Abstract
IMPORTANCE
Previous studies using data from the 1980s found relatively little geographic variation in cataract surgery rates across the United States. We do not know whether similar patterns hold true today, nor do we know the patient- and community-level factors that might explain any recent geographic variations in the rate and timing of cataract surgery.
OBJECTIVE
To assess the extent of geographic variation in patient age at initial cataract surgery and the age-standardized cataract surgery rate in a large group of insured US patients with cataracts.
DESIGN, SETTING, AND PARTICIPANTS
Retrospective cross-sectional study of 1 050 815 beneficiaries older than 40 years of age with cataracts who were enrolled in a nationwide managed-care network during the period from 2001 to 2011. The data analysis was started in 2014 and refined in 2015.
MAIN OUTCOMES AND MEASURES
Median age at initial cataract extraction, age-standardized cataract surgery rate, and time from initial diagnosis to first surgery for patients with cataracts were compared among 306 US communities. Multivariable regression modeling generated hazard ratios (HRs) with 95% CIs identifying factors associated with patients’ likelihood of undergoing cataract surgery.
RESULTS
A total of 243 104 patients with cataracts (23.1%) underwent 1 or more surgical procedures (55.1% were female patients). Communities with the youngest and oldest patients at initial surgery differed in age by nearly 20 years (59.9–60.1 years in Lansing, Michigan, and Aurora, Illinois, vs 77.0–79.6 years in Marquette, Michigan; Rochester, New York; and Binghamton, New York). The highest age-standardized cataract surgery rate (37.3% in Lake Charles, Louisiana) was 5-fold higher than the lowest (7.5% in Honolulu, Hawaii). The median time from initial cataract diagnosis to date of first surgery ranged from 17 days (Victoria, Texas) to 367 days (Yakima, Washington). Compared with white patients, black patients had a 15% decreased hazard of surgery (HR, 0.85 [95% CI, 0.83–0.87]), while Latino patients (HR, 1.08 [95% CI, 1.05–1.10]) and Asian patients (HR, 1.09 [95% CI, 1.05–1.12]) had an increased hazard. For every 1° higher latitude, the hazard of surgery decreased by 1% (HR, 0.99 [95% CI, 0.98–0.99]). For every additional optometrist per 100 000 enrollees in a community, the hazard of surgery increased 0.1% (HR, 1.001 [95% CI, 1.001-1.001]).
CONCLUSIONS AND RELEVANCE
In recent years, patient age at first cataract surgery and the age-standardized surgery rate have varied considerably among some US communities. Future research should explore the extent to which such variations may affect patient outcomes.
Cataract is a leading cause of visual impairment, affecting more than 24 million Americans.1 With the aging of the US population, this number is projected to increase to 38.7 million by 2030.2 The rate of cataract surgery has also increased over the past several decades. From 1980 to 2003, the cataract surgery rate for Medicare beneficiaries increased from 13.4 to 61.8 persons per 1000 person-years.3
Using Medicare claims data from the late 1980s, Javitt and colleagues4 found that cataract surgery rates in US communities varied relatively little compared with other surgical procedures. In addition to identifying communities with disproportionately high and low surgery rates, they ascertained several variables associated with communities’ cataract surgery rate, including patient age, sex, race, latitude, density of optometrists, and allowed cataract surgery charge. Other variables, including density of practicing ophthalmologists, were not statistically significant.
Approximately 20 years after Javitt and colleagues’ seminal work,4 we revisit geographic variation in cataract surgery rates among US communities using 2001–2011 data from a large managed-care network. We assess whether communities with relatively low and high surgery rates in the earlier study4 continue to show similar patterns. Moreover, we assess variation in the time from first cataract diagnosis to surgery and evaluate whether factors affecting cataract surgery rates years ago remain important now.
Methods
Data Source
The Clinformatics DataMart database (OptumInsight) has deidentified records of all beneficiaries in a nationwide managed-care network. We had access to data for all eye care recipients during the period from 2001 to 2011. Beneficiaries were included in the data set if they had 1 or more International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for any eye-related diagnosis (ICD-9-CM codes 360–379.9); a Current Procedural Terminology (CPT) code for any eye-related visits or for diagnostic or therapeutic procedures (CPT codes 65091–68899 or CPT codes 92002–92499); or any other ophthalmologist- or optometrist-submitted claim during their time in the plan. The data contain all of beneficiaries’ medical claims for ocular and nonocular conditions and their sociodemographic information (age, sex, race, education, and income); they have been used in other ocular disease–related studies.5–7 The University of Michigan institutional review board approved our study as a nonregulated study. Informed consent was not obtained because the data were deidentified.
Sample Selection
We identified all persons older than 40 years of age who had 1 or more diagnoses of cataract (ICD-9-CM codes 366, 366.0-04, 366.09, 366.1x, 366.41, and 366.45) during their time in the plan. Prior work comparing billing records with medical records found that billing records accurately capture persons with cataracts.8
Identification of Cataract Surgery Recipients
Cataract surgery recipients were identified based on the following CPT codes: 66830, 66840, 66850, 66852, 66920, 66930, 66940, and 66982-4. Validation studies have demonstrated that billing records accurately capture receipt of cataract surgery.9 Enrollees who were documented to be pseudophakic or aphakic (ICD-9-CM codes V43.1, 379.3, and 379.31) prior to their first cataract surgery were excluded because they must have undergone surgery in the contralateral eye prior to entry into the plan.
Geographic Areas
We divided the United States into 306 hospital referral regions (HRRs) representing regional health care markets for tertiary medical care,10 according to methods described in The Dartmouth Atlas of Health Care.11 Hospital referral regions have been used extensively to study geographic variation in medical service utilization.12,13 Each enrollee was assigned to a given HRR based on his or her residential zip code.
Analyses
Statistical analyses were performed using SAS, version 9.3 (SAS Institute Inc). Participants’ characteristics were summarized for the entire sample using mean values and standard deviations (SDs) for continuous variables and frequencies and percentages for categorical variables.
In each HRR, we determined the median age of enrollees who had received a diagnosis of cataract, and were thus eligible for surgery, and the median age at first cataract surgery among surgery recipients. To account for differences among HRRs in the ages of persons eligible for cataract extraction, we calculated age-standardized cataract surgery rates by HRR using an indirect standardization technique.14
To assess variation in age at first cataract surgery within a given HRR, we computed the SD for the age of all the cataract surgery recipients in each HRR and then compared the SDs across HRRs. Next, we assessed timing from the first-recorded cataract diagnosis to the date of first extraction. To do this, we determined the median number of days between the time of first diagnosis and first surgery for enrollees residing in each HRR. We compared the timing from first cataract diagnosis by any eye care professional (ophthalmologist or optometrist) to that of cataract surgery among the HRRs. We also assessed the timing from first cataract diagnosis by the same ophthalmologist who performed the surgery and compared the median timing from first diagnosis to surgery among the HRRs.
Factors Affecting Receipt of Cataract Surgery
Hierarchical Cox regression modeling was performed to identify community- and patient-level variables affecting receipt of cataract surgery. The community-level variables considered in the model were supply of ophthalmologists and optometrists,15 average cost of living,16 number of days of sunshine annually,16 latitude,16 longitude,16 UV index,16 proximity to an ophthalmology residency program, median charge, and proportion of persons in the HRR who drive to work.16 Patient-level variables included race, sex, income, educational level, urban/rural status of residence, common medical and ocular comorbidities, and the Charlson Comorbidity Index,17 which is a measure of overall health. The best subset selection method identified which covariates to include in the model. The regression models generated hazard ratios (HRs) with 95% CIs. For all analyses, P < .05 was considered statistically significant.
Results
Of the 1 050 815 eligible enrollees who received a diagnosis of cataracts, 243 104 (23.1%) underwent cataract surgery in 1 or 2 eyes during their time in the plan. The mean (SD) duration in the plan of all eligible enrollees was 1539 (977) days; 238 242 enrollees (98.0%) were followed up for 6 months or more while in the plan. Among cataract surgery recipients, the mean (SD) time from plan enrollment to first cataract surgery was 933 (814) days. A higher proportion of men with cataracts than women with cataracts underwent surgery (109 106 of 460 615 men [23.7%] vs 133 998 of 590 200 women [22.7%]; P < .001). The proportions of white, black, Latino, and Asian patients who underwent surgery were 24.4% (176 518 of 723 262), 21.2% (11 816 of 55 624), 22.2% (10 321 of 46 414), and 19.5% (4284 of 21 966), respectively (P < .001). Among all eligible enrollees (except those with missing data in their records), 202 794 of 900233 enrollees (22.5%) had at least a college diploma, and 166 802 of 862 970 enrollees (19.3%) had an income of $100 000 or more (Table 1). The mean and median number of eligible patients with cataracts in a given HRR was 3434 and 1312, respectively (range, 61–68 872 patients). The mean and median number of patients undergoing surgery in an HRR were 795 and 307, respectively (range, 21–16 259 patients).
Table 1.
Sociodemographic Characteristics of Enrollees With Cataracts and Those Who Underwent Cataract Surgery
| Characteristic | Patients With Cataracts, No. (%) | P Value | ||
|---|---|---|---|---|
| Who Did Not Undergo Surgery |
Who Underwent Surgery |
All | ||
| Total | 807 711 (76.9) | 243 104 (23.1) | 1 050 815 (100.0) | |
| Race (n = 196 131a) | ||||
| White | 546 744 (84.1) | 176 518 (86.3) | 723 262 (84.6) | <.001b |
| Black | 43 808 (6.7) | 11 816 (5.8) | 55 624 (6.5) | |
| Latino | 36 093 (5.6) | 10 321 (5.0) | 46 414 (5.4) | |
| Asian | 17 682 (2.7) | 4284 (2.1) | 21 966 (2.6) | |
| Other | 5779 (0.9) | 1639 (0.8) | 7418 (0.9) | |
| Sex | ||||
| Male | 351 509 (43.5) | 109 106 (44.9) | 460 615 (43.8) | <.001b |
| Female | 456 202 (56.5) | 133 998 (55.1) | 590 200 (56.2) | |
| Education (n = 151 223a) | ||||
| <High school | 10 417 (1.5) | 3370 (1.6) | 13 787 (1.5) | <.001b |
| High school diploma | 253 961 (37.1) | 86 452 (40.1) | 340 413 (37.8) | |
| Some college | 260 333 (38.0) | 82 906 (38.5) | 343 239 (38.1) | |
| College diploma | 158 228 (23.1) | 42 408 (19.7) | 200 636 (22.3) | |
| Advanced degree | 1784 (0.3) | 374 (0.2) | 2158 (0.2) | |
| Income, $ (n = 188 518a) | ||||
| <30 000 | 79 956 (12.2) | 32 314 (15.7) | 112 270 (13.0) | <.001b |
| 30 000 to <60 000 | 238 263 (36.3) | 81 778 (39.6) | 320 041 (37.1) | |
| 60 000 to <100 000 | 204 497 (31.1) | 59 360 (28.8) | 263 857 (30.6) | |
| 100 000 to <125 000 | 69 895 (10.6) | 17 987 (8.7) | 87 882 (10.2) | |
| ≥125 000 | 63 905 (9.7) | 15 015 (7.3) | 78 920 (9.1) | |
| Diabetesc | ||||
| None | 561 117 (69.5) | 161 282 (66.3) | 722 399 (68.7) | <.001b |
| Uncomplicated | 148 861 (18.4) | 44 551 (18.3) | 193 412 (18.4) | |
| Complicated | 97 733 (12.1) | 37 271 (15.3) | 135 004 (12.8) | |
| Age at enrollment, y | ||||
| Mean (SD) | 61.45 (9.95) | 65.39 (10.85) | 62.36 (10.30) | <.001d |
| Median | 61.00 | 65.20 | 62.00 | |
| Time in the plan, d | ||||
| Mean (SD) | 1487.53 (971.89) | 1710.47 (975.57) | 1539.10 (977.28) | <.001d |
| Median | 1280 | 1675 | 1430 | |
| Time from enrollment to first surgery, d | ||||
| Mean (SD) | NA | 932.58 (814.14) | NA | |
| Median | NA | 702 | NA | |
Abbreviation: NA, not applicable.
Number of patients with missing data in records for the given variables.
Determined by use of the χ2 test.
Uncomplicated diabetes refers to diabetes with no record of end-organ damage from this condition. Complicated diabetes refers to diabetes with a record of end-organ damage (eg, nephropathy).
Determined by use of the 2-sample t test.
Median Age of Patients at First Cataract Surgery
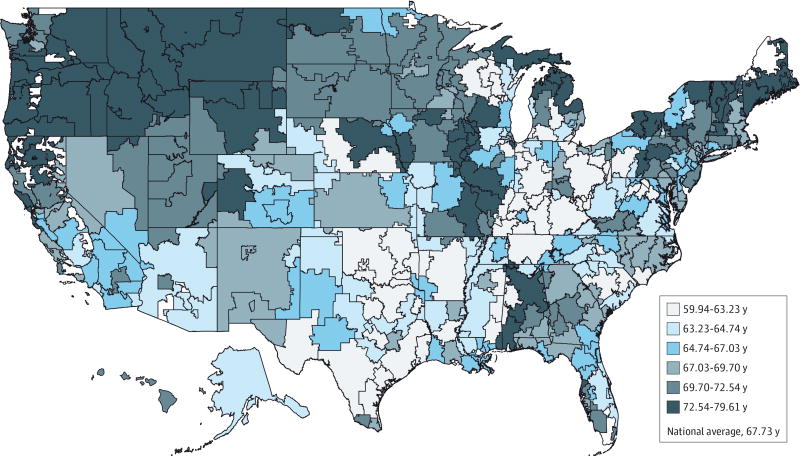
The overall median age of patients at first cataract surgery was 67.7 years. The median age of patients at first cataract surgery was youngest among residents of Lansing, Michigan; Aurora, Illinois; and Lafayette, Indiana (range, 59.9–61.0 years), and was oldest among residents of Marquette, Michigan; Rochester, New York; and Binghamton, New York (range, 77.0–79.6 years) (Figure 1; Table 2; Table 3).
Figure 1. Geographic Variation in the Median Age of Patients at Initial Cataract Surgery Throughout the United States.
Communities with a younger median age of patients at initial cataract surgery are shaded lighter in color, while those an older median age of patients at initial cataract surgery are shaded with darker colors.
Table 2.
Top 10 Communities With the Highest Values in Timing and Rate of Cataract Surgery
| Parameter and HRR | Value | Patients, No. | |
|---|---|---|---|
| Total | Surgery | ||
| Age of patients at initial cataract surgery, median, y | |||
| Binghamton, NY | 79.61 | 503 | 176 |
| Rochester, NY | 78.42 | 1070 | 306 |
| Marquette, MI | 77.02 | 88 | 22 |
| Lebanon, NH | 77.00 | 272 | 62 |
| San Francisco, CA | 76.76 | 2940 | 840 |
| Iowa City, IA | 76.54 | 1013 | 192 |
| Springfield, IL | 76.42 | 1332 | 532 |
| Great Falls, MT | 76.23 | 178 | 66 |
| Medford, OR | 76.20 | 723 | 276 |
| Yakima, WA | 75.77 | 325 | 100 |
| Age of patient at initial cataract surgery, SD, y | |||
| Bloomington, IL | 12.74 | 106 | 33 |
| Santa Cruz, CA | 12.74 | 272 | 60 |
| Flint, MI | 12.58 | 145 | 40 |
| Altoona, PA | 12.51 | 111 | 35 |
| Marquette, MI | 12.42 | 88 | 22 |
| Bangor, ME | 12.31 | 279 | 60 |
| Alameda County, CA | 12.11 | 1506 | 269 |
| Minneapolis, MN | 12.10 | 34 643 | 9592 |
| Duluth, MN | 12.08 | 3965 | 793 |
| Santa Barbara, CA | 11.96 | 324 | 58 |
| Age-standardized cataract surgery ratea | |||
| Lake Charles, LA | 0.373 | 1617 | 547 |
| Indianapolis, IN | 0.338 | 3895 | 1211 |
| Billings, MT | 0.326 | 827 | 317 |
| Springfield, IL | 0.325 | 1332 | 532 |
| Colorado Springs, CO | 0.322 | 2787 | 863 |
| Denver, CO | 0.316 | 11 755 | 3428 |
| Gary, IN | 0.313 | 1165 | 318 |
| Mesa, AZ | 0.311 | 5460 | 1538 |
| Topeka, KS | 0.310 | 397 | 119 |
| Reno, NV | 0.308 | 1015 | 303 |
| Time from cataract diagnosis to cataract surgery,b median, d | |||
| Yakima, WA | 367 | 325 | 100 |
| Mason City, IA | 278 | 300 | 55 |
| San Francisco, CA | 232 | 2940 | 840 |
| Springfield, IL | 218 | 1332 | 532 |
| San Mateo County, CA | 188 | 2201 | 529 |
| Traverse City, MI | 174 | 124 | 25 |
| Sayre, PA | 174 | 372 | 106 |
| Olympia, WA | 167.5 | 503 | 154 |
| Minot, ND | 159 | 61 | 21 |
| Medford, OR | 152 | 723 | 276 |
| Time from cataract diagnosis to cataract surgery by same physician,c median, d | |||
| San Francisco, CA | 90 | 2940 | 840 |
| San Mateo County, CA | 78 | 2201 | 529 |
| Burlington, VT | 69 | 289 | 56 |
| Lebanon, NH | 67 | 272 | 62 |
| Hartford, CT | 64 | 4537 | 836 |
| Manchester, NH | 61 | 1406 | 302 |
| Worcester, MA | 61 | 975 | 206 |
| Springfield, MA | 60 | 1090 | 206 |
| Ridgewood, NJ | 58 | 1563 | 263 |
| Newport News, VA | 58 | 967 | 159 |
| Portland, OR | 57.5 | 4447 | 1283 |
Abbreviation: HRR, hospital referral region.
The HRR was omitted if there were less than 20 patients in any age group (40–49, 50–59, 60–69, 70–79, or ≥80 years).
Length of time between first diagnosis of cataract by any eye care professional (ophthalmologist or optometrist) and surgery.
Length of time between first diagnosis of cataract (by the same ophthalmologist who performed the surgery) and surgery.
Table 3.
Top 10 Communities With the Lowest Values in Timing and Rate of Cataract Surgery
| Parameter and HRR | Value | Patients, No. | |
|---|---|---|---|
| Total | Surgery | ||
| Age of patients at initial cataract surgery, median, y | |||
| Lansing, MI | 59.94 | 1907 | 502 |
| Aurora, IL | 60.12 | 316 | 66 |
| Lafayette, IN | 60.97 | 464 | 163 |
| Lawton, OK | 61.51 | 98 | 29 |
| Tuscaloosa, AL | 61.57 | 206 | 47 |
| Florence, SC | 61.59 | 313 | 67 |
| Gary, IN | 61.70 | 1165 | 318 |
| Odessa, TX | 61.88 | 437 | 115 |
| Lexington, KY | 61.92 | 2740 | 597 |
| Columbus, OH | 62.04 | 22 278 | 4407 |
| Age of patient at initial cataract surgery, SD, y | |||
| Lawton, OK | 6.43 | 98 | 29 |
| Yakima, WA | 7.20 | 325 | 100 |
| Victoria, TX | 7.21 | 200 | 90 |
| Petoskey, MI | 7.66 | 143 | 47 |
| Binghamton, NY | 7.84 | 503 | 176 |
| Hattiesburg, MS | 7.92 | 1684 | 374 |
| Great Falls, MT | 7.92 | 178 | 66 |
| Albany, GA | 8.13 | 1338 | 337 |
| Muncie, IN | 8.20 | 133 | 46 |
| Meridian, MS | 8.31 | 663 | 136 |
| Age-standardized cataract surgery ratea | |||
| Honolulu, HI | 0.075 | 2651 | 226 |
| Salisbury, MD | 0.138 | 1440 | 187 |
| White Plains, NY | 0.145 | 3172 | 438 |
| East Long Island, NY | 0.153 | 16 705 | 2417 |
| Manhattan, NY | 0.160 | 11 778 | 1876 |
| Syracuse, NY | 0.162 | 2629 | 408 |
| Elmira, NY | 0.162 | 560 | 85 |
| Hackensack, NJ | 0.163 | 4811 | 751 |
| Providence, RI | 0.166 | 26 013 | 4634 |
| Harlingen, TX | 0.167 | 502 | 77 |
| Time from cataract diagnosis to cataract surgery,b median, d | |||
| Victoria, TX | 16.5 | 200 | 90 |
| Hattiesburg, MS | 20 | 1684 | 374 |
| Oxford, MS | 20.5 | 111 | 30 |
| Lawton, OK | 22 | 98 | 29 |
| Lafayette, IN | 23 | 464 | 163 |
| Flint, MI | 23 | 145 | 40 |
| Muncie, IN | 24 | 133 | 46 |
| Miami, FL | 24 | 19 925 | 5066 |
| Altoona, PA | 24 | 111 | 35 |
| Dothan, AL | 24.5 | 747 | 170 |
| Time from cataract diagnosis to cataract surgery by same physician,c median, d | |||
| Muncie, IN | 14 | 133 | 46 |
| Dothan, AL | 15 | 747 | 170 |
| Abilene, TX | 17 | 245 | 67 |
| Jackson, TN | 17 | 490 | 126 |
| Tuscaloosa, AL | 18 | 206 | 47 |
| Flint, MI | 18 | 145 | 40 |
| Minot, ND | 18 | 61 | 21 |
| Idaho Falls, ID | 18.5 | 233 | 101 |
| Fort Myers, FL | 19 | 10 252 | 3127 |
| Springdale, AR | 19 | 1125 | 237 |
| Fort Smith, AR | 19 | 787 | 182 |
Abbreviation: HRR, hospital referral region.
The HRR was omitted if there were less than 20 patients in any age group (40–49, 50–59, 60–69, 70–79, or ≥80 years).
Length of time between first diagnosis of cataract by any eye care professional (ophthalmologist or optometrist) and surgery.
Length of time between first diagnosis of cataract (by the same ophthalmologist who performed the surgery) and surgery.
Variation in Age of Patients at First Cataract Surgery
Communities with the highest variation in median age of patients at first cataract surgery (ie, there is a wide age range from younger to older beneficiaries undergoing surgery within the community) include Bloomington, Illinois; Santa Cruz, California; Flint, Michigan; Altoona, Pennsylvania; and Marquette, Michigan. In these communities, the variation in median age of patients at first cataract surgery ranged from 12.4 to 12.7 years. By comparison, communities with the lowest variation include Lawton, Oklahoma; Yakima, Washington; Victoria, Texas; Petoskey, Michigan; and Binghamton, New York, where the dispersion in age of surgery recipients was 6.4 to 7.8 years (eFigure 1 in the Supplement; Tables 2 and 3). eFigure 2 in the Supplement shows a distribution of the median age of patients at initial cataract surgery for all the communities, stratified by urban/rural status, along with error bars capturing the variability in the point estimates.
Age-Standardized Cataract Surgery Rates
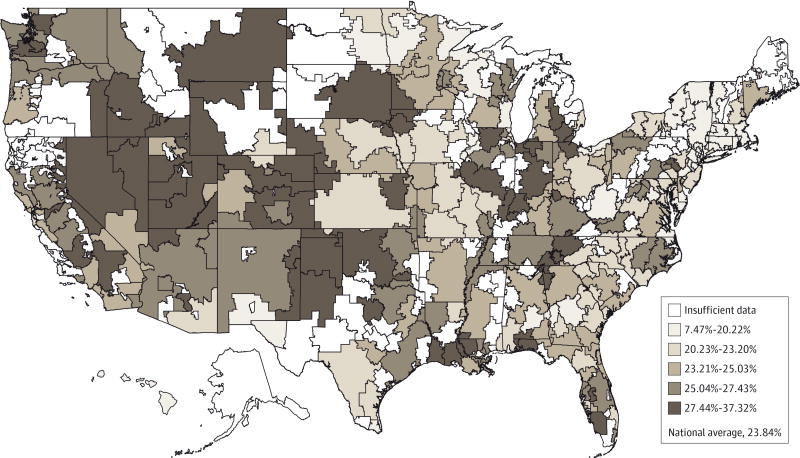
After excluding 82 of the 306 HRRs with limited numbers of enrollees to adequately perform the age-standardization procedure to account for differences in the average age of patients at the first diagnosis of cataract among the various HRRs, we observe a nearly 5-fold difference in the cataract surgery rate between the HRRs with the lowest and the HRRs with the highest age-standardized cataract surgery rates (7.5% in Honolulu, Hawaii, vs 37.3% in Lake Charles, Louisiana). Of the 10 HRRs with the highest age-standardized cataract surgery rates, 2 were in Indiana (Indianapolis, 33.8%; Gary, 31.3%), and 2 were in Colorado (Denver, 31.6%; Colorado Springs, 32.2%). Six of the 10 HRRs with the lowest age-standardized rates were in New York or northern New Jersey (Figure 2; Tables 2 and 3).
Figure 2. Geographic Variation in the Age-Standardized Cataract Surgery Rate Throughout the United States.
Communities with a lower age-standardized rate of initial cataract surgery are shaded lighter in color, while those a higher age-standardized rate of initial cataract surgery are shaded with darker colors.
Timing From Diagnosis to Surgery
Communities with the longest median time from initial cataract diagnosis to first surgery include Yakima, Washington (367 days); Mason City, Iowa (278 days); and San Francisco, California (232 days). By comparison, those with the shortest time include Victoria, Texas (17 days); Hattiesburg, Mississippi (20 days); and Oxford, Mississippi (21 days) (Tables 2 and 3).
Communities with the highest median number of days between initial diagnosis and surgery by the same ophthalmologist include San Francisco, California (90 days); San Mateo County, California (78 days); and Burlington, Vermont (69 days), while the communities with the lowest median number of days include Muncie, Indiana (14 days); Dothan, Alabama (15 days); Abilene, Texas (17 days); and Jackson, Tennessee (17 days) (eFigure 3 in the Supplement; Tables 2 and 3).
Factors Associated With Cataract Surgery
After adjusting potential confounders, we found that for every additional year of patient age at initial cataract diagnosis, the hazard for surgery increased by 2.5% (adjusted HR, 1.02 [95% CI, 1.02–1.03]). Compared with white patients, black patients had a 15% decreased hazard for surgery (adjusted HR, 0.85 [95% CI, 0.83–0.87]), whereas Asian patients (adjusted HR, 1.09 [95% CI, 1.05–1.12]) and Latino patients (adjusted HR, 1.08 [95% CI, 1.05–1.10]) had an increased hazard for surgery. Beneficiaries earning less than $30000 had an elevated hazard for cataract surgery, relative to those with incomes of $60000 or more (P < .001 for all comparisons), and the higher one’s income level, the lower the hazard for surgery. Compared with the least-educated patient group, all other patients had a lower likelihood of surgery (P < .001 for all comparisons).
For every 1° increase in latitude, the likelihood of cataract surgery decreased by 1% (adjusted HR, 0.99 [95% CI, 0.98–0.99]). For example, the hazard for cataract extraction was 20% lower in Portland, Oregon (45° latitude), than in Miami, Florida (25° latitude). Persons residing in rural communities had a 5% to 7% increased hazard of surgery compared with those living in urban locales (P < .001). For every additional optometrist in the community per 100000 enrollees, the hazard increased by 0.1% (adjusted HR, 1.001 [95% CI, 1.001-1.001]). Persons with ocular trauma had a 30% increased hazard for surgery. Patients with diabetes (uncomplicated or involving end-organ damage) had a lower hazard for surgery than did patients without diabetes (P < .001). The hazard for surgery was 60% decreased in communities with higher, vs lower, overall practice expenses for medical care (adjusted HR, 0.40 [95% CI, 0.38–0.43]) (Table 4).
Table 4.
Cox Proportional Hazards Model Estimating the Hazard of Cataract Surgerya
| Covariate | HR (95% CI) | P Value |
|---|---|---|
| Race | ||
| White | 1 [Reference] | |
| Black | 0.85 (0.83–0.87) | <.001 |
| Latino | 1.08 (1.05–1.10) | <.001 |
| Asian | 1.09 (1.05–1.12) | <.001 |
| Other | 1.04 (0.99–1.10) | .01 |
| Income, $ | ||
| <30 000 | 1 [Reference] | |
| 30 000 to <60 000 | 0.99 (0.98–1.01) | .35 |
| 60 000 to <100 000 | 0.94 (0.93–0.96) | <.001 |
| 100 000 to <125 000 | 0.90 (0.88–0.92) | <.001 |
| ≥125 000 | 0.84 (0.82–0.87) | <.001 |
| Education | ||
| <High school | 1 [Reference] | |
| High school diploma | 0.91 (0.88–0.95) | <.001 |
| Some college | 0.83 (0.80–0.86) | <.001 |
| College diploma | 0.76 (0.73–0.79) | <.001 |
| Advanced degree | 0.69 (0.61–0.78) | <.001 |
| Diabetesb | ||
| None | 1 [Reference] | |
| Uncomplicated | 0.94 (0.93–0.95) | <.001 |
| Complicated | 0.95 (0.93–0.96) | <.001 |
| Urban vs rural status | ||
| Urban | 1 [Reference] | |
| Large rural | 1.07 (1.05–1.09) | <.001 |
| Small rural | 1.05 (1.03–1.07) | <.001 |
| Age at cataract diagnosis | 1.02 (1.02–1.03) | <.001 |
| Eye trauma | 1.30 (1.26–1.34) | <.001 |
| Charlson Comorbidity index | 1.01 (1.01-1.01) | <.001 |
| Latitude | 0.99 (0.98–0.99) | <.001 |
| PE GPCI | 0.40 (0.38–0.43) | <.001 |
| Average time in plan | 1.00 (1.00-1.00) | <.001 |
| No. of optometrists per 100 000 population | 1.00 (1.00-1.00) | <.001 |
Abbreviations: ACGME, Accreditation Counsel for Graduate Medical Education; HR, hazard ratio; PE PGCI, Practice Expense–Geographic Practice Cost Index.
Community-level covariates that were considered but not selected as part of the best subset include cost of living index, number of ophthalmologists per 100 000 population, number of physicians per 100 000 population, proportion of population driving to work, longitude, median total charges per patient, number of days of sunshine, UV index, and ACGME Ophthalmology Residency. Patient-level covariates that were considered but not selected as part of the best subset include sex, dementia, and depression.
Uncomplicated diabetes refers to diabetes with no record of end-organ damage from this condition. Complicated diabetes refers to diabetes with a record of end-organ damage (eg, nephropathy).
Discussion
In this large analysis of insured US patients with cataracts, we find substantial variation across communities in the median age of patients at first cataract surgery and in the age-standardized cataract surgery rate. The median age of patients at initial cataract surgery was as young as 60 years in some communities but approached 80 years in others. Furthermore, the age-standardized cataract surgery rate varied considerably among communities—notably, from 7.5% in Honolulu, Hawaii, to 37.3% in Lake Charles, Louisiana.
In addition to Javitt and colleagues’ US-based analysis,4 the literature contains studies of within-country geographic variation in cataract surgery in England and Canada, where considerable variation was documented.18,19 Although these analyses and our analysis had different study designs and insurance types, making direct comparison difficult, all 4 studies identified substantial differences in communities between the lowest and highest surgery rates. Javitt and coworkers4 found many communities with similar cataract surgery rates but observed an 11-fold difference between the communities with the lowest (Billings, Montana) and the communities with highest (Lake Charles, Louisiana) rate. Likewise, we find a 5-fold difference between the lowest (Honolulu, Hawaii) and highest (Lake Charles, Louisiana) age-standardized cataract surgery rates. Of interest, Lake Charles, Louisiana, had the country’s highest cataract surgery rate in both studies despite the studies’ use of different data sources (commercial insurance plan vs Medicare) and an approximately 20-year difference in observation periods. Although it is unclear why this particular community has such high surgery rates, possible reasons include patient-related factors (eg, increased patient motivation for surgery), health care professional–related factors (eg, differences in health care professionals’ aggressiveness in recommending surgery), or factors specific to that particular community (eg, environmental exposures). Lake Charles is a major center for petrochemical refining, and chronic exposure to naphthalene and other pollutants involved in the refinery process increase the risk for cataracts.20 In contrast, Billings, Montana, which had the lowest surgery rate in the study by Javitt and colleagues,4 is among the top 10 communities with the highest age-standardized cataract surgery rates in our analysis.
We are unaware of other studies comparing age at initial cataract surgery among persons residing in different communities throughout the United States. While our analysis identified large variations in the timing of first cataract surgery, more work is required to understand the factors contributing to the large differences in timing observed. Communities differ with respect to the characteristics of the patients residing in them, eye care professional availability, how assertive the ophthalmologists are at recommending surgery, and different environmental and lifestyle factors that can affect the timing of surgery. Visual demands may also vary among persons residing in one community vs another. For example, some communities have better public transportation systems, so there may be less of a need to see well enough to operate a motor vehicle to drive to work.
Factors Associated With Cataract Surgery
Age
Our study and the study by Javitt and colleagues4 indicate an increased likelihood of cataract surgery among older patients. Studies have shown that lens opacities of all types are more likely to be present in older persons. This is attributable to the natural aging process. Increased cataract density has a greater effect on visual acuity and quality of life, and this effect is likely influencing the decision for surgery.21–25 In addition, as patients age, the majority of them have spouses or acquaintances who have undergone successful cataract surgery, which may factor into their decision-making process.
Race
Our finding of a reduced likelihood for cataract surgery among black patients, as was noted 2 decades ago, indicates that racial disparities persist. While it is known that racial inequities exist in the proportions of patients carrying health insurance and that this affects utilization,26,27 in both our analysis and that of Javitt and coworkers,4 all the eligible patients had health insurance; thus, at least theoretically, everyone had access to eye care services. Possible explanations for black patients’ decreased hazard for surgery include racial differences in the type of lens opacification present by race,28 reduced health care resource use,3,29 and less awareness of the potential benefits of cataract surgery.30 In focus groups of older black patients and eye care professionals, the most frequently cited barrier to care was the lack of transportation and accessibility to ophthalmologists’ offices for the surgery and postoperative care.31 Other barriers to surgery for black patients may include issues with trust and communication with physicians, differences in social support, and out-of-pocket costs (copayments, deductibles, and prescription medications).31 Given that cataracts are a leading cause of blindness among black people,26,32 and yet racial disparities in receipt of cataract surgery persist, additional work is needed to better identify and to eliminate black patients’ barriers to surgery.
Socioeconomic Status and Education
In our analyses, persons with incomes of less than $30000 had an increased hazard for surgery. Some,18,33–35 but not all,36 previous studies similarly found that lower socioeconomic status was associated with an increased likelihood of cataract surgery. Less-affluent persons may have greater exposure to environmental influences (eg, sunlight and pollutants) from their jobs, increasing their cataract density and precipitating the need for surgery. Lifestyle factors, including cigarette smoke, diet, UV exposure, and stress, may also contribute.37–39 Our finding regarding persons of lower socioeconomic status is particularly noteworthy given that this population has been documented generally to have lower utilization rates and poorer access to health care services.40
UV Light Exposure
In our study and in the study by Javitt and colleagues,4 the hazard of surgery was reduced for persons living in communities further away from the equator (higher latitude). This highlights the importance that UV light exposure can have on the development and progression of cataracts.
Urban vs Rural Residence
An interesting finding from our analysis is the relationship between location of residence and likelihood of undergoing cataract surgery. We find that patients in rural communities are more likely than patients in urban communities to undergo cataract extraction. This may be due to differences in environmental, employment, and lifestyle factors, with greater exposure to sunlight among those living in rural communities. Alternatively, those living in rural communities, where there is less access to public transportation and greater distances to travel for work and leisure activities, may require better vision for driving.
Number of Ophthalmologists or Optometrists
We and Javitt and colleagues4 found that cataract surgery rates were not associated with the number of ophthalmologists in the community but were associated with the number of optometrists per 100 000 residents. It may be easier for patients who are struggling with their eyesight to access eye care services in communities with more optometrists. With increased access, more patients are receiving cataract diagnoses and referrals for surgery.
Study Strengths and Limitations
Our large sample of patients with cataracts enabled us to compare the timing and rates of surgery among various communities. Second, because all the enrollees had health insurance, we could identify the variables associated with the timing and rate of surgery beyond the known factor of inadequate access to care. Third, the use of health care professional–submitted billing codes to identify the presence of cataracts and the timing of surgery provides greater accuracy than self-reports by patients.41
Our study has several limitations. First, we could not consider information absent in claims data, including best-corrected visual acuity, degree of symptoms, and the visual needs of each enrollee. These variables all clearly affect the decision to undergo surgery and the timing of surgery; yet, the variation among communities is unknown. Second, our findings may not be generalizable to persons with other insurance types or to noninsured individuals who would surely have lower surgery rates. Third, with claims data alone, we cannot assess the appropriateness of the surgical procedures that were performed. Fourth, some community-level variation in median age and rate of surgery could be due to chance alone. However, because most of the communities studied contributed hundreds of patients or more, this is unlikely to have much of an effect on our results. Finally, the patients’ community of residence was known only for the time of plan enrollment, and we could not account for persons who may have moved from one community to another.
Conclusions
In conclusion, considerable geographic variation exists in the timing of initial cataract surgery and in the cataract surgery rates among different US communities. Future studies should explore the underlying causes for this geographic variation and its effect on patient outcomes.
Supplementary Material
At a Glance.
We determined geographic variation in the median age of patients at initial cataract surgery and the age-standardized cataract surgery rate among many US communities.
The median age of patients at initial cataract surgery was as young as 60 years in some communities and nearly 80 years in others.
The age-standardized cataract surgery rate varied 5-fold across communities, from 7.5% in Honolulu, Hawaii, to 37.3% in Lake Charles, Louisiana.
Black patients had a 15% decreased hazard of undergoing cataract surgery compared with white patients.
Acknowledgments
Funding/Support: This work was supported by the National Eye Institute K23 Mentored Clinician Scientist Award 1K23EY019511 (Dr Stein), the Research to Prevent Blindness “Physician Scientist” Award (Dr Stein), and the W. K. Kellogg Foundation.
Role of the Funder/Sponsor: The funding organizations and study sponsors had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Stein had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Lichter, Lee, Stein.
Acquisition, analysis, or interpretation of data: Kauh, Blachley, Lee, Stein.
Drafting of the manuscript: Kauh, Blachley, Stein.
Critical revision of the manuscript for important intellectual content: Kauh, Blachley, Lichter, Lee.
Statistical analysis: Blachley.
Obtained funding: Stein.
Administrative, technical, or material support: Lee.
Study supervision: Stein
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
References
- 1.Vision Problems in the U.S. Prevalence of age-related eye disease in America. [Accessed July 18, 2015];Prevent Blindness America website. http://www.visionproblemsus.org.
- 2.National Eye Institute (NIH) Cataracts. [Accessed July 18, 2015];NIH website. http://www.nei.nih.gov/eyedata/cataract.asp#3b.
- 3.Schein OD, Cassard SD, Tielsch JM, Gower EW. Cataract surgery among Medicare beneficiaries. Ophthalmic Epidemiol. 2012;19(5):257–264. doi: 10.3109/09286586.2012.698692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Javitt JC, Kendix M, Tielsch JM, et al. Geographic variation in utilization of cataract surgery. Med Care. 1995;33(1):90–105. doi: 10.1097/00005650-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Stein JD, Shekhawat N, Talwar N, Balkrishnan R. Impact of the introduction of generic latanoprost on glaucoma medication adherence. Ophthalmology. 2015;122(4):738–747. doi: 10.1016/j.ophtha.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stein JD, Childers D, Gupta S, et al. Risk factors for developing thyroid-associated ophthalmopathy among individuals with Graves disease. JAMA Ophthalmol. 2015;133(3):290–296. doi: 10.1001/jamaophthalmol.2014.5103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stein JD, Talwar N, Laverne AM, Nan B, Lichter PR. Trends in use of ancillary glaucoma tests for patients with open-angle glaucoma from 2001 to 2009. Ophthalmology. 2012;119(4):748–758. doi: 10.1016/j.ophtha.2011.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muir KW, Gupta C, Gill P, Stein JD. Accuracy of International Classification of Diseases, Ninth Revision, Clinical Modification billing codes for common ophthalmic conditions. JAMA Ophthalmol. 2013;131(1):119–120. doi: 10.1001/jamaophthalmol.2013.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Javitt JC, McBean AM, Sastry SS, DiPaolo F. Accuracy of coding in Medicare part B claims: cataract as a case study. Arch Ophthalmol. 1993;111(5):605–607. doi: 10.1001/archopht.1993.01090050039024. [DOI] [PubMed] [Google Scholar]
- 10.Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science. 1973;182(4117):1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 11.Wennberg JE, Cooper MM, editors. The Dartmouth Atlas of Health Care. Chicago, IL: American Hospital Publishing, Inc; 1996. [PubMed] [Google Scholar]
- 12.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48(1 suppl):S42–S53. [PubMed] [Google Scholar]
- 13.Fisher ES, Wennberg JE. Health care quality, geographic variations, and the challenge of supply-sensitive care. Perspect Biol Med. 2003;46(1):69–79. doi: 10.1353/pbm.2003.0004. [DOI] [PubMed] [Google Scholar]
- 14.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 15.Jobson Medical Information LLC. The Blue Book of Optometrists 2012: Who’s Who in Optometry. Woodstock, VT: Jobson Medical Information LLC; 2012. [Google Scholar]
- 16.Compare climates. [Accessed June 24, 2015];Sperling's Best Places Website. http://www.bestplaces.net/climate.
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Keenan T, Rosen P, Yeates D, Goldacre M. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol. 2007;91(7):901–904. doi: 10.1136/bjo.2006.108977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatch WV, Cernat G, Singer S, Bell CM. A 10-year population-based cohort analysis of cataract surgery rates in Ontario. Can J Ophthalmol. 2007;42(4):552–556. [PubMed] [Google Scholar]
- 20.US Environmental Protection Agency. Addressing air emissions from the petroleum refinery sector: risk and technology review and new source performance standard rulemaking. [Accessed July 14, 2015]; http://www.epa.gov/apti/video/10182011Webinar/101811webinar.pdf.
- 21.Klein BE, Klein R, Lee KE. Incidence of age-related cataract: the Beaver Dam Eye Study. Arch Ophthalmol. 1998;116(2):219–225. doi: 10.1001/archopht.116.2.219. [DOI] [PubMed] [Google Scholar]
- 22.Congdon N, O’Colmain B, Klaver CCW, et al. Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122(4):477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 23.Congdon N, Vingerling JR, Klein BE, et al. Eye Diseases Prevalence Research Group. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004;122(4):487–494. doi: 10.1001/archopht.122.4.487. [DOI] [PubMed] [Google Scholar]
- 24.Lewis A, Congdon N, Muñoz B, et al. Cataract surgery and subtype in a defined, older population: the SEECAT Project. Br J Ophthalmol. 2004;88(12):1512–1517. doi: 10.1136/bjo.2004.045484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leske MC, Chylack LT, Jr, He Q, et al. LSC Group. Longitudinal Study of Cataract. Risk factors for nuclear opalescence in a longitudinal study. Am J Epidemiol. 1998;147(1):36–41. doi: 10.1093/oxfordjournals.aje.a009364. [DOI] [PubMed] [Google Scholar]
- 26.Tielsch JM, Javitt JC, Coleman A, Katz J, Sommer A. The prevalence of blindness and visual impairment among nursing home residents in Baltimore. N Engl J Med. 1995;332(18):1205–1209. doi: 10.1056/NEJM199505043321806. [DOI] [PubMed] [Google Scholar]
- 27.Mainous AG, III, Johnson SP, Saxena SK, Wright RU. Inpatient bariatric surgery among eligible black and white men and women in the United States, 1999–2010. Am J Gastroenterol. 2013;108(8):1218–1223. doi: 10.1038/ajg.2012.365. [DOI] [PubMed] [Google Scholar]
- 28.West SK, Muñoz B, Schein OD, Duncan DD, Rubin GS. Racial differences in lens opacities: the Salisbury Eye Evaluation (SEE) project. Am J Epidemiol. 1998;148(11):1033–1039. doi: 10.1093/oxfordjournals.aje.a009579. [DOI] [PubMed] [Google Scholar]
- 29.Orr P, Barrón Y, Schein OD, Rubin GS, West SK. Eye care utilization by older Americans: the SEE Project: Salisbury Eye Evaluation. Ophthalmology. 1999;106(5):904–909. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 30.Williams A, Sloan FA, Lee PP. Longitudinal rates of cataract surgery. Arch Ophthalmol. 2006;124(9):1308–1314. doi: 10.1001/archopht.124.9.1308. [DOI] [PubMed] [Google Scholar]
- 31.Owsley C, McGwin G, Scilley K, Girkin CA, Phillips JM, Searcey K. Perceived barriers to care and attitudes about vision and eye care: focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006;47(7):2797–2802. doi: 10.1167/iovs.06-0107. [DOI] [PubMed] [Google Scholar]
- 32.Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. N Engl J Med. 1991;325(20):1412–1417. doi: 10.1056/NEJM199111143252004. [DOI] [PubMed] [Google Scholar]
- 33.Chang JR, Koo E, Agrón E, et al. Age-Related Eye Disease Study Group. Risk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmology. 2011;118(11):2113–2119. doi: 10.1016/j.ophtha.2011.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Delcourt C, Cristol JP, Tessier F, Léger CL, Michel F, Papoz L. Risk factors for cortical, nuclear, and posterior subcapsular cataracts: the POLA study: Pathologies Oculaires Liées à l’Age. Am J Epidemiol. 2000;151(5):497–504. doi: 10.1093/oxfordjournals.aje.a010235. [DOI] [PubMed] [Google Scholar]
- 35.Leske MC, Wu SY, Connell AM, Hyman L, Schachat AP. Lens opacities, demographic factors and nutritional supplements in the Barbados Eye Study. Int J Epidemiol. 1997;26(6):1314–1322. doi: 10.1093/ije/26.6.1314. [DOI] [PubMed] [Google Scholar]
- 36.Javitt JC, Taylor HR. Cataract and latitude. Doc Ophthalmol. 1994–1995;88(3–4):307–325. doi: 10.1007/BF01203684. [DOI] [PubMed] [Google Scholar]
- 37.Mares JA, Voland R, Adler R, et al. CAREDS Group. Healthy diets and the subsequent prevalence of nuclear cataract in women. Arch Ophthalmol. 2010;128(6):738–749. doi: 10.1001/archophthalmol.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mares-Perlman JA, Lyle BJ, Klein R, et al. Vitamin supplement use and incident cataracts in a population-based study. Arch Ophthalmol. 2000;118(11):1556–1563. doi: 10.1001/archopht.118.11.1556. [DOI] [PubMed] [Google Scholar]
- 39.Glynn RJ, Rosner B, Christen WG. Evaluation of risk factors for cataract types in a competing risks framework. Ophthalmic Epidemiol. 2009;16(2):98–106. doi: 10.1080/09286580902737532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang X, Saaddine JB, Lee PP, et al. Eye care in the United States: do we deliver to high-risk people who can benefit most from it? Arch Ophthalmol. 2007;125(3):411–418. doi: 10.1001/archopht.125.3.411. [DOI] [PubMed] [Google Scholar]
- 41.Patty L, Wu C, Torres M, Azen S, Varma R Los Angeles Latino Eye Study Group. Validity of self-reported eye disease and treatment in a population-based study: the Los Angeles Latino Eye Study. Ophthalmology. 2012;119(9):1725–1730. doi: 10.1016/j.ophtha.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.