Abstract
Research on nonsuicidal self-injury (NSSI) has moved beyond examination of factors that associate with the mere presence or absence of the behavior, and into more nuanced examination of which discrete features of NSSI behavior relate to pathology. This study examined two features of NSSI, frequency of occurrence and recency, as cross-sectional predictors of psychopathology in a large community sample of adults with a history of NSSI (N = 315). Results of 2 × 2 factorial ANOVAs testing the interactive effects of NSSI frequency (clinical, subclinical) and recency (current, past) revealed that current NSSI was consistently associated with poorer emotional and behavioral health (e.g., greater symptoms of depression, panic, and anxiety, worse emotion regulation, greater alcohol misuse). Results for NSSI frequency were more variable, though preliminary evidence suggested significant interactions of current NSSI and clinical frequency on emotion dysregulation, general anxiety, and panic. Possible clinical and empirical implications of the NSSI disorder frequency criteria proposed in DSM-5 are discussed.
Keywords: Nonsuicidal Self-Injury (NSSI), NSSI Frequency, NSSI Recency, NSSI Disorder, DSM-5, Diagnostic Criteria, Emotion Dysregulation
1. Introduction
Decades of research have established that intentionally causing physical injury to one’s body without intending to cause death, or nonsuicidal self-injury (NSSI), is associated with indicators of psychological dysfunction including suicidality (Hamza et al., 2012), symptoms of psychopathology (Giletta et al., 2012; Gollust et al., 2008), and difficulties managing emotions and interpersonal relationships (Saraff and Pepper, 2014). While the aforementioned research has clearly established NSSI as being of clinical concern, there has been considerable debate regarding whether NSSI should be considered a standalone, diagnosable mental health disorder or whether it is more appropriately considered a symptom of general psychiatric distress (see Zetterqvist, 2015 for a review). Nonetheless, NSSI disorder was included in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), as a condition for further study (i.e., Section III: Emerging Measures and Models; American Psychiatric Association [APA], 2013). The proposed criteria of NSSI disorder are repeated self-injurious behaviors over the past year (Criterion A), which are maintained by intrapersonal and interpersonal reinforcement (Criterion B), associated with NSSI-related interpersonal difficulties, negative moods, or internal preoccupation (Criterion C), are not socially sanctioned (Criterion D), and are associated with distress or interference (Criterion E). Because inclusion or exclusion of an NSSI disorder in future versions of the DSM could have significant implications for treatment access and/or cost for the many millions of individuals who engage in this form of self-harm (Klonsky, 2011; Muehlenkamp et al., 2012; Swannell et al., 2014), more research on facets of NSSI included in the proposed criteria is of high priority.
The value of NSSI frequency and recency as indicators of psychopathology is worthy of additional empirical attention – particularly among general community samples of adults – because these facets of NSSI have been examined almost exclusively among select clinical samples, adolescents, and undergraduate students (though see Andover, 2014; Turner et al., 2013 for studies conducted with community adults). NSSI frequency refers to the number of times an individual has engaged in NSSI behavior, while recency refers to the amount of time since NSSI behavior has occurred. Individuals must have self-injured on at least five days during the past year to meet criteria for the proposed disorder, as per the DSM-5 (APA, 2013). Because both recency and frequency contribute to Criterion A of the proposed NSSI disorder, more evidence is needed to determine the utility of the proposed criteria among a variety of age groups and clinical presentations. Specifically, the following questions must be empirically examined: (1) whether NSSI frequency and recency are both associated with impairment and (2) whether there is an interaction between frequency and time, where the combination of higher frequency and recency indicative of disorder is associated with more impairment than either feature alone.
Current evidence suggests that depressive symptoms and hopelessness discriminate between individuals who endorse past-year NSSI engagement and those with a history of NSSI engagement over a year prior (Taliaferro and Muehlenkamp, 2015). People who have discontinued NSSI also report better emotional and interpersonal functioning than those who continue to self-injure (Andrews et al., 2013; Rotolone and Martin, 2012), further suggesting that NSSI recency is clinically relevant. NSSI frequency also positively correlates with suicidality (Ammerman et al., 2016; Anestis et al., 2013; Guan et al., 2012), including lethality and number of suicide attempts (Andover and Gibb, 2010), anxiety (Di Pierro et al., 2012), and depression (Glenn and Klonsky, 2011; Weierich and Nock, 2008). However, no research has examined a potential interaction between NSSI frequency and recency, despite the criteria’s assumption that NSSI is expected to be less problematic as a historical experience rather than an ongoing behavioral pattern.
Therefore, the purpose of this study was to examine NSSI frequency and recency in relation to psychopathology (symptoms of depression and anxiety), transdiagnostic mechanisms of psychopathology (emotion dysregulation), and indices of behavioral dysregulation (alcohol abuse, eating pathology). We hypothesized that higher frequency and current NSSI would each be associated with greater symptomatology. We also predicted interactions between frequency and recency such that among those with higher frequency NSSI, symptoms would be greater among individuals with current NSSI compared to individuals who had discontinued this behavior at least a year prior.
2. Method
2.1 Participants and procedure
Participants were 315 adults with a history of NSSI (Mage = 30.73, SDage = 9.09, 68.8% Female, 80.7% White) who were recruited via Amazon Mechanical Turk and completed survey measures online via Qualtrics. People in this study were selected from a larger sample of MTurk workers (N = 1128) who completed measures to be considered for several other studies, including one that focused on NSSI and suicidality (i.e., Zielinski et al., 2017)1. Individuals from the larger sample were included in this investigation if they endorsed a history of NSSI by means of skin cutting, carving, or burning or self-punching.
MTurk is an online worker platform which numerous studies have supported as a valid source of research data (Buhrmester et al., 2011; Casler et al., 2013), including recruitment of clinical populations (Raines et al., 2015; Shapiro et al., 2013; Taylor et al., 2014). All workers were paid a small amount of money ($3 US) for completing a series of surveys and were required to: (1) live in the United States2 and (2) evidence a positive worker history (i.e., a payment approval rating of 90% or greater on previously completed work). The procedures for this study were approved by the institutional review board at the University of Arkansas.
2.2 Study measures
2.2.1 Psychopathology and behavioral dysregulation
The 21-item Depression Anxiety Stress Scale (DASS-21; Henry and Crawford, 2005) was used to assess symptoms of depression, general anxiety, and panic. The measure contains three subscales consisting of seven items each: “Depression” which indexes depressive symptoms, “Stress” which indexes general anxiety symptoms, and “Anxiety” which indexes physiological symptoms of anxiety (e.g., heart racing, shortness of breath) associated with panic. All items are rated on a 4-point Likert type scale ranging from 0 (Did not apply to me at all) to 3 (Applied to me very much or most of the time). Subscale scores range from 0–42 (after raw scores are multiplied by two to map on to the scoring of the original DASS; Lovibond and Lovibond, 1995), with higher summed scores indicating more symptoms. Internal consistency in this sample was good or excellent for all subscales (α = 0.85 for Depression, α = 0.94 for Anxiety, and α = 0.89 for Stress).
The 10-item Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993) was used to index current alcohol use problems as an indicator of current behavioral dysregulation. The AUDIT, which was only completed by individuals who endorsed alcohol use (≥ 12 drinks) during the past year, includes items assessing alcohol consumption frequency and number of drinks, as well as characteristics of hazardous/harmful drinking and alcohol addiction (e.g., needing to drink first thing in the morning, failing to meet expectations due to use). Items are rated on a variable response scale ranging from 0 to 4. Total scores on the measure therefore range from 0–40, with higher summed scores indicating a greater likelihood of hazardous/harmful alcohol use. Internal consistency in this sample was good (α = 0.85).
The 22-item Eating Disorder Diagnostic Scale (Stice et al., 2000) was used to assess eating pathology, and was designed to index the presence of DSM-IV eating disorders. and includes questions about eating restriction, binge eating, and purging behaviors, as well as body attitudes. The scale uses a combination of Likert-type, yes/no and frequency responses; due to the variability in response types, an alpha score cannot be calculated for this measure. We used a composite score as described by Stice et al. (2000) which involved summing standardized (i.e., z) scores to all items except items assessing height, birth control use and amenorrhea.
2.2.2 Transdiagnostic mechanisms of psychopathology
The 36-item Difficulties in Emotion Regulation Scale (Gratz and Roemer, 2004) was used to assess current emotion dysregulations. Items primarily focus on aspects of emotion regulation during times of distress, and are rated on a 5-point Likert type scale ranging from 1 (Almost never) to 5 (Almost always). Consistent with recommendations by Bardeen and colleagues (2012), the awareness subscale was omitted due to poor psychometric properties. Total scores on the revised measure range from 30–150, with greater scores indicating greater problems in emotion regulation. Internal consistency in this sample was excellent (α = .96).
2.2.3 Non-suicidal self-injury
Selected items from the Deliberate Self-Harm Inventory (DSHI; Gratz, 2001) were used to assess NSSI behavior across four different methods (skin cutting, carving, and burning, self-punching). The selected methods have been invariably conceptualized as NSSI, and have been included in all primary NSSI measures used in past research (which do vary in their inclusion or exclusion of other behaviors). Items assessed current (within the past 12 months) and past engagement, and lifetime frequency of occurrence. Participant responses of the DSHI were used to create dichotomous variables representing for NSSI frequency and recency. We considered NSSI in the past 12 months to be current, while NSSI prior to 12 months was considered historical. Based on the DSM-5 proposed criteria (APA, 2013), we considered frequency of NSSI that exceeded 5 occurrences to be clinical, while frequency under 5 occurrences was considered subclinical. Because the DSHI asks respondents to indicate the number of cumulative lifetime NSSI incidents, rather than specify the number of days on which the person engaged in NSSI during the past year, our approach diverges somewhat from the DSM-5 proposed criteria. Specifically, we remain consistent with DSM-5 in terms of requiring at least 5 instances of NSSI behavior, but our use of a lifetime assessment does not align with the time frame over which the DSM-5 criteria suggests this behavior should occur to be considered disordered.
3. Results
3.1 Data preparation
Data on our predictor and criterion variables was examined for compatibility with the assumptions of two-way analysis of variance prior to analyses (i.e., normality, homogeneity of variances). Five participants were excluded due to missing data on one or more NSSI variables, leaving a total sample of 310 for primary analyses.
3.2 NSSI frequency and recency
Sample characteristics are reported in Table 1, separately by NSSI frequency and recency categories. In our sample of 310 adults with a history of NSSI, 22.6% (n = 70) reported NSSI in the last 12 months and 54.2% (n = 168) reported NSSI on 5 or more lifetime occasions. The most common past NSSI method in the sample was skin cutting (63.9% endorsed; n = 198), though only 7.4% of the sample reported skin cutting in the past year (n = 23). Self-punching was the most commonly endorsed current NSSI method (13.9% of sample endorsed; n = 43), persisting for almost a third of participants who reported self-punching in their lifetime (36.8%; n = 114).
Table 1.
Descriptive Data for Demographic Data and Baseline Questionnaires
| Past NSSI | Current NSSI | |||
|---|---|---|---|---|
| Subclinical | Clinical | Subclinical | Clinical | |
|
M or n (SD or %) n = 124 |
M or n (SD or %) n = 116 |
M or n (SD or %) n = 18a |
M or n (SD or %) n = 52 |
|
|
Demographics
| ||||
| Age | 33.32 (10.42) | 29.58 (7.53) | 28.89 (6.71) | 27.92 (8.24) |
| Sex | ||||
| Male | 44 (35.5%) | 25 (21.6%) | 8 (44.4%) | 18 (34.6%) |
| Female | 80 (64.5%) | 90 (77.6%) | 10 (55.6%) | 33 (63.5%) |
| Transgender | – | 1 (0.9%) | – | 1 (1.9%) |
| Race | ||||
| White (non-Hispanic) | 94 (75.8%) | 101 (87.1%) | 15 (83.3%) | 40 (76.9%) |
| African American | 10 (8.1%) | – | 1 (5.6%) | 4 (7.7%) |
| Hispanic/Latino | 10 (8.1%) | 7 (6.0%) | – | 4 (7.7%) |
| Asian American | 4 (3.2%) | 4 (3.4%) | 2 (11.1%) | 3 (5.8%) |
| Other | 6 (4.8%) | 4 (3.5%) | – | 1 (1.9%) |
| Marital Status | ||||
| Never married | 66 (53.2%) | 73 (62.9%) | 12 (66.7%) | 37 (71.2%) |
| Married | 41 (33.1%) | 31 (26.7%) | 2 (11.1%) | 10 (19.2%) |
| Previously married | 13 (10.5%) | 12 (10.3%) | 3 16.7%) | 5 (9.6%) |
| Employment Status | ||||
| Unemployed | 32 (25.8%) | 39 (33.6%) | 5 (27.8%) | 16 (30.8%) |
| Part time | 30 (24.2%) | 37 (31.9%) | 5 (27.8%) | 16 (30.7%) |
| Full time | 62 (50.0%) | 40 (34.5%) | 8 (44.4%) | 20 (38.5%) |
|
Outcome Measures | ||||
| Emotion dysregulation | 71.91 (23.25) | 77.38 (23.67) | 76.39 (17.52) | 99.13 (25.25) |
| Depression | 9.16 (8.38) | 11.34 (10.05) | 13.44 (8.86) | 16.15 (10.31) |
| Anxiety/Worry | 15.03 (9.83) | 16.43 (10.08) | 15.56 (9.98) | 24.58 (10.01) |
| Panic | 13.42 (10.86) | 14.90 (12.27) | 17.67 (11.44) | 24.50 (11.80) |
| Alcohol problemsb | 8.17 (5.31) | 8.30 (5.75) | 10.21 (8.03) | 11.00 (8.37) |
| Eating pathology | 2.03 (12.19) | 4.02 (11.42) | 4.52 (16.29) | 7.73 (13.62) |
Notes: Clinical NSSI refers to 5 or more lifetime incidents and subclinical NSSI refers to 4 or fewer incidents. Current NSSI refers to NSSI in the past 12 months and past NSSI refers to NSSI occurring more than 12 months prior to data collection.
Missing marital status data on one participant,
Because the AUDIT was only completed by individuals who endorsed drinking in the past year, the total n for these analyses was 200 (81 past subclinical NSSI, 71 past clinical NSSI, 14 current subclinical NSSI, 34 current clinical NSSI).
3.3 Relationship of NSSI frequency and recency to current symptoms of depression, anxiety, and panic
Three (2 × 2) factorial ANOVAs testing the interactive effects of NSSI frequency (clinical, subclinical; assessed across lifetime) and recency (current, past) were conducted on the outcomes of depression, anxiety, and panic symptoms as measured by the DASS-21. There was a significant main effect of NSSI recency on both depression, F(1, 306) = 10.24, p = 0.002, and panic F(1, 306) = 15.60, p < .001, such that current NSSI was associated with greater symptomology. There was also a significant main effect of lifetime NSSI frequency on panic, F(1, 306) = 5.62, p = 0.02, with clinical frequency being associated with greater panic symptoms. There was not a significant main effect of lifetime NSSI frequency on depressive symptoms, F(1, 306) = 2.97, p = 0.09, and no significant interaction effects for either depression, F(1, 306) = 0.03, p = 0.85, or panic, F(1, 306) = 2.33, p = 0.13.
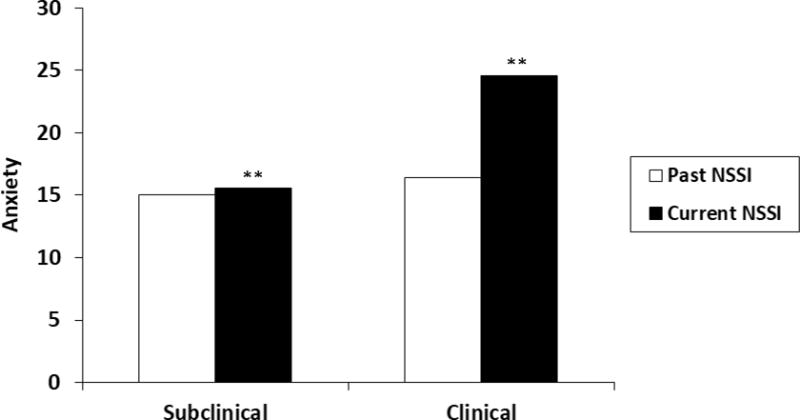
For general anxiety, results revealed significant main effects of both recency, F(1, 306) = 8.28, p = 0.004, and lifetime frequency, F(1, 306) = 11.96, p = 0.001. These were qualified by a significant interaction between lifetime frequency and recency, F(1, 306) = 6.34, p = 0.01 (see Figure 1). Simple effects analyses revealed that among individuals endorsing clinical NSSI frequency, current NSSI was associated with higher anxiety than past NSSI (p < 0.001), while people with past and current subclinical NSSI reported similar current anxiety symptoms (p = 0.835).
Figure 1.
3.4 Relationship of NSSI frequency and recency to behavioral dysregulation
A 2 (NSSI frequency) × 2 (NSSI recency) ANOVA was conducted on alcohol use problems as measured by the AUDIT. Results revealed a main effect of recency, F(1, 200) = 4.49, p = 0.04. However, Levene’s test of Equality of Error Variances was significant, F(3, 196) = 4.971, p = 0.002, indicating violation of the ANOVA assumption of homogeneity of variance. Therefore, we also conducted a more stringent Welch test examining recency and found that people endorsing NSSI during the past year evidenced greater alcohol problems than those who did not (Welch = 4.04, p = 0.049). There was no main effect of lifetime NSSI frequency and the interaction between NSSI frequency and recency was not significant (both Fs < 1).
A similar 2 × 2 ANOVA was conducted on eating pathology (EDDS composite score). There was not a significant main effect of lifetime frequency, F(1, 306) = 1.92, p = 0.18, nor of recency, F(1, 306) = 2.72, p = 0.10. The means were in the expected directions (e.g., higher means in the clinical NSSI group and higher means in the current NSSI group), though the differences were not statistically significant. There was also not a significant interaction between NSSI frequency and recency, F(1, 306) = 0.11, p = 0.74.
3.5 Relationship of NSSI frequency and recency to current emotion dysregulation
A two-way ANOVA evaluated the effect of lifetime NSSI frequency and NSSI recency on current emotion dysregulation as measured by the DERS. In addition to significant main effects of recency, F(1, 306) = 13.65, p < 0.001, and frequency, F(1, 306) = 15.79, p < 0.001, there was a significant interaction between NSSI frequency and recency, F(1, 306) = 5.92, p = 0.016 (See Figure 2). Simple effects analyses revealed that for people with clinical levels of NSSI, those with current NSSI had greater emotion dysregulation than those with past NSSI (p < 0.001). However, there were no differences in emotion dysregulation based on recency for people with subclinical NSSI levels (p = 0.45).
Figure 2.
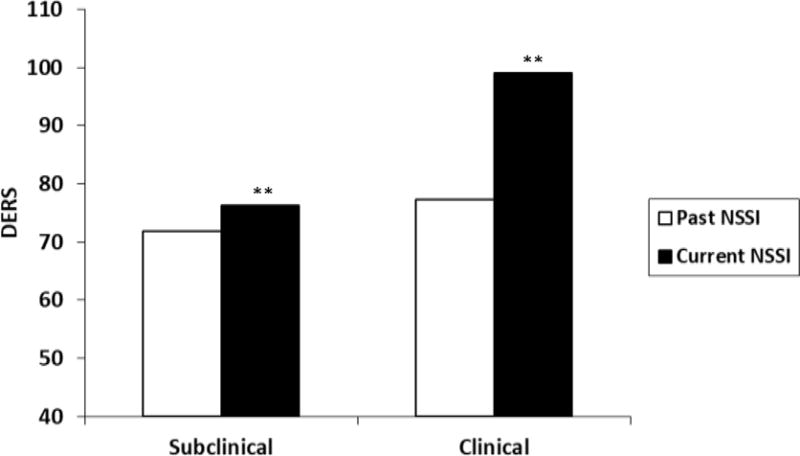
Note for figures: ** indicates a statistically significant difference (p = 0.01 for Figure 1 and p < 0.001 for Figure 2).
4. Discussion
This study investigated the relations between NSSI frequency and recency – facets of NSSI that were prioritized in the diagnostic criteria for NSSI Disorder (APA, 2013) – and indices of current emotional and behavioral impairment. People who endorsed current NSSI reported significantly poorer psychological health than individuals who had last self-injured over one year prior, including greater symptoms of depression, panic, and anxiety, emotion dysregulation, and alcohol misuse. In contrast, NSSI frequency was less consistently associated with clinical outcomes. Anxiety, panic, and emotion dysregulation were elevated for the clinical NSSI group compared to the non-clinical NSSI group, but degree of depression and alcohol misuse did not differ. Finally, we found that the proposed “disorder” group—who engaged in NSSI at clinical frequency levels (e.g., 5 or more times) and who endorsed NSSI in the past year – indeed seemed to have greater dysfunction than the other groups, at least in terms of poorer emotion dysregulation and greater general anxiety. Together, the only outcome we assessed that was not significantly discriminated by NSSI recency and/or frequency was eating pathology.
Our study thus converges with prior evidence that both recently and frequency are clinically-relevant features of NSSI behavior (Ammerman et al., 2016; Andrews et al., 2013; Manca et al., 2014; Rotolone and Martin, 2012; Taliaferro and Muehlenkamp, 2015; Weierich and Nock, 2008). Our results may also lend support to the inclusion of criteria that consider recency and frequency in the proposed NSSI disorder (APA, 2013), particularly because the differential patterns of association between NSSI frequency and recency may indicate that they are discrete behavioral indicators. It may be that NSSI recency is an indicator of current levels of broad clinical impairment that has recently overwhelmed an individual’s ability to cope through other means, while frequency associates with particular symptoms. For example, individuals experiencing symptoms characterized by high levels of arousal (e.g., anxiety, panic) may engage in NSSI more frequently as a means of regulating intense emotions, while individuals suffering from symptoms of depression may experience lower levels of arousal, and thus may be less inclined to engage in the behavior as frequently in order to regulate their emotions. However, if we take our results at face value, we found that the clinical cut-point of 5+ incidents, which is currently supported only by a single study (Ammerman et al., 2016), was less consistently associated with the emotional and behavioral impairment indices that were elevated for individuals who endorsed recent NSSI. Therefore, we also assert that further consideration of how to best approach the NSSI disorder frequency criteria is warranted – particularly in light of recent research by Muehlenkamp and colleagues (2017) which found evidence for a vastly different frequency cut point (e.g., 25 days in the last year) among a sample of inpatient adolescents.
For example, it may be that a different frequency cut-point would have better converged with our recency results, or that a defined time-period of occurrence (which was not indexed by this study) is critical to the five-incident cut-point to be useful for diagnosis. The latter seems unlikely given that NSSI frequency counts have been examined in a variety of ways, including considering number of lifetime incidents, and still been associated with poorer outcomes (e.g., Borrill et al., 2009; Nock et al., 2006; You et al., 2011). Alternatively, specifying a particular clinical cut-point could have minimal incremental value in identifying when an individual’s NSSI behavior is causing impairment worthy of categorical “disorder” status. Use of clinical cut-points inherently introduce a degree of arbitrariness to clinical diagnoses (Skodol, 2014). Moreover, data from a very large sample of university students found that NSSI frequency had a curvilinear relationships with suicidal ideation, plan, and attempts where risk for self-injurious thoughts and behaviors peaked and then decreased (Paul et al., 2015); this data indicates that the relation between NSSI frequency and pathology or impairment may not be as straightforward as can be summed up by a defined frequency cut point. Because diagnostic status is typically associated with treatment access, it is critical for the field to specifically investigate whether use of a defined frequency cut-point reliably and incrementally increases the validity of the NSSI disorder diagnosis beyond the performance of a more flexible frequency criteria (e.g., a requirement of “repetitive” NSSI behavior in which a pre-determined cut-point is not defined).
Our study had several notable strengths and limitations. Limitations included the use of cross-sectional methodology in which our frequency variable was a lifetime count variable instead of the 12-month, 5-incidence count variable proposed in DSM-5. We therefore cannot determine whether people who have injured themselves 5 or more times in the past year differ from people who have injured on 5 or more occasions over the course of a longer time interval. Additionally, all variables were measured via self-report and did not include an examination of interpersonal impairment, though interpersonal motives are linked to some NSSI behavior. While self-report measures do allow for greater privacy and may engender more honest responses, we recognize that such measures are amenable to distortion. Strengths of this study include the use of a community sample, investigation of NSSI frequency and recency together in the same sample, and consideration of a wide array of transdiagnostic emotional and behavioral criterion variables.
The results of this study should also be considered in context of the larger literature base that has compared people with a history of NSSI to people with no NSSI history, as well as the emerging literature on NSSI cessation. Recent research on NSSI cessation, which has begun to examine whether discontinuing NSSI is associated with improvement, has also found that cessation is associated with greater cognitive reappraisal, lower emotional suppression, and better interpersonal functioning (Andrews et al., 2013; Rotolone and Martin, 2012), suggesting that the problems associated with NSSI may dissipate over time; some have even hypothesized that growth occurs post-NSSI-cessation (Whitlock et al., 2015). Conversely, it is possible that improvements (e.g., in emotion regulation abilities and the development of important social relationships) predict cessation rather than the reverse. It is also possible that mental health treatment may influence these findings. However, beginning to consider interactions between NSSI recency and frequency in relation to psychopathology and emotion dysregulation (particularly in a community sample) is in many ways a novel deviation from the dominant historical approach to NSSI assessment, which often considered NSSI history as a stable risk factor for future pathology rather than a behavior that acutely increases risk.
Ultimately, from a clinical perspective, the question of diagnosis may matter less than what features of NSSI behavior can tell a provider about a particular individual. People engage in NSSI for different reasons, which may influence the form, frequency, and recency of NSSI. As such, a comprehensive functional evaluation of NSSI should remain the gold standard for clinical evaluation, as researchers continue to further solidify what individual components of this behavior can tell us about the person’s current struggles and expected trajectory.
Highlights.
Examined frequency and recency of NSSI as predictors of psychopathology.
Current NSSI was consistently related to poorer emotional and behavioral health.
NSSI recency and frequency interacted to predict emotion dysregulation and anxiety.
Implications for the proposed NSSI disorder criteria in DSM-5 are discussed.
Acknowledgments
5. Financial acknowledgements
Preparation of this work was supported in part by grants R25DA037190 (PI: Beckwith) and T32DA022981 (PI: Kits) from the National Institute on Drug Abuse, which support the first author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Of note, participants were not aware of the inclusion/exclusion criteria for these additional studies, but did consent to being considered for additional research based on the baseline measures.
Participants from across the US were represented in our sample and identified the region in which they were living as follows: 18.1% Northeast, 22.5% Midwest, 25.7% Southeast, 10.8% Southwest, 22.9% West.
References
- American PsychiatricAssociation. Diagnostic and Statistical Manual of Mental Disorders. 5th. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Ammerman BA, Jacobucci R, Kleiman EM, Muehlenkamp JJ, McCloskey MS. Development and validation of empirically derived frequency criteria for NSSI disorder Using exploratory data mining. Psychol Assess. 2016;29:221–231. doi: 10.1037/pas0000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andover MS. Non-suicidal self-injury disorder in a community sample of adults. Psychiatry Res. 2014;219:305–310. doi: 10.1016/j.psychres.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andover MS, Gibb BE. Non-suicidal self-injury, attempted suicide, and suicidal intent among psychiatric inpatients. Psychiatry Res. 2010;178:101–105. doi: 10.1016/j.psychres.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Andrews T, Martin G, Hasking P, Page A. Predictors of continuation and cessation of nonsuicidal self-injury. J Adolesc Heal. 2013;53:40–46. doi: 10.1016/j.jadohealth.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Anestis MD, Knorr AC, Tull MT, Lavender JM, Gratz KL. The importance of high distress tolerance in the relationship between nonsuicidal self-injury and suicide potential. Suicide Life-Threatening Behav. 2013;43:663–675. doi: 10.1111/sltb.12048. [DOI] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA, Orcutt HK. An examination of the latent structure of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2012;34:382–392. doi: 10.1007/s10862-012-9280-y. [DOI] [Google Scholar]
- Borrill J, Fox P, Flynn M, Roger D. Students who self-harm: Coping style, Rumination and Alexithymia. Couns Psychol Q. 2009;22:361–372. doi: 10.1080/09515070903334607. [DOI] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect Psychol Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Casler K, Bickel L, Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput Human Behav. 2013;29:2156–2160. doi: 10.1016/j.chb.2013.05.009. [DOI] [Google Scholar]
- Di Pierro R, Sarno I, Perego S, Gallucci M, Madeddu F. Adolescent nonsuicidal self-injury: The effects of personality traits, family relationships and maltreatment on the presence and severity of behaviours. Eur Child Adolesc Psychiatry. 2012;21:511–520. doi: 10.1007/s00787-012-0289-2. [DOI] [PubMed] [Google Scholar]
- Giletta M, Scholte RHJ, Engels RCME, Ciairano S, Prinstein MJ. Adolescent non-suicidal self-injury: a cross-national study of community samples from Italy, the Netherlands and the United States. Psychiatry Res. 2012;197:66–72. doi: 10.1016/j.psychres.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Prospective Prediction of Nonsuicidal Self-Injury: A 1-Year Longitudinal Study in Young Adults. Behav Ther. 2011;42:751–762. doi: 10.1016/j.beth.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollust SE, Eisenberg D, Golberstein E. Prevalence and Correlates of Self-Injury Among University Students. J Am Coll Heal. 2008;56:491–498. doi: 10.3200/JACH.56.5.491-498. [DOI] [PubMed] [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. J Psychopathol Behav Assess. 2001;23:253–263. doi: 10.1023/A:1012779403943. [DOI] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Guan K, Fox KR, Prinstein MJ. Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. J Consult Clin Psychol. 2012;80:842–849. doi: 10.1037/a0029429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza Ca, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clin Psychol Rev. 2012;32:482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychol Med. 2011;41:1981–6. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Manca M, Presaghi F, Cerutti R. Clinical specificity of acute versus chronic self-injury: Measurement and evaluation of repetitive non-suicidal self-injury. Psychiatry Res. 2014;215:111–119. doi: 10.1016/j.psychres.2013.10.010. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Brausch AM, Washburn JJ. How much is enough? Examining frequency criteria for NSSI disorder in adolescent inpatients. J Consult Clin Psychol. 2017;85:611–619. doi: 10.1037/ccp0000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6:10. doi: 10.1186/1753-2000-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Nonsuicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Paul E, Tsypes A, Eidlitz L, Ernhout C, Whitlock J. Frequency and functions of non-suicidal self-injury: Associations with suicidal thoughts and behaviors. Psychiatry Res. 2015;225:276–282. doi: 10.1016/j.psychres.2014.12.026. [DOI] [PubMed] [Google Scholar]
- Raines AM, Boffa JW, Allan NP, Short NA, Schmidt NB. Hoarding and eating pathology: The mediating role of emotion regulation. Compr Psychiatry. 2015;57:29–35. doi: 10.1016/j.comppsych.2014.11.005. [DOI] [PubMed] [Google Scholar]
- Rotolone C, Martin G. Giving up self-injury: A comparison of everyday social and personal resources in past versus current self-injurers. Arch Suicide Res. 2012;16:147–158. doi: 10.1080/13811118.2012.667333. [DOI] [PubMed] [Google Scholar]
- Saraff PD, Pepper CM. Functions, lifetime frequency, and variety of methods of nonsuicidal self-injury among college students. Psychiatry Res. 2014;219:298–304. doi: 10.1016/j.psychres.2014.05.044. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, Mueller PA. Using Mechanical Turk to study clinical populations. Clin Psychol Sci. 2013;1:213–220. doi: 10.1177/2167702612469015. [DOI] [Google Scholar]
- Skodol AE. Personality disorder classification: stuck in neutral, how to move forward? Curr Psychiatry Rep. 2014;16:480. doi: 10.1007/s11920-014-0480-x. [DOI] [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol Assess. 2000;12:123–31. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide Life-Threatening Behav. 2014 doi: 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- Taliaferro L, Muehlenkamp J. Factors associated with current versus lifetime self-injury among high school and college students. Suicide Life-Threatening Behav. 2015;45:84–97. doi: 10.1111/sltb.12117. [DOI] [PubMed] [Google Scholar]
- Taylor S, McKay D, Crowe KB, Abramowitz JS, Conelea CA, Calamari JE, Sica C. The sense of incompleteness as a motivator of obsessive-compulsive symptoms: An empirical analysis of concepts and correlates. Behav Ther. 2014;45:254–262. doi: 10.1016/j.beth.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Layden BK, Butler SM, Chapman AL. How often, or how many ways: Clarifying the relationship between non-suicidal self-injury and suicidality. Arch Suicide Res. 2013;17:397–415. doi: 10.1080/13811118.2013.802660. [DOI] [PubMed] [Google Scholar]
- Weierich MR, Nock MK. Posttraumatic stress symptoms mediate the relation between childhood sexual abuse and nonsuicidal self-injury. J Consult Clin Psychol. 2008;76:39–44. doi: 10.1037/0022-006X.76.1.39. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Prussien K, Pietrusza C. Predictors of self-injury cessation and subsequent psychological growth: results of a probability sample survey of students in eight universities and colleges. Child Adolesc Psychiatry Ment Health. 2015;9:19. doi: 10.1186/s13034-015-0048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You J, Leung F, Fu K, Lai CM. The prevalence of nonsuicidal self-injury and different subgroups of self-injurers in Chinese adolescents. Arch Suicide Res. 2011;15:75–86. doi: 10.1080/13811118.2011.540211. [DOI] [PubMed] [Google Scholar]
- Zetterqvist M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: A review of the empirical literature. Child Adolesc Psychiatry Ment Health. 2015;9:31. doi: 10.1186/s13034-015-0062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski MJ, Veilleux JC, Samuel Winer E, Nadorff MR. A short-term longitudinal examination of the relations between depression, anhedonia, and self-injurious thoughts and behaviors in adults with a history of self-injury. Compr Psychiatry. 2016;73:187–195. doi: 10.1016/j.comppsych.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


