Abstract
A 67-year-old man developed a suspected adverse drug reaction during treatment with topical 5-fluorouracil (5-FU) for multiple actinic keratosis of the face, neck, and forearms. The man received topical 5-FU at a dosage of 0.5% for the actinic keratoses. After 1 week, he developed extreme lethargy, fatigue, fever, and mouth erosions. Several days later, and after discontinuation of 5-FU, painful mucositis and systemic side effects occurred, meeting criteria for hospitalization because of dehydration and a 6.8 kg weight loss. Hematology/oncology was consulted, and a possible systemic 5-FU reaction, similar to reactions to intravenous chemotherapy seen with a dihydropyrimidine dehydrogenase deficiency was suggested. The patient was not taking any concurrent medications, and he refused dihydropyrimidine dehydrogenase deficiency testing.
Key Points
| We report a life-threatening reaction, possibly from topical 0.5% 5-fluorouracil cream, which is a lower strength dose than the only reported case of a life-threatening adverse event with 5.0% 5-fluorouracil cream. |
| Given the common use of topical 5-fluorouracil cream, it is important for clinicians to consider the adverse side effects that can occur, especially in patients with a dihydropyrimidine dehydrogenase deficiency. |
Introduction
5-Fluorouracil (5-FU) is a common chemotherapeutic for the treatment of different malignancies, including carcinomas of the gastrointestinal tract, breast, and skin [1]. The rate-limiting enzyme in the catabolic pathway is dihydropyrimidine dehydrogenase (DPD), and studies have shown that decreased DPD activity leads to less drug clearance and increased toxicity [1]. Toxicities from systemic exposure include diarrhea, stomatitis, mucositis, pancytopenia, sepsis, cardiotoxicity, and—in some cases—death [2, 3]. The treatment for actinic keratosis includes cryotherapy, topical 5-FU, topical imiquimod, topical diclofenac, photodynamic therapy, and surgical excision. Topical 5-FU has been a gold standard treatment for years, especially with multiple lesions [4]. The most common side effects from topical 5-FU include skin irritation with associated erythema, dryness, and burning [4]. Very few reports of severe adverse reactions from topical 5-FU exist, but reactions include allergic contact dermatitis and inflammatory colitis [4]. Only one known life-threatening case of toxicity has been reported from topical 5-FU [1], but this case was reported after 5% 5-FU. To our knowledge, no similar adverse event has been reported with the lower-strength 0.5% 5-FU in the literature.
Case Report
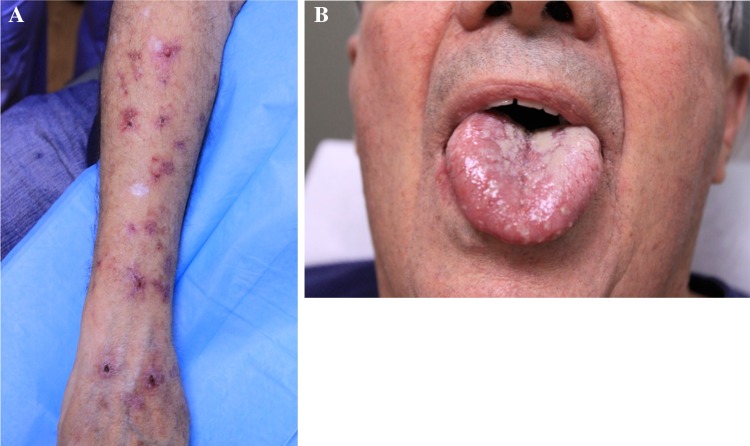
We report the case of an otherwise healthy 67-year-old man with no past medical history who presented with multiple actinic keratoses of the face, neck, and forearms. He was prescribed 0.5% 5-FU topical cream, which was to be applied to the skin daily for 30 days on his bilateral forearms. He was receiving no other medications that could have caused adverse interactions. After 1 week of topical use, he reported extreme lethargy, fatigue, fever, and mouth erosions. The medication was discontinued immediately. Physical examination revealed erythematous, scaly, and erosive plaques located on the bilateral anterior forearms (Fig. 1a) and multiple small ulcers of the hard palate. Several days after discontinuation of 5-FU, painful mucositis (Fig. 1b) and systemic 5-FU side effects occurred, including severe mucositis with mouth ulcerations, anorexia, 15-pound weight loss, and dehydration. No diarrhea was noted. The patient’s white blood cell count was normal. These systemic effects met criteria for hospitalization. Viral, bacterial, and fungal cultures of the mouth were negative, confirming a medication-induced mucositis. Complete blood count (CBC) and comprehensive metabolic panel (CMP) revealed dehydration but no signs of active infection or immunosuppression. Hematology/oncology was consulted, which stated that this presentation was likely due to a systemic 5-FU reaction, similar to the intravenous chemotherapy reaction seen with 5-FU. However, the patient refused DPD deficiency testing, so confirmation of deficiency could not be obtained. Supportive treatment along with intravenous fluids were administered for management. The medication was stopped before more possible adverse reactions, such as severe diarrhea or bone marrow suppression, were observed. The mucositis and systemic symptoms took approximately 1 month to resolve.
Fig. 1.
a Forearms post 1-week of nightly 0.5% 5-FU topical cream; b oral mucositis post 1-week with nightly 0.5% 5-FU cream
Discussion and Conclusion
Johnson and Diasio [5] reported the first patient with cancer known to develop life-threatening reactions after treatment with topical 5% 5-FU. This patient was found to be deficient in DPD, which contributed to the life-threatening toxicity. Review of the literature suggests approximately 3–5% of the general population have partial DPD deficiency [3]. In addition, DPD deficiency has been reported to be responsible for at least 50% of severe 5-FU treatment toxicity [3]. Further, 5-FU has been shown to have a narrow therapeutic index, and the literature also demonstrates it has a marked individual pharmacokinetic variability [6]. Therefore, a certain dose may produce a therapeutic response in one individual but a possible life-threatening toxicity in another [7, 8].
Because 5-FU is commonly used, and severe toxicity effects are associated with DPD deficiency, several methods have been developed to detect DPD deficiency. These include genotyping, radio-immunoassays, and measuring serum uracil concentrations, but these tests are expensive and time-consuming [9]. Given the rarity of life-threatening adverse events caused by topical 5-FU, developing a test to detect DPD deficiency would be more suitable for systemic therapy.
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and for inclusion of the accompanying images. A copy of the written consent may be requested for review from the corresponding author.
Conflicts of interest
Patrick Kishi and Cynthia J Price have no conflicts of interest that are directly relevant to the content of this manuscript.
References
- 1.Johnson M, Hageboutros A, Wang K, High L, Smith JB, Diasio RB. Life-threatening toxicity in a dihydropyrimidine dehydrogenase—deficient patient after treatment with topical 5—fluorouracil. Clin Cancer Res. 1999;5(8):2006–2011. [PubMed] [Google Scholar]
- 2.Van Kuilenburg AB, Baars JW, Meinsma R, van Gennip AH. Lethal 5-fluorouracil toxicity associated with a novel mutation in the dyhydropyrimidine dehydrogenase gene. Ann Oncol. 2003;14(2):341–342. doi: 10.1093/annonc/mdg056. [DOI] [PubMed] [Google Scholar]
- 3.Papnastasopoulos P, Stebbing J. Molecular basis of 5-fluorouracil-related toxicity: lessons from clinical practice. Anticancer Res. 2014;34(4):1531–1535. [PubMed] [Google Scholar]
- 4.Tutrone W, Saini R, Selin Caglar, et al. Topical therapy for actinic keratoses, I: 5—fluorouracil and imiquinod. Cutis. 2003;71(5):365–370. [PubMed] [Google Scholar]
- 5.Johnson M, Diasio R. Importance of dihydropyrimidine dehydrogenase (DPD) deficiency in patients exhibiting toxicity following treatment with 5-fluorouracil. Adv Enzyme Regul. 2001;41:151–157. doi: 10.1016/S0065-2571(00)00011-X. [DOI] [PubMed] [Google Scholar]
- 6.Gamelin E, Boisdron-Celle MB. Dose monitoring of 5-fluorouracil in patients with colorectal or head and neck cancer – status of the art. Crit Rev Oncol Hematol. 1999;30(1):71–79. doi: 10.1016/S1040-8428(98)00036-5. [DOI] [PubMed] [Google Scholar]
- 7.Gamelin E, Boisdron-Celle M, Delva R, Regimbeau C, Cailleux PE, Alleaume C, et al. Long-term weekly treatment of colorectal metastatic cancer with fluorouracil and leucovorin: results of a multicentric prospective trial of fluorouracil dosage optimization by pharmacokinetic monitoring in 152 patients. J Clin Oncol. 1998;16(4):1470–1478. doi: 10.1200/JCO.1998.16.4.1470. [DOI] [PubMed] [Google Scholar]
- 8.Gamelin E, Danquechin-Dorval E, Dumesnil Y, Maillart PJ, Goudier MJ, Burtin PC, et al. Relationship between 5-fluorouracil (5-FU) dose intensity and therapeutic response in patients with advanced colorectal cancer receiving infusional therapy containing 5-FU. Cancer. 1996;77(3):441–451. doi: 10.1002/(SICI)1097-0142(19960201)77:3<441::AID-CNCR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 9.Ezzeldin H, Diasio R. Dihydropyrimidine dehydrogenase deficiency, a pharmacogenetic syndrome associated with potentially life-threatening toxicity following 5-fluorouracil administration. Clin Colorectal Cancer. 2004;4(3):181–189. doi: 10.3816/CCC.2004.n.018. [DOI] [PubMed] [Google Scholar]