Abstracts
Background
Even though, the disclosure of HIV sero- status to sexual partners, friends or relatives is the main tool for prevention and care strategies, most of the HIV/AIDS patients do not inform their close friends. The most common reasons for not disclosure of their status to the community were majorly fear of social rejection and discriminations. Therefore, this study assessed the HIV positive sero-status disclosure and its determinants among People Living with HIV /AIDS (PLWH/A) followed by the Antiretroviral therapy (ART) Clinic in Jimma University Specialized Hospital, Southwest Ethiopia.
Methods
A facility based cross-sectional study design was used among 351 ART patients that selected by systematic random sampling from ART clinic of Jimma University Specialized Hospital in March-2014. Data were collected through interviewer-administered questionnaires and analyzed using SPSS version 20.0 software. In a descriptive analysis frequency, mean and percentage were calculated. Bivariate and multivariate analyses were used to identify associated factors and the association between the explanatory and dependent variables was estimated.
Results
Only 37.6% (n = 132) were revealed their HIV positive status to anyone. Disclosure was done towards the sexual partners (88.6%), close family (72.7%) and a larger population (18.2%). Age ≤ 39 years (AOR = 0.014 [95%, CI = 0.005, 0.037]),Male sex (AOR = 3.039, [95% CI = 1.164, 7.935]), WHO stage III – IV at ART start(AOR = 2.766, [95%, CI = 1.321, 5.791]), presence of comorbidity (AOR = 2.500, [95%, CI = 1.483, 4.214]), having any clinical symptoms for HIV(AOR = 2.98, [95%, CI = 1.724, 5.152]),Low physical domain related quality of life (AOR = 3.83, [95%, CI = 2.008, 7.315]) and high social domain related quality of life (AOR = 0.053, [95%, CI = 0.022, 0.125]) were statistically significant association with their HIV sero-status disclosure.
Conclusions
Findings of this study indicated, the disclosure of HIV status is very low. Discloser is more likely when the patient is older, male, and has a higher level of education. Clinical determinants for disclosure was the WHO stage III-IV, treatment duration of ≥2 years, comorbidity, presence of clinical symptoms for HIV, low physical domain related quality of life, low social domain related quality of life and low overall quality of life.
Keywords: ART patients, associated factors, Disclosure, Jimma University Specialized Hospital, and People living with HIV/AIDS
Background
HIV is referred to (Human Immunodeficiency Infection) which is the most dangerous virus which is the major cause of AIDS in human life. It continued to spread worldwide and one of serious health challenges. Although much of the news on AIDS is encouraging, the challenges become continued [1].
Globally, there were 36.7 million people living with HIV in 2015. This was high of 33.3 million in 2010. These increments in a number of patients were resulted because of continuing new infections, people living longer with HIV, and general population growth. 1.1 million People died of AIDS in 2015. There were about 2.1 million new infections in 2015 or about 5700 new infections per day. An estimated 32.1 million of adults aged 15–49 years worldwide are living with HIV [2]. 1.8 million Children living with HIV, 110,000 AIDS-related deaths, and 150,000 new infections among children in 2015 [3].
Sub-Saharan Africa, the hardest hit region, is home to nearly 70% of people living with HIV but only about 13% of the world’s population [4]. The sub-region of Eastern and Southern Africa were home to more than half (52%) of all people living with HIV, as well as more than half of the children living with HIV (56%) [5].
Ethiopia has a large and very vulnerable populations that there were more than half million (671,941) HIV positive population, 14,405 new HIV infections and 24,813 deaths in 2016 [6].
Disclosure of human immune deficiency virus (HIV) positive status has a key role in the prevention and control of HIV/AIDS. The failure of people infected with HIV to disclose their positive status can expose their sexual partners and other relatives that have close contact with them to the virus [7]. In developing countries, the rates of disclosure of HIV sero- status was very low compared to developed countries. The study showed that the rates ranged from 16.7% to 86% with the average of 49% that was almost half of the HIV positive patients not exposed their sero-status to other people including their sexual partners. Whereas, in average 79% of HIV positive patients were disclosed their HIV sero-status to other peoples’ in study done in developed countries [8]. Likewise, in Ethiopia, very low percentage of HIV positive patients disclosed their sero- status to other people including their sexual partners.
There are different factors that affect the disclosure of their HIV status; such as Marital status, knowledge of partner HIV status, fearing negative outcomes of disclosure, their communication skills, initiation of anti-retroviral, receiving ongoing counseling and duration of HIV related care follow up are some of the identified reasons [9, 10]. The knowledge of those factors is cored for prevention and control of HIV/AIDS strategies. Therefore, this study assessed the prevalence of HIV positive sero - status disclosure and its determinants among People Living with HIV /AIDS following ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia.
Methods
Study setting and participants
Facility (Hospital) based cross- sectional study design was conducted in Jimma University Specialized Hospital ART clinic from March 1 to 30, 2014. Jimma University Specialized Hospital (JUSH) is one the oldest public hospital in the country. It was established in 1937 by Italian invaders for the service of their soldiers. Geographically, it is located in Jimma city that is located at 357 km from Addis Ababa [11]. JUSH is the teaching and referral hospital that have around 450 beds and more than 750 staffs of both supportive and professionals. It provides services approximately for 9000 inpatients and 80,000 outpatients’ attendants in a year. JUSH ART clinic pioneered the use of antiretroviral drugs in Ethiopia in 2002. The clinic currently gives follow up service for about 6260 HIV/AIDS patients. On average, about130 patients were visiting the clinic on a day. The appointments follow up given to patients in every one to two months. The clinic staffed with internist, the senior health officer and nurses who were trained in specific HIV/AIDS disease patient cares [12].
Sample size determinations and Sampling techniques
The sample was determined using single population proportion formula using EPI Info 7.1.0.6 version was applied with an assumption of a level of confidence of the study 95%, sampling error tolerated 5%, Proportion of disclosure to relatives 33.2% in the same institution (Jimma University Specialized Hospital) at 2007 [13]. Finally, 358 sample sizes were obtained.
Study participants were selected by using systematic random sampling technique. There were a total of 6260 patients registered for ART care in the hospital. Per day, there was a high patient flow; approximately 130 patients attend the PLWHA clinic each day. To finish data collection within one month, every day around 18 study participants were recruited. Therefore, within the interval of the 7th or every 7th patient attending the clinic were involved in an interview until the required sample of 358 was recruited. As patients attended the clinic on a monthly basis and above, no patients included twice during the recruitment period. The study includes adult patients above the age of eighteen years old due to ethical issues.
Data collection Instruments and methods
The questioners were adapted from related kinds of literature [13–18]. The questioners assessed mainly socio - demographic factors like age, educational status, occupation, marital status, etc.; disease related care factors like CD4 count, WHO stage, the length of treatment, general health conditions, etc. and social relationship related factors such as reminder of drugs, with whom they live, self-care status, Data were collected both by Afan Oromo and Amharic questionnaires. Five BSc nurses working in JUSH ART clinic who could speak both Amharic and Afan Oromo were collected the data by face-to-face interview. One BSc Nurse who works in JUSH ART clinic was assigned as the supervisor at the time of data collections to supervise the overall data collection conditions including technical activities. The patients were interviewed after they got the service they required from the ART clinic.
Data quality assurance
The questionnaires were pre-tested on 5% of the sample in Jimma town, Shanan Gibe Hospital on HIV positive patients that started HAART drug treatment at the ART clinic before the actual data collections and amendments were made accordingly. Language experts translated the questioners into two local languages (Amharic and Afan Oromo) and then back to English to make sure the consistency of the questionnaires, then correction was done accordingly. The data collectors and supervisors were trained on data collection tools and procedures for one day. On top of this, supervisors were followed data collectors. Both supervisors and investigators were also checked for the collected data clear and completeness in every day of a period of data collections.
Data Processing and analysis
Before data entry, questionnaires were checked for its completeness. Data was entered into Epidata version 3.0 and then exported to SPSS version 20.0 for further analysis. The descriptive analysis like percentage, frequency and mean were calculated. The bivariate logistic regression analysis was used to identify associations between variables. The variables that had p – value ≤0.3, have association in other similar research and variables that suspected to have association study variables were transferred to multiple logistic regression models. The possible effects of confounders were controlled through multivariate logistic regression analysis. The association between the explanatory and dependent variables were assessed at the p-value of 0.05. The variables that shown p - value <0.05 were considered as statistically significant variables in multiple logistic regression model. The degree of association between independent and dependent variables were assessed using adjusted odds ratio with 95% confidence interval. The findings were presented in the form of narratives, tables, pie charts, and graphs.
Results
Socio-demographic Characteristics
From the total 358 sampled and 351 of the study participants participated in the study that result in 98.1% of response rate. From total of study participants, 228 (65%) of them were females. Most of the participants, 237 (67.5%) aged less than 40 years with the mean age of 34.9 (SD ± 8.68) (min 20 years and max 67 years old). Never married were dominant that accounts 152 (43.3%), then followed by married 99 (28.2%) and divorced 69 (19.7%). The majority, 143 (40.7%) were attended primary school educations and followed by secondary school 104 (30.5%). Oromo accounts 153 (42.7%) by ethnicity and Muslims 102 (29%) by religion. Whereas, 247 (70.4%) of them were currently employed [Table 1].
Table 1.
Socio demographic characteristics of PLWHA on follow up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014 (N = 351)
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age of the respondent | ||
| 1. ≤ 39 years | 237 | 67.5 |
| 2. ≥ 40 years | 114 | 32.5 |
| Sex of Sex of respondents respondents | ||
| 1. Male | 123 | 35 |
| 2. Female | 228 | 65 |
| Marital status | ||
| 1. Single | 152 | 43.3 |
| 2. Married | 99 | 28.2 |
| 3. Widowed | 31 | 8.8 |
| 4. Divorce | 69 | 19.7 |
| Educational level | ||
| 1. No formal education | 72 | 20.5 |
| 2. Grade: 1–8 | 141 | 40.2 |
| 3. Grade: 9–10 | 107 | 30.5 |
| 4. 10+, certificate and above | 31 | 8.8 |
| Ethnicity | ||
| 1. Oromo | 153 | 43.6 |
| 2. Amhara | 96 | 27.4 |
| 3. Tigre | 18 | 5.1 |
| 4. Dawuro | 34 | 9.7 |
| 5. Yem | 36 | 10.3 |
| 6. Other* | 14 | 4 |
| Religion | ||
| 1. Muslim | 102 | 29.1 |
| 2. Orthodox | 181 | 51.6 |
| 3. Protestant | 68 | 19.3 |
| Occupation | ||
| 1. Currently Employed | 239 | 68.1 |
| 2. Currently not employed | 112 | 31.9 |
| Income of respondents | ||
| 1. ≤ 500 ETB | 253 | 72.1 |
| 2. 501–1000 ETB | 48 | 13.7 |
| 3. ≥ 1001 ETB | 50 | 14.2 |
Clinical conditions of Participants
The majority, 248 (70.7%) had CD4 count less than <250 cell/ml when they started ART follow up services. About, 278 (79.2%) of the respondents had ≥250 cells/ml CD4 count level. Three- forth, 283 (80.6%) of the them were on stage I - II of WHO classifications. Large number, 233 (66.4%) of them was taking prophylaxes. Moreover, 247 (70.4%) of respondents were found in good general health conditions currently. Around, 273 (77.8%) of them were present on better life currently than last year [Table 2].
Table 2.
Clinical conditions of PLWHA on follow up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014(N = 351)
| Variables | Alternatives | Frequency | Percentage |
|---|---|---|---|
| CD4 count when ART started | 1. < 250 cell/ml | 248 | 70.7 |
| 2. ≥ 250 cell/ml | 103 | 29.3 | |
| CD4 count currently | 1. < 250 cell/ml | 73 | 20.8 |
| 2. ≥ 250 cell/ml | 278 | 79.2 | |
| WHO stage at start | 1. Stage I - II | 286 | 81.5 |
| 2. Stage III - V | 65 | 18.5 | |
| Current WHO stage of HIV | 1. Stage I - II | 283 | 80.6 |
| 2. Stage III- V | 68 | 19.4 | |
| Vests clinic for health seeking | 1. Yes | 285 | 81.2 |
| 2. No | 66 | 18.8 | |
| Discontinuation of OI prophylaxes | 1. Yes | 233 | 66.4 |
| 2. No | 118 | 33.6 | |
| How long they stayed on treatment | 1. < 2 years | 143 | 40.7 |
| 2. ≥ 2 years | 208 | 59.3 | |
| General health condition | 1. Good | 247 | 70.4 |
| 2. Poor | 104 | 29.6 | |
| 1.1.Faced body pain in last 4 weeks | 1. Not faced | 217 | 61.8 |
| 2. mild pain | 103 | 29.3 | |
| 3. severe pain | 31 | 8.8 | |
| Healthy as any body | 1. Yes | 223 | 63.5 |
| 2. No | 128 | 36.5 | |
| Compared to last year how they rate their health status | 1. better now than a year | 273 | 77.8 |
| 2. worse now than a year | 78 | 22.2 | |
| Can perform any physical exercise | 1. yes | 215 | 61.3 |
| 2. No | 136 | 38.7 | |
| Have attended health education | 1. Yes | 287 | 81.8 |
| 2. No | 64 | 18.2 |
HIV-positive status disclosure
Of the respondents, only 132 (37.6%) were disclosed as they were HIV sero -status positive patients [Fig. 1). Out of these disclosed patients, almost all of them 117 (88.6%) exposed to their sexual partner followed by their close families 96 (72.7%). But, only 24 (18.2%) of them disclosed to any people. [Fig. 2].
Fig. 1.
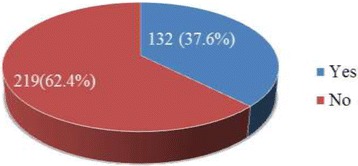
The HIV Disclosure status of PLWHA on follow up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014
Fig. 2.
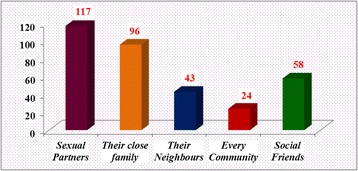
The HIV Disclosure status to others peoples among PLWHA on follow up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014
Socio demographic, social and behavioral factors that associated with HIV positive status disclosure among participants
In bivariate analysis; age, sex, educational status, marital status, relationship with other people, drinking alcohol, perceived HIV related stigma, a social domain of quality of life and Substance abusing behaviors of participants had significant association with HIV sero-status disclosure.. But in multivariate analysis; age, sex, educational status and the social domain of quality of life were significantly associated with HIV sero-status disclosure.
Elaborately, participants those aged ≤39 years were less likely to disclose (AOR = 0.014 [95%, CI = 0.005, 0.037]) than those aged ≥40 years. Similarly, males were three times more likely to disclose their HIV sero - status than females (AOR = 3.039, [95% CI = 1.164, 7.935]). Again, secondary school (AOR = 4.368, [95%, CI = 1.450, 13.153]) and ≥10+ and above attendants (AOR = 26.291, [95%, CI = 3.886, 7.876]) were more likely to disclose their HIV sero -status to other persons than the rest. Moreover, those had high level of social domain of quality of life were less likely to disclose than those had low level of social domain of quality of life (AOR = 0.053, [95%, CI = 0.022, 0.125]) [Table 3].
Table 3.
Associations of Socio demographic, social and behavioral factors with HIV positive status disclosure of PLWHA on follow up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014
| Independent Variables | Alternatives | HIV status disclosure | COR [95% C.I] | P- Value | AOR [95% C.I] | ||
|---|---|---|---|---|---|---|---|
| Yes | No | COR | AOR | ||||
| Age of respondents | ≤ 39 years | 31 | 206 | 0.019 (0.010–0.039) | .000 | .000 | 0.014(0.005–0.037) |
| ≥ 40 years | 101 | 13 | 1.00 | 1.00 | |||
| Sex of respondents | Male | 71 | 52 | 3.536 (2.230–5.607) | .001 | .023 | 3.039(1.164–7.935) |
| Female | 61 | 167 | 1.00 | 1.00 | |||
| Marital Status | Single | 39 | 113 | 1.00 | 1.00 | ||
| Married | 29 | 70 | 8.330 (3.445–20.144) | .000 | .554 | 1.338(.510–3.509) | |
| Divorce | 41 | 28 | 6.940 (2.78–17.301) | .000 | .097 | .407(.141–1.175) | |
| Widowed | 23 | 8 | 1.963 (0.769–5.012) | .158 | .316 | .441(.089–2.186) | |
| Educational level of respondents | No formal education | 29 | 41 | 1.00 | 1.00 | ||
| Grade 1–8 | 76 | 68 | 0.745 (.421–1.318) | .312 | .899 | 1.066(.396–2.872) | |
| Grade 9–10 | 21 | 86 | 3.276 (1.683–6.377) | .000 | .009 | 4.368(1.450–13.153) | |
| 10+ and above | 6 | 24 | 3.333 (1.220–9.106) | .019 | .001 | 26.291(3.886–7.876) | |
| Occupation of respondents | Currently employed | 83 | 156 | .684 (.432–1.082) | .105 | .889 | 1.064(.442–2.563) |
| Currently not employed | 49 | 63 | 1.00 | 1.00 | |||
| Average monthly income | ≤ 500ETB | 103 | 150 | 1.00 | 1.00 | ||
| 501- 1000ETB | 16 | 32 | 1.373 (.717–2.632) | .339 | .320 | 1.974(.517–7.532) | |
| ≥ 1001ETB | 13 | 37 | 1.954 (.990–3.857) | .053 | .476 | 1.531(.474–4.944) | |
| Discontinuation of OI prophylaxes | No | 84 | 149 | 0 .822(.522–1.295) | .398 | ||
| Yes | 48 | 70 | 1.00 | 1.00 | |||
| Reminder while they took drugs | Self | 106 | 169 | 1.206(.708–2.054) | .490 | ||
| Other person | 26 | 50 | 1.00 | ||||
| Currently with whom they live | With another person | 112 | 190 | 1.170(.632–2.165) | .617 | ||
| Alone | 20 | 29 | 1.00 | ||||
| Relationship with other people | Friendly | 104 | 132 | 2.297(1.402–3.761) | .001 | .979 | 1.013(0.385–2.667) |
| Discrimination | 29 | 86 | 1.00 | ||||
| Drinks alcohol | Yes | 49 | 64 | 5.408 (2.219–13.178) | .000 | .270 | 1.647(.679–3.994) |
| No | 83 | 155 | 1.00 | ||||
| Do you smoke cigarette | yes | 38 | 59 | 1.096 (.678–1.773) | .708 | ||
| No | 94 | 160 | 1.00 | ||||
| Vests clinic for health seeking | Yes | 107 | 178 | 0.986(.568–1.712) | .960 | ||
| No | 25 | 41 | 1.00 | ||||
| Perceived HIV related stigma | High | 65 | 164 | 1.00 | 1.00 | ||
| Low | 64 | 52 | 3.105(1.950–4.945) | .000 | .561 | 1.323(.515–3.396) | |
| Social domain of quality of life | Low | 40 | 183 | 1.00 | 1.00 | ||
| High | 92 | 36 | 11.692(6.984–19.573) | .000 | .000 | 0.053(0.022–0.125) | |
| Substance abusing | Yes | 94 | 113 | 2.320(1.464–3.678) | .000 | .487 | 1.342(.586–3.073) |
| No | 38 | 106 | 1.00 | 1.00 | |||
| Self-care status | Low | 96 | 139 | 1.535(.958–2.459) | .075 | .795 | .883(0.348–2.246) |
| High | 36 | 80 | 1.00 | 1.00 | |||
Clinical factors that associated with HIV positive status disclosure among participants
Those variables such as; performing of any physical exercise, CD4 count level when ART started, WHO stage at start of ART, general health conditions of the patients, how long they stayed on treatment, whether they perceive themselves as healthy as anybody or not, having comorbidity conditions of other diseases, having any clinical symptoms for HIV/AIDS, Feeling they had about their health conditions, how they rate their health status by comparing to last year, their status of physical domains of quality of life and their status of quality of life showed significant association with disclosure of HIV sero – status during bivariate analysis.
Then those variables that had p – values ≤0.3 were transferred to multiple logistic regression models. Accordingly, ability to perform of any physical exercise, WHO stage at start of ART, general health conditions, length of time they stayed on HAART treatment, having comorbidity conditions with other diseases, having any clinical symptoms of HIV/AIDS, status of physical domains of quality of life and overall quality of life had statistically significant association with disclosure of HIV positive sero – status.
For further explanation, participants those couldn’t perform any physical exercise were two times more likely to disclose their HIV sero – status (AOR =1.922, [95% CI = 1.142, 3.235]). In addition, those at stage III – IV were around triply more to disclose their HIV sero – status when compared to those at stage I- II (AOR = 2.766, [95%, CI = 1.321, 5.791]). Moreover, participants those had comorbidity with other diseases were 2.5 times more likely to disclose than those had no comorbidities (AOR = 2.500, [95%, CI = 1.483, 4.214]). Similarly, those had any clinical symptoms of HIV/AIDS were three times more to disclose than those hadn’t clinical symptoms (AOR = 2.98, [95%, CI = 1.724, 5.152]). Likewise, participants that present on low status of the physical domain of quality of life were four times higher to disclose than their opponents(AOR = 3.83, [95%, CI = 2.008, 7.315]). Finally, clients those present on the low general quality of life were twofold more likely to disclose than their counterparts[Table 4].
Table 4.
Association of Clinical factors with HIV positive status disclosure of PLWHA on follows up in Jimma University Specialized hospital in ART clinic, southwest Ethiopia, 2014
| Independent Variables | Alternatives | HIV status disclosure | COR [95% C.I] | P- Value | AOR [95% C.I] | ||
|---|---|---|---|---|---|---|---|
| Yes | No | COR | AOR | ||||
| Perform any physical exercise | Yes | 67 | 148 | 1.00 | 1.00 | ||
| No | 65 | 71 | 2.022(1.298–3.150) | .002 | .014 | 1.922(1.142–3.235) | |
| CD4 count when ART started | < 250 cell/ml | 82 | 91 | 2.192(1.410–3.409) | .000 | .138 | 1.509(0.876–2.600) |
| ≥ 250 cell/ml | 51 | 127 | 1.00 | 1.00 | |||
| CD4 count currently | < 250 cell/ml | 12 | 61 | 1.060(.657–1.711) | .811 | ||
| ≥ 250 cell/ml | 82 | 196 | 1.00 | ||||
| WHO stage at start | Stage I-II | 119 | 167 | 2.850(1.486–5.469) | .002 | .007 | 2.766(1.321–5.791) |
| Stage III-IV | 13 | 52 | 1.00 | 1.00 | |||
| Current WHO stage of HIV | Stage I-II | 107 | 178 | 0.986(.568–1.712) | .960 | ||
| Stage III-IV | 25 | 41 | 1.00 | ||||
| General health condition | Good | 82 | 165 | 1.00 | 1.00 | ||
| Poor | 50 | 54 | 1.863 (1.168–2.972) | .009 | .048 | 1.741(1.005–3.017) | |
| How long they stayed on treatment | < 2 years | 39 | 104 | 1.00 | 1.00 | ||
| ≥ 2 years | 93 | 115 | 2.157(1.364–3.411) | .001 | .015 | 1.941(1.136–3.316) | |
| They healthy as any body | Yes | 99 | 158 | 1.00 | 1.00 | ||
| No | 33 | 61 | 1.601(1.166–2.198) | .004 | .600 | 1.185(0.628–2.237) | |
| Have comorbidity conditions | Yes | 75 | 62 | 3.332(2.119–5.240) | .000 | .001 | 2.500(1.483–4.214) |
| No | 57 | 157 | 1.00 | 1.00 | |||
| Have any Clinical symptoms for HIV | Yes | 103 | 104 | 3.927(2.406–6.411) | .000 | .000 | 2.980(1.724–5.152) |
| No | 29 | 115 | 1.00 | 1.00 | |||
| Felt their health is excellent | Yes | 86 | 166 | 1.00 | 1.00 | ||
| No | 46 | 53 | 1.675(1.044–2.689) | .033 | .853 | 0.945(0.520–1.717) | |
| Felt sick earlier than other people | Yes | 89 | 156 | 0.836(.524–1.333) | .452 | ||
| No | 43 | 63 | 1.00 | ||||
| Compared to last year how they rate your health | Better now than a year | 89 | 184 | 1.00 | 1.00 | ||
| Worse now than a year | 43 | 35 | 2.540(1.521–4.242) | .000 | .087 | 1.698(0.926–3.113) | |
| Bathing and dressing | Not limited | 82 | 155 | 1.00 | |||
| Limited | 50 | 64 | 1.477(.935–2.331) | .094 | .313 | 1.537(0.666–3.546) | |
| Physical domain of quality of life | Low | 59 | 77 | 1.490(.959–2.317) | .076 | .000 | 3.833(2.008–7.315) |
| High | 73 | 142 | 1.00 | 1.00 | |||
| Psychological domain | Low | 91 | 147 | 0.920(.578–1.46) | .724 | ||
| High | 41 | 72 | 1.00 | ||||
| Quality of life of HIV/AIDS patients | Low | 70 | 67 | 2.634(1.687–4.111) | .000 | .000 | 4.349(2.301–8.219) |
| High | 62 | 152 | 1.00 | 1.00 | |||
Discussions
This study had assessed the HIV positive sero-status disclosure and its determinants among People Living with HIV /AIDS following ART Clinic in Jimma University Specialized Hospital, Southwest Ethiopia. Accordingly, from the total respondents, only 132 (37.6%) were disclosed their HIV sero –status positivity in general. Out of these disclosed patients, almost all of them, 117 (88.6%) exposed to their sexual partner followed by their close families 96 (72.7%). But, only 24 (18.2%) of them publicized as they infected by the HIV/AIDS to every community.
In contrary to this study results, the study done in National Hospital Abuja, Nigeria showed that 228 (95.0%) had disclosed their HIV status and most, 121 (50.4%) had disclosed to their sexual partners [19]. In a similar way, the research done in North-Eastern Nigeria reflected that most 97.5% had disclosed their HIV status and majority 36.8%disclosed to their spouses [17]. Also the study done in Mwanza, Tanzania, 252 (93.3%) of participants disclosed their sero-status to other people [20]. Moreover, this study has in contrary result with the study done at Sokode Regional Hospital, Togo that 131 (60.9%) had disclosed their HIV sero-status to their sexual partners [21]. The above articles’ findings showed that there was higher disclosure rate to other peoples and low disclosure rate to their sexual partners. But, for this study finding, disclosure to sexual partners were higher than that the total people. This difference in findings might be resulted due to the sociocultural differences of the underlying communities.
Again, this study results were inconsistent with the research done in Mekelle Hospital, Ethiopia, in that the overall HIV status disclosure to sexual partner was 186 (57.4%) [7]. Moreover, the other study done in Mekelle Hospital, Ethiopia on women revealed that 201 (63.8%) of women were disclosed their HIV sero- status to their partners [22]. This discrepancy in the results of both studies might be resulted due to the time period and difference in socio- demography, cultures and socio - economies of the study participants.
In another way, this study results were almost conformed with the study done in Kampala, Uganda that 646 (81%) reportedas they had disclosed their HIV status to their sexual partners [23].
Again, the findings of this study similar to the study done in Hawassa University Referral Hospital, SNNPR, Ethiopia, which 85.7% of the women had disclosed their HIV positive status to their sexual partners [14]. Similar to the above study, the investigation done in Jimma Hospital, Ethiopia has shown that the majority (94.5%) disclosed their HIV sero- positive status result to at least one person and 90.8% disclosed to their current main partners [13]. The resulted similarity might be due to study place the closeness and the same with this study area.
Moreover, this study were in line with the study done in Kemissie district, Northeast Ethiopia that 335 (93.1%) had disclosed their HIV sero- positive results to their main current sexual partners, 263 (73.1%) had disclosed their HIV sero- status positivity results to at least one of their families and 219 (60.8%) had told their HIV sero- positive result to one or more of their friends [16]. Additionally, the research done in Axum Health Facilities, Tigray, Northern Ethiopia obtained that the majority (80.1%) disclosed their HIV sero - positive result to at least one person. From currently have a sexual partner, 81.2% disclosed to their current sexual partners [24]. Furthermore, a study done in Ambo Hospital, Ethiopia also revealed that the prevalence of HIV sero-positive status disclosure to at least one person was 86.2% and 84.9% study subjects were disclosed their HIV positive sero status to their sexual partners [25]. Those above listed studies had similar findings with this study. This similarity might be due to study period closeness to each other and underlying study participants had a much close sociocultural and economic background.
The practice of the disclosure of their HIV-positive status information to other peoples is not stress-free itself. They had terror or fear of the community reactions towards them after their disclosure. As a result, to make smooth the disclosure process for better consequences for individuals and their close groups, scanning of factors that contribute to the decision to disclose is very core points in supporting the actions of disclosure in multi dimensions. Accordingly, this investigation identified different factors such as; Age, sex, educational status, ability to perform any physical exercise, WHO stage at start of HAART drugs, general health conditions, length of time they stayed on ART treatment, comorbidity conditions with other diseases, having any clinical symptoms for HIV/AIDS, physical domain of quality of life, social domain of quality of life and the general quality of life status had statistically significant associations with HIV sero-positive status disclosure.
Similar to this study findings, the research done in China displayed that disclosing HIV sero- status to sexual partners was significantly related to better quality of relationship with partners and as well as open and effective communication within family members [26]. In similar to the above study, the other study done as Africa continent also shown that fear of discriminations; an anticipated disruption of relationships in their social life, a desire to protect oneself and others emotions possibility of verbal and physical abuse, stigma and confidentiality of their HIV positive sero - status information were factors that have statistical associations with HIV positive sero-status disclosure [18]. Likewise, the study done in South Africa showed that women were more likely to disclose their HIV positive sero - status as compared to their male counterparts [27].
In additional in concordant to this study findings, the study done in Mekelle Hospital, Ethiopia publicized that the knowledge of HIV status of their sexual partners, getting pretest counseling from caregivers, passing longer time since the HIV testing positivity detected, knowing people who disclose their HIV positive sero - status to the community before and having discussion with their sexual partners prior to HIV testing could influence disclosure of HIV status [22]. Likewise, this study results supported by the study done in Kemissie District, Northeast Ethiopia that shown prior discussions on HIV related issues, a smooth relationship with their sexual partners and communities and knowing the sexual partner status before were significantly associated with disclosure of their HIV positive sero-status [16]. The other factors that can affect HIV sero- status disclosure were also duration of remain on HIV related care follow up, Marital status, length of time since HIV test was done, knowing the partners HIV status before and prior discussion to each other with sexual partners were the main factors which affect the practice of HIV positive sero-status disclosure [7, 24, 25, 28].
Strengths and limitations
The data of this study were collected by their caregivers and no discomforts were resulted related to their information secret and this can decrease the social desirability bias and fear of information leakage.. Since it’s done only in one hospital, generalizing of these findings for entire population as the region cannot possible. Moreover, the study participants were selected in a systematic random sampling method that can result may be homogeneous or repetition of study participants that had the similar characteristics by its nature. Also data were collected only by quantitative methods and it doesn’t address the information that possible to address only by qualitative methods. Therefore, in future, it is better if both qualitative and quantitative methods of data collections will considered while conduction of investigation on similar study title.
Conclusions
The findings of this study indicated that the disclosure of HIV positive sero - status were very low. Age, sex, educational status, ability to perform any physical exercises, WHO stage at start of HAART drugs, general health conditions, length of time stayed on HAART treatment, presence of comorbidities, presence of any clinical symptoms for HIV/AIDS, physical domain of quality of life social domain of quality of life and the general or overall quality of life status were those factors that affected HIV sero-status positive disclosure.
Acknowledgments
We would like to acknowledge Jimma University for supporting this study financially. Our thanks also extended to Jimma University specialized Hospital manager and Staffs for their cooperation. In addition, our heartfelt thanks also extended to study participants who shared their priceless time to give information. Again, we acknowledge data collectors for their full commitment during data collections. Not the least, but the last, we our gratitude extends to our families, friends and colleagues for all their supports and encouragements during conduction of this study.
Funding
This study was done by Jimma University financial support that received by hands of Tamiru Tesfaye. However, the funder had no role in overall activities in the study such as; in study design, data collection and analysis. Finally, the funder had no role in decision to publish, or preparation of the manuscript for publication.
Availability of data and materials
The data sets that used in this study for analysis and other information are available currently in the hands of the corresponding author and principal investigator. Therefore, they can provide it if requested.
Abbreviations
- AIDS
Acquired Immunodeficiency Syndrome
- AOR
Adjusted Odds Ratio
- ART
Antiretroviral therapy
- CI
Confidence interval
- COR
Crude Odds Ratio
- HAART
Highly active antiretroviral therapy
- HIV
Human Immune Deficiency Virus
- JUSH
Jimma University Specialized Hospital
- PLWHA
People Living with HIV/AIDS
- WHO
World Health Organization
Authors’ contributions
TT is the principal investigator. TT, TB and AA conceived and designed the study. JD assisted the design of the study. TT and JD analyzed the data and interpreted the results. TT and JD prepared and critically reviewed the manuscript. All authors have read and approved the manuscript.
Ethics approval and consent to participate
Before the data collection, Ethical clearance and approval to conduct this research was obtained from the Ethical review Committee of College of Public Health and Medical Sciences, Jimma University. Permission was obtained from JUSH to implement the study. Prior to administering the questionnaires, the aims and objectives of the study were clearly explained to the participants and oral informed consent was obtained. Confidentiality and anonymity were ensured throughout the execution of this study. Since participants were not required disclosing personal information on the questionnaire number was used instead of their name. Participants have been informed that their participation was voluntary and that they can withdraw from the study at any time if they wish to do so. Finally they were assured whether they participate or refuse to participate, they had full right and totally it not have any relationship with their care or services.
Consent for publication
It is not applicable.
Competing interests
None of the authors have any competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tamiru Tesfaye, Email: tamirutesfaye00@gmail.com.
Jiregna Darega, Phone: +251-910-6722-02, Phone: +251- 973-7605-00, Email: jiregnadarega@yahoo.com.
Tefera Belachew, Email: terabelachew@gmail.com.
Abebe Abera, Email: abeef2011@gmail.com.
References
- 1.UNAIDS. 2016 Core Epidemiology Slides; 2016. UNAIDS. www.unaids.org/sites/default/files/media_asset/AIDS-by-the-numbers-2016_en.pdf.
- 2.UNAIDS. UNAIDS 2016-2021 Strategy; August 2015. www.unaids.org/sites/default/.../20151027_UNAIDS_PCB37_15_18_EN_rev1.pdf.
- 3.UNAIDS. Fact Sheet 2016; www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf.
- 4.Population Reference Bureau. 2015 World Population Data Sheet; 2015. www.prb.org/pdf15/2015-world-population-data-sheet_eng.pdf.
- 5.The Global HIV/AIDS Epidemic. Fact sheet. 2017. www.unaids.org/en/resources/documents/2017/2017_data_book.
- 6.HIV/AIDS Estimates and Projections in Ethiopia, 2011-2016. http://fitun.etharc.org/resources/finish/53-hiv-aids-estimates-and-projections/327-hiv-aids-estimates-and-projections-in-ethiopia-2011-2016.
- 7.Genet M, Sebsibie G and Gultie T. Disclosure of HIV seropositive status to sexual partners and its associated factors among patients attending antiretroviral treatment clinic follow up at Mekelle Hospital, Ethiopia: a cross-sectional study BMC Research Notes (2015) 8:109. doi:10.1186/s13104-015-1056-5. [DOI] [PMC free article] [PubMed]
- 8.WHO Document Summary. HIV Status Disclosure to Sexual Partners: Rates, Barriers and Outcomes for Women, Rates of HIV status disclosure. 2004. apps.who.int/iris/bitstream/10665/42717/2/9241590734_summary.pdf.
- 9.Isaac K. And Fred N. Factors influencing disclosure of HIV positive status in Mityana district of Uganda. African Health Sciences. Vol 9 No 1, 2009. [PMC free article] [PubMed]
- 10.Lorenz R, Grant E, Muyindike W, Maling S, Card C, Henry C, et al. Caregivers’ Attitudes towards HIV Testing and Disclosure of HIV Status to At-Risk Children in Rural Uganda. PLoS ONE. 2016;11(2):e0148950. https://doi.org/10.1371/journal.pone.0148950. [DOI] [PMC free article] [PubMed]
- 11.Profile of Jimma University Specialized Hospital. 2014. http://www.ju.edu.et/jimma-university-specialized-hospital.
- 12.Jimma University Specialized Hospital report. Jimma, Oromiya, Ethiopia. 2014.
- 13.Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A. Disclosure experience and associated factors among HIV positive men and women clinical service users in southwest Ethiopia. BMC Public Health. 2008;8:81. https://doi.org/10.1186/1471-2458-8-81 [DOI] [PMC free article] [PubMed]
- 14.Taye G, Dereje H, Endrias M. HIV positive status disclosure to sexual partner among women attending ART clinic at Awassa University Referral Hospital. Ethiopia Ethiop J Health Dev. 2010;24(1):9–14. [Google Scholar]
- 15.Deribe K, Lingerh W. Determinants and outcomes of disclosing HIV-sero positive status to sexual partners among women in Gore and Mettu Town, Illubabor Zone. Southeast Ethiopia Ethiop J Health Dev. 2005;19(2):126–131. [Google Scholar]
- 16.Seid M, Wasie B, Admassu M. Disclosure of HIV Positive Result to a Sexual Partner among Adult Clinical Service Users in Kemissie District, Northeast Ethiopia. Afr J Reprod Health March. 2012;16(1):97–104. [PubMed] [Google Scholar]
- 17.Raymond SD, Alhaji AA, Peter N, Patrick N, Okechukwu O, Dahiru T, et al. HIV disclosure status and factors among adult HIV positive patients in a secondary health facility in North-Eastern Nigeria, 2011. Pan Afr Med J. 2014;18(Supp 1):4. doi: 10.11694/pamj.supp.2014.18.1.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minrie G, Rene P, Lucia NM, Priscilla SD, William LH, Joanne RN, et al. Disclosure of HIV Status: Experiences and Perceptions of Persons Living With HIV/AIDS and Nurses Involved in Their Care in Africa. Qual Health Res. 2008;18(3):311–24. http://journals.sagepub.com/doi/abs/10.1177/1049732307311118. [DOI] [PubMed]
- 19.Olutayo FM, Hipoletus CN, Iliya SD and Kingsley CN. Rates, Factors, Timing and Outcomes of HIV Status Disclosure Among Patients Attending the Special Treatment Clinic of the National Hospital Abuja Nigeria. Int J HIV/AIDS Prev, Educ Behav Sci. 2016;2(3):13–19. doi: https://doi.org/10.11648/j.ijhpebs.20160203.11.
- 20.Yonah et al.: HIV serostatus disclosure among people living with HIV/AIDS in Mwanza, Tanzania. AIDS Research and Therapy 2014 11:5. doi:10.1186/1742-6405-11-5. [DOI] [PMC free article] [PubMed]
- 21.Yaya I, Saka B, Landoh DE, Patchali PM, Patassi AA, Aboubakari AS, et al. HIV Status Disclosure to Sexual Partners, among People Living with HIV and AIDS on Antiretroviral Therapy in Sokodé Regional Hospital, Togo. PLoS One. 2015;10(2):e0118157. doi: 10.1371/journal.pone.0118157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alemayehu et al.: HIV disclosure to sexual partners and associated factors among woART clinicsing ART clinic at Mekelle hospital, Northern Ethiopia. BMC Public Health 2014 14:746. doi:10.1186/1471-2458-14-746. [DOI] [PMC free article] [PubMed]
- 23.Okello E, Wagner G, Ghosh-Dastidar B, Garnett J, Akena D, Nakasujja N, et al. Depression. Internalized HIV Stigma and HIV Disclosure World Journal of AIDS. 2015;5:30–40. [Google Scholar]
- 24.Berhane H, Awoke W, Bedimo M and Gebremedhin M. HIV Positive Status Disclosure and Associated Factors among HIV Positive Adults in Axum Health Facilities, Tigray, Northern Ethiopia. Science Journal of Public Health. Vol. 3, No. 1, 2015, pp. 61–66. doi: 10.11648/j.sjph.20150301.21.
- 25.Natae SF and Negawo MK. Factors Affecting HIV Positive Status Disclosure among People Living with HIV in West Showa Zone, Oromia, Ethiopia; 2013. Abnorm Behav Psychol 2: 114. 2016. doi:10.4172/abp.1000114.
- 26.Shan Qiao XL, Yuejiao Z, Zhiyong S, ZhenzhuT. AIDS impact special issue 2015: interpersonal factors associated with HIV partner disclosure among HIV-infected people in China. AIDS Care. 2016;28, 37(sup1):–43. 10.1080/09540121.2016.1146397. [DOI] [PMC free article] [PubMed]
- 27.Tshweneagae G.T., Oss, V.M. & Mgutshini T. Disclosure of HIV status to sexual partners by people living with HIV’, Curationis 38(1), Art. #1174, 6 pages. 2015. 10.4102/curationis.v38i1.1174. [DOI] [PMC free article] [PubMed]
- 28.Fekadu H, Addisie M, Mellie H. Sero Status Disclosure and Condom use among Plwhas on Art in Assela Town Health Facilities. Oromiya Region J AIDS Clin Res. 2014;6:414. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets that used in this study for analysis and other information are available currently in the hands of the corresponding author and principal investigator. Therefore, they can provide it if requested.


