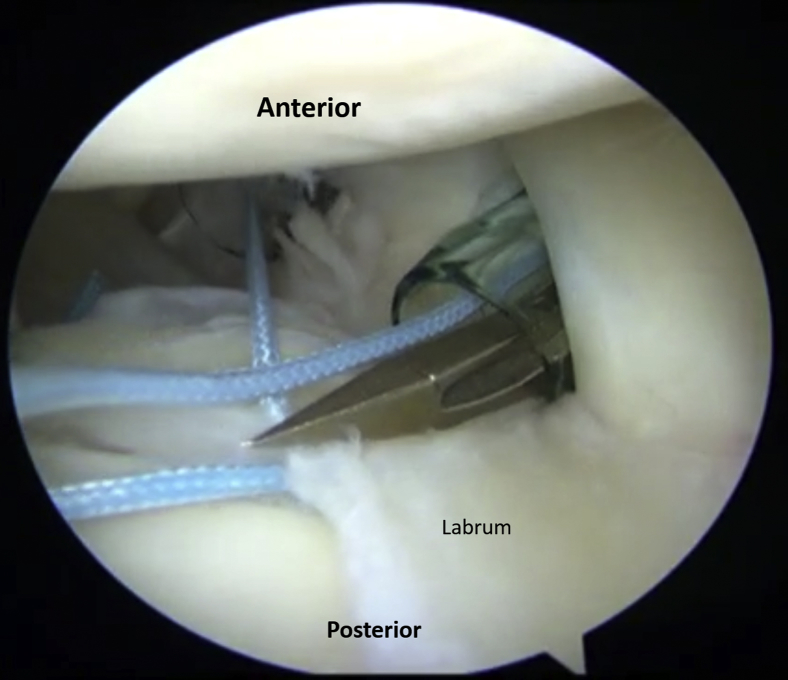
Fig 7.
With the patient in the lateral decubitus position, viewing from the posterior portal, a suture penetrator is used to pass the suture across the labrum. Suture limbs are then brought out through the same cannula.
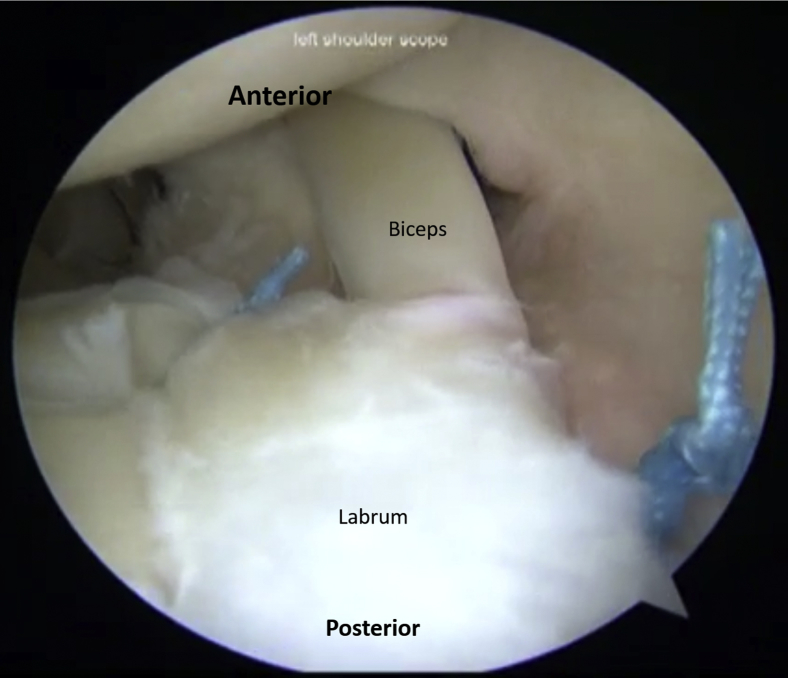
Fig 8.
With the patient in the lateral decubitus position, viewing from the posterior portal, the complete repair can be appreciated. The biceps anchor is probed to verify stability after the labrum is repaired.
Table 2.
Pearls and Pitfalls of Arthroscopic SLAP Repair
| Pearls | Pitfalls | Complications |
|---|---|---|
| The surgeon should assess for potential anatomic variants—chondral fraying at the site of insertion is indicative of an injury, whereas smooth cartilage represents an anatomic variant of a more medial attachment. | Failure to completely assess and consider anatomic variations can result in unnecessary procedures. | Adhesive capsulitis |
| Dynamic arthroscopy should be performed to assist with diagnosis. The peel-back test should be performed. A positive result is consistent with a labral tear. | Improperly addressing a normal anatomic variant may result in chronic pain and stiffness, especially an appreciable loss of external rotation. | Damage to articular cartilage from anchor placement |
| The surgeon should have a high index of suspicion for concomitant injuries while evaluating a patient with a SLAP tear. | Failure to address concomitant pathology may lead to suboptimal results. | Residual pain |
| When repairing a SLAP tear, the surgeon should only capture the labrum. | Capturing the capsule and rotator interval structures may result in constraining the joint and loss of motion. | Repair failure with aggressive rehabilitation |
| Use of the port of Wilmington or trans-cuff portal gives adequate access to the posterosuperior labrum, allowing appropriate anchor placement and limiting surgical time. | Persistent rotator cuff tears near portals | |
| For more anterior lesions, a suture penetrator can be used through the anterior cannula instead of a suture-shuttling device. | Non-return to previous activity levels | |
| Knots should be placed superiorly and medially, away from the articular surfaces. Knotless devices can also be used. |
Postoperative Rehabilitation
A standard postoperative rehabilitation protocol is used consisting of sling use for 4 weeks with active-assisted and active range of motion (ROM) as tolerated. From weeks 4 through 6, the sling is discontinued with emphasis on increased range of forward flexion as well as internal and external rotation. From weeks 6 through 12, ROM is progressed to full active ROM with light-weight strength training. After 12 weeks, strength training is advanced with a specific program.
Discussion
The incidence of operative management of SLAP tears has been increasing over the past 12 years.4, 5 As our understanding of SLAP tears with concomitant biceps or rotator cuff pathology improves, treatments have been tailored to appropriately treat the entire shoulder and not simply the superior labrum. This is evidenced by the recent analysis of the American Board of Orthopaedic Surgery database by Patterson et al.,6 reporting a 24.5% decrease in isolated SLAP repairs as a percentage of all SLAP repairs. Conversely, the incidence of biceps tenodesis and tenotomy procedures has increased.6, 7 Recent studies have shown a 72% to 88% incidence of concomitant pathology including rotator cuff tears, anterior instability, acromioclavicular joint arthritis, and paralabral cysts.8, 9
Establishing the diagnosis of a SLAP tear can be challenging. Physical examination findings and special tests have been shown to not be accurate for making the diagnosis.10 Advanced imaging including magnetic resonance arthrography has also recently been shown to have poor accuracy and predictive value in diagnosing SLAP lesions.11 Clinicians should maintain a high index of suspicion of concomitant pathology in seemingly isolated SLAP tears and be prepared to change the operative plan appropriately based on diagnostic arthroscopy findings.
Several techniques have been described for the treatment of isolated SLAP tears, including debridement, repair, and biceps tenodesis or tenotomy. Repair of the labrum has been shown to have good to excellent results, particularly for type II SLAP lesions.12, 13, 14, 15 Rates of return to sport and preinjury performance vary from 51% to 91%.9, 16, 17 The most commonly used technique involves surgical repair with bioabsorbable anchors loaded with nonabsorbable sutures.10 Biomechanical studies support both simple and mattress-type suture configurations.18, 19, 20 Anchor placement should be where the glenoid rim bone stock is greatest, at the articular margin at a 45° angle to the osseous surface, as shown by Lehtinen et al.21
SLAP repair failure rates vary in the literature from 0% to 30%.6, 7, 22 Most recently, Mollon et al.7 found a reoperation rate of 10.1% over a minimum 3-year follow-up period. Risk factors routinely cited for failure of SLAP repair include Workers' Compensation claims,22, 23 age, patient activity level, and patient expectations. Perhaps most important, patients should be counseled preoperatively with regard to prognosis, outcomes, and revision surgery rate.
The described technique has several advantages. A configuration using 1 posterior suture and 1 anterior suture has been shown to be biomechanically equivalent to 2 posterior simple sutures at resisting “peel-back” forces.19 Yet, it is easier to place 1 anterior anchor and 1 posterior anchor. In addition, our use of the accessory portal of Wilmington facilitates the placement of these anchors. Advantages and disadvantages are further explored in Table 3.
Table 3.
Advantages and Disadvantages of SLAP Repair
| Advantages | Disadvantages | |
|---|---|---|
| General SLAP repair | The procedure is relatively straightforward. | Diagnostic tests have poor sensitivity and specificity. |
| Good to excellent results with suture anchors have been reported in the literature. | The surgeon must confirm the tear arthroscopically before decisions can be made. | |
| Variable failure rates from 0%-30% have been reported. | ||
| Technique specific | Using a configuration with 1 posterior suture and 1 anterior suture is biomechanically equivalent to using 2 posterior simple sutures. | |
| The accessory portal of Wilmington facilitates anchor placement. |
We present a technique for repairing a type II SLAP tear using a transosseous anchor and mattress suture technique. This technique for treating type II SLAP tears simplifies what can be a technically demanding procedure to restore the glenolabral relation.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the lateral decubitus position and the operative arm is placed in 40 to 50 degrees of abduction and approximately 15 degrees of forward flexion. Bony landmarks are drawn including the coracoid process, acromion, scapular spine, and clavicle. First, a standard posterior viewing portal is made. The scope is then inserted into the glenohumeral joint. An anterior working portal is then made using an outside-in technique. An arthroscopic rasp and a shaver are used to prepare the glenoid rim for repair. An accessory portal of Wilmington is used. This is a trans-cuff portal through the musculotendinous portion of the rotator cuff to aid in anchor placement. Next, an anchor is placed adjacent to the detached labrum through the port of Wilmington after drilling through a drill sleeve/trocar. The anchor is then tested for stability before the sutures are passed. Each suture limb is the shuttled through the labrum back through the port of Wilmington. Once the limbs are passed, they are brought through the anterior working portal and an arthroscopic knot is tied. Knots should be placed superior and medial, away from the articular surfaces. A second anchor is placed anterior to the biceps tendon in this case. The biceps anchor is probed to verify stability after the labrum is repaired.
References
- 1.Andrews J.R., Carson W.G., Jr., McLeod W.D. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337–341. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 2.Snyder S.J., Banas M.P., Karzel R.P. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4:243–248. doi: 10.1016/s1058-2746(05)80015-1. [DOI] [PubMed] [Google Scholar]
- 3.Snyder S.J., Karzel R.P., Del Pizzo W., Ferkel R.D., Friedman M.J. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 4.Onyekwelu I., Khatib O., Zuckerman J.D., Rokito A.S., Kwon Y.W. The rising incidence of arthroscopic superior labrum anterior and posterior (SLAP) repairs. J Shoulder Elbow Surg. 2012;21:728–731. doi: 10.1016/j.jse.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Weber S.C., Martin D.F., Seiler J.G., III, Harrast J.J. Superior labrum anterior and posterior lesions of the shoulder: Incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40:1538–1543. doi: 10.1177/0363546512447785. [DOI] [PubMed] [Google Scholar]
- 6.Patterson B.M., Creighton R.A., Spang J.T., Roberson J.R., Kamath G.V. Surgical trends in the treatment of superior labrum anterior and posterior lesions of the shoulder: Analysis of data from the American Board of Orthopaedic Surgery certification examination database. Am J Sports Med. 2014;42:1904–1910. doi: 10.1177/0363546514534939. [DOI] [PubMed] [Google Scholar]
- 7.Mollon B., Mahure S.A., Ensor K.L., Zuckerman J.D., Kwon Y.W., Rokito A.S. Subsequent shoulder surgery after isolated arthroscopic SLAP repair. Arthroscopy. 2016;32:1954–1962.e1. doi: 10.1016/j.arthro.2016.01.053. [DOI] [PubMed] [Google Scholar]
- 8.Kim T.K., Queale W.S., Cosgarea A.J., McFarland E.G. Clinical features of the different types of SLAP lesions: An analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am. 2003;85:66–71. [PubMed] [Google Scholar]
- 9.Morgan C.D., Burkhart S.S., Palmeri M., Gillespie M. Type II SLAP lesions: Three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14:553–565. doi: 10.1016/s0749-8063(98)70049-0. [DOI] [PubMed] [Google Scholar]
- 10.Abrams G.D., Safran M.R. Diagnosis and management of superior labrum anterior posterior lesions in overhead athletes. Br J Sports Med. 2010;44:311–318. doi: 10.1136/bjsm.2009.070458. [DOI] [PubMed] [Google Scholar]
- 11.Sheridan K., Kreulen C., Kim S., Mak W., Lewis K., Marder R. Accuracy of magnetic resonance imaging to diagnose superior labrum anterior-posterior tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:2645–2650. doi: 10.1007/s00167-014-3109-z. [DOI] [PubMed] [Google Scholar]
- 12.Brockmeier S.F., Voos J.E., Williams R.J., III Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595–1603. doi: 10.2106/JBJS.H.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burkhart S.S., Morgan C.D., Kibler W.B. The disabled throwing shoulder: Spectrum of pathology. Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19:531–539. doi: 10.1053/jars.2003.50139. [DOI] [PubMed] [Google Scholar]
- 14.Nho S.J., Provencher M.T., Seroyer S.T., Romeo A.A. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–793. doi: 10.1016/j.arthro.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Ozbaydar M., Elhassan B., Warner J.J. The use of anchors in shoulder surgery: A shift from metallic to bioabsorbable anchors. Arthroscopy. 2007;23:1124–1126. doi: 10.1016/j.arthro.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Kim S.H., Ha K.I., Kim S.H., Choi H.J. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981–985. doi: 10.2106/00004623-200206000-00012. [DOI] [PubMed] [Google Scholar]
- 17.O'Brien S.J., Allen A.A., Coleman S.H., Drakos M.C. The trans-rotator cuff approach to SLAP lesions: Technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372–377. doi: 10.1053/jars.2002.30646. [DOI] [PubMed] [Google Scholar]
- 18.Domb B.G., Ehteshami J.R., Shindle M.K. Biomechanical comparison of 3 suture anchor configurations for repair of type II SLAP lesions. Arthroscopy. 2007;23:135–140. doi: 10.1016/j.arthro.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 19.Morgan R.J., Kuremsky M.A., Peindl R.D., Fleischli J.E. A biomechanical comparison of two suture anchor configurations for the repair of type II SLAP lesions subjected to a peel-back mechanism of failure. Arthroscopy. 2008;24:383–388. doi: 10.1016/j.arthro.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 20.Yoo J.C., Ahn J.H., Lee S.H. A biomechanical comparison of repair techniques in posterior type II superior labral anterior and posterior (SLAP) lesions. J Shoulder Elbow Surg. 2008;17:144–149. doi: 10.1016/j.jse.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 21.Lehtinen J.T., Tingart M.J., Apreleva M., Ticker J.B., Warner J.J. Anatomy of the superior glenoid rim. Repair of superior labral anterior to posterior tears. Am J Sports Med. 2003;31:257–260. doi: 10.1177/03635465030310021701. [DOI] [PubMed] [Google Scholar]
- 22.Erickson J., Lavery K., Monica J., Gatt C., Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: A systematic review. Am J Sports Med. 2015;43:1274–1282. doi: 10.1177/0363546514536874. [DOI] [PubMed] [Google Scholar]
- 23.Provencher M.T., McCormick F., Dewing C., McIntire S., Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: Outcomes and factors associated with success and failure. Am J Sports Med. 2013;41:880–886. doi: 10.1177/0363546513477363. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the lateral decubitus position and the operative arm is placed in 40 to 50 degrees of abduction and approximately 15 degrees of forward flexion. Bony landmarks are drawn including the coracoid process, acromion, scapular spine, and clavicle. First, a standard posterior viewing portal is made. The scope is then inserted into the glenohumeral joint. An anterior working portal is then made using an outside-in technique. An arthroscopic rasp and a shaver are used to prepare the glenoid rim for repair. An accessory portal of Wilmington is used. This is a trans-cuff portal through the musculotendinous portion of the rotator cuff to aid in anchor placement. Next, an anchor is placed adjacent to the detached labrum through the port of Wilmington after drilling through a drill sleeve/trocar. The anchor is then tested for stability before the sutures are passed. Each suture limb is the shuttled through the labrum back through the port of Wilmington. Once the limbs are passed, they are brought through the anterior working portal and an arthroscopic knot is tied. Knots should be placed superior and medial, away from the articular surfaces. A second anchor is placed anterior to the biceps tendon in this case. The biceps anchor is probed to verify stability after the labrum is repaired.