Dear Editor,
I am Dr. Zhao PQ, from the Department of Ophthalmology, Xin Hua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China. I write to present a case report of tissue plasminogen activator (tPA)-assisted vitrectomy in the early treatment of acute massive suprachoroidal hemorrhage (SCH) complicating cataract surgery.
SCH is a vision-threatening complication associated with certain surgical procedures, such as cataract extraction, glaucoma filtering surgery, retinal detachment repair, and penetrating trauma. Generally, SCH has a guarded prognosis and poor visual outcome. Surgical drainage is a topic of much controversy. A suggested time for surgical drainage is 10-14d when the hemorrhagic clot begins to liquefy. However, if adequate thrombolysis can be achieved earlier, retinal complications may be prevented or reduced. Previously, several reports have been published about tPA in the treatment of vitreoretinal diseases[1]. However, no reports were about tPA assisted vitrectomy in the management of acute massive SCH complicating cataract surgery. Here we present a patient with massive SCH during cataract surgery who underwent an early successful tPA-assisted vitrectomy and attained good visual outcome. It may be the earliest drainage of the clot by recombinant tPA (r-tPA) in SCH after cataract extraction surgery up to our knowledge.
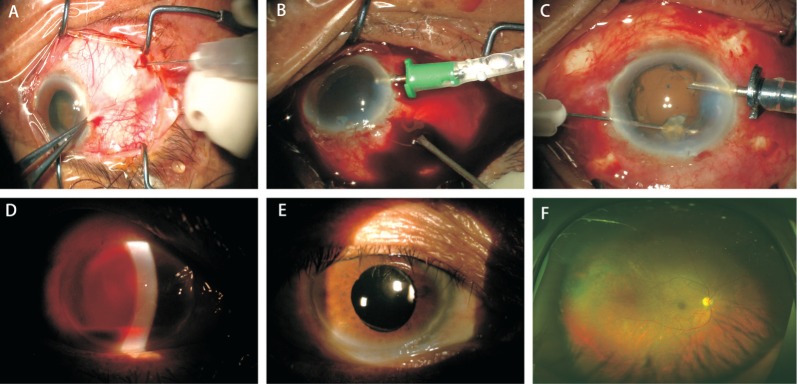
A 73-year-old male underwent phacoemulsification surgery for cataract of right eye in other hospital. SCH was complicated during the surgery with ruptured posterior capsule. Four days after surgery, the patient was referred to our clinic with visual acuity of light perception (suspected) in right eye. The right eye was aphakia with a few lens cortex residue and massive SCH (Figure 1A). The intraocular pressure (IOP) was 20 mm Hg. Ultrasound scan further showed kissing choroidal detachment of all the four quadrants (Figure 1B). He had a history of hypertension but with a normal blood pressure at the time of examination.
Figure 1. Acute SCH after cataract surgery.
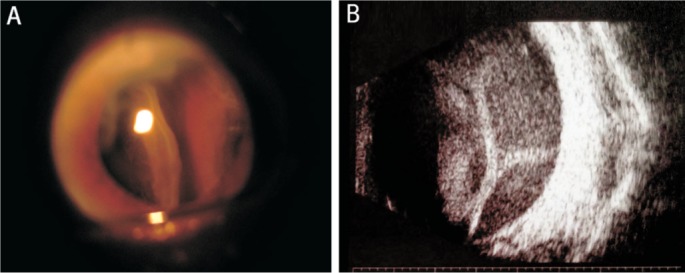
A: Acute massive SCH 4d later after cataract surgery under slit-lamp biomicroscope; B: B-mode echo images showed choroidal detachment configuration of all the four quadrants.
The patient was scheduled for r-tPA suprachoroidal cavity injection the following day. r-tPA (alteplase, 10 µg/0.2 mL) was injected into each quadrant of the suprachoroidal space (Figure 2A). The next day, sclerotomy 5 mm behind the limbus were created in four quadrants to drain the liquefied hemorrhage with the anterior chamber maintainer placed at the limbus (Figure 2B). We chose the location where the choroid detached most and the direction of microvitreoretinal (MVR) blade was oblique. Standard three-port vitrectomy was performed after drainage at the same session. The residual cortex was firstly removed by lensectomy (Figure 2C). Vitrectomy, liquid gas exchange combined with C3F8 tamponade were performed later. The next day after PPV, 2 mm hyphema was noticed, but the IOP remained normal (Figure 2D). The hyphema was spontaneously absorbed 6d later. During the follow up, the choroid was attached. Secondary IOL was implanted 10mo later (Figure 2E, 2F). Best corrected vision was 30/60.
Figure 2. r-tPA assisited vitrectomy in SCH complicating catract surgery.
A: r-tPA (alteplase, 10 µg/0.2 mL) was injected into each quadrant of the suprachoroidal space; B: Surgery performed the next day after r-tPA injection. Posterior sclerotomy 4-5 mm behind the limbus were created in four quadrants to drain the liquefied hemorrhage with anterior chamber maintainer; C: Removal of the residual cortex; D: Of 2 mm hyphema was noticed the next day after PPV; E: Secondary IOL was implanted 10mo later; F: Fundus photo showed the flat retina.
The actual incidence of SCH during or after cataract surgery is somewhat difficult to reliably estimate. The advent of phacoemulsification lens extraction, topical anesthesia, and clear corneal incision techniques have lowered the incidence of SCH secondary to cataract surgery from previously reported 0.2% to 0.03%-0.06%[2]. However, compared with normal situation, SCH will occur more frequently if there are surgical complications, such as posterior capsule rupture, or in pathologic myopia, or with systemic hypertension.
There is some disagreement on timing of surgery. Some authors suggest waiting 10-14d for the clot to liquefy, whereas others advocate early surgical intervention for better anatomic and visual outcome. Waiting for spontaneous resolution can result in retinal detachment when there is vitreous incarceration and lead to poor vision prognosis. In cases of extensive hemorrhage, patients have sustained vision loss from chronic atrophy or phthisis bulbi in the absence of prompt surgical intervention. Prompt drainage may provide the best chance for maintaining useful vision.
tPA is a naturally occurring thrombolytic enzyme which activates fibrin-bound plasminogen to plasmin. r-tPA has been reported in the successful treatment of various vitreoretinal diseases, including SCH after ocular trauma or retinal detachment repair[3]–[4]. Animal experiments have shown the efficacy of r-tPA in treating experimental SCHs[5]. r-tPA has been proved effective and safe.
Our results showed that an early two-step surgical strategy could lead to good visual outcomes for massive SCH after cataract surgery. The initial surgery is r-tPA suprachoroidal cavity injection 4-5d after SCH. Preoperative B-scan can be a guide to perform r-tPA suprachoroidal space injection. The combined SCH drainage and vitrectomy can be performed 1h later or the next day when the clot is liquefied. The timing of the combined SCH drainage and vitrectomy for secondary retinal detachment, vitreoretinal traction, vitreous hemorrhage, and/or dislocated lens fragments is critical. Perfluorocarbon liquid, has been used successfully in assisting the drainage of SCH. Differed from the report of SCH after retinal detachment repair, C3F8 tamponade was performed instead of silicone oil because the retina was at a good status in our case of SCH after cataract surgery[4].
Based on this case study, in which our patient has a fortunate outcome, we hypothesize that further study is warranted regarding the use of r-tPA in the timely treatment of acute SCH complicating cataract surgery.
Acknowledgments
Foundations: Supported by the National Natural Science Foundation of China (No.81500725; No.81770963; No.81470642); Shanghai Science and Technology Committee (No.15XD1502800).
Conflicts of Interest: Fei P, None; Jin HY, None; Zhang Q, None; Li X, None; Zhao PQ, None.
REFERENCES
- 1.Kamei M, Estafanous M, Lewis H. Tissue plasminogen activator in the treatment of vitreoretinal diseases. Semin Ophthalmol. 2000;15(1):44–50. doi: 10.3109/08820530009037850. [DOI] [PubMed] [Google Scholar]
- 2.Ling R, Cole M, James C, Kamalarajah S, Foot B, Shaw S. Suprachoroidal haemorrhage complicating cataract surgery in the UK: epidemiology, clinical features, management, and outcomes. Br J Ophthalmol. 2004;88(4):478–480. doi: 10.1136/bjo.2003.026138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto K, Matsumoto CS, Shinoda K, Watanabe E, Mizota A. Tissue plasminogen activator-assisted vitrectomy for ruptured eye with suprachoroidal hemorrhage. Case Rep Ophthalmol. 2012;3(2):258–261. doi: 10.1159/000342136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunjukunju N, Gonzales CR, Rodden WS. Recombinant tissue plasminogen activator in the treatment of suprachoroidal hemorrhage. Clin Ophthalmol. 2011;5:155–157. doi: 10.2147/OPTH.S16134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwon OW, Kang SJ, Lee JB, Lee SC, Yoon YD, Oh JH. Treatment of suprachoroidal hemorrhage with tissue plasminogen activator. Ophthalmologica. 1998;212(2):120–125. doi: 10.1159/000027295. [DOI] [PubMed] [Google Scholar]