Abstract
Anterior cruciate ligament reconstruction is one of the most commonly performed procedures in orthopaedics, with more than 125,000 performed in the United States per year. There are several reconstruction graft choices that can be used to reconstruct the native anterior cruciate ligament, with autograft hamstring tendons being one of the most commonly used. Preparation of a hamstring autograft varies depending on patient characteristics and physician preference. The purpose of this Technical Note is to describe in detail different variants of hamstring graft preparation techniques that are commonly used in practice.
Anterior cruciate ligament (ACL) injuries are one of the most common injuries in orthopaedics, especially in the young and athletic populations. Given the importance of its biomechanical function, ACL tears are commonly addressed surgically.1 Although there is consensus among surgeons that most ACL injuries require surgical resolution, there is still controversy surrounding different technical aspects of the reconstruction, such as graft choice.
Reconstruction autograft versus allograft, specific graft type (hamstring, patellar tendon, quadriceps), and graft preparation all vary according to surgeons' preferences, patients' needs/expectations, or grafts' characteristics.2, 3, 4 Although some of these considerations have been addressed in previously published outcome studies, such as autograft versus allograft, with numerous studies showing the superiority of an autograft in terms of patient-reported outcomes, decreased failure rate, and return to sport,5, 6, 7, 8 other aspects of the graft election remain unclear. Graft types, particularly hamstring (Table 1) and patellar tendon grafts, have shown good results, and there is no strong evidence demonstrating the superiority of either graft type.9, 10
Table 1.
Advantages and Disadvantages of Hamstring Autografts
| Advantages | Disadvantages |
|---|---|
|
|
ACL, anterior cruciate ligament; BTB, bone–patellar tendon–bone; MRI, magnetic resonance imaging.
Another variable, which has been reported to have an effect on graft strength and longevity, is graft size. According to Conte et al.,11 grafts less than 8 mm in diameter are a risk factor for poor patient outcomes, with an increase in failure rates, particularly in patients younger than 20 years.12 This is of particular importance in hamstring autograft procedures because hamstring tendons, specifically in younger female population, tend to be insufficient and more prone to failure.13 Therefore, to address this issue, techniques that involve increasing hamstring graft thickness by folding the graft on top of itself have been developed.14, 15 The purpose of this Technical Note is to describe in detail different variants of hamstring graft preparation techniques that are commonly used in practice.
Surgical Technique
Graft Harvest
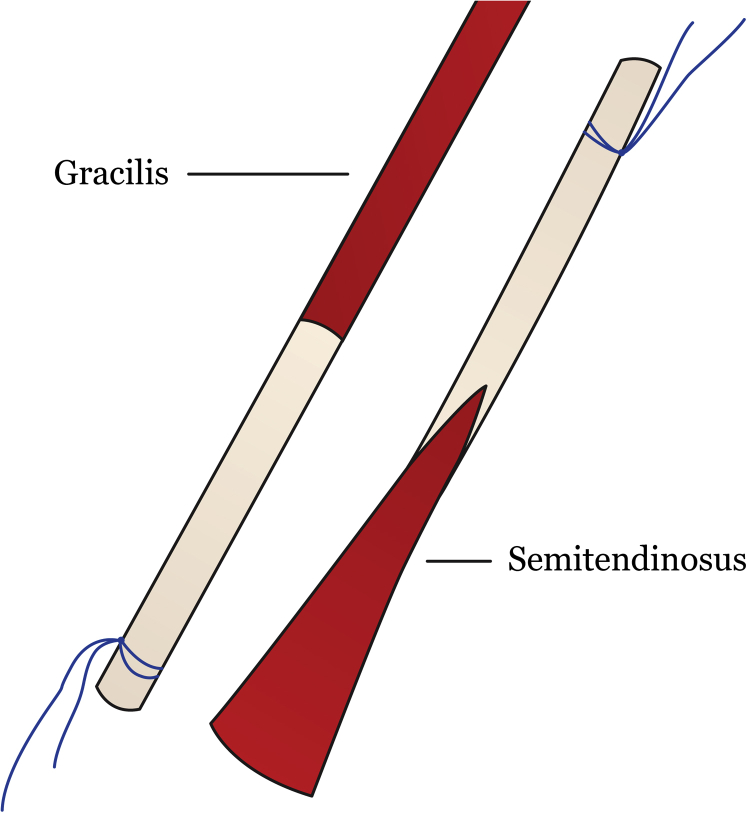
For hamstring tendon autografts, the semitendinosus (ST) and/or gracilis (GC) can be harvested from the surgical side or the contralateral side. A vertical anteromedial incision at the level of the tibial tubercle is used to expose the sartorius fascia and pes anserine bursa, which covers the hamstring tendons. An incision in the sartorial fascia allows the exposure of the tendons. The tendons are identified and then placed individually through an open tendon stripper and released from its muscular attachment proximally while flexing the knee and advancing the stripper in a proximal direction. Each tendon is identified according to the muscle belly pattern and harvest position: GC is above and proximal to ST and has a rounded-shaped muscular belly; the ST is below and distal to GC and has a U-shaped muscular belly (Fig 1).
Fig 1.
Identification of the gracilis and semitendinosus tendon according to muscular belly shape and anatomic location. The gracilis tendon is above and proximal to semitendinosus and has a rounded-shaped muscular belly, whereas the semitendinosus is below and distal to the gracilis and has a U-shaped muscular belly.
Graft Preparation
The graft preparation and configuration is easily done in a graft preparation station (Arthrex, Naples, FL) (Video 1). The graft is loaded in a cortical suspensory adjustable-length device (ENDOBUTTON CL ULTRA, Smith & Nephew, Andover, MA), and high-strength sutures are used (FiberWire No. 2 Curved Needle, Arthrex; FiberLoop No. 2 Braided Straight Needle, Arthrex).
Removal of excess muscular tissue from each tendon graft is performed, and unstable portions of the tendon are removed. If ST and GC tendons are harvested, they should be twisted in a reverse orientation in order that the proximal end of the ST is adjacent to the distal end of the GC graft and vice versa.18
The graft(s) are evaluated in a graft preparation station on the back table, and measurements of length of each harvested tendon(s) are made to determine which graft preparation is more suitable for that specific ACL reconstruction. The graft configuration is then simulated (folded) to determine the appropriate graft length and diameter.
Other pearls and pitfalls should be taken into account in the surgical graft preparation technique for obtaining an optimal hamstring graft (Table 2).
Table 2.
Pearls and Pitfalls of the Hamstring Graft Technique for ACL Reconstruction
| Pearls | Pitfalls |
|---|---|
|
|
ACL, anterior cruciate ligament; BTB, bone–patellar tendon–bone.
Graft Configuration
Two-Strand Graft Preparation
With One Tendon (Either GC or ST)
The tendon is loaded in a suspensory device with the middle portion of the tendon in the clamp (Fig 2; Video 1). The 2 free ends of the graft are folded on top of one another, and are stitched together with a nonabsorbable suture trying to equalize both the ends of the graft. The graft is whipstiched in the distal site of the graft.
Fig 2.
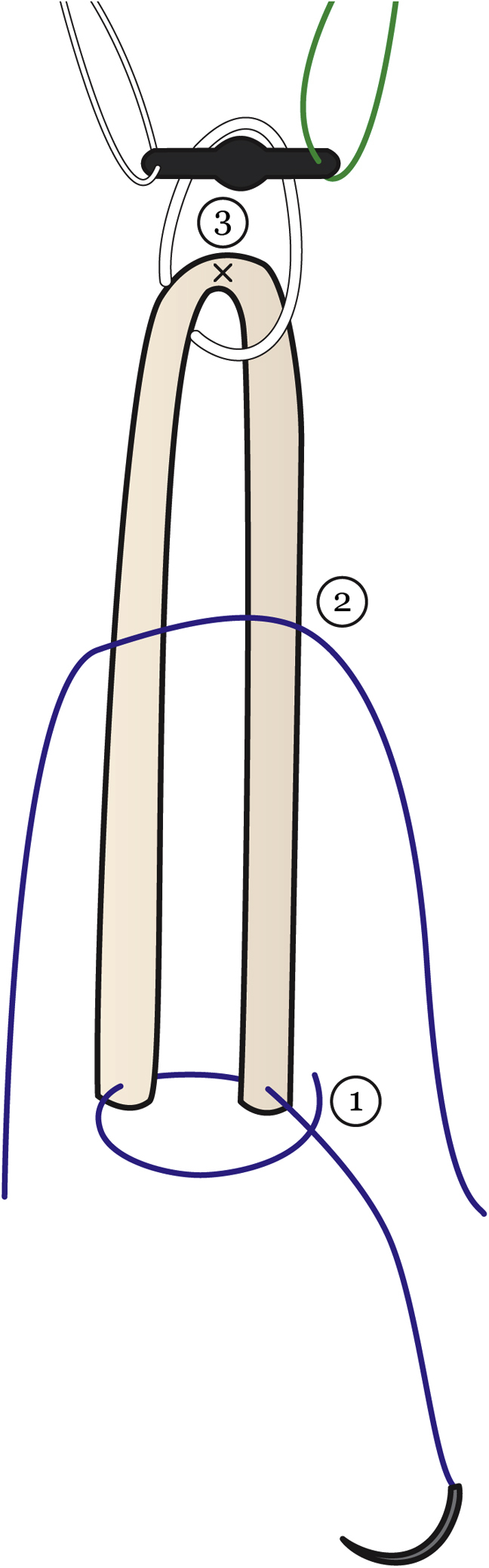
Two-strand and 4-strand graft preparation with 1 tendon. (1) Both ends of the tendon are sutured together. In 4-strand graft preparation, (2) a nonabsorbable suture is passed in the middle and the tendons are folded. (3) The needle is passed through the proximal part, grabbing and tensioning the distal part with the nonabsorbable suture.
Three-Strand Graft Preparation (If the Tendon Is Very Thick but Very Short)
With One Tendon (Either GC or ST)
The tendon is folded to effectively divide the tendon into 3 equal parts (Fig 3; Video 1). The ends of each fold are marked. One-third of the tendon is loaded in a suspensory device according to the marks. A stitch in each end of the tendon is made with a nonabsorbable suture. The needle is then passed through the 2 other strands of the graft. The same procedure is then repeated at the other end.
Fig 3.
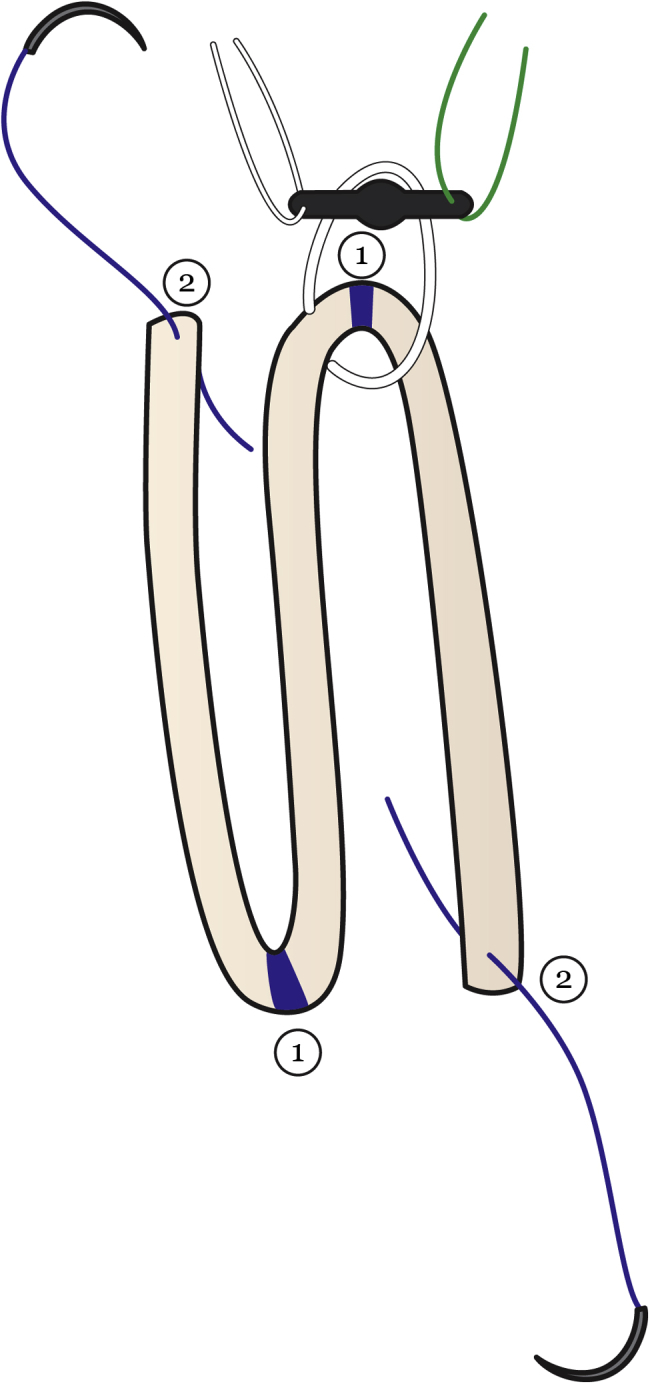
Three-strand graft preparation with 1 tendon. The tendon is divided into 3 equal parts. (1) The ends of each fold are marked. One-third of the tendon is loaded in a suspensory device according to the marks. (2) A stich in each end of the tendon is made with a nonabsorbable suture. The needle is then passed through the 2 other strands of the graft. The same procedure is then repeated at the other end.
Four-Strand Graft Preparation
With One Tendon (Either GC or ST)
Either a GC or a ST tendon is loaded in a suspensory device (Fig 2; Video 1). The free ends of the graft are whipstiched together with a nonabsorbable suture. A nonabsorbable suture is passed in the middle, and the tendons are folded. The needle is passed through the proximal part, grabbing and tensioning the distal part with the nonabsorbable suture. Sutures are reinforced in the distal site of the graft.
This technique can also be used with 2 suspensory devices for an all-inside ACL reconstruction.16
With Two Tendons (GC and ST or a ST Cut in Half)
Both tendons are loaded in a suspensory device in a reverse orientation. A nonabsorbable suture is passed twice around the 4 free ends of the graft. The graft is whipstiched distally with a nonabsorbable suture.
Five-Strand Graft Preparation (If the Tendon Is Thin With Triple Bundle)
With One Tendon (Either GC or ST—Triple Bundle) and Another Tendon (GC or a ST—Double Bundle)
Three-strand graft preparation is done with 1 tendon. The other tendon is loaded in a suspensory device (in the middle) (Video 1). A stich is made in the end of the 5 strands. The 5-strand graft is then whipstiched from proximal to its distal end.
Six-Strand Graft Preparation (If the Tendon Is Thin With Quadruple Bundle)
With Two Tendons (GC and ST)
Each tendon is divided into 3 equal parts (Fig 4). The ends of each fold are marked. A stich is placed into both ends of the tendons with a nonabsorbable suture. One-third of each tendon is loaded in a suspensory device according to the marks. The needle of each end of both strands is then passed through the other 2 strands. The same procedure is repeated for the other end of the tendons.
Fig 4.
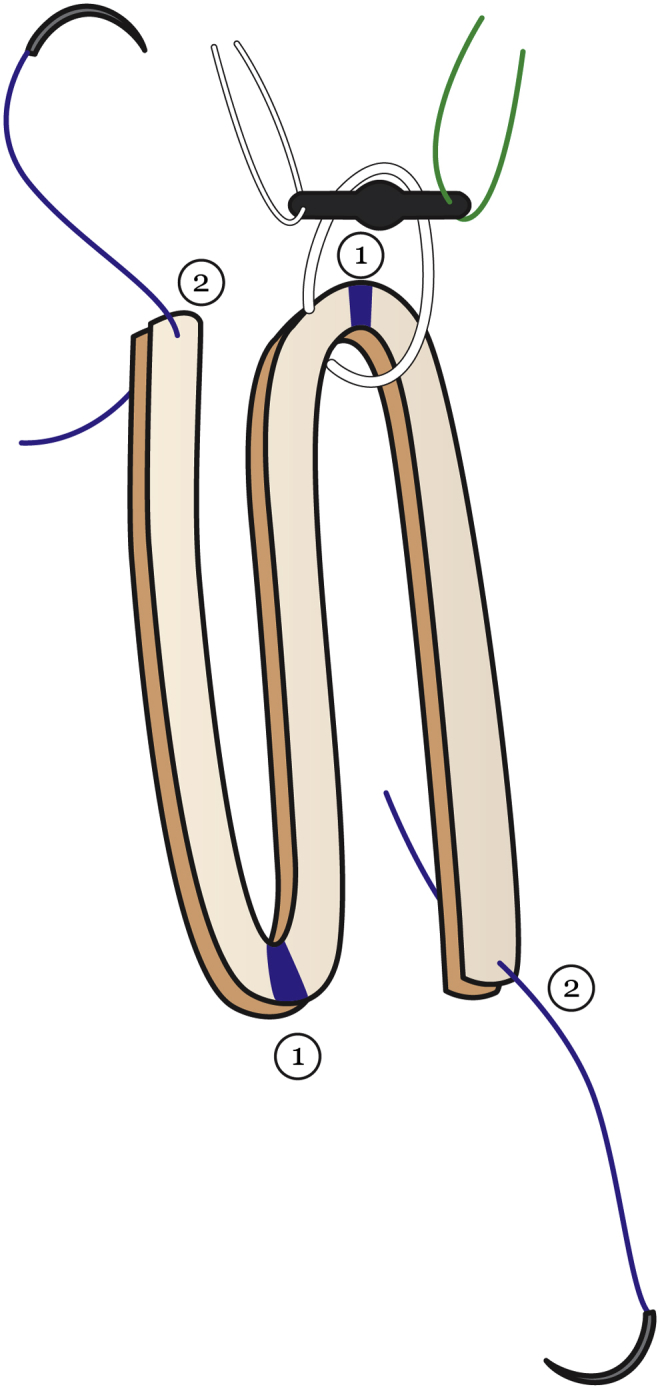
Six-strand graft preparation with 2 tendons. The tendons are divided into 3 equal parts. (1) The ends of each fold are marked. One-third of each tendon is loaded in a suspensory device according to the marks. (2) A stitch in each end of both tendons is made with a nonabsorbable suture. The needle is then passed through the 4 other strands of the graft. The same procedure is then repeated at the other end.
Another way for 6-strand graft preparation is to use a 4-strand graft with 1 tendon and load another tendon as a 2-strand graft or to use 2 suspensory devices for an all-inside ACL reconstruction.17
Eight-Strand Graft Preparation
With Two Tendons (GC and ST)
Both tendons are loaded in a suspensory device. The free ends of the grafts are whipstiched together with a nonabsorbable suture (Fig 5). A nonabsorbable suture is passed in the middle and the tendons are folded. The needle is passed through the proximal part, grabbing and tensioning the distal part with the nonabsorbable suture. Sutures are reinforced in the distal site of the graft.
Fig 5.
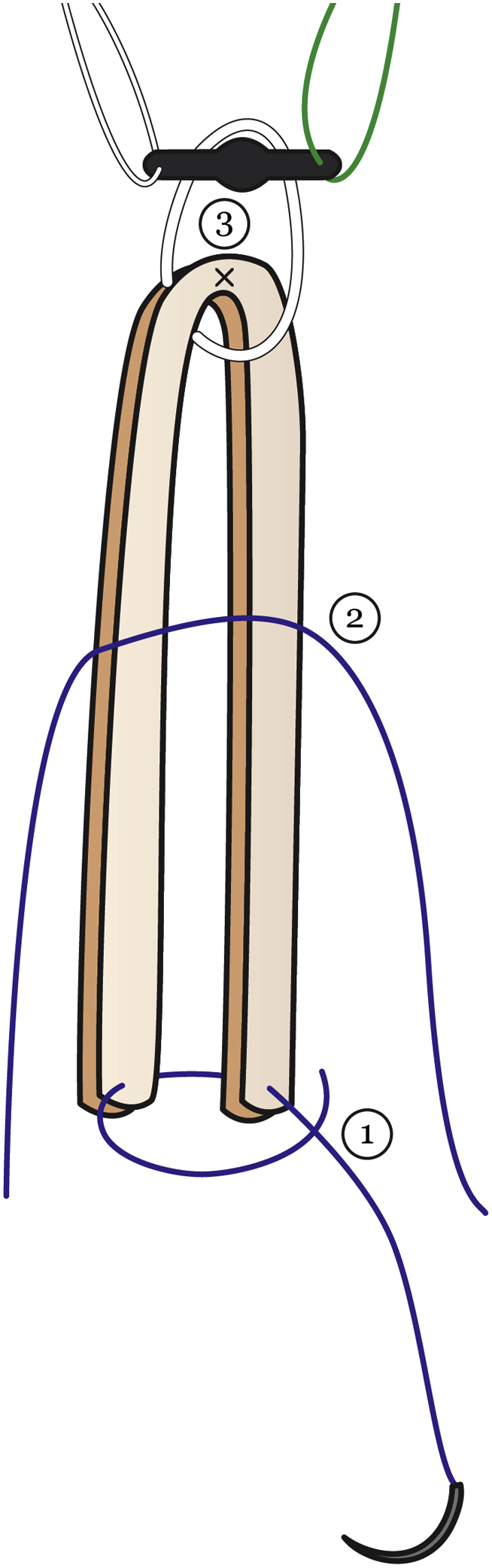
Eight-strand graft preparation with 2 tendons. (1) Both ends of both tendons are sutured together. (2) A nonabsorbable suture is passed in the middle and the tendons are folded. (3) The needle is passed through the proximal part of both tendons, grabbing and tensioning the distal part with the nonabsorbable suture.
This technique can also be performed with 2 suspensory devices for an all-inside ACL reconstruction.18
Discussion
Our Technical Note describes commonly used graft preparation techniques available for hamstring autografts. There are quite a few options for graft type, which have been shown to have good subjective and objective outcomes.
Although numerous studies have shown the superiority of an autograft compared with an allograft in regard to subjective outcomes, graft failure rate, and return to sport, there are far fewer studies comparing types of autografts.3, 5, 6, 7, 8 Comparative studies between a patellar tendon and a hamstring tendon that have been performed to date have failed to show clinically significant differences in failure rate, subjective outcome scores, or return to sport.19, 20, 21 Sajovic et al.22 in a prospective study on 64 patients (32 patellar tendon, 32 hamstring) with minimum 11 years of follow-up showed no difference in the failure rate or subjective outcomes. However, they did show an increased prevalence of pivot shift and signs of osteoarthritis in the patellar tendon group.22 Because numerous studies have shown equivalence with shorter term outcomes such as return to sport and graft failure, longer follow-up studies are needed for comparing rates of osteoarthritis and long-term outcome scores.
Numerous different hamstring preparation techniques have been described in the literature.9, 23 There is, however, a scarcity of studies looking at superiority within hamstring graft types. Conte et al.11 showed that graft size, specifically the hamstring autograft (>8 mm in diameter), led to significantly improved results. Furthering the argument that larger graft size leads to improved outcomes, the study by Dai et al.9 showed that a 6-strand hamstring tendon autograft had decreased pivot shift, less graft failure rate, and improved KT-1000 outcomes when compared with a patellar tendon autograft. Although studies like these help to make the argument that larger graft size with more strands may lead to increased anteroposterior stability, they do not say anything regarding long-term outcomes, and rates of osteoarthritis. It is possible that a larger graft could overcrowd intra-articular spaces changing joint kinematics, which could increase rates of arthrofibrosis or osteoarthritis.
In conclusion, we recommend the use of any of the described hamstring graft preparation techniques as long as they meet minimum diameter requirements, and are also appropriately fitted for the patient. Further biomechanical studies as well as long-term outcome studies should be performed comparing different hamstring autograft techniques. These studies should also address how different sized grafts affect patients of different ages and stature.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives support from Arthrex, Ossur, Siemans, and Smith & Nephew; receives consultancy fees from Arthrex, Smith & Nephew, and Ossur; has grants/grants pending from Health East, Norway; NIH R-13 grant for biologics; has patents (planned, pending, or issued) from Ossur and Smith & Nephew; and receives royalties from Arthrex, Ossur, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Hamstring graft preparation techniques for ACL reconstruction. First, we show the 2-strand technique with 1 tendon. The tendon is loaded into a suspensory device. The 2 free ends of the graft are stitched together with a nonabsorbable suture to create equal lengths of each half. The graft is then whipstiched with Fiberloop at the end to reinforce it. Then, we show the 4-strand technique with 1 tendon. Once the 2 free ends of the graft are stitched together, a suture is passed in the middle and the tendons are folded. The needle is passed through the proximal part of the graft stump, grabbing and tensioning the distal part with a nonabsorbable suture. The 4-strand graft is then whipstiched with Fiberloop from proximal to distal. Next, we show the 3-strand technique with 1 tendon. The tendon is folded into 3 equal parts, and the junction at each fold is marked. The tendon is loaded in a suspensory device at one of the marks. A stitch at each end of the tendon is made with a nonabsorbable suture leaving a tail. The needle is then passed through the other 2 strands of the graft. The same procedure is then repeated at the other end. Then, we show the 5-strand technique with 2 tendons. A 3-strand graft is prepared with 1 tendon as showed previously. The other tendon is loaded in the same suspensory device, alongside it. A needle is passed at the end of the 3-strand graft, through all 5 strands. The 5-strand graft is then whipstiched with Fiberloop from proximal to distal. Finally, we show the 4-strand technique with 2 tendons. Both tendons are loaded in a suspensory device with a reverse orientation. A nonabsorbable suture is passed twice around the 4 free ends of the graft. The graft is whipstiched with a continuous nonabsorbable suture from distal to proximal and then from proximal to distal to reinforce the distal site of the graft.
References
- 1.Saltzman B.M., Cvetanovich G.L., Nwachukwu B.U., Mall N.A., Bush-Joseph C.A., Bach B.R., Jr. Economic analyses in anterior cruciate ligament reconstruction: A qualitative and systematic review. Am J Sports Med. 2016;44:1329–1335. doi: 10.1177/0363546515581470. [DOI] [PubMed] [Google Scholar]
- 2.Duchman K.R., Lynch T.S., Spindler K.P. Graft selection in anterior cruciate ligament surgery: Who gets what and why? Clin Sports Med. 2017;36:25–33. doi: 10.1016/j.csm.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Koh H.S., In Y., Kong C.G., Won H.Y., Kim K.H., Lee J.H. Factors affecting patients' graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg. 2010;2:69–75. doi: 10.4055/cios.2010.2.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Struewer J., Ziring E., Oberkircher L., Schuttler K.F., Efe T. Isolated anterior cruciate ligament reconstruction in patients aged fifty years: Comparison of hamstring graft versus bone-patellar tendon-bone graft. Int Orthop. 2013;37:809–817. doi: 10.1007/s00264-013-1807-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hettrich C.M., Dunn W.R., Reinke E.K., Group M., Spindler K.P. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: Two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engelman G.H., Carry P.M., Hitt K.G., Polousky J.D., Vidal A.F. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42:2311–2318. doi: 10.1177/0363546514541935. [DOI] [PubMed] [Google Scholar]
- 7.Kaeding C.C., Aros B., Pedroza A. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., Consortium M., Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dai C., Wang F., Wang X., Wang R., Wang S., Tang S. Arthroscopic single-bundle anterior cruciate ligament reconstruction with six-strand hamstring tendon allograft versus bone-patellar tendon-bone allograft. Knee Surg Sports Traumatol Arthrosc. 2016;24:2915–2922. doi: 10.1007/s00167-015-3569-9. [DOI] [PubMed] [Google Scholar]
- 10.Xie X., Liu X., Chen Z., Yu Y., Peng S., Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100–110. doi: 10.1016/j.knee.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Conte E.J., Hyatt A.E., Gatt C.J., Jr., Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882–890. doi: 10.1016/j.arthro.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 12.Iriuchishima T., Shirakura K., Yorifuji H., Aizawa S., Fu F.H. Size comparison of ACL footprint and reconstructed auto graft. Knee Surg Sports Traumatol Arthrosc. 2013;21:797–803. doi: 10.1007/s00167-012-1949-y. [DOI] [PubMed] [Google Scholar]
- 13.Barrett G.R., Noojin F.K., Hartzog C.W., Nash C.R. Reconstruction of the anterior cruciate ligament in females: A comparison of hamstring versus patellar tendon autograft. Arthroscopy. 2002;18:46–54. doi: 10.1053/jars.2002.25974. [DOI] [PubMed] [Google Scholar]
- 14.Liu Y., Cui G., Yan H., Yang Y., Ao Y. Comparison between single- and double-bundle anterior cruciate ligament reconstruction with 6- to 8-stranded hamstring autograft: A prospective, randomized clinical trial. Am J Sports Med. 2016;44:2314–2322. doi: 10.1177/0363546516650876. [DOI] [PubMed] [Google Scholar]
- 15.Ahn J.H., Lee S.H. Anterior cruciate ligament double-bundle reconstruction with hamstring tendon autografts. Arthroscopy. 2007;23:109.e101–109.e104. doi: 10.1016/j.arthro.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 16.Lubowitz J.H. All-inside anterior cruciate ligament graft link: Graft preparation technique. Arthrosc Tech. 2012;1:e165–e168. doi: 10.1016/j.eats.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kern M., Love D., Cotter E.J., Postma W. Quadruple-bundle semitendinosus-gracilis graft technique for all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1317–e1320. doi: 10.1016/j.eats.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park K., Brusalis C.M., Ganley T.J. The 8-strand hamstring autograft in anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1105–e1109. doi: 10.1016/j.eats.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feller J.A., Webster K.E. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 20.Aglietti P., Giron F., Buzzi R., Biddau F., Sasso F. Anterior cruciate ligament reconstruction: Bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. [PubMed] [Google Scholar]
- 21.Maletis G.B., Cameron S.L., Tengan J.J., Burchette R.J. A prospective randomized study of anterior cruciate ligament reconstruction: A comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35:384–394. doi: 10.1177/0363546506294361. [DOI] [PubMed] [Google Scholar]
- 22.Sajovic M., Strahovnik A., Dernovsek M.Z., Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: An 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161–2169. doi: 10.1177/0363546511411702. [DOI] [PubMed] [Google Scholar]
- 23.Courvoisier A., Grimaldi M., Plaweski S. Good surgical outcome of transphyseal ACL reconstruction in skeletally immature patients using four-strand hamstring graft. Knee Surg Sports Traumatol Arthrosc. 2011;19:588–591. doi: 10.1007/s00167-010-1282-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hamstring graft preparation techniques for ACL reconstruction. First, we show the 2-strand technique with 1 tendon. The tendon is loaded into a suspensory device. The 2 free ends of the graft are stitched together with a nonabsorbable suture to create equal lengths of each half. The graft is then whipstiched with Fiberloop at the end to reinforce it. Then, we show the 4-strand technique with 1 tendon. Once the 2 free ends of the graft are stitched together, a suture is passed in the middle and the tendons are folded. The needle is passed through the proximal part of the graft stump, grabbing and tensioning the distal part with a nonabsorbable suture. The 4-strand graft is then whipstiched with Fiberloop from proximal to distal. Next, we show the 3-strand technique with 1 tendon. The tendon is folded into 3 equal parts, and the junction at each fold is marked. The tendon is loaded in a suspensory device at one of the marks. A stitch at each end of the tendon is made with a nonabsorbable suture leaving a tail. The needle is then passed through the other 2 strands of the graft. The same procedure is then repeated at the other end. Then, we show the 5-strand technique with 2 tendons. A 3-strand graft is prepared with 1 tendon as showed previously. The other tendon is loaded in the same suspensory device, alongside it. A needle is passed at the end of the 3-strand graft, through all 5 strands. The 5-strand graft is then whipstiched with Fiberloop from proximal to distal. Finally, we show the 4-strand technique with 2 tendons. Both tendons are loaded in a suspensory device with a reverse orientation. A nonabsorbable suture is passed twice around the 4 free ends of the graft. The graft is whipstiched with a continuous nonabsorbable suture from distal to proximal and then from proximal to distal to reinforce the distal site of the graft.