SUMMARY:
DSC perfusion MR imaging in brain tumors requires a trade-off between spatial and temporal resolution, resulting in less spatial coverage to meet the temporal resolution requirements for accurate relative CBV estimation. DSC-MR imaging could potentially benefit from the advantages associated with simultaneous multi-slice imaging, including increased spatiotemporal resolution. In the current article, we demonstrate how simultaneous multi-slice EPI can be used to improve DSC-MR imaging spatiotemporal resolution in patients with glioblastoma.
DSC perfusion MR imaging estimates of relative CBV (rCBV) have been shown to differentiate histologic tumor grade,1,2 predict survival, and be useful for therapeutic monitoring in brain tumors3; however, DSC requires compromises in image resolution, slice coverage, and temporal resolution. The TR must be short enough to capture the rapid passage of the contrast bolus through the blood vasculature, but at the same time, there must be enough spatial coverage to encapsulate the entire tumor or brain. Simultaneous multi-slice (SMS) EPI4 has drawn widespread attention due to the advent of highly accelerated images5 through the application of composite radiofrequency pulses to simultaneously excite multiple slice planes.6 The SMS technique excites multiple slices physically separated across the z-axis simultaneously so that each SMS “slab” has slices acquired interleaved within that section. SMS has been shown to not have appreciable loss in SNR compared with traditional methods,4 and studies have shown that SMS is effective in reducing the acquisition time with higher spatiotemporal resolution.5,7,8 In the current article, we demonstrate the clinical utility of using SMS-EPI to increase the spatiotemporal resolution of DSC-MR imaging in patients with glioblastoma.
Materials and Methods
Patients
Thirteen patients with pathologically confirmed primary glioblastoma with recurrence based on either MR imaging, clinical deterioration, and/or histology were enrolled in this prospective study, which was approved by our local ethics institutional review board (University of California, Los Angeles). All patients underwent DSC-MR imaging with conventional single-shot EPI followed by SMS-EPI, 1–2 months later.
DSC-MR Imaging Acquisition
A preload bolus of 0.025 mmol/kg of Gd-DTPA (Magnevist; Bayer HealthCare Pharmaceuticals, Wayne, New Jersey) was administered to reduce leakage effects followed by 0.075 mmol/kg of Gd-DTPA at a rate of 5 mL/s. Two minutes of data were acquired, including a 30-second prebolus baseline and 90 seconds of data during and following contrast injection.
Conventional DSC-MR imaging was then acquired using a single-shot gradient-echo EPI at 3T (Prisma; Siemens, Erlangen, Germany) with TE = 35 ms, TR = 1.25–1.9 seconds, flip angle = 60°, FOV = 24 × 24 cm, matrix size = 128 × 128, generalized autocalibrating partially parallel acquisition = 2, slice thickness = 5 mm with no interslice gap, and 15- to 20-slice coverage. The voxel size was 1.875 × 1.875 × 5 mm, and the temporal resolution was 1.25–1.90 seconds.
Accelerated DSC-MR imaging was obtained with single-shot SMS-EPI with TE = 35ms, TR = 750 ms, flip angle = 60°, FOV = 21.6 × 24 cm, matrix size = 180 × 200, slice thickness = 4 mm with no interslice gap, controlled aliasing in parallel imaging results in higher acceleration factor = 2, and an SMS acceleration factor of 4 for a total of 30 slices through the whole brain. Voxel sizes were 1.2 × 1.2 × 4 mm with temporal resolution of 0.75 seconds.
Postprocessing of DSC-MR Imaging
Relative cerebral blood volume maps were generated with custom scripts including correction for bidirectional contrast agent exchange between the vascular and extravascular space.9 All rCBV values were normalized to contralateral normal-appearing white matter.
ROI and Statistical Analyses
Contrast-enhancing tumor ROIs were defined in 3D using custom scripts from Analysis of Functional Neuro Images (AFNI; http://afni.nimh.nih.gov/afni), excluding hemorrhage, large vessels, and central necrosis, followed by manual editing to exclude nonlesional voxels.9 Additionally, 2-cm-diameter spheric ROIs were placed on contralateral normal-appearing white matter for normalization of rCBV measurements. The percentage difference in the mean rCBV ratio, maximum tumor rCBV difference, and voxelwise correlations between single-shot EPI and SMS-EPI were estimated from the resulting data for all 13 patients. GraphPad Prism software, Version 6.0h (GraphPad Software, San Diego, California) was used for all statistical analyses.
Results
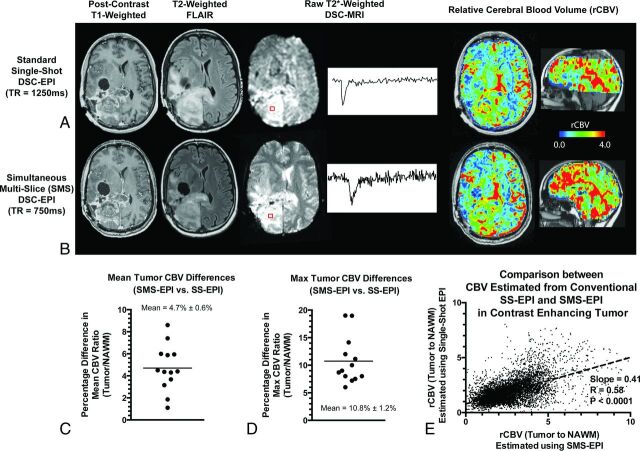
Both raw DSC and calculated rCBV maps were of comparable quality; however, rCBV maps calculated with SMS-EPI were obtained for the entire brain and at slightly higher spatial resolution compared with rCBV maps obtained with conventional single-shot EPI (Fig 1A, -B). The mean tumor rCBV difference between these 2 techniques was 4.7% ± 0.6% (Fig 1C), and the maximum tumor rCBV difference was 10.8% ± 1.2% (Fig 1D). Voxelwise correlations in rCBV between the 2 techniques showed a significant association in all patients examined (Fig 1E), with rCBV ratios in the tumor with respect to normal-appearing white matter slightly higher when estimated using SMS-EPI.
Fig 1.
Postcontrast T1-weighted images, T2-weighted FLAIR images, and raw T2*-weighted DSC MR images with corresponding signal-time curves across time from tumor regions accompanied by resulting relative cerebral blood volume maps for conventional single-shot EPI (A) and simultaneous multi-slice EPI (B) (left to right). Percentage difference in mean tumor rCBV ratio (tumor to normal-appearing white matter) (C) and percentage difference in the maximum tumor rCBV ratio (tumor to normal-appearing white matter) (D) in 13 patients with recurrent glioblastoma. E, Voxelwise correlation of rCBV ratio between conventional single-shot EPI and SMS-EPI.
Conclusions
SMS-EPI can increase the spatiotemporal resolution in DSC-MR imaging, resulting in larger brain coverage (12 versus 10 cm), higher in-plane spatial resolution (1.2 × 1.2 × 4 mm versus 1.875 × 1.875 × 5 mm), and faster temporal resolution (0.75 versus 1.25–1.90 seconds), with comparable results in quantification of tumor vascularity and clinical feasibility. While the potential impact on slice-to-slice perfusion quantitation is not currently known and results suggest that there may be little effect, a larger study is warranted. Together, these data demonstrate the potential clinical value of using SMS-EPI to estimate rCBV in patients with brain tumors with a high degree of reproducibility in terms of vascular biology quantification compared with historical test-retest studies.10
ABBREVIATIONS:
- rCBV
relative CBV
- SMS
simultaneous multi-slice
Footnotes
Disclosures: Whitney B. Pope—RELATED: Consulting Fee or Honorarium: Bracco; UNRELATED: Grants/Grants Pending: Guerbet.* Benjamin M. Ellingson—RELATED: Grant: Siemens; UNRELATED: Board Membership: MedQIA, Medicenna, Roche, Agios Pharmaceuticals, Bristol-Myers Squib; Consultancy: MedQIA, Medicenna, Roche, Agios Pharmaceuticals, Bristol-Myers Squib. *Money paid to the institution.
This work was supported by the American Cancer Society Research Scholar Grant RSG-15-003-01-CCE (B.M.E.); the National Institutes of Health/National Cancer Institute R21CA167354 (B.M.E.); an American Brain Tumor Association Research Collaboration Grant supported by Humor to Fight the Tumor, ARC1700002 (B.M.E.); a National Brain Tumor Society research grant (B.M.E.); a National Institutes of Health/National Institute of General Medical Sciences training grant, GM08042 (K.L.); and the University of California, Los Angeles Medical Scientist Training Program (K.L.).
References
- 1. Aronen HJ, Gazit IE, Louis DN, et al. Cerebral blood volume maps of gliomas: comparison with tumor grade and histologic findings. Radiology 1994;191:41–51 10.1148/radiology.191.1.8134596 [DOI] [PubMed] [Google Scholar]
- 2. Cha S, Knopp EA, Johnson G, et al. Intracranial mass lesions: dynamic contrast-enhanced susceptibility-weighted echo-planar perfusion MR imaging. Radiology 2002;223:11–29 10.1148/radiol.2231010594 [DOI] [PubMed] [Google Scholar]
- 3. Law M, Yang S, Wang H, et al. Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol 2003;24:1989–98 [PMC free article] [PubMed] [Google Scholar]
- 4. Barth M, Breuer F, Koopmans PJ, et al. Simultaneous multislice (SMS) imaging techniques. Magn Reson Med 2016;75:63–81 10.1002/mrm.25897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feinberg DA, Moeller S, Smith SM, et al. Multiplexed echo planar imaging for sub-second whole brain FMRI and fast diffusion imaging. PLoS One 2010;5:e15710 10.1371/journal.pone.0015710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maudsley AA. Multiple-line-scanning spin density imaging. J Magn Reson 1980;41:112–26 [Google Scholar]
- 7. Chen L, T Vu A, Xu J, et al. Evaluation of highly accelerated simultaneous multi-slice EPI for fMRI. Neuroimage 2015;104:452–59 10.1016/j.neuroimage.2014.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Feinberg DA, Setsompop K. Ultra-fast MRI of the human brain with simultaneous multi-slice imaging. J Magn Reson 2013;229:90–100 10.1016/j.jmr.2013.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ellingson BM, Cloughesy TF, Lai A, et al. Quantitative volumetric analysis of conventional MRI response in recurrent glioblastoma treated with bevacizumab. Neuro Oncol 2011;13:401–09 10.1093/neuonc/noq206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Henry ME, Kaufman MJ, Lange N, et al. Test-retest reliability of DSC MRI CBV mapping in healthy volunteers. Neuroreport 2001;12:1567–69 10.1097/00001756-200106130-00011 [DOI] [PubMed] [Google Scholar]