Abstract
Background
This study examined the effect of roughening of the root surface using an erbium-doped yttrium aluminum garnet (Er: YAG) laser on the binding strength of teeth undergoing root canal treatment.
Material/Methods
Ninety single-rooted teeth were used and assigned randomly to 9 groups (n=10 each). Root canals were prepared using the FlexMaster rotary system. An Er: YAG laser was applied to the root canals in Group 1, with no surface treatment of the glass-fiber post. In Group 2, aluminum oxide particles were applied. In Group 3, the laser was applied to the root canals, with Cojet treatment. Group 4 received laser treatment and Clearfil Ceramic Primer. In Group 5, Clearfil Ceramic Primer silane coupling was performed on post surfaces without laser treatment. In Group 6, hydrofluoric acid (HF) application was followed by Clearfil Ceramic Primer cementing of the glass post surfaces with laser application. In Group 7, HF acid treatment was performed without laser. In Group 8, the laser was applied, followed by sanding of post surfaces using Korox 50, and silane coupling with Clearfil Ceramic Primer. In Group 9, the post surfaces were sanded using Korox 50 with laser application to the root canals. The samples were subjected to a push-out experiment. The data were analyzed using Friedman’s test and the Wilcoxon signed-rank test.
Results
A significant difference in bonding strength was found among the groups (p<0.005).
Conclusions
Use of an Er: YAG laser in the root canal may be beneficial prior to bonding of glass posts.
MeSH Keywords: Lasers, Solid-State; Photoacoustic Techniques; Post and Core Technique; Smear Layer
Background
Re-incorporation of teeth with previous endodontic treatment and excessive substance loss may be possible using posts inserted into the root canal, which assist retention of the restoration [1–3]. Debridement during root canal treatment is mandatory and is a major element of endodontic success [4–9]. Lasers can be used to produce dentin surfaces suitable for bonding of adhesive resin cement. An erbium-doped yttrium aluminum garnet (Er: YAG) laser can be used to cleanse, shape, and widen the root canal. In this regard, photon-induced photoacoustic streaming (PIPS), in conjunction with an Er: YAG laser, represents a revolutionary method to cleanse, disinfect, and shape the root canal system. PIPS obviates the need for excessive widening of the root canal, which can weaken the tooth structure. PIPS allows a minimally invasive procedure and protects the hard tooth tissues [10–14]. Glass-fiber post can be used to strengthen and lengthen the root. Prefabricated post and resin cement is a viable technique for weakened endodontically treated roots [15–18].
In the current study, the effect on the bonding strengths of glass-fiber posts with different surface treatments in post spaces roughened by an Er: YAG laser was examined. In addition, the bonding strengths of prefabricated glass-fiber posts exposed to surface treatments in teeth with excessive substance loss were compared, and the effect of laser treatment of the root canal surface on bond strength was investigated.
Material and Methods
In total, 90 single-rooted and single-canaled teeth freshly extracted due to a medical indication were used. Teeth with caries, fissures, restoration, dilacerations, or open apices were excluded. To standardize the root canal lengths, the corona was cut perpendicular to the long axis of the tooth using a diamond blade (ZumSeparieren, Germany) under water cooling to achieve a root length of 14 mm. The endodontic access cavities were prepared using a round drill (Horico, Berlin, Germany). Root canal preparation was carried out by the crown-down technique using an endo-motor (Endo Mate TC2, NSK, Japan) and Ni-Ti files (S1–S2–F1–F2, F3; ProTaper Universal, Dentsply DeTrey, Konstanz, Germany), so that the length of the examined portion was 0.5 mm shorter than the apical foramen. After each file change, the root canal was rinsed with physiological saline using an injector. The canal was cleansed with 0.5% NaOCl for 1 min and rinsed with distilled water.
All canals undergoing expansion were detracted using the drill of the post system (Snowfiber post-drill, size 1.0) with an interval of approximately 4 mm at the tooth apex, and a post space of 10 mm was prepared. The prepared root canals were assigned to the following 9 groups (n=10 each):
Group 1: A flexible fiber tip of 300 μm thickness was used to apply the Er: YAG laser (Fotona Laser AT Fidelis Plus III, Fotona DD, Ljubljana, Slovenia) to the root canals. In accordance with the manufacturer’s instructions, an energy level of 15 Hz/40 MJ was applied to the root surface at a wavelength of 2.940 μm. The output power of the laser was 0.6 W. The fiber tip was placed parallel to the surface in the coronal third of the root. NaOCl solution (0.5%) was introduced into the canal using an injector. The fiber tip (a special tip for R13 root canal irrigation) was applied to the root surface for 2–3 s without water-spraying or physical contact, and a 1-min interval was allowed. Then, the fiber tip was applied to the root surface for 30 s under a water spray. The canal was dried using a paper point. No surface treatment was performed on the glass-fiber post surface (Snowpost; Carbotech, Ganges, France).
Group 2: Prior to surface treatment, posts were transferred to 95% ethanol for 20 s, rinsed with water, and dried. Next, Al2O3 particles (CoJet; 3M ESPE, Seefeld, Germany) 30 μm in diameter were applied to the Snowpost surface at a pressure of 2.8 bars for 20 s. The Snowposts were covered with Al2O3 particles overspread with silica, and silane was applied to the post surface using a brush (ESPE Sil; 3M ESPE) and dried for 5 min. No laser was applied to the root surfaces.
Group 3: The laser was applied to the root canals as in Group 1, and Cojet was applied to the surface of the Snowposts as in Group 2.
Group 4: The laser was applied to the root canals as in Group 1, and Clearfil Ceramic Primer (Kuraray Medical, Okayama, Japan) was applied to the Snowpost surface and dried for 5 min.
Group 5: No laser was applied to the root canals, and Clearfil Ceramic Primer silane coupling was applied to the Snowpost surface as in Group 4.
Group 6: HF acid was applied to the Snowpost surface for 60 s, followed by neutralization by rinsing with distilled water and drying. After acid-etching with HF, Clearfil Ceramic Primer silane coupling was applied to the glass post surface and dried for 5 min. The laser was applied to the root canals as in Group 1.
Group 7: HF acid was applied to the post surface as in Group 6, and no laser was applied to the root canals.
Group 8: The laser was applied to the root canals as in Group 1. Post surfaces were sanded using Korox 50 (Bego, Germany) for 15 s at a pressure of 3 bars and a distance of 10 mm at Gaziantep Ata Dental Laboratory. Following cleansing with an air spray, Clearfil Ceramic Primer silane coupling was applied to the post surfaces.
Group 9: The post surfaces were sanded using Korox 50, and no laser was applied to the root canals.
In all groups, Clearfil SA (Kuraray Medical, Tokyo, Japan) cement was applied to post spaces using a special endodontic tip. Posts were calibrated using mild digital pressure, and were carefully placed in the post space, irrespective of the presence of surface treatment. Thus, excess cement was allowed to pour out. While the digital pressure was maintained, the resin cement was polymerized using a light-emitting diode (LED; L.E. Demetron I/Kerr Corporation, Orange, CA, USA) beam device for 40 s. The samples were incubated in distilled water at 37°C for 24 h.
Eight teeth per group were subjected to push-out bonding strength testing, and 2 teeth per group were stored for scanning electron microscopy analysis. Teeth were embedded in methacrylate resin molds. Six cross-sections were obtained from each acrylic block using a slow rotating cut-off machine (Minitom; Struers, Copenhagen, Denmark) under distilled water cooling, yielding a total of 48 cross-sections per group with an approximate thickness of 1 mm. The first 2 cross-sections were obtained from the coronal segment of the post space, the next 2 from the middle, and the last 2 from the apical segment.
Push-out tests at a rate of 0.5 mm/min in the apical to coronal direction were carried out using a universal testing device at Ankara University Faculty of Dentistry Laboratory (Lloyd LR 50K; Lloyd Instruments plc, Fareham, Hampshire, UK) (Figure 1). The maximum tensile strength was determined in newtons (N), converted to megapascals (MPa) after being divided by the surface area of the binding surface, and recorded.
Figure 1.

Execution of the push-out test.
The data were analyzed by the Friedman test and the Wilcoxon signed-rank test.
The Wilcoxon test was used to compare the differences in the average of the push-out test results after adhesion of the snow posts with different surface treatments applied to the root canal. In addition, the Friedman multiple comparison test was used to compare push-out values within the group.
Results
The results of push-out tests on Snowposts following various surface procedures differed significantly between the laser-treated and laser-untreated groups (p<0.01) (Tables 1, 2).
Table 1.
Average push-out bond strength value of laser treated groups p<0.05.
| Average value (mean) | Std. deviation | Std. error Mean | |
|---|---|---|---|
| Control groups | 113.000 | 3.98372 | 2.39801 |
| Lazer/Cojet | 109.9000 | 2.42143 | 2.39801 |
| Lazer/Silan | 133.3333 | 8.51136 | 4.91404 |
| Laser/HF | 122.3667 | 12.36136 | 7.13684 |
| Laser/Al2O3 | 128.3333 | 9.90269 | 5.71732 |
Table 2.
Average push-out bond strength value of non-laser treated groups p<0.05.
| Average value (mean) | Std. deviation | Std. error Mean | |
|---|---|---|---|
| Control groups | 113.000 | 3.98372 | 2.39801 |
| Cojet | 86.2000 | 4.63177 | 2.46937 |
| Silan | 107.7333 | 1.090351 | 1.09899 |
| HF | 98.2667 | 4.27707 | 2.40937 |
| Al2O3 | 105.000 | 8.02247 | 4.63177 |
The average retention values of the silane treated groups were 107.7333 N and the average retention values of the silane and laser-treated groups were 133.3333 N. The mean retention values of the HF-treated groups were 98.2667 N, and the mean retention values of the HF-treated and laser-treated groups were 122.3667 N. The mean retention values of the Al2O3 treated groups were 105.0000 N, and the mean retention values of Al2O3 and laser-treated groups were 128.3333 N. The mean retention values of CoJet treated groups were 86.2000 N, and the mean retention values of CoJet and laser-treated groups were 109.9000 N. (Tables 1, 2). According these values, the tensile strengths in the groups that received surface treatments alone were in the following order: silane >Al2O3 >HF >Cojet. In the groups that received both laser and surface treatments, the corresponding order was: laser/silane >laser/Al2O3 >laser/HF >laser/Cojet (Tables 1, 2). According the Wilcoxon test results, there was a positive correlation between the laser-treated groups and the control group (p<0.005) (Table 3).
Table 3.
Effects of laser surface treatment.
| Cojet-Laser/control group | Silane-Laser/control group | HF-Laser/control group | Al2O3-Laser/control group | |
|---|---|---|---|---|
| Z | 2.028* | 2.014* | 2.366* | 2.366* |
| p | 0.0043 | 0.001 | 0.018 | 0.018 |
Z – asymptotic significance;
positive order value p<0.005.
In samples treated with the laser, opening of the tubular orifices was observed. In addition, partial or complete removal of the smear layer and exposure of the collagen fibers masking the tubular orifice were seen. In some areas, melting carbonization was found. The dentin tubules were obstructed after fusion, while the hydroxyapatite matrix and collagen fibers were preserved (Figure 2).
Figure 2.
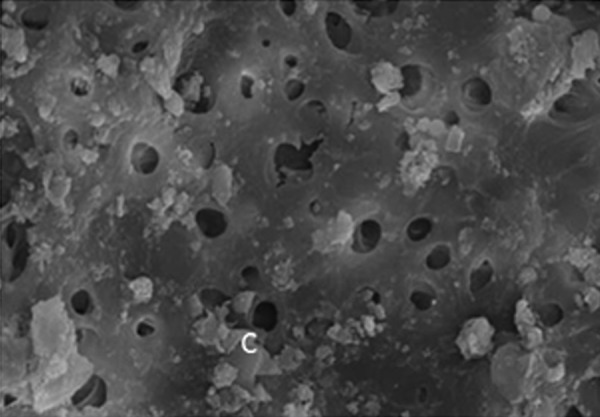
Scanning electron micrographs of root dentin surfaces after Er: YAG laser treatment.
Discussion
Laser treatment has been introduced to generate dentin surfaces appropriate for bonding of adhesive resin cement. Laser application results in the formation of roughened surfaces, potentially increasing the binding strength of adhesive restorations. Studies to date have reported the generation of a superficial smear layer using currently available root canal cleansing methods. In contrast, recent experience suggests that lasers enable the generation of surfaces with macromorphological variation without dentin demineralization and the opening of dentin tubules. Therefore, in this study, we used a laser to generate appropriate binding surfaces in the root canal dentin [19–23].
The special PIPS tip used in our study obviates the need for excessive widening of the root canal, which can weaken dental tissue. This property of PIPS tips allows a minimally invasive procedure and protects the dental tissues.
Takeda et al. reported that Er: YAG laser treatment removes the smear layer from both the middle and apical thirds of roots [24]. However, Kivanc et al. indicated that Er: YAG and Nd: YAG lasers had no effect on the debris and smear layers on root canal walls [25]. Inamoto et al. prepared root canals by applying 30 MJ of energy using an Er: YAG laser and observed no smear layer in the root canals, concluding that this method enhanced root canal preparation [26,27]. Visuril et al. reported good resin binding to dental tissues in laser treated samples, and that application of an Er: YAG laser to dentin yielded greater tensile strength than roughening [28]. Nasher et al. found no smear layer in root canals prepared using an Er: YAG laser, together with opening of dentin tubules and increased tensile strength [29]. Akyüz et al. also reported high tensile strength in samples activated using PIPS laser tips [30,31]. Following activation of the irrigation solutions by EndoActivator and an Er: YAG laser, removal of tissues and debris from the canal was enhanced [32,33]. It was seen that the results of the studies were in agreement with the results of our studies.
Our results showed that the Er: YAG group obtained the most efficient smear layer removal, in the end it scored the highest bond strength values compared to the control group (p<0.01). There was a positive correlation between the laser-treated groups and the control group (Table 3). Although the differences in mean bond strength values were statistically significant, this finding was still surprising. Few studies have examined the effect of PIPS using erbium lasers on FRC after bonding to root canal walls and we found this among tested groups. Laser-activated PIPS showed higher efficiency in increasing push-out bond strength of fiber posts.
We found that removal of the smear layer and opening of dentin tubules was enhanced using the Er: YAG laser. Application of the Er: YAG laser to the root canal dentin significantly increased its tensile strength (p<0.05). Thus, laser treatment resulted in increases in the tensile strength of dentin and the binding strength of Snowposts.
Conclusions
Use of an Er: YAG laser in dental root canal treatment facilitates disinfection, shaping, cleansing, and roughening (affecting bond strength of the root canal) of the canal. Laser application to the root surface increases the bonding strength of surface-treated prefabricated glass-fiber posts. However, few previous studies have assessed the utility of Er: YAG laser treatment of root dentin surfaces, and further research is required.
Footnotes
Conflicting interest
None.
Source of support: This work was supported by Research Fund of the Dicle University. Project Number: 11-DH-09
References
- 1.Cheung W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J Am Dent Assoc. 2005;136:611–19. doi: 10.14219/jada.archive.2005.0232. [DOI] [PubMed] [Google Scholar]
- 2.Boschian Pest L, Cavalli G, Bertani P, Gagliani M. Adhesive post-endodontic restorations with fiber posts: Push-out tests and SEM observations. Dent Mater. 2002;18:596–602. doi: 10.1016/s0109-5641(02)00003-9. [DOI] [PubMed] [Google Scholar]
- 3.Kececi AD, Ureyen Kaya B, Adanir N. Micro push-out bond strengths of four fiber-reinforced composite post systems and 2 luting materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:121–28. doi: 10.1016/j.tripleo.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Kaya S, Adıgüzel Ö, Ganidağlı Ayaz S. Effectiveness of three different application times of 17% EDTA and 7% maleic acid irrigation agents on the removal of debris and smear layer: A scanning electron microscope study. Int Dent Res. 2011;2:48–54. [Google Scholar]
- 5.Yiğit Özer S, Adıgüzel Ö, Kaya S. Removal of debris and smear layer in curved root canals using self-adjusting file with different operation times – A scanning electron microscope study. Int Dent Res. 2011;1:1–6. [Google Scholar]
- 6.Kaya S, Ayaz SG, Uysal İ, Akkuş Z. Comparison of the impact of long-term applications of MTAD and EDTA irrigation agents on dentin structure: A scanning electron microscope study. Int Dent Res. 2011;2:60–64. [Google Scholar]
- 7.Adiguzel O, Gokcen MG, Olcay AB. Evaluation of the effect of needle tilting angle on irrigant flow in the root canal using side-vented needle by an unsteady computational fluid dynamics model. Int Dent Res. 2016;6:1–8. [Google Scholar]
- 8.Kaya S. Smear-layer removal using two instrumentation and irrigation techniques in a closed system. Int Dent Res. 2012;2:60–66. [Google Scholar]
- 9.Adıgüzel Ö. A Literature review of self adjusting file. Int Dent Res. 2011;1:18–25. [Google Scholar]
- 10.Cekic-Nagas I, Sukuroglu E, Canay S. Does the surface treatment affect the bond strength of various fibre-post systems to resin-core materials? J Dent. 2011;39:171–79. doi: 10.1016/j.jdent.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Tuncdemir AR, Yildirim C, Guller F, et al. The effect of post surface treatments on the bond strength of fiber posts to root surfaces. Lasers Med Sci. 2013;28:13–18. doi: 10.1007/s10103-012-1053-z. [DOI] [PubMed] [Google Scholar]
- 12.Zhang S, Chen T, Ge LH. Scanning electron microscopy study of cavity preparation in deciduous teeth using the Er: YAG laser with different powers. Lasers Med Sci. 2012;27:141–44. doi: 10.1007/s10103-010-0854-1. [DOI] [PubMed] [Google Scholar]
- 13.DiVito E, Peters OA, Olivi G. Effectiveness of the erbium: YAG laser and new design radial and stripped tips in removing the smear layer after root canal instrumentation. Lasers Med Sci. 2012;27:273–80. doi: 10.1007/s10103-010-0858-x. [DOI] [PubMed] [Google Scholar]
- 14.Guneser MB, Arslan D, Usumez A. Tissue dissolution ability of sodium hypochlorite activated by photon-initiated photoacoustic streaming technique. J Endod. 2015;41:729–32. doi: 10.1016/j.joen.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Adıgüzel Ö, Kaya S, Yiğit Özer S, et al. Three-dimensional finite element analysis of endodontically treated tooth restored with carbon and titanium posts. Int Dent Res. 2011;2:55–59. [Google Scholar]
- 16.Agüloğlu S, Ayna E, Özdemir E. A fibre-reinforced fixed partial denture on a hemisectioned tooth: A case report. Int Dent Res. 2011;1:38–41. [Google Scholar]
- 17.Adıgüzel Ö, Yiğit Özer S, et al. Finite element analysis of endodontically treated tooth restored with different posts under thermal and mechanical loading. Int Dent Res. 2011;3:75–80. [Google Scholar]
- 18.Cangul S, Adiguzel O. The latest developments related to composite resins. Int Dent Res. 2017;7:32–41. [Google Scholar]
- 19.Grandini S, Goracci C, Tay FR, et al. Clinical evaluation of the use of fiber posts and direct resin restorations for endodontically treated teeth. Int J Prosthodont. 2005;18:399–404. [PubMed] [Google Scholar]
- 20.Paghdiwala AF, Vaidyanathan TK, Paghdiwala MF. Evaluation of erbium: YAG laser radiation of hard dental tissues: Analysis of temperature changes, depth of cuts and structural effects. Scanning Microsc. 1993;7:989–97. [PubMed] [Google Scholar]
- 21.Kimura Y, Yonaga K, Yokoyama K, et al. Root surface temperature increase during Er: YAG laser irradiation of root canals. J Endod. 2002;28:76–78. doi: 10.1097/00004770-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Arslan D, Guneser MB, Dincer AN, et al. Comparison of smear layer removal ability of QMix with different activation techniques. J Endod. 2016;42:1279–85. doi: 10.1016/j.joen.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 23.Kokuzawa C, Ebihara A, Watanabe S, et al. Shaping of the root canal using Er: YAG laser irradiation. Photomed Laser Surg. 2012;30:367–73. doi: 10.1089/pho.2012.3226. [DOI] [PubMed] [Google Scholar]
- 24.Takeda FH, Harashima T, Kimura Y, Matsumoto K. Comparative study about the removal of smear layer by three types of laser devices. J Clin Laser Med Surg. 1998;16:117–22. doi: 10.1089/clm.1998.16.117. [DOI] [PubMed] [Google Scholar]
- 25.Kivanc BH, Ulusoy OI, Gorgul G. Effects of Er: YAG laser and Nd: YAG laser treatment on the root canal dentin of human teeth: A SEM study. Lasers Med Sci. 2008;23:247–52. doi: 10.1007/s10103-007-0474-6. [DOI] [PubMed] [Google Scholar]
- 26.Inamoto K, Horiba N, Senda S, et al. Possibility of root canal preparation by Er: YAG laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e47–55. doi: 10.1016/j.tripleo.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Topcuoglu HS, Koseoglu M. Effect of Er: YAG and Nd: YAG lasers on the mineral content of root canal dentin. Lasers Med Sci. 2015;30:809–13. doi: 10.1007/s10103-013-1438-7. [DOI] [PubMed] [Google Scholar]
- 28.Visuri SR, Gilbert JL, Wright DD, et al. Shear strength of composite bonded to Er: YAG laser-prepared dentin. J Dent Res. 1996;75:599–605. doi: 10.1177/00220345960750011401. [DOI] [PubMed] [Google Scholar]
- 29.Nasher R, Franzen R, Gutknecht N. The effectiveness of the Erbium: Yttrium aluminum garnet PIPS technique in comparison to different chemical solutions in removing the endodontic smear layer-an in vitro profilometric study. Lasers Med Sci. 2016;31:1871–82. doi: 10.1007/s10103-016-2063-z. [DOI] [PubMed] [Google Scholar]
- 30.Akyuz Ekim SN, Erdemir A. Comparison of different irrigation activation techniques on smear layer removal: An in vitro study. Microsc Res Tech. 2015;78:230–39. doi: 10.1002/jemt.22466. [DOI] [PubMed] [Google Scholar]
- 31.Akyuz Ekim SN, Erdemir A. Effect of different irrigant activation protocols on push-out bond strength. Lasers Med Sci. 2015;30:2143–49. doi: 10.1007/s10103-015-1772-z. [DOI] [PubMed] [Google Scholar]
- 32.Conde AJ, Estevez R, Lorono G, et al. Effect of sonic and ultrasonic activation on organic tissue dissolution from simulated grooves in root canals using sodium hypochlorite and EDTA. Int Endod J. 2016;50:976–82. doi: 10.1111/iej.12717. [DOI] [PubMed] [Google Scholar]
- 33.Kalkan M, Usumez A, Ozturk AN, et al. Bond strength between root dentin and three glass-fiber post systems. J Prosthet Dent. 2006;96:41–46. doi: 10.1016/j.prosdent.2006.05.005. [DOI] [PubMed] [Google Scholar]


