Abstract
BACKGROUND
While individual-level determinants of health, such as education and income, have been well documented among breast cancer survivors, little is known about the role of neighborhood context on survivorship outcomes among this population. The present study examined the association of neighborhood stress with multiple health outcomes among ethnic minority breast cancer survivors (BCS).
METHODS
A mixed-methods approach was used to recruit 320 African-American and Hispanic BCS who were 26–89 years and lived in metropolitan Los Angeles, CA. Neighborhood stress was assessed by six items taken from the Life Stress Scale. Health outcomes included (i) self-rated health, measured by the Short-Form-36 Health Survey, (ii) number of comorbidities (0–14), (iii) depressive symptoms, assessed by the Center for Epidemiological Studies-Depression scale, and (iv) psychological difficulties.
RESULTS
Greater neighborhood stress was significantly associated with poorer self-reported health (adjusted β = −0.22, 95% confidence interval [CI]: −0.40, −0.05), greater number of comorbidities (adjusted risk ratio = 0.19, 95% CI: 0.07, 0.30), more depressive symptoms (adjusted β = 0.10, 95% CI: 0.06, 0.15), and a higher likelihood of psychological difficulties (adjusted odds ratio = 2.28, 95% CI: 1.51, 3.45) among ethnic minority BCS.
CONCLUSIONS
These findings underscored the importance of taking neighborhood context into account in examining the determinants of health, survivorship, and quality of life outcomes among cancer patients. Our findings may inform population health, health services, and interventions addressing neighborhood and individual-level factors to promote post treatment health and survivorship outcomes as well as to identify high-risk patients, especially among medically vulnerable communities.
Keywords: Minority health, mental health, residence characteristics, breast neoplasm, survivors, African Americans, Hispanic Americans
INTRODUCTION
Despite the fact that breast cancer mortality rates have dropped by 34% since 1990, it remains the most commonly diagnosed cancer in women and continues to be a major public health problem in the United States (U.S) (American Cancer Society, 2016). The substantially improved survival rates of breast cancer over the past 20 years, which is primarily attributable to the advances in early detection, increases in the use of mammography screening, and improvements in treatments, has led to a rapidly growing number of breast cancer survivors (BCS) in the U.S. (American Cancer Society, 2016; Aziz & Rowland, 2002; Berry et al., 2005). As of January 1, 2016, it is estimated that there were over 3.5 million women BCS in the U.S., and this number is expected to continue to grow due to increase in population size, life expectancy, and continued improvements in survival (Miller et al., 2016). The increase in the survivorship has led to a growing interest in investigating the health outcomes in this population.
Still, relatively few studies have focused on the post-treatment health outcomes among ethnic minority BCS. It has been well-documented that unfavorable survival, physical, functional, psychological, and social outcomes disproportionately affect African-American and Hispanic BCS (K. T. Ashing-Giwa, Rosales, Lai, & Weitzel, 2013; Chatman & Green, 2011; Morehead-Gee et al., 2012; Nurgalieva et al., 2013; Sturtz, Melley, Mamula, Shriver, & Ellsworth, 2014). Therefore, it is critically important for health researchers to identify the factors that contribute to disparate health outcomes among ethnic minority BCS. This type of research is especially urgent given the rapidly growing ethnic minority representation among cancer patients and survivors in the U.S. Targeted research can begin to fill the gap and inform practice guidelines to reduce health disparities and improve health and survivorship outcomes among medically vulnerable survivors.
Prior studies highlighted the role of individual-level factors such as socioeconomic status (SES), education, and financial difficulties in determining the health and well-being among BCS (Ahles et al., 2005; K. T. Ashing-Giwa & Lim, 2009; Lim & K. T. Ashing-Giwa, 2011). In addition, several studies have shed light on the impact of neighborhood context on health outcomes such as self-reported physical and mental health (Subramanian, Acevedo-Garcia, & Osypuk, 2005; Wen, Hawkley, & Cacioppo, 2006), physical activity (Powell, Slater, Chaloupka, & Harper, 2006), morbidity (Roux et al., 2001), and mortality (Pickett & Pearl, 2001) among general population. However, not enough attention has been paid to the relationship between neighborhood context and health among ethnic minority BCS. Recent studies show a connection between SES and quality of life. In a multi-ethnic study on BCS, socioecologic stress, was shown to be the most important factor influencing physical and mental health quality of life (K. T. Ashing-Giwa & Lim, 2009).
Over the past several decades in health sciences, there has been a growing interest in investigating the effects of neighborhood context on individuals’ physical and mental health (Clarke et al., 2014; Kawachi & Berkman, 2003). Most studies of health and cancer disparities have used measures at the census tract level such as SES (Byers et al., 2008), residential segregation (Landrine & Corral, 2009), and poverty level (Krieger, Chen, Waterman, Rehkopf, & Subramanian, 2003) to assess the objective conditions of neighborhood context. However, the use of census-based variables as a proxy for neighborhood context suffered from two major weaknesses. First, the area within the census tract in which people reside could economically and demographically diverse, and, therefore, may not correspond with the geographic area representing their defined neighborhood (Stockdale et al., 2007). Second, a limited number of measures makes it difficult to capture the dynamic and multi-dimensional effects of neighborhood context on individuals’ health. Thus, a growing body of research have used subjective self-rated neighborhood context, which is assumed to be the comprehensive reflection of objective conditions of the neighborhood context, as an alternative (Wen et al., 2006). For example, (Ellaway, Macintyre, & Kearns, 2001) found that perceptions of residential environment were risk factors for self-rated health and mental health. Similarly, Molinari and colleagues (Molinari, Ahern, & Hendryx, 1998) identified the association between men’s perceptions of the residential environment and their self-reported physical functioning and health.
Despite the large body of evidence on effects of subjective self-rating of neighborhood on health outcomes among general population, surprisingly little attention has been paid to ethnic minority cancer survivors. The purpose of the present study was to investigate the association of patient reported evaluation of neighborhood context with health outcomes among a sample of African-American and Hispanic post-treatment BCS, aged 26–89 years and living in metropolitan Los Angeles. We hypothesized that both African American and Hispanic participants would endorse high levels of self-evaluated neighborhood stress that would be associated with and manifest in poorer self-rated health, a greater number of comorbidities, more frequent depressive symptoms, and a higher likelihood of experiencing psychological difficulties.
MATERIALS AND METHODS
Recruitment and Participants
This study is a secondary data analyses investigation. We analyzed baseline data from the parent health-related quality-of-life (HRQOL) psycho-educational trial with African-American and Hispanic BCS. The parent study implemented randomized, controlled, 2-armed trial (materials plus 10–12 week telephonic intervention or materials, only) designed to improve BCS’ HRQOL. For this specific investigation, participant inclusion criteria consisted of disease-free women who were (i) 18 years of age and older, (ii) self-identified ethnically as African-American or Hispanic, (iii) within 1–5 years of a breast cancer diagnosis, (iv) diagnosed with stage 0–III breast cancer, and (v) not diagnosed with any other type of cancer. We used a mixed-method recruitment approach to enroll BCS from population-based sources (i.e., City of Hope, CA and University of California, Los Angeles-Cancer Registries, support groups). Institutional Review Board approval was obtained, and all participants signed an informed consent form for study participation. BCS who agreed to participate were mailed a package containing consent forms and the baseline assessment in their language of preference, and prepaid return envelopes. All participant materials were available in English and Spanish. Measures that were only available in English were translated into Spanish by two bilingual native Spanish speakers and back-translated into English by two separate bilingual individuals to verify accuracy. Trained bilingual staff conducted the participant recruitment. After completion of the baseline assessment, participants received a $20 grocery store gift card. Details of the parent study including trial procedures and trial outcomes have been reported elsewhere (K. T. Ashing-Giwa & Rosales, 2012; K.T. Ashing-Giwa & Rosales, 2014).
Outcomes
Self-Rated Health
Two different measures were used to assess general health. First, self-rated health was measured based a single survey question taken from the Short-Form-36 Health Survey. Participants were asked, “In general, would you say your health is 5 = excellent, 4 = very good, 3 = good, 2 = fair or 1 = poor?” Self-rated health has been shown to be a valid and reliable measure of general physical health (Dwyer & Mitchell, 1999), and poor self-rated health was found to be a risk factor for functional disability, chronic diseases, anxiety, depression, and mortality (Farmer & Ferraro, 1997; Idler & Benyamini, 1997; Wu, Parkerson, & Doraiswamy, 2002).
Comorbidities
Participants self-reported whether they had experienced any of the 14 chronic health conditions (e.g., arthritis, high blood pressure, diabetes). A composite variable counting the number of experienced comorbidities was constructed and used for further analyses. Inclusion of these chronic health conditions in the checklist is consistent with prior research focusing on ethnic minority cancer survivors (K. T. Ashing-Giwa & Lim, 2009).
Mental Health
Mental health was assessed using two distinct measurements. First, mental health was measured using 19 items taken from the 20-item Center for Epidemiologic Studies Depression (CES-D) Scale (Radloff, 1977), a well validated and widely used scale designed to measure depressive symptoms in the general as well as multiethnic population. The 19 items indicate how often in the past 4 months participants experienced a particular depressive symptom. Each of the 19 items have 4 possible responses that are rarely/none of the time, some/a little of the time (1–2 days), occasionally (3–4 days), and all of the time (5–7 days). After three items were reverse coded, all 19 items were added to calculate the composite depression score. The resulting sum score ranges from 19 to 76, with higher score indicating more frequent depressive symptoms. The Cronbach’s alpha for this scale was .88 showing adequate internal consistency. Alternatively, mental health was assessed by self-reported psychological difficulties after breast cancer treatment (yes or no). Participants were asked whether they “currently have moderate to major psychological difficulties such as depression, anxiety, recent suicide attempts, or recent mental health hospitalization.”
Predictors
Subjective perception of neighborhood stress was assessed by a subscale taken from the Life Stress Scale (K. T. Ashing-Giwa, Padilla, Tejero, & Kim, 2004), a 21-item Likert-type scale designed to measure the stress level of various socioecological contextual aspects of life and has been primarily used among African American and Hispanic samples (K. T. Ashing-Giwa & Lim, 2009; K. T. Ashing-Giwa, Ganz, & Petersen, 1999). This subscale had six items asking participants to indicate how much stress they have experienced during the past 3 months for the following aspects of neighborhood context: housing situation, neighborhood environment, transportation, availability of public services, crime and violence, and relation with police. Each of the six items was rated from 1 (no stress) to 5 (extreme stress). A composite index was generated averaging over six items. This scale had moderately high internal consistency (Cronbach’s α = 0.77). Principal component analysis, a data reduction technique widely utilized to create new composite variables, revealed that the scale only had one principal factor underlying the six items, suggesting it is reasonable to construct a composite variable based on these six items. Factor loadings of these six items ranged from 0.62 to 0.76 (Supplementary Table 1).
Covariates
All participants self-reported their age (years), race/ethnicity (African America or Hispanic), annual household income, number of years residing in the U.S., highest level of formal education, marital status (married/committed relationship or not), working status (currently working or not), occupation (homemaker/housewife, managerial/profession specialty, technical workers, service, operator/laborer/fabricator, or other), stage of breast cancer at diagnosis (0, I, II, or III), and receipt of surgery (lumpectomy and mastectomy), chemotherapy, and radiation. Annual household income was measured as one of seven self-reported income categories ranging from less than $15,000 to greater than $75,000. Education was measured in eight categories, self-reported as highest level of formal educational ranging from grade school to completed doctoral degree. The categories were collapsed into three groups that are low (less than a high school degree), medium (high school graduate), and high (more than a high school degree) according to the International Standard Classification of Education (Co-operation & Development, 1999).
Statistical Analysis
We first described the baseline characteristics of the study participants using mean and standard deviation for continuous variables and count and proportion for categorical variables. We also compared the characteristics between African American and Hispanic BCS using a two-sample t-test with unequal variance for continuous variables and a χ2 test for categorical variables.
We used a series of generalized linear regressions to identify the association of neighborhood stress with health outcomes (self-rated health, number of comorbidities, depressive symptoms, and psychological difficulties). Self-rated health was modeled as a continuous outcome using linear regression. Number of comorbidities was measured using a Poisson regression, which is commonly used for count data. CES-D score was modeled using a linear regression; because the distribution of the raw CES-D score was highly right-skewed, a logarithm-transformation was used to improve its normality. Psychological difficulties (yes or no) was modeled using a logistic regression. Age (years), race/ethnicity (African America or Hispanic), marital status (married or not), education (< high school, high school graduate, > high school), annual household income (<$15,000, $15,000–25,000, $25,000–35,000, $35,000–45,000, $45,000–60,000, $60,000–75,000, or $75,000), working status (currently working or not), stage of breast cancer at diagnosis (0, I, II, or III), and receipt of chemotherapy and radiation were adjusted in all four models. As an exploratory analysis, we examined whether the association of neighborhood stress with outcomes differed between African-American and Hispanic women using the interaction approach. No multi-collinearity was found in any statistical models according to the Variance Inflation Factor diagnostics. All covariates were assessed at baseline. All analyses were conducted using Stata 13.1 with two-sided tests of significant level at p < .05 (StataCorp, College Station, TX).
RESULTS
Sample Characteristics
A total of 320 participants were included in the study with 232 Hispanics and 88 African Americans. The mean age was 54.5 years (SD = 11.5; range: 26–89 years) (Table 1). Over 75% of the participants reported a diagnosis of stage I or II breast cancer. Regarding surgery and treatment, 38.9%, 58.8%, 73.4% and 61.9% of the participants received lumpectomy, mastectomy, chemotherapy and, radiation, respectively. More than 60% of the participants were not working outside the home, and the annual household income was less than $15,000 for approximately 30% of the participants. Age, place of birth, years residing in the U.S., marital status, education level, annual household income, occupation, and receipt of mastectomy and chemotherapy all significantly differed by ethnicity (all p’s < .05). Hispanic women were older, less educated, and more financially disadvantaged, compared to African-American women. In addition, Hispanic women were more likely to be married, to be homemakers, to be born outside of the United States, to have spent fewer years residing in the U.S., and to receive chemotherapy. There were no substantial differences in perceived neighborhood stress between African-American and Hispanic women.
Table 1.
Descriptive statistics for sociodemographic and medical characteristics of study participants (n = 320).
| All (n=320) | African (n=88) | Hispanic (n=232) |
χ2 or t | |
|---|---|---|---|---|
|
|
||||
| Mean±SD or N (%) | ||||
| Age | 54.49±11.49 | 57.98±13.16 | 53.19±10.53 | 3.04** |
| Place of birth | ||||
| US | 146 (46.06%) | 85 (97.7%) | 61 (26.4%) | 128.73*** |
| Not in US | 171 (53.94%) | 2 (2.3%) | 169 (73.6%) | |
| Years residing in U.S. | 56.21±31.31 | 86.33±11.02 | 44.42±28.67 | 18.68*** |
| Marital Status | ||||
| Married/committed relationship | 177 (57.8%) | 37 (42.0%) | 140 (60.6%) | 12.64*** |
| Not married | 129 (42.2%) | 51 (58%) | 78 (39.2%) | |
| Education | ||||
| < High school | 113 (36.7%) | 4 (4.6%) | 109 (49.5%) | 65.16*** |
| High school graduate | 45 (14.61%) | 12 (13.6%) | 33 (15%) | |
| > High school | 150 (48.7%) | 72 (81.8%) | 78 (35.5%) | |
| Annual Household Income | ||||
| <$15,000 | 94 (29.6%) | 17 (19.5%) | 77 (33.3%) | 19.26** |
| $15,000 – $24,999 | 58 (18.2%) | 10 (11.5%) | 48 (20.8%) | |
| $25,000 – $34,999 | 37 (11.6%) | 9 (10.3%) | 28 (12.1%) | |
| $35,000 – $44,999 | 36 (11.3%) | 17 (19.5%) | 19 (8.2%) | |
| $45,000 – $59,999 | 20 (6.3%) | 9 (10.3%) | 11 (4.8%) | |
| $60,000 – $74,999 | 21 (6.6%) | 7 (8.0%) | 14 (6.1%) | |
| >$75,000 | 52 (16.4%) | 18 (20.7%) | 34 (14.7%) | |
| Occupation | ||||
| Homemaker/housewife | 115 (35.9%) | 16 (18.2%) | 99 (42.7%) | 27.67*** |
| Managerial, profession specialty | 73 (22.8%) | 31 (35.2%) | 42 (18.1%) | |
| Technical workers | 54 (16.9%) | 17 (19.3%) | 37 (15.9%) | |
| Service | 46 (14.4%) | 10 (11.4%) | 36 (15.5%) | |
| Operator, laborer, fabricator | 12 (3.8%) | 3 (3.4%) | 9 (3.9%) | |
| Other | 20 (6.3%) | 11 (12.5%) | 9 (3.9%) | |
| Working status | ||||
| Currently working | 123 (38.6%) | 32 (36.4%) | 91 (39.4%) | .25 |
| Breast cancer stage | ||||
| 0 | 17 (5.4%) | 6 (7.0%) | 11 (4.8%) | .93 |
| I | 119 (37.8%) | 34 (39.5%) | 85 (37.1%) | |
| II | 127 (40.3%) | 32 (37.2%) | 95 (41.5%) | |
| III | 52 (16.5%) | 14 (16.3%) | 38 (16.6%) | |
| Lumpectomy | 124 (38.9%) | 29 (33.0%) | 95 (41.0%) | 1.72 |
| Mastectomy | 188 (58.8%) | 63 (71.6%) | 125 (53.9%) | 8.25** |
| Chemotherapy | 4.58* | |||
| Yes | 234 (73.4%) | 57 (64.8%) | 177 (76.6%) | |
| Radiation | .09 | |||
| Yes | 135 (61.9%) | 64 (72.7%) | 171 (74.3%) | |
| Perceived neighborhood stress | 1.63±0.69 | 1.57±0.70 | 1.65±0.68 | .91 |
Abbreviations. SD, standard deviation.
Note.
p<.05,
p<.01,
p<.001
Among 320 included participants, 14 of them had missing data on at least one covariate adjusted in the generalized linear regressions. These 14 participants were excluded from further analyses. No significance differences were found in the predictor (i.e., neighborhood stress), outcomes, or covariates. No advanced techniques for handling missing data were therefore not applied (e.g., missing data imputation).
The Association of Neighborhood Stress with Self-Rated Health
Neighborhood stress was significantly associated with self-rated health after adjusting for socio-demographic and medical covariates (p < .05), with each one-unit increase in the neighborhood stress scale corresponding to a 0.22-unit decrease (95% Confidence interval [CI]: 0.05–0.40) in the self-rated health scale (Table 2). The association of neighborhood stress with self-rated health did not differ between African-Amirian and Hispanic women (p for interaction = .61). In addition, self-rated health was shown to be significantly differed by working status (p < .05). Individuals who were still working after receiving cancer treatment had better self-rated health than those who were not working.
Table 2.
The association of neighborhood stress with self-rated health (n = 306).
| Self-rated health | |
|---|---|
|
|
|
| β (95% CIs) | |
| Neighborhood stress | −.22 (−.40, −.05)* |
| Race/ethnicity | |
| African American | Ref. |
| Hispanic | −.07 (−.36, .21) |
| Age, years | −.01 (−.02, .00) |
| Married/committed relationship | .18 (−.07, .43) |
| Education | |
| < High school | Ref. |
| High school graduate | −.14 (−.50, .22) |
| >High school | .07 (−.25, .38) |
| Annual household income | |
| < $15,000 | Ref. |
| $15,000 – 25,000 | −.03 (−.37, .31) |
| $25,000 – 35,000 | −.09 (−.49, .31) |
| $35,000 – 45,000 | .20 (−.20., .61) |
| $45,000 – 60,000 | .15 (−.37, .68) |
| $60,000 – 75,000 | .25 (−.26, .76) |
| >$75,000 | .26 (−.18, .70) |
| Currently working | .31 (.04, .56)* |
| Breast cancer stage | |
| Stage 0 | Ref. |
| Stage I | .24 (−.27, .75) |
| Stage II | .09 (−.43, .62) |
| Stage III | .10 (−.46, .66) |
| Chemotherapy | .03 (−.25, .32) |
| Radiation | −.10 (−.37, .18) |
Abbreviations. CIs, confidence intervals.
Notes.
p<.05,
p<.01,
p<.001
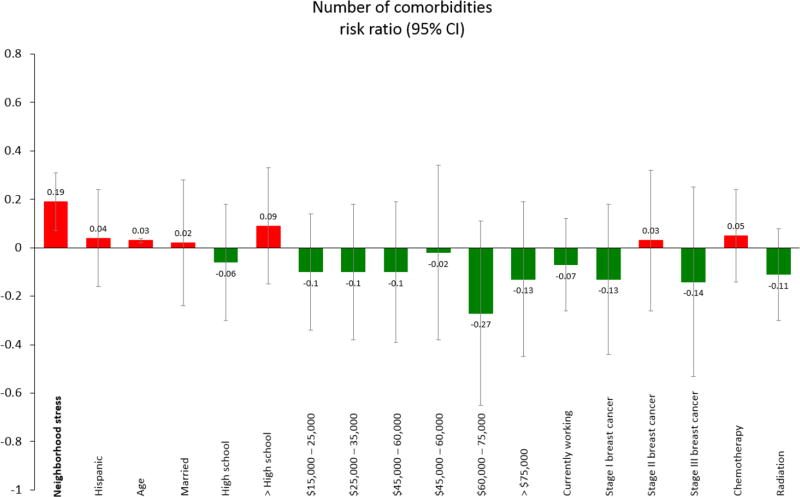
The Association of Neighborhood Stress with Comorbidities
In the multivariate-adjusted model, neighborhood stress was positively associated with number of self-reported comorbidities (Table 3). A one-unit higher on the neighborhood stress scale was related to approximately 0.2 (95% CI: 0.07–0.30) more comorbidities, adjusting for other covariates (Figure 1). The association of neighborhood stress with comorbidities did not differ between African-Amirian and Hispanic women (p for interaction = .82).
Table 3.
The association of neighborhood stress with number of comorbidities (n = 306).
| Number of Comorbidities | |
|---|---|
|
|
|
| Risk ratio (95% CIs) | |
| Neighborhood stress | .19 (.07, .30)** |
| Race/ethnicity | |
| African American | Ref. |
| Hispanic | .04 (−.16, .24) |
| Age, years | .03 (.02, .03)*** |
| Married/committed relationship | .02 (−.16, .19) |
| Education | |
| < High school | Ref. |
| High school graduate | −.06 (−.32, .20) |
| >High school | .09 (−.13, .31) |
| Annual household income | |
| < $15,000 | Ref. |
| $15,000 – 25,000 | −.10 (−.34, .13) |
| $25,000 – 35,000 | −.10 (−.38, .19) |
| $35,000 – 45,000 | −.10 (−.39, .19) |
| $45,000 – 60,000 | −.02 (−.38, .33) |
| $60,000 – 75,000 | −.27 (−.65, .11) |
| >$75,000 | −.13 (−.45, .19) |
| Currently working | −.07 (−.26, .12) |
| Breast cancer stage | |
| Stage 0 | Ref. |
| Stage I | −.13 (−.46, .21) |
| Stage II | .03 (−.32, .37) |
| Stage III | −.14 (−.53, .24) |
| Chemotherapy | .05 (−.14, .24) |
| Radiation | −.11 (−.30, .08) |
Abbreviations. CIs, confidence intervals.
Notes.
p<.05,
p<.01,
p<.001.
Figure 1.
The association of neighborhood stress with self-rated health. Participants self-reported whether they had experienced any of the 14 chronic health conditions. The reference group for education is less than high school; the reference group for income is less than $15,000; the reference group for breast cancer is stage 0.
The Association of Neighborhood Stress with Mental Health
The median CES-D score was significantly higher for those who experienced higher level of neighborhood stress compared to those who reported less neighborhood stress, adjusting for covariates (Table 4). In addition, Hispanic participants had significantly more depressive symptoms than African American participants (p < .01). The association of neighborhood stress with CES-D score did not differ between African-Amirian and Hispanic women (p for interaction = .52).
Table 4.
The association of neighborhood stress with depressive symptoms (n = 306).
| Log (CES-D) | |
|---|---|
|
|
|
| eβ (95% CIs) | |
| Neighborhood stress | .10 (.06, .15)*** |
| Race/ethnicity | |
| African American | Ref. |
| Hispanic | .11 (.03, .18)** |
| Age, years | .00 (−.003, .003) |
| Married/committed relationship | −.01 (−.07, .06) |
| Education | |
| < High school | Ref. |
| High school graduate | .06 (−.04, .15) |
| >High school | .02 (−.06, .10) |
| Annual household income | |
| < $15,000 | Ref. |
| $15,000 – 25,000 | −.03 (−.12, .06) |
| $25,000 – 35,000 | −.06 (−.16, .04) |
| $35,000 – 45,000 | −.02 (−.12, .08) |
| $45,000 – 60,000 | −.15 (−.29, −.02)* |
| $60,000 – 75,000 | −.07 (−.20, .04) |
| >$75,000 | −.16 (−.27, −.05)** |
| Currently working | .00 (−.08, .06) |
| Breast cancer stage | |
| Stage 0 | Ref. |
| Stage I | .10 (−.03, .23) |
| Stage II | .13 (.00, .26) |
| Stage III | .07 (−.08, .21) |
| Chemotherapy | −.05 (−.12, .02) |
| Radiation | .04 (−.03, .11) |
Abbreviations. CES-D, Center for Epidemiological Studies-Depression; CIs, confidence intervals.
Note.
p<.05,
p<.01,
p<.001
Neighborhood stress was significantly associated with the likelihood of having psychological difficulties (Table 5). A one-unit increase in the neighborhood stress scale was associated with a 128% (95% CI: 51%–245%) higher odds of experiencing psychological difficulties. The association of neighborhood stress with psychological difficulties did not differ between African-Amirian and Hispanic women (p for interaction = .34). In addition, Hispanic BCS had higher likelihood of experiencing psychological difficulties than African Americans (odds ratio = 2.27, 95% CI: 1.03–5.00).
Table 5.
The association of neighborhood stress with psychological difficulties among ethnic minority cancer survivors (n = 306).
| Psychological difficulties | |
|---|---|
|
|
|
| Odds ratio (95% CIs) | |
| Neighborhood stress | 2.28 (1.51, 3.45)*** |
| Race/ethnicity | |
| African American | Ref. |
| Hispanic | 2.27 (1.03, 5.00)* |
| Age, years | .99 (.96, 1.02) |
| Married/committed relationship | .80 (.43, 1.47) |
| Education | |
| < High school | Ref. |
| High school graduate | 1.40 (.60, 3.26) |
| >High school | .85 (.40, 1.79) |
| Annual household income | |
| < $15,000 | Ref. |
| $15,000 – 25,000 | .66 (.30, 1.49) |
| $25,000 – 35,000 | .76 (.29, 1.97) |
| $35,000 – 45,000 | .71 (.26, 1.89) |
| $45,000 – 60,000 | .78 (.21, 2.92) |
| $60,000 – 75,000 | 1.44 (.44, 4.64) |
| >$75,000 | .50 (.16, 1.57) |
| Currently working | .83 (.44, 1.55) |
| Breast cancer stage | |
| Stage 0 | Ref. |
| Stage I | 2.01 (.41, 10.67) |
| Stage II | 2.53 (.50, 13.17) |
| Stage III | 2.29 (.42, 13.32) |
| Chemotherapy | .46 (.21, .99)* |
| Radiation | 1.45 (.75, 2.81) |
Abbreviations. CIs, confidence intervals.
Note.
p<.05,
p<.01,
p<.001
DISCUSSION
This study focused on investigating the patient rated stress arising from neighborhood context and its associations with multiple health indicators among a sample of ethnic minority BCS. As was hypothesized, our results showed the negative impact of neighborhood stress on multiple health outcomes among African American and Hispanic BCS. We found that after adjusting important individual socio-demographic and medical characteristics, higher level of neighborhood stress was significantly associated with poorer self-rated general health, more co-occurring chronic illnesses, more frequent depressive symptoms, and higher likelihood of experiencing psychological difficulties.
This study is not without limitations. First, the analyses are cross-sectional, and therefore, the results should be interpreted with caution, and no causal relationship can be established between self-rated neighborhood stress and health outcomes. It is possible that individuals with decreased physical functioning or deteriorating mental status are more likely to feel more negative about their neighborhood contexts(Ellaway et al., 2001). This limitation suggests that future research utilizing longitudinal design is needed to corroborate the causality. In addition, since no objective measure of health was included, participants’ self-reported health status might overestimate or underestimate their actual health conditions. Second, only six items were selected in this study to reflect the objective features of the neighborhood. Although the internal consistency of the scale is remarkably high (α = 0.77) and single-factor solution was shown to be the best fit of the data by factor analysis with all six items having equivalently high loadings on the underlying neighborhood context construct, other important aspects of neighborhood such as accessibility to health care services and relationship with other ethnicities in the same neighborhood are not included. Since there has been no consensus reached on the definition and measurement of neighborhood environment (Aber & Nieto, 2000), inclusion of a broader range of neighborhood-level factors may result in revealing more than one underlying neighborhood contextual factor (Steptoe & Feldman, 2001). Another limitation is that we used the total score of 19 CES-D items instead of 20 to indicate the depression level because only 19 items were assessed in the survey. The missing item is “I was happy”; the primary reason was that this item is culturally biased and difficult to interpret based on previous studies (K. T. Ashing-Giwa, Rosales, Lai, & Weitzel, 2013; Jang, Kwag, & Chriboga, 2010; Maclntosh & Strickland, 2010). In addition, using 19 items is unlikely to lead to severely biased results in our study because we treated the total CES-D score as a continuous variable rather than a binary indicator (cutoff) to screen for depression. Moreover, the Cronbach's alpha for this 19-item scale was 0.88, suggesting good internal consistency.
In addition, future studies may benefit from including additional features of neighborhood and therefore higher content validity of the neighborhood context scale can be achieved and more individual variability in various health outcomes can be explained. As (Feldman & Steptoe, 2004) suggested, many features of neighborhood context may have impact on individual health through different pathways. Third, only subjective measurement of neighborhood context was included in our study. We assume that subjective self-rated neighborhood stress is a reflection of the objective features of the neighborhood context in which people reside. Feldman et al. found that self-rated neighborhood strain mediated the association between neighborhood socioeconomic and individual physical functioning using structural equation modeling. However, it is possible that self-rated neighborhood stress is attributable to sources other than the objective neighborhood characteristics and has separate impact on health. Fourth, the sample included in the study is geographically homogeneous, as all study participants resided in the Los Angeles metropolitan area. Thus, it is difficult to generalize our findings to other populations and geographic locations. For example, rural residents may not perceive the same amount of stress from certain aspects of their neighborhood as urban residents do. Despite the limitations mentioned above, the current study makes a number of contributions in understanding the relationship between neighborhood-level factors and health among ethnic minority BCS. The results highlight the importance of neighborhood contextual factors on patient-reported health and survivorship outcomes.
Overall, our findings are consistent with prior literature showing that neighborhood context is a significant predictor of self-rated health (Ellaway et al., 2001; Steptoe & Feldman, 2001) and mental health (Gary, Stark, & LaVeist, 2007; Stockdale et al., 2007) among general populations. In addition, our results are consistent with a previous study showing the negative relationship between socioecologic stress and health-related quality of life among BCS (K. T. Ashing-Giwa & Lim, 2009). One unique contribution of the present study is that it utilized multiple health outcomes measures within a cancer patient population; this provides a more comprehensive understanding of the broad health influence of neighborhood context. As our results showed, the neighborhood contexts seem to be important health predictors of general, physical and emotional health.
In conclusion, our findings suggest neighborhood context, in addition to individual-level health determinants, may be an important contributor to post cancer treatment outcomes. This study is among the first to investigate the relationship between neighborhood-related stress and health outcomes among minority cancer survivor. Our findings may inform population health, and health services interventions addressing neighborhood and individual-level factors to promote post treatment health and survivorship outcomes, especially among medically vulnerable communities. Future research, especially those with longitudinal data and objective neighborhood-level variables, is needed to obtain in-depth understanding of the complex relationship among objective neighborhood features, subjective patient-driven evaluations of neighborhood context, and health. This type of research is urgently needed in order to provide more conclusive evidence of the effect of neighborhood on cancer outcomes as well as guidance for targeted interventional remedy. Therefore, the study may have both scientific and clinical implications. Our results contribute to identifying the most robust predictors of disease outcomes that is essential to developing targeted, patient centered therapies and interventions to improve this outcome in ethnic minority BCS. Moreover, our findings add to the mounting evidence suggesting that for all patients including ethnic minority patients, we must begin to examine the sources of disparate outcomes beyond the race or ethnicity factors. Specifically, our results join emerging research suggesting that socioeconomic status and contextual factors including neighborhood factors must be considered in predicting and addressing health, disease and life expectancy outcomes.
Supplementary Material
References
- Aber MS, Nieto M. Suggestions for the investigation of psychological wellness in the neighborhood context: Toward a pluralistic neighborhood theory. The promotion of wellness in children and adolescents. 2000:185–219. [Google Scholar]
- Ahles TA, Saykin AJ, Furstenberg CT, Cole B, Mott LA, Titus-Ernstoff L, Silberfarb PM. Quality of life of long-term survivors of breast cancer and lymphoma treated with standard-dose chemotherapy or local therapy. Journal of Clinical Oncology. 2005;23(19):4399–4405. doi: 10.1200/JCO.2005.03.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. Cancer Facts & Figures 2016. American Cancer Society; Atlanta, GA, USA: 2016. [Google Scholar]
- Ashing-Giwa K, Rosales M. Recruitment and retention strategies of African American and Latina American breast cancer survivors in a longitudinal psycho-oncology study. Paper presented at the Oncology nursing forum. 2012 doi: 10.1188/12.ONF.E434-E442. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa KT, Lim J-w. Examining the impact of socioeconomic status and socioecologic stress on physical and mental health quality of life among breast cancer survivors. Paper presented at the Oncology nursing forum. 2009 doi: 10.1188/09.ONF.79-88. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa K, Ganz PA, Petersen L. Quality of life of African-American and white long term breast carcinoma survivors. Cancer. 1999;85(2):418–426. doi: 10.1002/(sici)1097-0142(19990115)85:2<418::aid-cncr20>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa K, Rosales M, Lai L, Weitzel J. Depressive symptomatology among Latina breast cancer survivors. Psycho-Oncology. 2013;22(4):845–853. doi: 10.1002/pon.3084. [DOI] [PubMed] [Google Scholar]
- Ashing-Giwa KT, Padilla GV, Tejero JS, Kim J. Breast cancer survivorship in a multiethnic sample. Cancer. 2004;101(3):450–465. doi: 10.1002/cncr.20370. [DOI] [PubMed] [Google Scholar]
- Ashing K, Rosales M. A telephonic-based trial to reduce depressive symptoms among Latina breast cancer survivors. Psycho-Oncology. 2014;23(5):507–515. doi: 10.1002/pon.3441. [DOI] [PubMed] [Google Scholar]
- Aziz NM, Rowland JH. Cancer survivorship research among ethnic minority and medically underserved groups. Paper presented at the Oncology Nursing Forum-Oncology Nursing Society. 2002 doi: 10.1188/02.ONF.789-801. [DOI] [PubMed] [Google Scholar]
- Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Feuer EJ. Effect of screening and adjuvant therapy on mortality from breast cancer. New England Journal of Medicine. 2005;353(17):1784–1792. doi: 10.1056/NEJMoa050518. [DOI] [PubMed] [Google Scholar]
- Byers TE, Wolf HJ, Bauer KR, Bolick-Aldrich S, Chen VW, Finch JL, Van Heest S. The impact of socioeconomic status on survival after cancer in the United States. Cancer. 2008;113(3):582–591. doi: 10.1002/cncr.23567. [DOI] [PubMed] [Google Scholar]
- Chatman MC, Green RD. Addressing the unique psychosocial barriers to breast cancer treatment experienced by African-American women through integrative navigation. Journal of National Black Nurses' Association: JNBNA. 2011;22(2):20–28. [PubMed] [Google Scholar]
- Clarke P, Morenoff J, Debbink M, Golberstein E, Elliott MR, Lantz PM. Cumulative exposure to neighborhood context consequences for health transitions over the adult life course. Research on aging. 2014;36(1):115–142. doi: 10.1177/0164027512470702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Co-operation, O. f. E. & Development. Classifying educational programmes: manual for ISCED-97 implementation in OECD countries. OECD; Paris: 1999. [Google Scholar]
- Dwyer DS, Mitchell OS. Health problems as determinants of retirement: Are self-rated measures endogenous? Journal of health economics. 1999;18(2):173–193. doi: 10.1016/s0167-6296(98)00034-4. [DOI] [PubMed] [Google Scholar]
- Ellaway A, Macintyre S, Kearns A. Perceptions of place and health in socially contrasting neighbourhoods. Urban studies. 2001;38(12):2299–2316. [Google Scholar]
- Farmer MM, Ferraro KF. Distress and perceived health: mechanisms of health decline. Journal of Health and Social Behavior. 1997:298–311. [PubMed] [Google Scholar]
- Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Annals of Behavioral Medicine. 2004;27(2):91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health & place. 2007;13(2):569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997:21–37. [PubMed] [Google Scholar]
- Jang Yuri, Kwag Kyung Hwa, Chiriboga David A. Not saying I am happy does not mean I am not: cultural influences on responses to positive affect items in the CES-D. The Journals of Gerontology Series B. Psychological Sciences and Social Sciences. 2010;65.6:684–690. doi: 10.1093/geronb/gbq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Neighborhoods and health. Oxford University Press; 2003. [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian S. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures-the public health disparities geocoding project. American journal of public health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H, Corral I. Separate and unequal: residential segregation and black health disparities. Ethnicity & disease. 2009;19(2):179. [PubMed] [Google Scholar]
- Lim J-w, Ashing-Giwa KT. Examining the effect of minority status and neighborhood characteristics on cervical cancer survival outcomes. Gynecologic oncology. 2011;121(1):87–93. doi: 10.1016/j.ygyno.2010.11.041. [DOI] [PubMed] [Google Scholar]
- MacIntosh RC, Strickland OJ. Differential item responses on CES-D inventory: a comparison of elderly Hispanics and non-Hispanic Whites in the United States and item usage by elderly Hispanics across time. Aging & Mental Health. 2010;14(5):556–564. doi: 10.1080/13607860903421045. [DOI] [PubMed] [Google Scholar]
- Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Jemal A. Cancer treatment and survivorship statistics, 2016. CA: a cancer journal for clinicians. 2016 doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- Molinari C, Ahern M, Hendryx M. The relationship of community quality to the health of women and men. Social science & medicine. 1998;47(8):1113–1120. doi: 10.1016/s0277-9536(98)00114-2. [DOI] [PubMed] [Google Scholar]
- Morehead-Gee AJ, Pfalzer L, Levy E, McGarvey C, Springer B, Soballe P, Stout NL. Racial disparities in physical and functional domains in women with breast cancer. Supportive Care in Cancer. 2012;20(8):1839–1847. doi: 10.1007/s00520-011-1285-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurgalieva Z, Franzini L, Morgan R, Vernon S, Liu C, Du X. Surveillance mammography use after treatment of primary breast cancer and racial disparities in survival. Medical Oncology. 2013;30(4):1–8. doi: 10.1007/s12032-013-0691-8. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of epidemiology and community health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. American journal of public health. 2006;96(9):1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- Roux AVD, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Watson RL. Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD. The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc Sci Med. 2007;65(9):1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturtz LA, Melley J, Mamula K, Shriver CD, Ellsworth RE. Outcome disparities in African American women with triple negative breast cancer: a comparison of epidemiological and molecular factors between African American and Caucasian women with triple negative breast cancer. BMC cancer. 2014;14(1):1. doi: 10.1186/1471-2407-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, Acevedo-Garcia D, Osypuk TL. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Soc Sci Med. 2005;60(8):1667–1679. doi: 10.1016/j.socscimed.2004.08.040. [DOI] [PubMed] [Google Scholar]
- Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: An analysis of older adults in Cook County, Illinois. Soc Sci Med. 2006;63(10):2575–2590. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Wu LR, Parkerson GR, Doraiswamy PM. Health perception, pain, and disability as correlates of anxiety and depression symptoms in primary care patients. The Journal of the American Board of Family Practice. 2002;15(3):183–190. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.