Abstract
Background
Infections of skin and soft tissue (SSTI) commonly cause visits to hospital emergency departments (EDs). The Infectious Diseases Society of America (IDSA) has published guidelines for the management of SSTI, but it is unclear how closely these guidelines are followed in practice.
Methods
We reviewed records of patients seen in the ED at a large tertiary care hospital to determine guidelines adherence in 4 important areas: the decision to hospitalize, choice of antibiotics, incision and drainage (I&D) of abscesses, and submission of specimens for culture.
Results
The decision to hospitalize did not comply with guidelines in 19.6% of cases. Nonrecommended antibiotics were begun in the ED in 71% of patients with nonpurulent infections and 68.4% of patients with purulent infections. Abscesses of mild severity were almost always treated with antibiotics, and I&D was often not done (both against recommendations). Blood cultures were done (against recommendations) in 29% of patients with mild-severity cellulitis. Abscess drainage was almost always sent for culture (recommendations neither favor nor oppose). Overall, treatment fully complied with guidelines in 20.1% of cases.
Conclusions
Our results show a striking lack of concordance with IDSA guidelines in the ED management of SSTI. Social factors may account for discordant decisions regarding site of care. Use of trimethoprim/sulfamethoxazole (TMP/SMX) in cellulitis was the most common source of discordance; this practice is supported by some medical literature. Excess antibiotics were often used in cellulitis and after I&D of simple abscesses, opposing antibiotic stewardship. Ongoing education of ED doctors and continued review of published guidelines are needed.
Keywords: abscess, antibiotic stewardship, cellulitis, skin and soft tissue infection
Infections of the skin and soft tissues (SSTIs) commonly cause visits to emergency departments (EDs). Between 2005 and 2010, >3 million people yearly received ED care for SSTI, a 3-fold increase from the preceding 15 years [1, 2]. Hospitalizations for SSTI have increased similarly [3]. The emergence of community-acquired methicillin-resistant Staphylococcus aureus as a prominent cause [4] has required a far more nuanced approach to antibiotic selection than in the past. The Infectious Diseases Society of America (IDSA) published guidelines in 2005 [5] with a revision in 2014 [6] in order to aid in the management of SSTI. The authors state that they developed these guidelines in the absence of prospective studies to validate them.
Up to the present time, to our knowledge, no validation studies have been reported, although several teams of investigators have separately reported criteria that predict the need for hospitalization in cases of SSTI [2, 7–9]. We have been unable to identify publications that report how completely IDSA guidelines are being followed in clinical practice. Accordingly, we chose to study the degree to which ED physicians at a large tertiary care medical center adhere to IDSA guidelines for the management of SSTI, with particular attention to the need for hospital admission, selection of antibiotics, drainage of abscesses, and submission of specimens for microbiologic testing.
METHODS
In this retrospective analysis, we reviewed the records of 240 consecutive patients who were discharged from the ED at the Michael E. DeBakey Veterans Affairs Medical Center, Houston, with a diagnosis of SSTI. In accordance with IDSA guidelines [6], we categorized infections as: (1) nonpurulent (cellulitis/erysipelas) or (2) purulent. We further stratified purulent lesions into abscesses or infected wounds, as recommended by the US Food and Drug Administration (FDA) [10].
Patients were then classified based on the severity of infection. Mild-severity nonpurulent infection was defined as cellulitis/erysipelas without a purulent focus or systemic signs of infection. Moderate-severity nonpurulent infections included cellulitis/erysipelas with systemic symptoms of infection such as subjective fever or signs that did not satisfy criteria for systemic inflammatory response syndrome (SIRS). Patients with cellulitis/erysipelas whose findings met SIRS criteria, who had failed prior treatment with oral antibiotics or who had signs of deeper infection such as bullae or necrosis of skin, were defined as having severe infection. Disease severity was defined similarly for wound infections and abscesses. Patients with cellulitis surrounding an abscess were included in the purulent infection group. In reporting antibiotic therapy for patients who were subsequently hospitalized, we confined our observations to antibiotics that were begun in the ED. For each case, we assessed 50 variables, including baseline characteristics, underlying comorbid conditions, clinical and laboratory findings, and specifics of treatment received.
Decisions regarding management were initially made by the treating ED physician. Our medical center does not have an observation unit, and, by policy, patients are either discharged to their homes or hospitalized within 24 hours of admission to the ED. The current study investigated care given in the ED. The ED is staffed during working hours by full-time physicians, and by contract physicians after hours, most of whom have recently completed their training in programs throughout the United States. There is no protocol in place regarding management of SSTI.
Relationships among categorical variables and the decision to hospitalize were assessed with χ2 tests or Fisher’s exact test. The odds ratio describing the association between the decision to hospitalize and various potential predictors, along with 95% confidence intervals, was calculated via univariate logistic regression models. A stepwise forward selection algorithm with cutoff of P < .2 was used to develop a final multivariate logistic regression model, after excluding variables due to practical concerns such as collinearity and sparse data. The Hosmer-Lemeshow test was used to assess the final model for adequacy. All analyses were performed using Stata 12 (College Station, Texas).
RESULTS
Site of Management
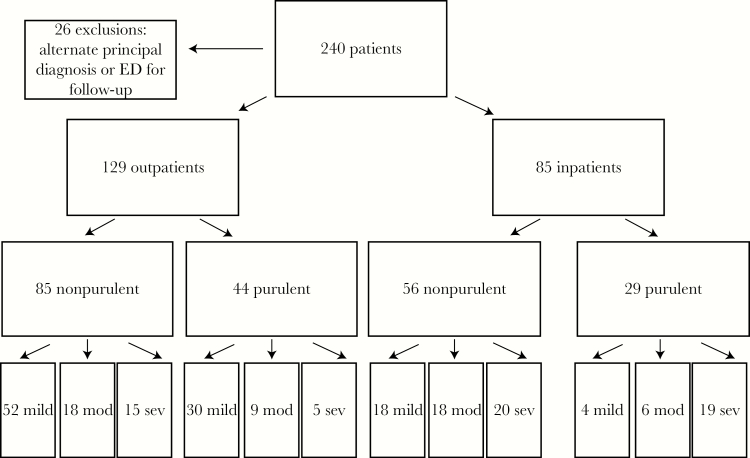
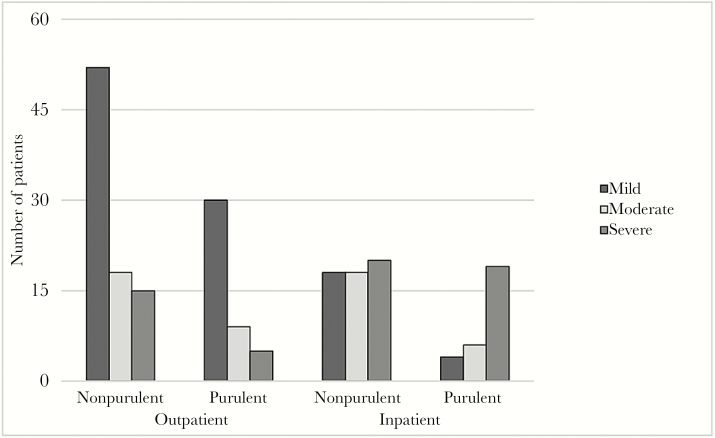
Of 240 patients, 26 were excluded because the diagnosis of SSTI was incorrect, there was an alternate principal diagnosis, or the ED visit was for follow-up of earlier treatment (Figure 1). Of 214 remaining, 85 (39.7%) were admitted to the hospital from the ED and 129 (60.3%) were discharged (Figure 2). Guidelines recommend that patients with disease of mild severity not be hospitalized and patients with severe disease be hospitalized. Of 104 patients with mild-severity disease, 22 (21.1%) were hospitalized, and 59 with severe disease 20 (33.9%) were discharged home (Figure 2). Thus, the site of management was not in accordance with guidelines in 42 (19.6%) of 214 cases.
Figure 1.
Algorithm for assessment of patients with skin and soft tissue infection.
Figure 2.
Severity of skin and soft tissue infection categorized by site of treatment.
By univariate analysis, factors predictive of hospitalization (Table 1) included moderate or severe infection, age > 50 years, alcohol abuse, fever, tachycardia (pulse > 90), criteria for SIRS, peripheral vascular disease, and diabetes mellitus. Multivariate analysis revealed that moderate-severity infections, alcohol abuse, redness, and SIRS were significantly associated with hospitalization (P < .05 for each).
Table 1.
Factors Predictive for Hospitalization
| Variable | Inpatient (n = 85) |
Outpatient (n = 129) | Univariate OR | Univariate CI |
Univariate P Value |
Multivariate OR |
Multivariate CI |
Multivariate P Value |
|---|---|---|---|---|---|---|---|---|
| Infection severity | ||||||||
| Moderate/severe | 63 | 47 | 4.99 | 2.73–9.13 | <.001 | 4.22 | 2.03–8.76 | <.001 |
| Baseline traits | ||||||||
| Age > 50 y | 72 | 84 | 2.96 | 1.48–5.93 | .02 | 1.90 | 0.85–4.28 | .119 |
| IDDM | 20 | 17 | 2.02 | 0.99–4.14 | .053 | - | - | - |
| CHF | 8 | 7 | 1.81 | 0.63–5.19 | .269 | - | - | - |
| PVD | 11 | 5 | 3.68 | 1.23–11.0 | .020 | - | - | - |
| ETOH abuse | 19 | 12 | 2.80 | 1.28–6.14 | .010 | 3.36 | 1.33–8.45 | .010 |
| Immunocompromised | 2 | 1 | 3.08 | 0.27–34.5 | .361 | - | - | - |
| Cirrhosis | 7 | 3 | 3.76 | 0.94–15.0 | .06 | - | - | - |
| CKD | 10 | 11 | 1.43 | 0.57–3.53 | .438 | - | - | - |
| BMI > 30 | 33 | 44 | 1.22 | 0.69–2.16 | .482 | - | - | - |
| Subjective fever | 21 | 7 | 5.71 | 2.30–14.1 | <.001 | - | - | - |
| Objective findings | ||||||||
| Redness | 50 | 49 | 2.33 | 1.33–4.08 | .003 | 2.11 | 1.06–4.20 | .033 |
| Warmth | 13 | 8 | 2.73 | 1.07–6.90 | .034 | 2.92 | 0.95–9.00 | .062 |
| Swelling | 49 | 77 | 0.919 | 0.52–1.60 | .766 | - | - | - |
| Tenderness | 59 | 76 | 1.58 | 0.88–2.82 | .121 | - | - | - |
| Temp > 99.4F | 13 | 3 | 7.58 | 2.09–27.5 | .002 | 3.94 | 0.84–18.4 | .081 |
| HR > 90 | 36 | 29 | 2.53 | 1.39–4.60 | .002 | - | - | - |
| SIRS | 26 | 8 | 6.66 | 2.85–15.6 | <.001 | 3.98 | 1.44–11.0 | .008 |
| Lab findings | ||||||||
| Blood cultures drawn | 72 | 22 | 26.9 | 12.75–56.9 | <.001 | |||
Abbreviations: BMI, body mass index; CHF, congestive heart failure; CI, confidence interval; CKD, chronic kidney disease; ETOH, alcohol; HR, hazard ratio; IDDM, insulin-dependent diabetes mellitus; OR, odds ratio; PVD, peripheral vascular disease; SIRS, systemic inflammatory response syndrome.
Antibiotic Selection, Nonpurulent Infection
There were 70, 36, and 35 cases, respectively, of mild, moderately severe, and severe nonpurulent SSTI. For mild cases of cellulitis/erysipelas, guidelines strongly recommend antibiotic treatment directed at groupable streptococci, including penicillins, cephalosporins, and clindamycin, but not trimethoprim/sulfamethoxazole (TMP/SMX). Only 25 of 70 (35.7%) patients received treatment in accordance with guidelines. The great majority of those who were discharged home on a nonrecommended drug were treated with TMP/SMX. Of the 18 with mild infection who were hospitalized, 16 of 18 were begun on a nonrecommended antibiotic regimen in the ED, usually vancomycin and an antipseudomonal penicillin.
Of 71 patients with moderate or severe cellulitis/erysipelas, antibiotic selection followed guidelines in 7 of 33 (21.2%) treated as outpatients and 9 of 38 (23.7%) treated as inpatients. The most common discrepancy in treating outpatients again resulted from the use of TMP/SMX. Of 18 patients with moderate or severe infections who were hospitalized, 16 received vancomycin (88.9%) and 6 received an antipseudomonal agent (33.3%), neither of which is recommended. Of 35 patients with severe infection, 9 (25.7%) received the recommended regimen of vancomycin plus piperacillin/tazobactam. Others were treated with agents such as linezolid, ciprofloxacin, and cefazolin. Thus, in total, 41 of 141 patients (29.1%) with nonpurulent SSTI received a recommended antibiotic in the ED.
Antibiotic Selection and Incision and Drainage, Purulent Infection
Of 73 patients with purulent infection, 34 were classified as mild, 15 as moderately severe, and 24 as severe. Following FDA recommendations, we stratified these 73 cases into 19 with wound infection and 54 with abscess. Of the 6 patients with mild-severity wound infections, 2 (33.3%) received recommended antibiotic therapy, and of 13 patients with moderate to severe wound infection, 4 (30.8%) received recommended antibiotic therapy.
For patients with abscesses of mild severity, guidelines recommend incision and drainage (I&D) without antibiotic therapy. Of 28 patients in this category, 25 (89.3%) were treated as outpatients. Eleven of the 25 outpatients appropriately underwent I&D for drainable abscesses, but all received an antibiotic. Of those 14 who did not undergo I&D, 11 were treated with an antibiotic. Three patients with mild-severity abscesses underwent I&D in the ED and were hospitalized after having been begun on vancomycin, piperacillin-tazobactam, or both.
For patients with moderately severe abscesses, guidelines recommend I&D and therapy with TMP/SMX or doxycycline. Six of 8 outpatients and 3 of 4 inpatients underwent I&D. Six of the 8 outpatients received recommended antibiotic therapy. None of the inpatients received appropriate antibiotics, instead receiving vancomycin and piperacillin-tazobactam or a carbapenem.
For abscesses judged to be severe, guidelines recommend I&D together with antibiotic therapy directed against methicillin-resistant Staph aureus (MRSA) (e.g., vancomycin, daptomycin, linezolid, telavancin, or ceftaroline). Four of 5 outpatients with severe infection underwent I&D, but 3 were prescribed an antibiotic that would be suboptimal for MRSA. One of 9 patients who were admitted for an abscess did not undergo I&D. For patients with moderate or severe infection who meet SIRS criteria or have impaired defenses, treatment should include an antibiotic active against MRSA; in our study, 23 of 26 patients (88.5%) who met these criteria received recommended antibiotic treatment for MRSA. Thus, in total, of 73 patients with purulent infections, 41 (43.8%) received therapy in accordance with guidelines.
Microbiological Studies
Guidelines recommend that blood cultures for patients with nonpurulent infection only be done in more severe disease. Twenty of 70 patients (28.6%) with mild cellulitis had blood cultures drawn; only 1 (5%) was positive (methicillin-sensitive Staph aureus [MSSA]). Among 71 patients with moderate to severe cellulitis, 41 (57.7%) had blood cultures obtained, of which only 1 (2.4%) was positive (Streptococcus pyogenes).
Guidelines do not specify requirements for obtaining blood cultures in patients with purulent infection. Eight of 44 (18.2%) outpatients with purulent infection had blood cultures drawn; only 1 was positive (MSSA). Twenty-four of 29 (82.8%) inpatients with purulent infection had blood cultures drawn; 2 were positive (1 for MSSA, 1 for Moraxella).
Guidelines recommend culture of pus from abscesses but state that treatment without these studies is “reasonable in typical cases.” All 36 patients who underwent I&D had fluid sent for gram stain and culture; cultures yielded a likely bacterial pathogen in 33 (92%) cases.
Follow-up
In order to assess the reliability of diagnosis and outcome of treatment, we reviewed medical records of patients who were not hospitalized for 6 weeks following ED discharge. Four patients who had been treated for cellulitis and 1 who had been treated for wound infection returned within 8 days of discharge; all were found to have an abscess at the infected site. These abscesses were debrided and cured. The opinion of the surgeon in each case was that, in retrospect, the abscess had been present at the time of the initial visit. All abscesses that were treated without I&D resolved, although resolution occurred very slowly (over 5 weeks) in 1 patient.
Summary of Results
Of 214 cases of SSTI, the total number in which management was in accordance with guidelines in all 4 categories that we examined—site of treatment, choice of antibiotic, I&D of abscess (if present), and ordering of cultures—was 43 of 214 (20.1%) (Table 2).
Table 2.
Concordance/Discordance Between Guidelines and Practice
| Category | Cellulitis (n = 141) | Abscess (n = 54) | Wound infection (n = 19) |
|---|---|---|---|
| Treated in accordance with guidelines, 4 categories | 30 | 17 | 5.2 |
| Hospitalized when not indicated | 18 | 3 | 1 |
| Discharged when hospitalization was indicated | 15 | 5 | 0 |
| Antibiotic selection inappropriate | 99 | 45 | 18 |
| Purulence not drained | N/A | 17 | 6 |
| Blood culture obtained when not indicated | 21 | 5 | 3 |
Data are presented as percentages; the denominator for each is shown in the top row.
DISCUSSION
We examined, systematically, the degree to which ED physicians in a tertiary care academic medical center adhere to IDSA guidelines for the management of SSTI. Using 4 important criteria, namely the decision to hospitalize, selection of antibiotic, use of I&D, and submission of samples for bacteriologic study, we found that management fully complied with guidelines in only 20.1% of cases. Earlier studies have examined some of these factors individually [11–13], and Marwick et al. [9] studied hospitalized patients, but none has looked at compliance with treatment guidelines in patients seen in an ED for SSTI, as we did in this study. Lack of concordance may indicate poor practice or a lack of awareness of guidelines, but it may also suggest that, at least in some regards, competent ED physicians do not agree with guidelines or find them difficult to follow, an issue that has received too little attention in the medical literature [14, 15].
IDSA guidelines suggest that patients with infection of mild severity, whether purulent or nonpurulent, be treated as outpatients and those with severe infection be hospitalized. Among patients with cellulitis, equal numbers of patients with mild, moderate, and severe infection were hospitalized. Hospital admission for patients with purulent infection more closely correlated with severity of infection. Nevertheless, overall, in 38 of 221 (18.0%) cases, the decision to hospitalize or to discharge from the ED was not in accordance with guidelines.
Previous studies have suggested specific criteria that predict the need for hospitalization to manage SSTI [2, 7, 8]. In a prospective study, Talan et al. [2] found that the perceived need for intravenous antibiotics was the principal reason for hospitalization of patients with cellulitis. Adherence to guidelines might have avoided parenteral antibiotics, thereby permitting outpatient care in a substantial proportion of our patients. In others, however, admission for mild disease may have reflected concerns about patients’ social setting or compliance, or concern for comorbid conditions, factors that are difficult to assess in a retrospective review [2].
Lack of concordance between guidelines and management was more prominent in the case of antibiotic selection than in the decision to hospitalize. For cellulitis or erysipelas, which are regarded as streptococcal, guidelines recommend therapy directed at streptococci (strong recommendation) and add that treatment for S. aureus could be considered (weak recommendation, low-quality evidence). While the recommendation to treat for streptococcal infection appears to be well supported [16–19], it is worth noting that many of the recommended antibiotics are also active against MSSA. The broad use of TMP/SMX in our study probably reflected concern for MRSA. In comparative studies of clindamycin vs TMP/SMX in uncomplicated skin infections, Hyman et al. [20] found no differences in outcomes, although Miller et al. [21] reported trends toward better responses of cellulitis to clindamycin and of abscesses to TMP/SMX.
For purulent infections, SSTI guidelines recommend that treatment be directed against S. aureus. IDSA guidelines that specifically address treatment of MRSA infections recommend TMP/SMX as appropriate for purulent infections [22]. Nearly three-quarters of the patients with purulent infections were prescribed nonrecommended antibiotics by ED physicians. This tendency was more prominent for patients who were hospitalized than for those who were discharged home, suggesting that, for patients with illness severe enough to be hospitalized, ED physicians sought to broadly “cover” gram-positive and gram-negative organisms rather than direct therapy against the most likely pathogens. This approach might have a place in treating patients with severe sepsis, but not in those with less severe infection, and it would have been appropriate for only a handful of patients in this series. Such broad-spectrum use of antibiotics is a particularly relevant concern with the current emphasis on antibiotic stewardship and rapidly evolving antibiotic resistance patterns.
According to guidelines, abscesses of mild severity should be treated by I&D without an antibiotic. The majority of patients in this category underwent I&D, but nearly all also received an antibiotic, generally TMP/SMX, a practice previously described by Pallin et al. [11]. Although against guidelines, such treatment has recently been shown to enhance cure rates [23], which supports this choice by ED physicians. Traditionally I&D has been regarded as necessary to treat abscesses. It has become increasingly clear, however, that small abscesses, for example, in the peritoneal cavity and brain [24], can be cured with antibiotic therapy alone. More severe abscesses were treated with I&D. Antibiotic treatment usually included vancomycin for MRSA (recommended by guidelines); however, piperacillin/tazobactam or another drug effective against gram-negative bacilli was often added without an apparent indication.
The proportion of patients who received recommended treatment in all 4 categories that we studied—hospitalization or discharge home, antibiotic selection, I&D if indicated, and appropriate use of microbiology—was only 20.1%, a very low figure, but similar to that found by Marwick et al. [9]. With this low rate of compliance, one conclusion might be that the standard of care is very poor. Alternative conclusions, however, are that the guidelines are difficult to interpret, do not fit individual circumstances, or do not include other approaches that are based on evidence or good clinical judgment. For example, IDSA guidelines include abscesses and wound infections under the single heading of purulent infections. The FDA [10] made these recommendations more readily interpretable by separating purulent infections into wound infection and abscesses, and this modification has been followed in subsequent studies, including a recent one by Talan et al. [25]. In addition, social factors or concern by the ED physician that a patient will not comply with oral antibiotics may lead to hospitalization when there is no specific medical indication. Finally, an antibiotic such as TMP/SMX that is not recommended may still be regarded as appropriate therapy based on published reports in the medical literature.
Strengths of the present study include the completeness of electronic medical records, particularly regarding comorbid conditions, and follow-up data, since our patients receive nearly all their care within the VA medical system. The availability of medical records also allows for more accurate determination of diagnosis than does review of ICD codes [11]. Our study focused on concordance with guidelines in the ED, not on outcomes. Nonetheless, numerous studies have shown in hospitalized patients that the systematic application of an evidence-based care pathway [26] reduces antibiotic use, costs, and length of hospital stay, and that treatment of SSTI in the hospital setting provides important opportunities for antibiotic stewardship [2, 9, 26, 27]. IDSA guidelines suggest that these same principles should also apply to practice in the ED. Once ED physicians began patients on an antibiotic, there appeared to be a definite reluctance to narrow that treatment during the hospital course, at least in the first 48–72 hours.
Several limitations are also apparent. Our study was relatively small-scaled and was based on predominantly male patients seen at a single institution within a single year-long period. However, our ED does not have an SSTI protocol in place, and ED physicians at our medical center have trained in geographically varied programs; therefore, our results may reflect general, rather than institution-specific, behavior. Finally, even though medical records were all available, the reasoning that went into certain decisions, especially the one to hospitalize, was often unstated in the patient record. The ED physician may consider patient unreliability and other social factors; since this was not a prospective study, we have no further information in many cases.
In conclusion, the results of the present study show a striking lack of adherence to published guidelines. Patients who had mild-severity cellulitis were often hospitalized, and some with severe disease were sent home on antibiotic therapy. The choice of antibiotics was often not in accordance with guidelines, largely because of the use of TMP/SMX, although some recent literature supports this practice. Abscesses were often not drained, but those of mild severity responded to antibiotic therapy. Antibiotics were regularly prescribed after I&D of abscesses of mild severity, which goes against recommendations. Stratification of cases into purulent and nonpurulent infections may have created confusion. These results suggest that a nuanced approach toward the revision and updating of guidelines, one that includes definitions of infection severity, may bridge the disconnect between guidelines and clinical practice.
Acknowledgements
Author contributions. R. S. Kamath and D. Sudhakar contributed equally to this project.
Potential conflicts of interest. All authors: no reported conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Pallin DJ, Egan DJ, Pelletier AJ et al. . Increased US emergency department visits for skin and soft tissue infections, and changes in antibiotic choices, during the emergence of community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med 2008; 51:291–8. [DOI] [PubMed] [Google Scholar]
- 2. Talan DA, Salhi BA, Moran GJ et al. . Factors associated with decision to hospitalize emergency department patients with skin and soft tissue infection. West J Emerg Med 2015; 16:89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Edelsberg J, Taneja C, Zervos M et al. . Trends in US hospital admissions for skin and soft tissue infections. Emerg Infect Dis 2009; 15:1516–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moran GJ, Krishnadasan A, Gorwitz RJ et al. ; EMERGEncy ID Net Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–74. [DOI] [PubMed] [Google Scholar]
- 5. Stevens DL, Bisno AL, Chambers HF et al. ; Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis 2005; 41:1373–406. [DOI] [PubMed] [Google Scholar]
- 6. Stevens DL, Bisno AL, Chambers HF et al. ; Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 2014; 59:e10–52. [DOI] [PubMed] [Google Scholar]
- 7. Sabbaj A, Jensen B, Browning MA, John Ma O, Newgard CD. Soft tissue infections and emergency department disposition: predicting the need for inpatient admission. Acad Emerg Med 2009; 16:1290–7. [DOI] [PubMed] [Google Scholar]
- 8. Figtree M, Konecny P, Jennings Z et al. . Risk stratification and outcome of cellulitis admitted to hospital. J Infect 2010; 60:431–9. [DOI] [PubMed] [Google Scholar]
- 9. Marwick C, Rae N, Irvine N, Davey P. Prospective study of severity assessment and management of acute medical admissions with skin and soft tissue infection. J Antimicrob Chemother 2012; 67:1016–9. [DOI] [PubMed] [Google Scholar]
- 10. US Food and Drug Administration. Guidance for industry. Acute bacterial skin and skin structure infections: developing drugs for treatment. US Food and Drug Administration; 2010. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071185.pdf. Accessed 10 January 2016. [Google Scholar]
- 11. Pallin DJ, Camargo CA Jr, Schuur JD. Skin infections and antibiotic stewardship: analysis of emergency department prescribing practices, 2007–2010. West J Emerg Med 2014; 15:282–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hurley HJ, Knepper BC, Price CS et al. . Avoidable antibiotic exposure for uncomplicated skin and soft tissue infections in the ambulatory care setting. Am J Med 2013; 126:1099–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Daly JM, Levy BT, Ely JW et al. . Management of skin and soft tissue infections in community practice before and after implementing a “best practice” approach: an Iowa Research Network (IRENE) intervention study. J Am Board Fam Med 2011; 24:524–33. [DOI] [PubMed] [Google Scholar]
- 14. Amaro R, Liapikou A, Cilloniz C et al. . Predictive and prognostic factors in patients with blood-culture-positive community-acquired pneumococcal pneumonia. Eur Respir J 2016; 48:797–807. [DOI] [PubMed] [Google Scholar]
- 15. Montravers P, Snauwaert A, Welsch C. Current guidelines and recommendations for the management of skin and soft tissue infections. Curr Opin Infect Dis 2016; 29:131–8. [DOI] [PubMed] [Google Scholar]
- 16. Jeng A, Beheshti M, Li J, Nathan R. The role of beta-hemolytic streptococci in causing diffuse, nonculturable cellulitis: a prospective investigation. Medicine (Baltimore) 2010; 89:217–26. [DOI] [PubMed] [Google Scholar]
- 17. Pallin DJ, Binder WD, Allen MB et al. . Clinical trial: comparative effectiveness of cephalexin plus trimethoprim-sulfamethoxazole versus cephalexin alone for treatment of uncomplicated cellulitis: a randomized controlled trial. Clin Infect Dis 2013; 56:1754–62. [DOI] [PubMed] [Google Scholar]
- 18. Obaitan I, Dwyer R, Lipworth AD et al. . Failure of antibiotics in cellulitis trials: a systematic review and meta-analysis. Am J Emerg Med 2016; 34:1645–52. [DOI] [PubMed] [Google Scholar]
- 19. Bruun T, Oppegaard O, Kittang BR et al. . Etiology of cellulitis and clinical prediction of streptococcal disease: a prospective study. Open Forum Infect Dis. doi: 10.1093/ofid/ofv181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hyun DY, Mason EO, Forbes A, Kaplan SL. Trimethoprim-sulfamethoxazole or clindamycin for treatment of community-acquired methicillin-resistant Staphylococcus aureus skin and soft tissue infections. Pediatr Infect Dis J 2009; 28:57–9. [DOI] [PubMed] [Google Scholar]
- 21. Miller LG, Daum RS, Creech CB et al. ; DMID 07-0051 Team. Clindamycin versus trimethoprim-sulfamethoxazole for uncomplicated skin infections. N Engl J Med 2015; 372:1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu C, Bayer A, Cosgrove SE et al. ; Infectious Diseases Society of America. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011; 52:e18–55. [DOI] [PubMed] [Google Scholar]
- 23. Talan DA, Mower WR, Krishnadasan A et al. . Trimethoprim-Sulfamethoxazole versus placebo for uncomplicated skin abscess. N Engl J Med 2016; 374:823–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brouwer MC, van de Beek D. Epidemiology, diagnosis, and treatment of brain abscesses. Curr Opin Infect Dis 2017; 30:129–34. [DOI] [PubMed] [Google Scholar]
- 25. Talan DA, Lovecchio F, Abrahamian FM et al. . A randomized trial of Clindamycin versus Trimethoprim-sulfamethoxazole for uncomplicated wound infection. Clin Infect Dis 2016; 62:1505–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yarbrough PM, Kukhareva PV, Spivak ES et al. . Evidence-based care pathway for cellulitis improves process, clinical, and cost outcomes. J Hosp Med 2015; 10:780–6. [DOI] [PubMed] [Google Scholar]
- 27. Jenkins TC, Sabel AL, Sarcone EE et al. . Skin and soft-tissue infections requiring hospitalization at an academic medical center: opportunities for antimicrobial stewardship. Clin Infect Dis 2010; 51:895–903. [DOI] [PubMed] [Google Scholar]