Abstract
Background:
Differential diagnosis of periapical cysts and granulomas is required as their treatment modalities are different.
Aim:
The aim of this study was to evaluate the efficacy of cone beam computed tomography (CBCT) in the differential diagnosis of periapical cysts from granulomas.
Settings and Design:
A single-centered observational study was carried out in the Department of Conservative Dentistry and Endodontics, Dr. R. Ahmed Dental College and Hospital, using CBCT and dental operating microscope.
Methods:
Forty-five lesions were analyzed using CBCT scans. One evaluator analyzed each CBCT scan for the presence of the following six characteristic radiological features: cyst like-location, shape, periphery, internal structure, effect on the surrounding structures, and cortical plate perforation. Another independent evaluator analyzed the CBCT scans. This process was repeated after 6 months, and inter- and intrarater reliability of CBCT diagnoses was evaluated. Periapical surgeries were performed and tissue samples were obtained for histopathological analysis. To evaluate the efficacy, CBCT diagnoses were compared with histopathological diagnoses, and six receiver operating characteristic (ROC) curve analyses were conducted.
Statistical Analysis Used:
ROC curve, Cronbach's alpha (α) test, and Cohen Kappa (κ) test were used for statistical analysis.
Results:
Both inter- and intrarater reliability were excellent (α = 0.94, κ = 0.75 and 0.77, respectively). ROC curve with regard to ≥4 positive findings revealed the highest area under curve (0.66).
Conclusion:
CBCT is moderately accurate in the differential diagnosis of periapical cysts and granulomas.
Keywords: Area under curve, cone beam computed tomography, differential diagnosis, histopathology, periapical cyst, periapical granuloma, receiver operating characteristic
INTRODUCTION
One of the most frequently diagnosed pathologies of odontogenic origin is the periapical lesion.[1] This occurs due to the entry of microorganisms within the pulp canal system which release pro-inflammatory mediators into the periapical tissues due to which there is resorption of bone surrounding the root and periapical pathosis develops.[2]
One of the biggest queries in endodontics today is whether a periapical pathology is a cyst or granuloma. It is understood that periapical granulomas and periapical pocket cysts heal nonsurgically whereas a periapical true cyst requires surgery.[3]
However, the problem lies in the fact that presently there is no preoperative nonsurgical diagnostic method which can accurately assess the nature of the periapical pathology. Postoperative histopathological examination is the only confirmatory test of the nature of the lesion.[4,5]
Preoperative periapical radiographs are only 26%–48% accurate in diagnosing the periapical lesion.[6,7] It has been proved in several studies[8,9,10,11,12,13,14] that cone beam computed tomography (CBCT) can reveal periapical pathologies much better than periapical radiographs.
Currently, CBCT has been utilized in the place of periapical radiographs as a nonsurgical method for differentiating periapical cyst and granuloma.[4,15,16] However, limited studies[15,16,17] are there which validate the usefulness of CBCT in the differential diagnosis of periapical pathologies. The reliability and accuracy level of differential diagnosis of periapical cysts from granulomas was seen to be different in these studies. The CBCT finding was taken as potential preoperative diagnosis which was compared with the actual nature of the lesion through histopathological report of the biopsy sample. All CBCT-diagnosed cysts did not prove to be cysts histopathologically. Similarly, all CBCT-diagnosed granulomas were not granulomas and some were proved to be cysts. This is because all CBCT diagnostic features may not be present in all cysts and granulomas. However, its ability to diagnose a cyst preoperatively is convincing and has potential clinical significance that has been pointed by Guo et al.[17] in their study. Here lies the importance of assessing its reliability and accuracy as a preoperative diagnostic tool.
Keeping this in view, the present study was designed to evaluate the ability of CBCT in the differential diagnosis of periapical cysts and granulomas. Here, the CBCT images of the lesions were analyzed with the help of the fixed radiological features for provisional diagnoses which were then compared with histopathology reports. Presence of optimum number of CBCT features was determined to diagnose a lesion as a cyst. Subsequently, reliability and accuracy of CBCT were evaluated.
METHODS
Forty-five patients with periapical lesions diagnosed by clinical symptoms and radiographic findings in periapical radiographs were selected for the study. The minimum criterion was 5-mm diameter of the lesion. The study protocol was approved by the Institutional Ethics Committee. Consent form was signed by all the patients according to Helsinki Declaration.
Periapical radiolucency was imaged by MyRay CBCT scanner at the Probe Diagnostic Centre, Dr. R. Ahmed Dental College and Hospital. Fixed field of view volume was 7 cm × 7 cm × 7 cm. The gray levels were 4096 (12 bit). The scanner was operated at 90 kV and 10 mA. The Digital Imaging and Communications in Medicine format images were exported from MyRay CBCT scanner and imported into iRYS viewer software (MyRay CBCT, Kolkata, West Bengal, India). The minimum average diameter of 5 mm was checked through sagittal view of CBCT scan.
The set of diagnostic criteria for periapical cysts based on radiological features[18] was as follows:
Location - Apex of the tooth
Periphery – Corticated border
Shape – Curved or circular
Internal structure – Radiolucent
Effect on surrounding structures – Displacement and resorption of the roots
Cortical plate perforation – Present.
For each lesion, CBCT images were evaluated prior to histopathological examination and assigned a score on the basis of the number of the above radiologic features seen. For example, if the CBCT score of the lesion was 3, it meant that only three of the above six criteria were found to be present in the corresponding CBCT scan. The procedure of analysis of the CBCT scan was done by two separate evaluators having no interaction between them.
Since all the six criteria were not possessed by every CBCT-assessed lesion (e.g., cortical bone may not be perforated by a cyst), the minimum number of criteria in CBCT scan was required to be ascertained for diagnosing a cyst. For this purpose, six receiver operating characteristic (ROC) curve analyses were conducted. ROC curves provide measure of accuracy of any diagnostic test.[19] This was done by comparing CBCT findings with the corresponding histopathological report of the periapical lesion.
Hence, after CBCT analysis, endodontic therapy was performed. Subsequent to proper investigations, periapical surgery was done using standard clinical protocols under the view of the dental operating microscope. The specimen obtained was submitted to the Department of Oral and Maxillofacial Pathology, Dr. R. Ahmed Dental College and Hospital, for histopathological examination. The histopathological report was sent by the department only when the faculty oral pathologists were unanimous about the report. They were kept in dark about the CBCT analysis of the lesion.
Results of histologic analysis were tabulated against the corresponding score of the particular lesion for all 45 cases [Table 1]. Six scoring systems were used in which the 1st scoring system corresponded to a CBCT score (≥1), 2nd scoring system (≥2), and so on until the 6th scoring system (=6). Each lesion was evaluated by every scoring system, and the number of true-positive (TP), true-negative (TN), false-positive (FP), and false-negative (FN) cases were evaluated [Table 2]. Four CBCT scans showing different clinical situations are shown in Figures 1 and 2.
Table 1.
CBCT score and corresponding histopathological report
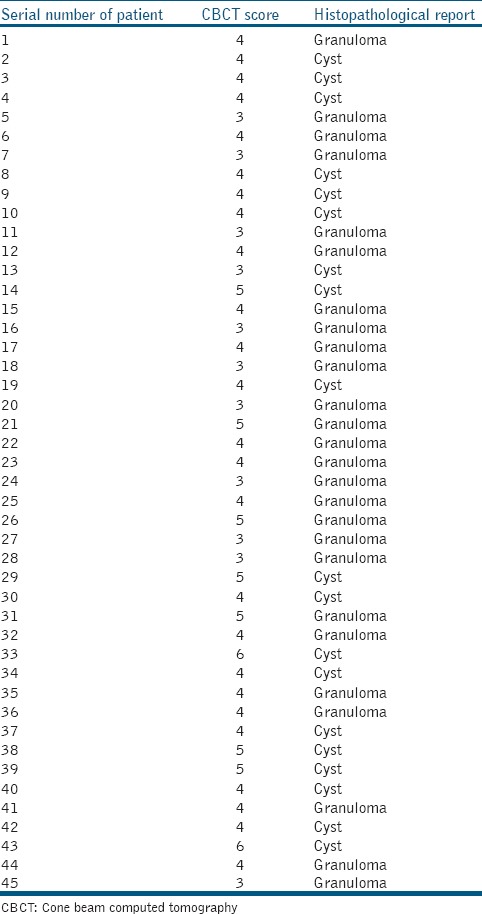
Table 2.
Evaluation of 45 lesions by six scoring systems
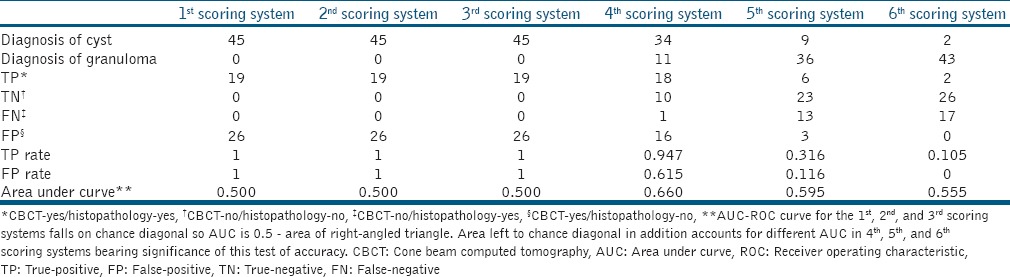
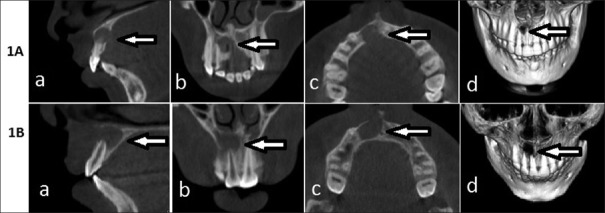
Figure 1.
A: Cyst in cone beam computed tomography and histology: Patient no. 8. (a) Sagittal view (b) coronal view (c) axial view (d) three-dimensional view. B: Cyst in cone beam computed tomography and granuloma in histology: Patient no. 12. (a) Sagittal view (b) coronal view (c) axial view (d) three-dimensional view
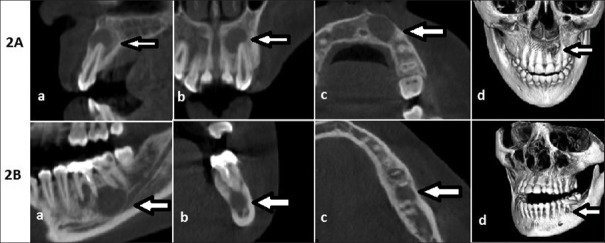
Figure 2.
A: Granuloma in cone beam computed tomography and histology: Patient no. 27. (a) Sagittal view (b) coronal view (c) axial view (d) three-dimensional view. B: Granuloma in cone beam computed tomography and cyst in histology: Patient no. 13. (a) Sagittal view (b) coronal view (c) axial view (d) three-dimensional view
The CBCT images were again evaluated 2nd time after 6 months by the two evaluators separately. Results of histopathological reports were kept in dark to them.
For intrarater reliability, two evaluations of each evaluator were tested through Cohen's Kappa (κ) which assesses the extent an evaluator agrees in two evaluations (κ ≥ 0.75 – excellent; 0.60 ≤ κ< 0.75 – good; 0.40 ≤ κ < 0.60 – intermediate; and κ < 0.40 – poor).
For interrater reliability, the evaluations of the two evaluators were tested through Cronbach's alpha (α) test which assesses the agreement among multiple evaluators (excellent – α ≥ 0.80; Good – 0.60 < α< 0.79; Intermediate – 0.40< α ≤ 0.60; Poor – α ≤ 0.40).
ROC curve is constructed from TP rate (TP/[TP + FN] ×100) and FP rate (FP/[TN + FP] ×100) of this diagnostic test. The TP rate and FP rate are plotted, and area under curve (AUC) which is used for analysis of ROC curve is calculated for all the six scoring systems [Figure 3 and Table 2] (AUC: good if AUC >0.8, moderate – 0.6≤ AUC ≤0.8, and poor if AUC <0.6). The findings of both the evaluators were assessed through the optimum scoring system, and the accuracy level of the evaluators was analyzed.
Figure 3.
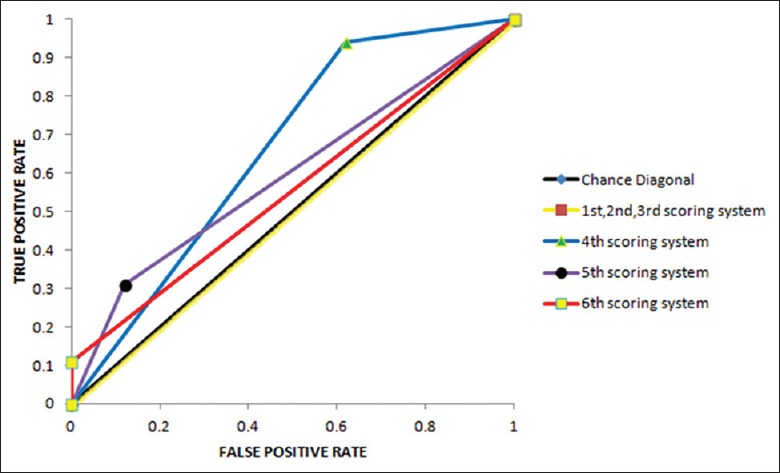
Receiver operating characteristic curves plotted for the 6 scoring systems (evaluator 1). The plotting of data for for 1st, 2nd, 3rd scoring systems reveals that the ROC curves coincides on chance diagonals and bears no significance
RESULTS
On histological examination of 45 lesions, 19 cysts and 26 granulomas were found.
Intrarater reliability for both evaluators was seen to be excellent as value of κ for evaluator 1 was 0.75 and evaluator 2 was 0.77.
Interrater reliability was also excellent as the value of α was 0.94.
A minimum number of three criteria (i.e., CBCT score of 3) was common in every lesion under study. Therefore, ROC curve analyses for the 4th (≥4 criteria), 5th (≥5 criteria), 6th (=6 criteria) scoring systems were important to ascertain the best scoring system among these three which is most suitable for diagnosis. It was found that AUC for the 4th scoring system had the highest value [Table 2].
Both the evaluators in this study showed moderate accuracy (AUC = 0.66 and 0.62, respectively) which showed that CBCT diagnosis is moderately accurate for differential diagnosis of periapical cysts and granulomas.
DISCUSSION
Though the incidence of true cysts is low compared to other periapical lesions, it needs to be diagnosed accurately because its treatment modality is surgery only and not conventional endodontic treatment.
In the present study, periapical pathology of 5 mm or more in diameter was included with the established conception of higher incidence of cysts as the size increases to 5 mm or more.[7,20,21]
The CBCT images provide more accurate diagnosis than periapical radiographs. Gray values were also used to diagnose periapical lesions.[22] In CBCT, gray values shows the difference in absorption of radiation by different matter.[23] They are not utilized here because of some inherent drawbacks. Field of view, spatial resolution selection (capability of an imaging system to distinguish between fine details of the object being studied at different levels), hard beaming (due to the absorption of low energy photons by the target tissue, the beam which exits, has only high-energy photons. This adversely affects gray values as dark bands occur on the resultant image formed) and scattered rays influence gray values.[24]
For diagnosis of a cyst, six CBCT features taken in the study are already established[18] but all features may or may not be present in a cystic lesion. Therefore in the present study, an optimum number of CBCT features were assessed to accurately differentiate cysts from granulomas. The ROC curve analyses clearly indicated that four or more positive findings were the best choice for a lesion to be diagnosed as a cyst. The plotting of data for 1st, 2nd, 3rd scoring systems reveals that the ROC curves coincide with chance diagonal and bears no significance.
As the interrater reliability was excellent, the ROC and AUC of one evaluator (evaluator 1) were shown here.
A similar study was done by Guo et al.[17] and they concluded that CBCT is a moderately accurate tool for diagnosis of cysts and granulomas. The same conclusion has been drawn in the present study.
However, conclusion of study by Rosenberg et al.[15] is different where it is shown that CBCT is not a reliable diagnostic tool. Possible reasons behind this conclusion are consideration of wide range of possibilities in the diagnosis of apical pathologies such as granuloma, granuloma like, cyst, cyst like, and others. Broad histological criteria of diagnosis were taken into consideration in their study. A definite conclusion could be drawn in the present study because differential diagnosis of only two lesions (cyst or granuloma) was taken into consideration and has clinical implications also.
In the same study by Rosenberg et al.,[15] the diagnosis of each lesion based on CBCT was made without a clear scoring system. The radiological criteria for each diagnosis were extensive and ambiguous. This led to a lot of inconsistencies and uncertainties. Hence, in the present study, an attempt was made to eliminate uncertainty by reducing the number of criteria to six and using a quantitative scoring system.
Evaluators examined the lesion based on the six predefined criteria and reported a diagnosis of cyst if four or more positive findings were present. It was assumed that this quantitative scoring system reduced uncertainty and increased the intra- and interrater reliability and accuracy compared with prior studies.
One of the limitations in this study was the small sample size. Further studies on a larger number of cases will be required to confirm the findings of the present study. The fact that at least three radiologic features were true for every lesion under study also led to a high incidence of cysts as determined by examiners through CBCT imaging. During the process of enucleation of the lesion, removal of the lesion in toto, along with the resected root tip/s, could not be done in all cases and led to submission of a sample which did not reflect the true characteristics of the pathology.
CONCLUSION
It can be stated that CBCT images are moderately accurate in diagnosing cysts from granulomas. However, further research needs to be undertaken to explore the potential of this novel diagnostic aid.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20:340–9. doi: 10.1016/0030-4220(65)90166-0. [DOI] [PubMed] [Google Scholar]
- 2.Nair PN. Apical periodontitis: A dynamic encounter between root canal infection and host response. Periodontol 2000. 1997;13:121–48. doi: 10.1111/j.1600-0757.1997.tb00098.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin LM, Ricucci D, Lin J, Rosenberg PA. Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cysts. J Endod. 2009;35:607–15. doi: 10.1016/j.joen.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Simon JH, Enciso R, Malfaz JM, Roges R, Bailey-Perry M, Patel A, et al. Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod. 2006;32:833–7. doi: 10.1016/j.joen.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Trope M, Pettigrew J, Petras J, Barnett F, Tronstad L. Differentiation of radicular cyst and granulomas using computerized tomography. Endod Dent Traumatol. 1989;5:69–72. doi: 10.1111/j.1600-9657.1989.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 6.Wais FT. Significance of findings following biopsy and histologic study of 100-periapical lesions. Oral Surg Oral Med Oral Pathol. 1958;11:650–3. doi: 10.1016/0030-4220(58)90012-4. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen H, Winther JE, Birn H. Periapical granulomas and cysts. An investigation of 1,600 cases. Scand J Dent Res. 1970;78:241–50. [PubMed] [Google Scholar]
- 8.Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008;34:1325–31. doi: 10.1016/j.joen.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Tsai P, Torabinejad M, Rice D, Azevedo B. Accuracy of cone-beam computed tomography and periapical radiography in detecting small periapical lesions. J Endod. 2012;38:965–70. doi: 10.1016/j.joen.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Ozen T, Kamburoǧlu K, Cebeci AR, Yüksel SP, Paksoy CS. Interpretation of chemically created periapical lesions using 2 different dental cone-beam computerized tomography units, an intraoral digital sensor, and conventional film. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:426–32. doi: 10.1016/j.tripleo.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 11.Bornstein MM, Lauber R, Sendi P, von Arx T. Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J Endod. 2011;37:151–7. doi: 10.1016/j.joen.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Soǧur E, Gröndahl HG, Baksı BG, Mert A. Does a Combination of two radiographs increase accuracy in detecting acid-induced periapical lesions and does it approach the accuracy of cone-beam computed tomography scanning? J Endod. 2012;38:131–6. doi: 10.1016/j.joen.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Uraba S, Ebihara A, Komatsu K, Ohbayashi N, Okiji T. Ability of cone-beam computed tomography to Detect periapical lesions that were not detected by periapical radiography: A Retrospective assessment according to Tooth Group. J Endod. 2016;42:1186–90. doi: 10.1016/j.joen.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 14.Villoria EM, Francio LA, Cunha CH, Manzi FR. Identification of simulated periapical diseases using five different diagnostic imaging methods. Rev Port Estomatol Med Dent Cir Maxilofac. 2016;57:138–45. [Google Scholar]
- 15.Rosenberg PA, Frisbie J, Lee J, Lee K, Frommer H, Kottal S, et al. Evaluation of Pathologists (Histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J Endod. 2010;36:423–8. doi: 10.1016/j.joen.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Bornstein MM, Bingisser AC, Reichart PA, Sendi P, Bosshardt DD, von Arx T, et al. Comparison between Radiographic (2-dimensional and 3-dimensional) and histologic findings of periapical lesions treated with apical surgery. J Endod. 2015;41:804–11. doi: 10.1016/j.joen.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Guo J, Simon JH, Sedghizadeh P, Soliman ON, Chapman T, Enciso R, et al. Evaluation of the reliability and accuracy of using cone-beam computed tomography for diagnosing periapical cysts from granulomas. J Endod. 2013;39:1485–90. doi: 10.1016/j.joen.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 18.White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. 7th ed. St Louis: Mosby/Elsevier; 2014. p. 335. [Google Scholar]
- 19.Obuchowski NA. ROC analysis. AJR Am J Roentgenol. 2005;184:364–72. doi: 10.2214/ajr.184.2.01840364. [DOI] [PubMed] [Google Scholar]
- 20.Morse DR, Patnik JW, Schacterle GR. Electrophoretic differentiation of radicular cysts and granulomas. Oral Surg Oral Med Oral Pathol. 1973;35:249–64. doi: 10.1016/0030-4220(73)90292-2. [DOI] [PubMed] [Google Scholar]
- 21.Zain RB, Roswati N, Ismail K. Radiographic evaluation of lesion sizes of histologically diagnosed periapical cysts and granulomas. Ann Dent. 1989;48:3–5, 46. [PubMed] [Google Scholar]
- 22.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–14. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Razi T, Niknami M, Alavi Ghazani F. Relationship between Hounsfield unit in CT scan and Gray Scale in CBCT. J Dent Res Dent Clin Dent Prospects. 2014;8:107–10. doi: 10.5681/joddd.2014.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parsa A, Ibrahim N, Hassan B, Motroni A, van der Stelt P, Wismeijer D, et al. Influence of cone beam CT scanning parameters on grey value measurements at an implant site. Dentomaxillofac Radiol. 2013;42:79884780. doi: 10.1259/dmfr/79884780. [DOI] [PMC free article] [PubMed] [Google Scholar]