Abstract
Importance
Morbidity and mortality associated with prescription opioid use is escalating in the United States. The extent to which chronic opioid use influences postoperative outcomes following elective surgery is not well understood.
Objective
To examine the extent to which preoperative opioid use is correlated with healthcare utilization and costs following elective surgical procedures.
Design
Truven Health Marketscan® Databases were used to identify patients.
Setting
Outpatient services claims from patients who underwent elective procedure requiring an inpatient stay.
Participants
Patients ages 18 and older who underwent elective hysterectomy, bariatric surgery, reflux procedures, and ventral hernia repair between 2009 and 2013 (n=184,053).
Exposure
Receipt of prescription opioid analgesic within 30 days of and 30 to 90 days prior to procedure. Preoperative opioid use was drawn from insurance claims and converted into oral morphine equivalents (OMEs).
Main Outcomes and Measures
Outcomes included postoperative healthcare utilization (length of stay, 30-day readmission rate, discharge destination) and cost (hospital stay, 90-, 180-, and 365-day). We used generalized linear regression to determine the effect of preoperative opioid use on healthcare utilization and cost outcomes after adjusting for number of comorbidities, psychological conditions, and demographic characteristics.
Results
In this cohort, 10.0% of patients used opioids preoperatively. Compared with non-users, patients using opioids preoperatively were more likely to have a longer and more expensive hospital stay (2.8 days vs. 2.5 days, p<0.001; $21,919.00 vs. $21,241.80, p = 0.02, respectively) and were more likely to be discharged to a rehabilitation facility (3.5% vs. 2.4%, p<0.001), adjusting for covariates. Preoperative opioid use was also correlated with a greater rate of 30-day readmission (3.7% vs. 3.1%, p<0.001) and overall greater expenditures at 90- ($5,405.40 vs. $3,681.70, p<0.001), 180- ($10,148.20 vs. $6,469.80, p<0.001), and 365-($19,695.60 vs. $11,419.40, p<0.001) days following surgery, adjusted for covariates.
Conclusions and Relevance
Preoperative opioid use is an independent risk factor for longer length of stay, higher 30-day readmission rates and probability of being discharged to a rehabilitation facility, and greater costs in the postoperative period. Preoperative interventions focused on opioid cessation and alternative analgesics may improve the safety and efficiency of elective surgery among chronic opioid users.
Introduction
In the United States, 1 out of every 25 adults regularly uses prescription opioid medications.1 Accordingly, opioid use is higher in the United States than any other country in the world, and opioid-associated morbidity and mortality has been cited by the Centers for Disease Control and Prevention as a major public health concern.2,3 Nonetheless, opioid prescribing continues to accelerate.4 For example, from 1999 to 2011, consumption of hydrocodone doubled, and oxycodone consumption increased by 500% within the United States.3 As such, the proportion of individuals who are chronically using prescription opioid medications is expected to accelerate in the coming years.
Although opioids can provide effective pain relief for acute pain, chronic use is associated with numerous adverse dose-related effects. Chronic opioid exposure results in structural and functional central nervous system changes that mediate affect, impulse, reward, and motivation.5 Prior to surgery, these effects may lead to dependence, tolerance, and even reduction in pain thresholds with diffuse hyperalgesia, which may complicate pain management and patient rehabilitation following surgery.6,7
In recent decades, much attention has been directed toward minimizing perioperative risk for patients with chronic conditions such as heart disease, diabetes, and tobacco use undergoing elective surgical procedures.8,9 However, the extent to which chronic opioid use independently influences surgical outcomes remains poorly understood. In this context, we sought to define the differences in healthcare utilization and associated costs among patients undergoing elective abdominal surgical procedures in the United States. We specifically examined three aspects of healthcare utilization: length of stay, discharge destination, and readmission within 30 days of the surgical procedure. Additionally, we examined postoperative costs at 90-, 180-, and 365- days following surgery. We hypothesized that patients who are chronically exposed to opioids undergoing surgery have higher healthcare utilization and associated costs compared with opioid naïve patients, and that these outcomes increase with greater average daily opioid doses.
Methods
Data source and study cohort
We analyzed the Truven Health MarketScan® Research Databases, including the MarketScan Commercial Claims and Encounters Database and the Medicare Supplemental and Coordination of Benefits Database. These databases capture patient-level utilization of medical services, payment, and enrollment across inpatient, outpatient and prescription drugs, represent the healthcare utilization of approximately 50 million active employees, early retirees, Medicare-eligible retirees with employer-provided Medicare Supplemental plans, and their dependents each year. We examined the outpatient services claims from patients ages 18 and older who underwent one of the following major elective procedures requiring an inpatient stay between 2009 and 2013: hysterectomy, ventral hernia repair, anti-reflux procedures, and bariatric surgery procedures. We identified these procedures using International Classification of Disease 9th revision codes (ICD-9 diagnosis codes) for the indication (primary diagnosis) and Current Procedural Terminology codes (CPT codes) for the procedure description (eTable 1). We specified that patients must be continually enrolled in healthcare plans captured by Marketscan with pharmaceutical coverage between 7/1/2009 to 12/30/2012 in order to capture comorbid conditions and opioid utilization in the 6 month period prior to surgery and healthcare cost and utilization up to 1 year following surgery.
Preoperative opioid use
Patients were classified as using preoperative opioid medications if they filled at least one opioid prescription within 30 days of their procedure and at least another prescription of opioid 30 to 90 days prior to the procedure in order to capture current and chronic use. We used generic drug names matched with National Drug Codes to identify opioid prescriptions from the insurance claims (eTable 2), and obtain specific drug dose and type. For each prescription, we first converted the unit of the opioid component to milligrams, and we then calculated average daily oral morphine equivalents (OMEs) for this prescription using the morphine equivalent conversion factor per milligram for this opioid medication.10,11 The total OME dosage for each opioid prescription was calculated as the daily OME exposure multiplied by number of days of supply filled in this prescription. In order to quantify the average daily OME exposure for patients within 90 days prior to the surgery, we calculated total OME dosage in this period by adding up OME dosage of all the opioid prescriptions within this period. We then divided the total OME dosage within 90 days prior to the surgery by the total number of days supplied provided in these prescriptions to calculate the average daily OME exposure within 90 days prior to the surgery.
Outcome variables
Our outcomes included measures of healthcare utilization and associated costs following surgery. We examined length of hospital stay in days, which was obtained from claims indicating the date of surgery until the date of discharge, as well as discharge destination (home vs. rehabilitation facility), and 30-day readmissions (for any cause) by examining associated claims in the postoperative period. We examined expenditures for the hospital stay, as well as 90-, 180-, and 365-day expenditures, excluding professional fees, including inpatient and outpatient financial data for procedural costs and facility fees for each patient. Expenditures were adjusted for inflation relative to the 2013 consumer price index.
Independent variables
We examined patient sociodemographic factors, specifically age (18–34 years, 35–44 years, 45–54 years, 55–64 years, and 65 years and older), gender, metropolitan statistical area (MSA), type of insurance plan, and geographic region of residence. The MSA describes geographical regions with a relatively high density of population at its core with adjacent communities with similar degree of social and economic factors as the core. We linked the MSA identifier for each patient to the 2010 census data and obtained median household income of each area where the patients resided. We then categorized regional median house income by quartiles for the patient cohort. We categorized insurance plan type into five groups: comprehensive health insurance, health maintenance organization (HMO) plans, preferred provider organization (PPO) plans, point of service (POS) plans and other (e.g. Medicare). Additionally, we included geographic region of the United States (northeast, north central, south and west regions) into the analysis. Finally, we included the presence of comorbid conditions using standard risk-adjustment techniques. We identified comorbid conditions using their corresponding ICD-9-CM codes, and these were classified using the Elixhauser method.12
Analysis
We generated descriptive statistics to describe the attributes of the study cohort. We created two independent variables describing the use of opioid before the procedure: 1) whether used opioids before surgery (dichotomous) and 2) average daily OME dosage within 90 days prior to the surgery. We categorized the latter variable into 7 groups (opioid naïve, 0–10 OME, 10–25 OME, 25–50 OME, 50–75 OME, 75–100 OME and >100 OME average per day). For each of the dependent variables (readmission within 30 days, discharge to home, length of hospital stay, cost of hospital stay and healthcare cost within 90, 180 and 365 days following discharge), we constructed two regression models, each with one of the two variables describing opioid use before surgery as the primary predictor, and controlled for all other patient characteristics. Length of hospital stay was treated as count data, and we used Poisson regression model for LOS; linear regression models were constructed to examine the relationship between preoperative opioid prescription fills and postoperative costs. Using the adjusted odds ratios from logistic regression models, lambda from Poisson regression models, and beta-coefficient from linear regression models, we back-calculated adjusted rate of readmission, adjusted rate of discharge to facilities, adjusted mean length of hospital stay and adjusted mean cost for hospital stay, and 90, 180, 365 days healthcare cost following surgery. P values <0.05 were considered significant in all final analyses and all statistical analyses were performed using SAS/STAT® software (Cary, NC).
Results
We identified 184, 053 patients who underwent elective abdominal procedures during the study period: 57% underwent hysterectomy, 29% bariatric surgery, 4% reflux surgery, and 10% ventral hernia repair (Table 1). The majority of hysterectomy and bariatric patients were between the ages of 35 and 54 (75% and 60%, respectively) and the majority of reflux and hernia patients were 45 and older (81% and 83%, respectively). More than half of the participants receiving a procedure were female (61% to 100% (hysterectomy)) and the majority of participants had a median annual household income of $40–60,000 (63% – 67 %). The greatest proportion of patients had a provider preferred organization insurance plan (55% – 58%), followed by health maintenance organization plans (12% – 16%). Although the majority of patients had multiple comorbidities with Elixhauser scores of 3 or more, concomitant psychiatric diagnoses were less common. Overall, approximately 1 in 10 patients had filled an opioid prescription prior to surgery (7% – 13%).
Table 1.
Characteristics of the Study Cohort by Surgical Procedure
| Characteristics | Hysterectomy (n = 105476) |
Bariatric (n = 52970) |
Reflux (n = 6545) |
Ventral Hernia (n = 19062) |
|---|---|---|---|---|
| Age, No. (%) | ||||
| 18–34 | 6995 (7) | 10095 (19) | 440 (7) | 763 (4) |
| 35–44 | 38188 (36) | 15654 (30) | 834 (13) | 2480 (13) |
| 45–54 | 41011 (39) | 15784 (30) | 1529 (23) | 4929 (26) |
| 55–64 | 12901 (12) | 9808 (19) | 1876 (29) | 5527 (29) |
| 65 and older | 6381 (6) | 1629 (3) | 1866 (29) | 5363 (28) |
| Sex, No. (%) | ||||
| Male | 8 (0) | 12098 (23) | 2158 (33) | 7431 (39) |
| Female | 105468 (100) | 40872 (77) | 4387 (67) | 11631 (61) |
| MSA median household income, No. (%) | ||||
| <40k | 3293 (3) | 1419 (3) | 151 (2) | 461 (2) |
| 40k–50k | 26540 (25) | 12074 (23) | 1788 (27) | 5171 (27) |
| 50k–60k | 41677 (40) | 23530 (44) | 2326 (36) | 6929 (36) |
| 60k–70k | 11190 (11) | 5851 (11) | 696 (11) | 2573 (13) |
| >70k | 3624 (3) | 2426 (5) | 245 (4) | 619 (3) |
| Missing | 19152 (18) | 7670 (14) | 1339 (20) | 3309 (17) |
| Insurance plan, No. (%) | ||||
| PPO | 61571 (58) | 30256 (57) | 3574 (55) | 10636 (56) |
| Comprehensive | 3963 (4) | 1819 (3) | 922 (14) | 2736 (14) |
| HMO | 16416 (16) | 8274 (16) | 838 (13) | 2339 (12) |
| POS | 8386 (8) | 5068 (10) | 403 (6) | 1304 (7) |
| Other | 8148 (8) | 4283 (8) | 345 (5) | 1011 (5) |
| Missing | 6992 (7) | 3270 (6) | 463 (7) | 1036 (5) |
| Elixhauser comorbidities score, No. (%) | ||||
| 0 or 1 | 36850 (35) | 811 (2) | 1110 (17) | 2224 (12) |
| 2 | 21407 (20) | 2943 (6) | 917 (14) | 2344 (12) |
| 3 | 16922 (16) | 5866 (11) | 983 (15) | 2568 (13) |
| More than 3 | 30297 (29) | 43350 (82) | 3535 (54) | 11926 (63) |
| Psychological conditions, No. (%) | ||||
| None | 93538 (89) | 32972 (62) | 5482 (84) | 16606 (87) |
| Depression | 3671 (3) | 5139 (10) | 372 (6) | 856 (4) |
| Anxiety | 4741 (4) | 4495 (8) | 425 (6) | 795 (4) |
| Substance | 2387 (2) | 946 (2) | 161 (2) | 555 (3) |
| Other | 1139 (1) | 9418 (18) | 105 (2) | 250 (1) |
| Preoperative opioid use, No. (%) | ||||
| No | 97927 (93) | 47933 (90) | 5900 (90) | 16630 (87) |
| Yes | 7549 (7) | 5037 (10) | 645 (10) | 2432 (13) |
Abbreviations: MSA, metropolitan statistical area; PPO, preferred provider organization; HMO, health maintenance organization; POS, point of service.
Healthcare Utilization
Table 2 details the differences in measures of healthcare utilization and expenditures between preoperative opioid users and opioid naïve patients across all procedures, adjusted for all patient demographic and clinical characteristics. On average, preoperative opioid users remained in the hospital longer than patients who did not use opioids preoperatively across all procedures (2.8 days vs. 2.5 days, p < 0.001). Preoperative opioid users were also more likely to be readmitted to the hospital within 30 days of their respective surgical procedure, and discharged to a rehabilitation facility in comparison to opioid naïve patients (3.7% vs. 3.1%, p < 0.001; 3.5% vs. 2.4%, p < 0.001, respectively).
Table 2.
Differences in Healthcare Utilization and Expenditure Following Surgery Between Preoperative Opioid Users and Non-usersa
| Opioid Naïveb | Preoperative Opioid Use | P Value | |
|---|---|---|---|
| Healthcare Utilization | |||
| Length of hospital stay, days | 2.5 | 2.8 | <0.001 |
| Patients discharged to rehabilitation facilities, % | 2.4 | 3.5 | <0.001 |
| Patients readmitted within 30 days, % | 3.1 | 3.7 | <0.001 |
| Healthcare Expenditure | |||
| Cost of hospital stay, USD | 21, 241.80 | 21, 919.00 | 0.02 |
| 90-day postoperative cost, USD | 3,681.70 | 5,405.40 | <0.001 |
| 180-day postoperative cost, USD | 6,469.80 | 10,148.20 | <0.001 |
| 365-day postoperative cost, USD | 11,419.40 | 19,695.60 | <0.001 |
All models were adjusted by all patient demographic and clinical characteristics
Opioid naïve patients served as the reference group
Figure 1 displays the differences in healthcare utilization postoperatively, stratified by the average daily preoperative opioid dose during the preceding 90 days. Preoperative opioid users, with the exception of those who had a 90 day preoperative dosage of less than 10 OME, had significantly longer lengths of stay than their opioid naïve counterparts (Figure 1a; p < 0.01 for all). Additionally, significantly more opioid users, with the exception of those who had a 90 day preoperative dosage of less than 10 OME and 50–75 OME, were readmitted to the hospital within 30 days of their procedure (Figure 1b; p < 0.05 for all). Similarly, significantly more opioid users, with the exception of those who had a 90 day preoperative dosage of less than 10 OME and 75–100 OME, were discharged to a rehabilitation facility after their procedure (Figure 1c; p < 0.01 for all).
Figure 1. Healthcare Utilization by Average Daily Oral Morphine Equivalent Exposure.
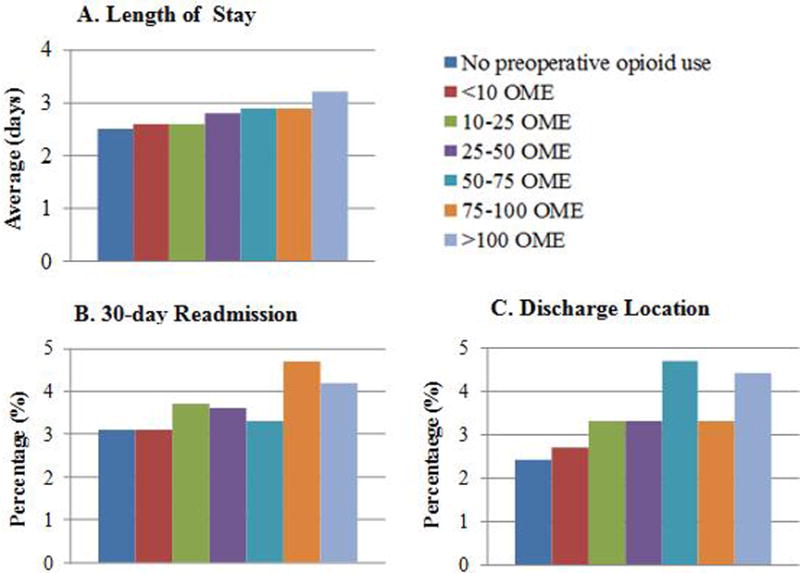
Abbreviations: OME, oral morphine equivalent. All healthcare utilization outcomes were adjusted for patient clinical and demographic characteristics.
Healthcare Expenditures
Across all procedures, patients that used opioids preoperatively accrued higher costs of their postoperative hospital stay ($21,919.00 vs. $21,241.80, p = 0.02) as well as higher total post-operative costs 90 ($5,405.40 vs. $3,681.70, p<0.001), 180 ($10,148.20 vs. $6,469.80, p<0.001), and 365 ($19,695.60 vs. $11,419.40, p<0.001) days after their procedure than their opioid naïve counterparts (Table 2).
Figure 2 illustrates measures of healthcare expenditure by category of oral morphine equivalent. Preoperative opioid users, with the exception of those who had a 90 day preoperative dosage of <10 OME, accrued significantly higher costs 90 days after surgery (p < 0.01 for all). Additionally, regardless of their 90 day preoperative daily dosage, all opioid users had significantly higher postoperative costs 180 and 365 days after surgery than their opioid naïve counterparts (p < 0.05 for <10 OME, p<0.001 for all other categories). When preoperative opioid use was examined as a continuous variable, we observed that increasing preoperative opioid dosage was correlated with an increase in hospital stay expenditures, (β = 17.93, p < 0.001) as well as 90- (β = 17.23, p < 0.001), 180- (β = 36.83, p < 0.001), and 365- (β = 83.17, p < 0.001) day post-operative expenditures.
Figure 2. Healthcare Expenditures by Average Daily Oral Morphine Equivalent Exposure.
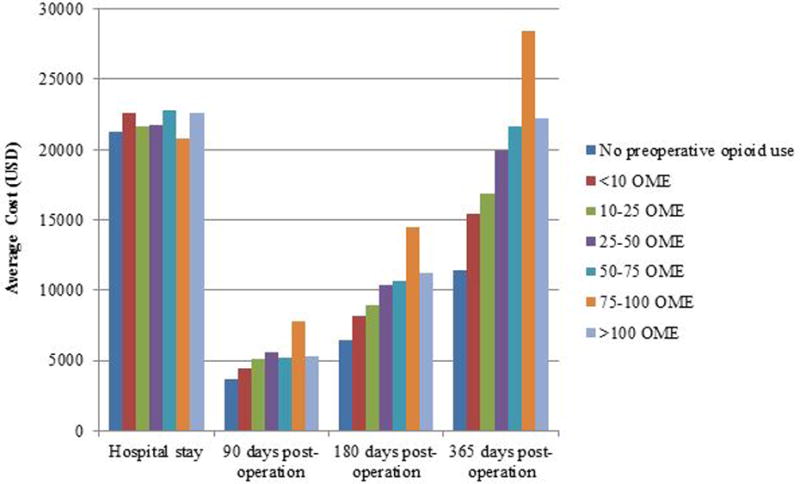
Abbreviations: OME, oral morphine equivalent. All healthcare expenditure outcomes were adjusted for patient clinical and demographic characteristics.
Discussion
In the United States, prescription opioids are widely used for chronic pain, and have grown increasingly popular in recent years. In this cohort of adults undergoing elective abdominal procedures, we observed that preoperative opioid use is an independent risk factor for longer length of stay, higher 30-day readmission rates, lower probability of being discharged home, and greater health expenditures in the postoperative period. Approximately 10% of patients regularly fill prescriptions for opioids medications in the preoperative period, with doses ranging from less than 10 OMEs (or the equivalent of 2 tablets of 5mg hydrocodone) to over 100 OMEs daily (or the equivalent of 20 tablets of 5mg hydrocodone).
Previous studies have examined the relationship between preoperative opioid use and postoperative outcomes, and have documented poorer outcomes among patients who use opioid preoperatively. For example, following total knee arthroplasty, chronic opioid users have poorer self-reported outcomes, greater stiffness, and more revision procedures, and chronic opioid users have a higher risk of in-hospital postoperative morbidity and mortality following elective orthopaedic surgical procedures.13,14 Similarly, preoperative opioid use has been shown to increase the risk of revision surgery for pain related conditions, such as compression neuropathy.15 Taken together, these findings suggest that identifying strategies to minimize opioid consumption prior to surgery, particularly elective surgery, is an opportunity to reduce patient risk, improve outcomes, and lower healthcare costs.
Our study has several notable limitations. First, our analysis focuses on insurance claims data, which is sensitive to detect perioperative events and medication fills, but lacks sufficient granularity to define opioid consumption and patient-reported pain. Additionally, this data is gathered from individuals with employer-based insurance and their beneficiaries, and may not be generalizable to the uninsured, underinsured, and those who rely solely on state and federal healthcare coverage. Finally, we do not have access to the extent to which provider-level variation explains differences in the outcomes we observed.
Despite these limitations, our findings have important implications for patients anticipating surgery, and clinicians and surgeons seeking to optimize patient safety and postoperative outcomes. Achieving acceptable pain control following surgery is critical, and the under-treatment of pain has garnered national attention as an indicator of poor surgical quality.16–19 In recent years, there is a keen awareness of pain as a component of health status, and pain has been termed the “5th vital sign.”20 Inadequately controlled postoperative pain delays important recovery milestones, such as ambulation or attending to activities of daily living, and results in longer hospital stays and chronic post-surgical pain.21–25 Poorly managed pain is also a common reason for readmission, and is correlated with poor patient satisfaction and experience.26,27 However, although some patients benefit from chronic opioid therapy, most do not, and morbidity and abuse outweigh any benefits derived. 28–31 Furthermore, the effectiveness of opioids is not uniform across individuals, and varies by genetic, environmental, and biopsychosocial factors.32 Opioids may also be less effective among individuals with mood disturbance, including depression, anxiety, and catastrophic thinking, as well as patients who suffer from fibromyalgia, neuropathic pain, and psychiatric disease.33–36
Preoperative opioid use complicates perioperative pain management and postoperative rehabilitation, and can result in including respiratory depression, sedation, postoperative nausea and vomiting, urinary retention, and ileus. Even controlling for complications and comorbid risk factors, preoperative opioid use results in longer length of stay, higher re-admission rates, and greater surgery-related expenditures.37–39 In this context, elective surgical procedures offer an opportunity for surgeons to pause, and identify strategies to optimize patient safety and minimize risk in the preoperative period. It also provides an opportunity to engage primary care providers at the time of surgical decision-making and preoperative work-up to streamline transitions of care for those patients who may continue to require opioids for an extended period of time following surgery. Finally, our findings suggest that highlighting opioid alternatives for pain control when possible may reduce postoperative costs and healthcare utilization.
In conclusion, chronic opioid use complicates management following surgery, and increases postoperative healthcare utilization and costs independent of other risk factors. Therefore, developing preoperative interventions that focus on opioid cessation and alternative prior to elective surgery may improve the quality of surgical care delivered in the United States.
Supplementary Material
Acknowledgments
Dr. Waljee receives research funding from the Agency for Healthcare Research and Quality (K08 1K08HS023313-01), the American College of Surgeons, and the American Foundation for Surgery of the Hand; serves as an unpaid consultant for 3M Health Information systems. Dr. Brummett receives research funding from the National Institutes of Health, NIAMS R01 AR060392 and NIDA 1R01DA038261-01A1, as well as the University of Michigan Medical School Dean’s Office (Michigan Genomics Initiative). Dr. Brummett also serves as a consultant for Tonix Pharmaceuticals (New York, NY), and receives research funding from Neuros Medical Inc. (Willoughby Hills, Ohio).
Funding/Support: This research was supported by a Mentored Clinical Investigator Award to Dr. Waljee through the Agency for Healthcare Research and Quality (1K08HS023313-01).
Role of the Funder/Sponsor: The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr. Zhong had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brummett, Cron, Englesbe, Waljee.
Acquisition, analysis, or interpretation of data: Zhong, Cron, Brummett, Englesbe, Waljee, Steiger.
Drafting of the manuscript: Waljee, Cron, Brummett, Englesbe, Steiger, Zhong.
Critical revision of the manuscript for important intellectual content: Waljee, Cron, Brummett, Englesbe, Steiger, Zhong.
Statistical analysis: Zhong.
Administrative, technical, or material support: Steiger, Zhong.
Study supervision: Waljee, Cron, Brummett.
Disclosures:
No other authors have any conflicts of interest to disclose.
References
- 1.Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000-2010. Open Med. 2012;6(2):e41–e47. [PMC free article] [PubMed] [Google Scholar]
- 2.Paulozzi LJ, Mack KA, Hockenberry JM. Variation among states in prescribing of opioid pain relievers and benzodiazepines-United States, 2012. J Safety Res. 2014;51:125–129. doi: 10.1016/j.jsr.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Paulozzi LJ, Weisler RH, Patkar AA. A national epidemic of unintentional prescription opioid overdose deaths: how physicians can help control it. J Clin Psychiatry. 2011;72(5):589–592. doi: 10.4088/JCP.10com06560. [DOI] [PubMed] [Google Scholar]
- 4.Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med. 2015;49(3):409–413. doi: 10.1016/j.amepre.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Younger JW, Chu LF, D’Arcy NT, Trott KE, Jastrzab LE, Mackey SC. Prescription opioid analgesics rapidly change the human brain. Pain. 2011;152(8):1803–1810. doi: 10.1016/j.pain.2011.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hina N, Fletcher D, Poindessous-Jazat F, Martinez V. Hyperalgesia induced by low-dose opioid treatment before orthopaedic surgery: an observational case-control study. Eur J Anaesthesiol. 2015;32(4):255–261. doi: 10.1097/EJA.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 7.Trang T, Al-Hasani R, Salvemini D, Salter MW, Gutstein H, Cahill CM. Pain and poppies: the good, the bad, and the ugly of opioid analgesics. J Neurosci. 2015;35(41):13879–13888. doi: 10.1523/JNEUROSCI.2711-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottle A, Mozid A, Grocott HP, et al. Preoperative risk factors in 10 418 patients with prior myocardial infarction and 5241 patients with prior unstable angina undergoing elective coronary artery bypass graft surgery. Br J Anaesth. 2013;111(3):417–423. doi: 10.1093/bja/aet107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godoy DA, Di Napoli M, Biestro A, Lenhardt R. Perioperative glucose control in neurosurgical patients. Anesthesiol Res Pract. 2012;2012:690362. doi: 10.1155/2012/690362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440–449. doi: 10.1016/j.pain.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013;51(8):646–653. doi: 10.1097/MLR.0b013e318293c2c0. [DOI] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res. 2015;473(7):2402–2412. doi: 10.1007/s11999-015-4173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011;93(21):1988–1993. doi: 10.2106/JBJS.J.01473. [DOI] [PubMed] [Google Scholar]
- 15.Gaspar MP, Jacoby SM, Osterman AL, Kane PM. Risk factors predicting revision surgery after medial epicondylectomy for primary cubital tunnel syndrome. J Shoulder Elbow Surg. 2016;25(4):681–687. doi: 10.1016/j.jse.2015.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Porter J, Jick H. Addiction rare in patients treated with narcotics. N Engl J Med. 1980;302(2):123. doi: 10.1056/nejm198001103020221. [DOI] [PubMed] [Google Scholar]
- 17.Acute pain management in adults: operative procedures. Agency for Health Care Policy and Research. Clin Pract Guidel Quick Ref Guide Clin. 1992;(1A):1–22. [PubMed] [Google Scholar]
- 18.Acute pain management: operative or medical procedures and trauma, Part 1. Agency for Health Care Policy and Research. Clin Pharm. 1992;11(4):309–331. [PubMed] [Google Scholar]
- 19.Cheatle MD. Prescription opioid misuse, abuse, morbidity, and mortality: balancing effective pain management and safety. Pain Med. 2015;16(Suppl 1):S3–S8. doi: 10.1111/pme.12904. [DOI] [PubMed] [Google Scholar]
- 20.Lorenz KA, Sherbourne CD, Shugarman LR, et al. How reliable is pain as the fifth vital sign? J Am Board Fam Pract. 2009;22(3):291–298. doi: 10.3122/jabfm.2009.03.080162. [DOI] [PubMed] [Google Scholar]
- 21.Lawton J, Waugh N, Barnard KD, et al. Challenges of optimizing glycaemic control in children with Type 1 diabetes: a qualitative study of parents’ experiences and views. Diabet Med. 2015;32(8):1063–1070. doi: 10.1111/dme.12660. [DOI] [PubMed] [Google Scholar]
- 22.American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116(2):248–273. doi: 10.1097/ALN.0b013e31823c1030. [DOI] [PubMed] [Google Scholar]
- 23.Alvarez MP, Foley KE, Zebley DM, Fassler SA. Comprehensive enhanced recovery pathway significantly reduces postoperative length of stay and opioid usage in elective laparoscopic colectomy. Surg Endosc. 2014;29(9):2506–2511. doi: 10.1007/s00464-014-4006-8. [DOI] [PubMed] [Google Scholar]
- 24.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 25.Huang A, Katz J, Clarke H. Ensuring safe prescribing of controlled substances for pain following surgery by developing a transitional pain service. Pain Manag. 2015;5(2):97–105. doi: 10.2217/pmt.15.7. [DOI] [PubMed] [Google Scholar]
- 26.Curtin CM, Hernandez-Boussard T. Readmissions after treatment of distal radius fractures. J Hand Surg Am. 2014;39(10):1926–1932. doi: 10.1016/j.jhsa.2014.07.041. [DOI] [PubMed] [Google Scholar]
- 27.Chang CB, Cho WS. Pain management protocols, peri-operative pain and patient satisfaction after total knee replacement: a multicentre study. J Bone Joint Surg Br. 2012;94(11):1511–1516. doi: 10.1302/0301-620X.94B11.29165. [DOI] [PubMed] [Google Scholar]
- 28.Reuben DB, Alvanzo AA, Ashikaga T, et al. National Institutes of Health Pathways to Prevention Workshop: the role of opioids in the treatment of chronic pain. Ann Intern Med. 2015;162(4):295–300. doi: 10.7326/M14-2775. [DOI] [PubMed] [Google Scholar]
- 29.Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162(4):276–286. doi: 10.7326/M14-2559. [DOI] [PubMed] [Google Scholar]
- 30.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350:g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell JN. The fifth vital sign revisited. Pain. 2016;157(1):3–4. doi: 10.1097/j.pain.0000000000000413. [DOI] [PubMed] [Google Scholar]
- 32.Ren ZY, Xu XQ, Bao YP, et al. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: a systematic review and meta-analysis. Pain Physician. 2015;18(2):131–152. [PubMed] [Google Scholar]
- 33.Helmerhorst GT, Vranceanu AM, Vrahas M, Smith M, Ring D. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014;96(6):495–499. doi: 10.2106/JBJS.L.01406. [DOI] [PubMed] [Google Scholar]
- 34.Goesling J, Henry MJ, Moser SE, et al. Symptoms of depression are associated with opioid use regardless of pain severity and physical functioning among treatment-seeking patients with chronic pain. J Pain. 2015;16(9):844–851. doi: 10.1016/j.jpain.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 35.Wasserman RA, Brummett CM, Goesling J, Tsodikov A, Hassett AL. Characteristics of chronic pain patients who take opioids and persistently report high pain intensity. Reg Anesth Pain Med. 2014;39(1):13–17. doi: 10.1097/AAP.0000000000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hooten WM, Shi Y, Gazelka HM, Warner DO. The effects of depression and smoking on pain severity and opioid use in patients with chronic pain. Pain. 2011;152(1):223–229. doi: 10.1016/j.pain.2010.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oderda GM, Evans RS, Lloyd J, et al. Cost of opioid-related adverse drug events in surgical patients. J Pain Symptom Manage. 2003;25(3):276–283. doi: 10.1016/s0885-3924(02)00691-7. [DOI] [PubMed] [Google Scholar]
- 38.Oderda GM, Gan TJ, Johnson BH, Robinson SB. Effect of opioid-related adverse events on outcomes in selected surgical patients. J Pain Palliat Care Pharmacother. 2013;27(1):62–70. doi: 10.3109/15360288.2012.751956. [DOI] [PubMed] [Google Scholar]
- 39.Raebel MA, Newcomer SR, Reifler LM, et al. Chronic use of opioid medications before and after bariatric surgery. JAMA. 2013;310(13):1369–1376. doi: 10.1001/jama.2013.278344. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


