Abstract
Loneliness may be related to psychotic symptoms but a comprehensive synthesis of the literature in this area is lacking. The primary aim of the current study is to provide a systematic review and meta-analysis of the association between loneliness and psychotic symptoms in people with psychosis. A search of electronic databases was conducted (PsychINFO, MEDLINE, EMBASE, and Web of Science). A random effects meta-analysis was used to compute a pooled estimate of the correlation between loneliness and psychotic symptoms. Study and outcome quality were assessed using adapted versions of the Agency for Healthcare Research and Quality (AHRQ) tool and GRADE approach, respectively. Thirteen studies were included, providing data from 15 647 participants. A moderate association between psychosis and loneliness was observed (k = 13, N = 15 647, r = .32, 95% CI 0.20, 0.44; I2 = 97.56%; moderate quality evidence). Whether loneliness was assessed by a single-item or a more comprehensive measure had no moderating effect on the estimate. Results indicate that there is a significant positive relationship between loneliness and psychosis. Further studies are needed to determine the causal status of this relationship, but this robust finding should be considered in clinical practice and treatment provision for those with psychotic disorders.
Keywords: psychotic disorders, schizophrenia, social isolation, loneliness measures, review
Introduction
People with psychotic disorders frequently feel lonely and many expect to be lonely in the future.1 Stain et al2 report that as many as 80% of adults with a diagnosis of psychosis in Australia endorsed feeling lonely in the past 12 months. People with psychosis often struggle to develop and preserve functioning relationships, have limited social networks and restricted access to social support outside of what is provided by mental health services.3,4
Although feelings of loneliness and social isolation are generally thought to reflect the negative impact of psychotic experiences,5 more recently it has been reported that loneliness may also play a causal role in the development of psychotic experiences.6 A self-perpetuating cycle of exclusion may develop, whereby the disorder limits connections and support, which then leads to a removal of important buffers, thereby increasing risk of relapse and causing an escalation of psychotic episodes, further social disengagement, and so forth.7
The majority of studies examining social support in psychosis have concentrated on quantitative features of the social network such as size and reciprocity instead of more functional aspects such as loneliness or satisfaction with relationships.7 This is of particular relevance, as objective features of social support are related but distinct from these more subjective aspects of social relationships. Loneliness is an unpleasant and distressing experience resulting from a perceived deficiency in the quantity or quality of one’s social relationships.8 While social isolation can be measured objectively, loneliness is a subjective emotional state of the individual, which may be present in individuals with large social networks, and absent in isolated individuals with minimal social contact.9
Loneliness has been associated with depression and suicide ideation,10 lower life satisfaction,11 elevated blood pressure levels,12 increased stress hormone levels,13 and compromised immune system.14 Loneliness has also been related to an increased tendency to experience subclinical and clinical hallucinations15,16 and to nonclinical paranoid thinking.17,18 Interested readers may consult Hawkley and Cacioppo for a comprehensive review of loneliness.19
There are several possible mechanisms linking loneliness to psychotic symptoms such as hallucinations. For example, loneliness may directly increase anxiety and depression10 which in turn may exacerbate symptoms of psychosis.20 Loneliness may also perpetuate negative beliefs about oneself and other people, which may in turn increase the frequency of paranoid thoughts. Another pathway may involve “anthropomorphism,” whereby social isolation and feelings of loneliness might lead to increased human agency detection in one’s immediate environment, therefore increasing likelihood of hearing voices or perceiving human agency in nonhuman stimuli.21 This relationship may also work in the other direction, whereby psychotic symptoms lead one to experience feelings of exclusion and stigma, which in turn increases likelihood of feeling lonely. Some authors report case-studies where hallucinating patients actually perceived their imaginary companions as helpful in managing their sense of loneliness.22 Similar findings have been reported with otherwise healthy children who have imaginary companions.
Although there has been much focus on the co-occurrence of loneliness and psychosis, their relationship is still unclear. While there is a consensus that loneliness is a prominent feature in psychosis, some researchers report correlations near zero between psychotic symptoms and loneliness.23 Additionally, while some authors report a high prevalence of loneliness in people with psychosis,15 this conclusion is often derived from a single-item measure of loneliness, rather than a valid and reliable instrument, which might lead to confusion and limited replicability of studies. There also appears to be no gold standard in regards to how single-item measures are conceptualized and interpreted, with various authors asking for feelings of loneliness across the past week, past 2 weeks or past 12 months, or taking a measure of the number of “lonely days in a week.” Some researchers divide Likert scale measures of loneliness into a dichotomous measure, while others keep it as a continuous variable.
Improving our understanding of the relationship between psychosis and loneliness has important theoretical and practical implications. In order to design effective interventions for loneliness, and potentially enable services to best organize their resources to support the wellbeing of individuals with psychosis, a deeper understanding of the nature of loneliness and its impact on mental functioning in this population is needed. An important first step is to provide a definitive estimate of the magnitude of the relationship, taking into account study quality. Whether the results depend on the way loneliness is measured is also important to consider, both for interpreting the available evidence and for planning future research. Therefore, the primary aim of the current study is to provide a systematic review and meta-analysis of the association between loneliness and psychotic symptoms in people with psychosis.
Methods
Search Strategy
The electronic databases (PsycINFO, MEDLINE, EMBASE, and Web of Science) were searched up to February 2016 using the following terms: (psychos* or schiz* or halluc* or paran* or delus* or psychotic) AND (lonel*) AND/OR (at risk or ultra high risk or clinical high risk or UHR or CHR or prodrom* or psychosis risk or psychosis transition or psychosis onset). Screening was undertaken independently by 2 authors (B.M. and E.V.) First, titles and abstracts were screened, followed by the full text of remaining articles. Hand searches of references in eligible articles and key review articles were also undertaken. Conference abstracts and theses identified through the searches were also followed-up. All corresponding authors of selected papers were contacted (where possible) regarding any unpublished work they were involved in that could be suitable for the purpose of the current review.
Inclusion and Exclusion Criteria
Studies were eligible for inclusion if they (1) measured psychotic symptoms and loneliness in people experiencing psychosis and (2) measured loneliness symptoms in people diagnosed with psychosis and provided a suitable control group. Cross-sectional baseline data were extracted from longitudinal studies where possible. If not possible an average of reported values was calculated. Authors were contacted in every case where usable but unpublished data were thought to exist.
For the purposes of this review we defined loneliness as dissatisfaction with the desired and actual number or quality of social relationships.24 We did not examine social isolation or size of social network unless it clearly reflected our measure of loneliness. While social isolation can be an objectively quantifiable variable, loneliness is a subjective emotional state of the individual, which may be present in non-isolated individuals with large social networks, and absent in isolated individuals with minimal social networks, and thus involves necessarily subjective measurement.
We defined psychotic disorders as severe mental disorders that cause abnormal thinking and perceptions and included studies that involved people diagnosed with schizophrenia, schizoaffective disorder, schizotypal personality disorder, bipolar disorder with psychotic features, depressive psychosis, delusional disorders, and other nonorganic psychosis. These included both long-term, established psychosis and first-episode psychosis.
Design
A range of study designs was suitable for inclusion, such as case-control studies, where the cases may be defined either by the presence or absence of psychosis, cross-sectional correlational studies and prospective designs where the relationship between psychosis and loneliness was examined over time. We did not include qualitative studies.
Additional Criteria
Only English language articles were included. We did not include studies that did not provide sufficient information for our analysis. For example, studies were excluded if they reported only mean loneliness scores for a group of people with psychosis, but with no control group provided and where no dichotomous distinction was made (lonely vs not lonely). We also did not include papers where a control group was used, but it was not representative of general population (eg, self-reported lonely people from the general population).
Data Extraction
Extraction of study details was undertaken by 1 author (B.M.) using a pre-specified data collection form. In case of any uncertainty articles were discussed further with other authors (P.H. and S.R.). In 2 cases additional information regarding unpublished studies was obtained from authors (Switaj, personal communication; Ludwig, personal communication). In another case further information regarding a relevant study was obtained from authors,25 while in 6 cases further information was needed but contact could not be established with the corresponding author.26–30 All relevant statistics were estimated from available datasets, with missing cases excluded. In longitudinal studies where correlation between psychotic symptoms and loneliness were reported across different time points, an average correlation was calculated. Similarly, for studies where correlations were reported for separate subscales of psychotic experiences, an average raw correlation was calculated. Where effect size transformation was required, guidelines in Borenstain et al31 were followed.
Methodological Quality
The methodological quality of studies was assessed using an adapted version of the Agency for Healthcare Research and Quality (AHRQ) tool.32 The assessment of all included studies was done by the lead author (BM). In order to ascertain that the quality assessment was accurate, a proportion of papers (6) was also independently assessed for quality by another author (E.V.) with an inter-rater reliability of 80%, and any disagreements resolved by a third author (P.H.). The devised quality criteria checklist followed closely from Taylor et al.33 Studies were rated on a number of methodological parameters as either fulfilling the criteria in full, partially or not fulfilling it. A copy of this adapted measure is provided in supplementary material.
The overall quality of the final outcome was assessed using an adapted version of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach GRADE Working.34 The general GRADE rating includes review of quality of data, publication bias, inconsistency and imprecision and produces the final grade of either high, moderate, low or very low quality. General data quality was assessed by using the AHRQ reports for studies contributing to that specific outcome. Publication bias was assessed using funnel plot, Egger’s regression test and the Rank correlation test. Inconsistency was assessed via assessment of heterogeneity and overall direction and magnitude of effect, and imprecision was assessed via assessment of effect size, confidence intervals and overall number of participants contributing to the analyses. The specific criteria that were used for making AHRQ and GRADE ratings are detailed in supplementary material.
Registration of Protocol and Subsequent Changes
The review protocol was registered and published in the public domain (PROSPERO Registration CRD42016015371) before searches, data extraction and analysis were conducted. Subsequent changes included narrowing the research question from psychosis continuum to people with established psychosis and addition of a second person to conduct the search in parallel. In addition, a decision was made to run the meta-analysis on correlational data rather than odds ratios. This decision was made once papers were screened in full and it became apparent that majority of the included studies reported correlations; it therefore seemed more appropriate to convert effect sizes to the one most commonly reported in our specific pool of studies, therefore reducing reliance on potentially untested assumptions. Due to insufficient data, it was decided to drop a comparison between people diagnosed with psychosis and those with other non-psychotic mental health problems or at risk of developing psychosis. Finally, we performed an additional moderator analysis to examine whether the results were affected by stage of illness of study participants.
Data Synthesis and Analysis
For each of the studies, a correlation coefficient (r) of the relationship between psychosis and loneliness was computed. Data conversion was conducted in accordance with guidelines in Borenstein et al31 Converting effect sizes into 1 metric allows continuous and binary data from a range of different measures reported in a range of different study designs to be combined, thus increasing the efficiency and power of the analysis. These correlation coefficients were then transformed into Fisher’s z and entered into a random-effects meta-analysis. Meta-analysis was conducted with a use of R version 3.2.3, package: Metafor.35
Results
Study Characteristics
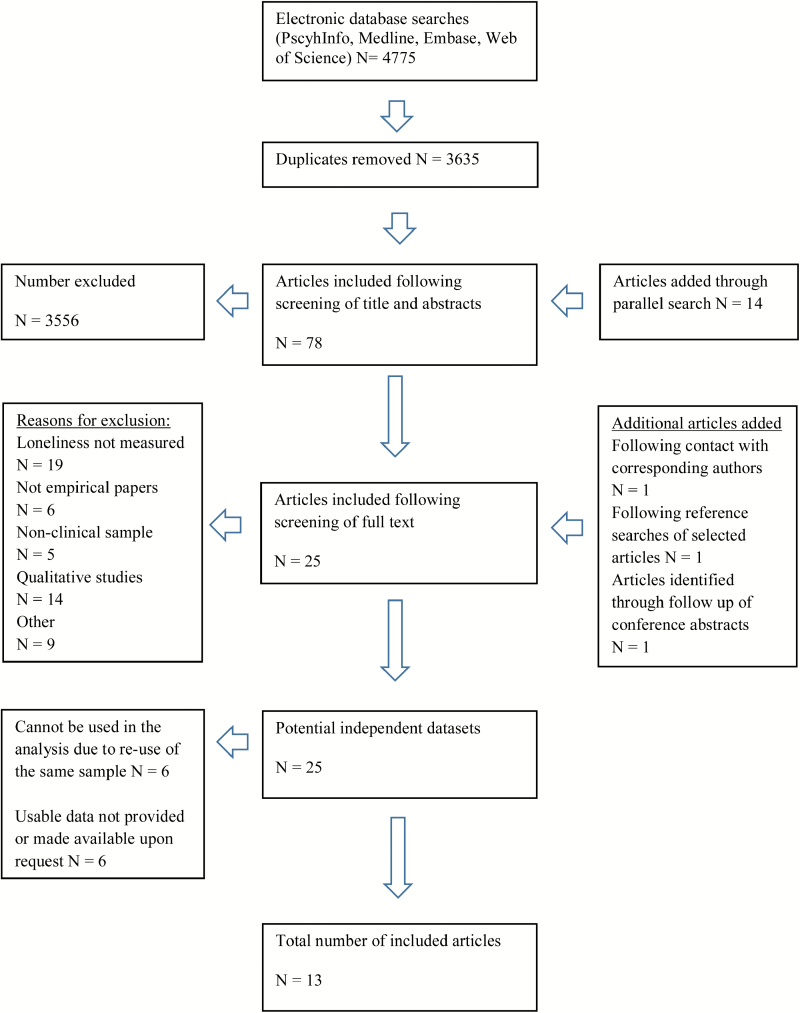
As shown in figure 1, there were 13 eligible studies, reported data related to 15 647 participants. Study characteristics are presented in table 1. Two studies were conducted on people with first onset psychosis and one related to people with late onset psychosis, while the remaining 10 assessed people with established psychosis. Nearly all of the studies employed a cross-sectional design. Studies originated from a variety of countries including the United States, Great Britain, Australia, Germany, Israel, and Poland. A list of excluded studies, with reasons for exclusion, is provided in the supplementary material.
Fig. 1.
Prisma chart.
Table 1.
Characteristics of Included Studies
| Authors, Year, Country | Groups Included in Review/Design | N Participants | Age, Mean (SD) | Proportion Male (%) | Recruitment Source | Ethnicity | Psychotic Symptoms Measure | Loneliness Measure |
|---|---|---|---|---|---|---|---|---|
| Angell et al, 2002, United States | Adults with schizophrenia | 61 | 20–24, n = 44 | 62/87 (71%) | Evaluation of the Program of Assertive Community Treatment (PACT) | Caucasian (95%) | 18-item version of the Brief Psychiatric Rating Scale | 1-item scale: Loneliness defined as the number of days (range = 0–7) in which the subject reported feeling lonely and in need of companionship during the week preceding the interview |
| Schizoaffective disorder | 21 | 25–29, n = 26 | African American (4%) | |||||
| Schizotypal personality disorder | 2 | 30–32, n = 17 | Latino (1%) | |||||
| Total longitudinal design | 87 | Mean age not reported | ||||||
| Badcock et al, 2015, Australia (also: Stain et al 2012) | Schizophrenia | 835 | Not lonely, 37.5 (11.4) | 979/1603 (61%) | The second Australian National Survey of Psychosis | Not reported | No measure/ Diagnostic Interview for Psychosis Diagnosis | 1-item scale: “In the last 12 months have you felt lonely?” 4-point scale: (1) I have plenty of friends and have not been lonely; (2) Although I have friends I have been lonely occasionally; (3) I have some friends but have been lonely for company; and (4) I have felt socially isolated and lonely |
| Schizoaffective disorder | 287 | |||||||
| Bipolar disorder with psychotic features | 314 | Lonely, 38.3 (10.9) | ||||||
| Depressive psychosis | 80 | |||||||
| Delusional disorders and other nonorganic psychosis | 87 | |||||||
| Total | 1603 | |||||||
| Authors referred to a similar survey conducted on general population in New Zealand as a control group/ cross-sectional | ||||||||
| Gayer-Anderson et al, 2014, England, conference abstract | First-presentation psychosis cases | 227 | Not reported | Not reported | The Childhood Adversity and Psychosis (CAPsy) Study | Not reported | Not reported | Not reported |
| Unaffected population- based controls | 199 | |||||||
| Giblin et al, 2004, United Kingdom | People with a diagnosis of Late-onset psychosis (LOP) | 14 | 77.7 (6.6) | 2/14 | Patients: recruited via mental health teams | Not reported | No measure/ diagnosis instead | “Lonely dissatisfaction” item on Philadelphia Geriatric Center Morale Scale |
| Late-onset depression (DEP) | 13 | 76.1 (6.4) | 5/13 | Controls: recruited from local community sources | (Higher score – higher morale) | |||
| Healthy older volunteers (HEV) cross- sectional design | 18 | 73.4 (7.8) | 3/18 | |||||
| Lindner at al, 2014, Germany | Schizophrenia patients | 36 | 30.8 (7.9) | 22/36 | Psychiatric in-patients | Not reported | SANS and SAPS | Multidimensional loneliness questionnaire (Multidimensionaler Einsamkeitsfragebogen; MEF) |
| Healthy controls cross- sectional design | 40 | 29.5 (8.3) | 27/40 | Controls: not reported | ||||
| Ludwig et al, 2013 United States, Conference abstract— unpublished study | Persons with schizophrenia | 34 | 34.1 (9.0) | 23:11 | Recruited from a pool of potential participants within the Brain Behavior Laboratory at the University of Pennsylvania | Not reported | SAPS, SANS | Revised UCLA |
| Controls cross-sectional design | 33 | 32.5 (11.2) | 22:11 | |||||
| Meltzer et al, 2013. England (also; Shevlin et al, 2015; Boyda et al, 2015; and McManus et al, 2009) | “Probable psychosis” of schizophrenia or affective disorder cross-sectional design. | 23 | Not reported | Not reported | Adult psychiatric morbidity survey 2007 | Not reported | No measure/ diagnosis based on SCAN (Schedule for Clinical Assessment in Neuropsychiatry) | 1-item “I feel lonely and isolated from other people” (over the past 2 weeks) |
| non-psychotic control group | 7398 | Likert scale ranging from “1– Not at all” to “4–Very much”. | ||||||
| Roe et al, 2011, Israel | People diagnosed with schizophrenia or schizoaffective disorder cross-sectional design | 159 | 43.2 (10.7) | 66.7% men | Psychiatric rehabilitation residential centers | Not reported | Modified BPRS-E | Social and emotional loneliness scale—short version (S-SELAS) |
| Stein et al, 2013, United States | Young adults diagnosed with schizophrenia or bipolar disorder | 30 | 23.7 (2.75) | 18 men, 12 women | Participants were part of a longitudinal research project that examined life course changes for individuals and families coping with serious mental illness. | Proportions in both samples were the same: Caucasian (80%) African American (20%). | No measure/ diagnosis | UCLA Loneliness Scale |
| Parents of these young adults cross-sectional design | 30 | 50.3 (7.4) | 28 mothers, 2 fathers | |||||
| Sundermann et al, 2014, England | Individuals with a first episode in psychosis cross- sectional design | 38 | 23/38 (60.5%) | 32.3 (9.6) | NHS outpatient services within a South London NHS Foundation Trust | Caucasian 20 (52.6%) | SAPS, SANS | 1-item measure “how many days have you felt lonely and in need of companionship in the past week?” |
| African American 13 (34.2%) | ||||||||
| Other 5 (13.3%) | ||||||||
| Switaj et al, 2014, Poland (also: Switaj et al, 2015, and Wciorka et al, 2015) | Patients with psychotic disorders cross-sectional design | 110 | 38.4 (11.4) | 43/110 (39.1%) | Mental health care facilities in Warsaw | Not reported | BPRS | A short version of the De Jong Gierveld Loneliness Scale (DJGLS) |
| Switaj et al, 2016, Poland (in press) | Patients with psychotic disorders (ICD-10 categories: F20–F29) | 207 | Not reported | Not reported | Not reported | Not reported | 18-item BPRS. | 11-item De Jong Gierveld Loneliness Scale |
| Control group | 207 | |||||||
| Tietjen, 1993, United States | No clinical diagnosis | 87 | Range: 24–59, mean/ SD not reported | 24/87 (30.8%) | Patients receiving treatment at psychiatric hospital | Non clinical, Black: 10.4%; White: 89.6% | SCL-90-R Symptom checklist 90 revised | ESLI, Emotional & Social Loneliness Inventory |
| Diagnosed with affective disorder | 92 | 29/92 (36.3%) | Controls: students of general studies | Affect. Disor., Black:13%; White: 87% | ||||
| Diagnosed with schizophrenia (DCM III) | 93 | 45/93 (57.7%) | Schizophrenia, Black:16.2%; White: 83.8% | |||||
Study Quality
The assessment of study methodological quality is outlined in table 2. The most prevalent methodological weaknesses related to justification of sample size, reporting of how missing data was handled and ascertaining an appropriately matched control group. Studies varied in how the psychotic symptoms were reported, with some studies reporting presence of diagnosis of psychosis only, while others reported scores on validated measures of psychotic symptoms such as BPRS or SANS/SAPS. This, however, is partially related to the fact that not all of the studies were designed to answer the specific question of the current meta-analysis. Four studies measured loneliness with a single-item measure. Only one study reported a power calculation (Sündermann et al36). Most studies provided adequate information regarding sample characteristics and used valid and reliable measures to rate loneliness and psychotic symptoms.
Table 2.
Assessment of Study Quality
| Study Ref | Unbiased Selection of the Cohort | Selection Minimizes Baseline Differences in Prognostic Factors? | Sample Size Calculated? | Adequate Description of the Cohort? | Validated Method for Ascertaining Psychotic Symptoms | Validated Method for Ascertaining Loneliness | Adequate Handling of Missing Data |
|---|---|---|---|---|---|---|---|
| Angell et al, 2002 | Partial | Yes | No/not reported | Yes | Yes | No | Yes |
| Badcock et al, 2015 | Yes | Partial | n/a | Yes | Yes | No | Yes |
| Gayer-Anderson et al, 2014 (conference abstract) | Not reported | Not reported | No/not reported | Not reported | Not reported | Not reported | Not reported |
| Giblin et al, 2004 | Partial | Partial | No/not reported | Partial | Yes | Yes | Not reported |
| Lindner et al, 2014 | Unclear | Not reported | No/not reported | Partial | Yes | Yes | Not reported |
| Ludwig et al, 2013 unpublished | Partial | Yes | No/not reported | Partial | yes | Yes | Not reported |
| Meltzer et al, 2013 | Yes | Yes | n/a | Yes | Partial | No | No |
| Roe et al, 2011 | Partial | n/a (no control group) | No/not reported | Yes | Yes | Yes | Yes |
| Sundermann et al, 2014 | Partial | n/a (no control group) | Yes | Yes | yes | No | Yes |
| Stein et al, 2013 | Partial | No | No/not reported | Yes | Partial | Yes | Not reported |
| Switaj et al, 2014 | Partial | n/a (no control group) | No/not reported | Partial | Yes | Yes | Not reported |
| Switaj et al, 2016—in press | Not reported | Yes | No/not reported | Not reported | Yes | Yes | Not reported |
| Tietjen, 1993 | Partial | No | No/not reported | Yes | Yes | Yes | Not reported |
Outcome Quality
Based on the GRADE criteria we downgraded the overall outcome by 1 point due to the high heterogeneity as indicated by the I2 statistic and estimated the quality of the final outcome as moderate (please see supplementary material for more detail).
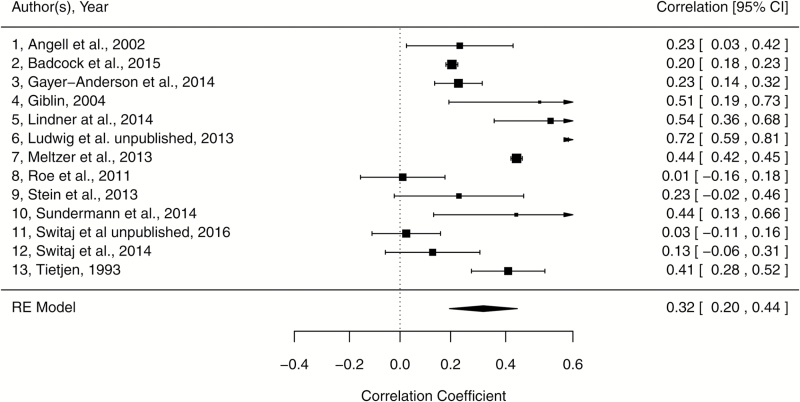
Association Between Loneliness and Psychotic Symptoms
There was moderate quality evidence suggesting a significant moderate association between psychosis and loneliness (Fisher’s z estimate = 0.33, SE = 0.07, z-value = 4.81, P < .001, 95% CI: 0.1981, 0.4704). These values were converted back to correlation coefficient which produced the estimate of r = .32 (95% CI: 0.20, 0.44) which is considered a medium effect size, according to Cohen’s criteria (see figure 2 for reference).37
Fig. 2.
Forest plot.
The I2 statistic was 97.56% indicating that the majority of variation in the estimated effect sizes reflected actual differences in the population mean (95% CI: 94.42, 99.20, Q(12) = 316.43, P < .001). A Bajaut plot suggested that one study (Ludwig et al, unpublished) was influential in its contribution to the overall heterogeneity and the overall result. However, because exclusion of this study did not lead to a reduction in the proportion of true heterogeneity (I2 = 95.93, 95% CI: 89.62, 98.83) nor did it significantly change the overall effect size (r = .28, 95% CI: 0.17, 0.38), consequently it was decided to keep the study in the meta-analysis.
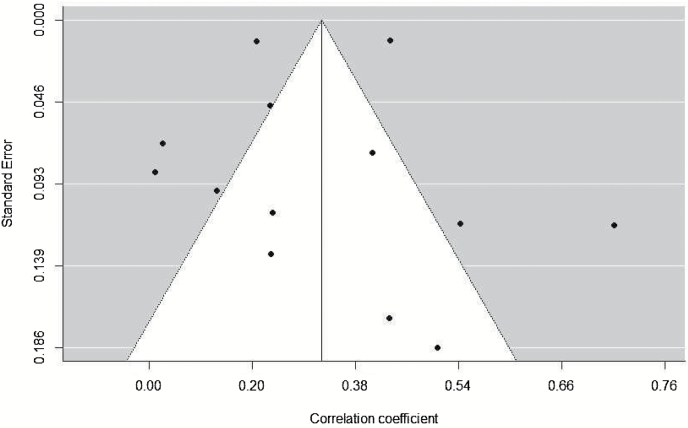
Publication Bias
Although a funnel plot of effect size against SE (figure 3) appeared to be asymmetric, neither Egger’s regression test (P = .29) nor the Rank correlation test (P = .13) was statistically significant. Overall, there was no clear evidence of publication bias according to these tests.
Fig. 3.
Funnel plot.
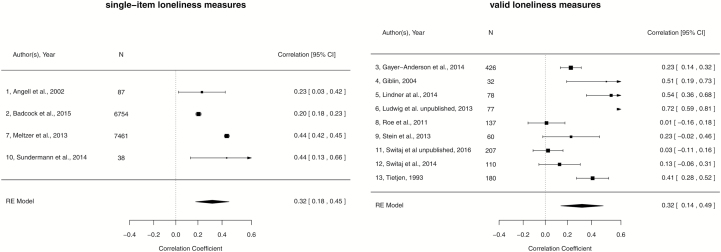
Moderator Analyses
Whilst blinding of researcher to participant status (eg, psychosis or control) had been pre-specified as a potential moderator of interest, none of the studies reported using blinding, therefore this analysis was not possible. Results of the moderator analysis for single-item vs comprehensive self-report measure of loneliness was not significant (Q(1) = 0.001, P = .97). As figure 4 illustrates, there was no evidence that studies that employed very brief measures of loneliness produced different estimates than studies using more comprehensive assessments. We also examined whether the results were affected by stage of illness (first onset/late onset [k = 3] vs established psychosis [k = 10]), and found no significant differences (Q(1) = 0.01, P = .92).
Fig. 4.
Sensitivity analysis.
Discussion
The current analysis confirms that there is a significant relationship between loneliness and psychotic symptoms in people with psychosis. This finding is in line with growing evidence that loneliness is a common feature in psychosis15,38 and should be considered in further conceptualizations of psychotic disorders and treatment planning.
Could Loneliness Cause Psychotic Symptoms?
While the evidence from the current analysis supports the concept of psychosis and loneliness being significantly inter-related, the nature of this relationship is still unclear. Gayer-Anderson and Morgan7 postulated the self-preserving cycle of psychosis and loneliness, and suggested that loneliness playing a maintaining role in psychotic experiences; however, it is also possible that loneliness might serve a crucial role in psychosis onset.6 The concept of a psychosis phenotype can be expressed at levels below its clinical manifestation, commonly referred to as psychosis proneness, psychotic experiences, schizotypy, or at-risk mental states.39,40 It therefore seems likely that loneliness might be inter-related to psychotic symptoms at earlier, subclinical stages of psychotic presentation. A cognitive model of psychosis proposed by Garety et al41 suggests that one of the pathways to the development of psychosis might be via poor self-concept and self-esteem42,43 which might impact on maladaptive cognitions of self and others. Self-esteem is poor in many people with psychosis44 while hallucinations and delusions that have negative content are associated with negative self-concepts.45 It would be reasonable to assume that feelings of loneliness can strengthen negative self-concepts and impact negatively on self-esteem. Garety et al41 suggest that psychotic beliefs are likely to be more rigidly held if they are consistent with firmly-held distorted beliefs about the self (eg, that one is different), others (eg, that others are hostile) and the world (eg, the world is dangerous). In other words, this cognitive model would fit well with the hypothesis that loneliness could increase psychotic symptoms. While some authors propose that loneliness mediates the development of psychotic symptoms,6,46 others suggest that loneliness might be secondary to psychotic experiences. Riggio and Kwong,18 eg, reported that deficits in social skills and paranoid thinking independently predicted greater loneliness and fewer social supports in otherwise healthy individuals. Further studies aimed at investigating the occurrence and role of loneliness across psychotic continuum would be helpful in determining whether it precedes the onset of psychosis or occurs as a result of the condition. In particular, studies of experimental design with loneliness as the manipulated variable would be helpful in establishing whether there is a casual relationship.
Single-Item Loneliness Measures
The findings of the moderator and sensitivity analyses regarding the type of loneliness measures used supports the idea that a single item loneliness measure produces results in line with those acquired using valid and reliable instruments. It seems important, however, to highlight that the way the single-item measures are used is usually influenced by the type of study conducted. They seem particularly prevalent in surveys, where participants respond to a large number of questions and the analysis of findings might be exploratory, rather than set out to test a primary hypothesis. There is a risk in interpreting results obtained in this fashion, as no reliability is guaranteed, while the large number of responders is likely to produce significant effects. One example of how unreliable single-item measures might be is provided in Angell and Test,47 where in their longitudinal design researchers took measure of loneliness across different time points (using a single-item measure). The correlation in endorsement of state loneliness between 2 time points (at 18 mo after study entry, and then at 24 mo) was r = .14, whereas the correlation on a valid measure of thought disturbance at these time points was r = .45. Although this may reflect inherent instability in state loneliness rather than poor reliability, it is important that results from single-item measures are considered with care.
Implications for Clinical Practice
Some authors suggest a link between loneliness and recovery from psychosis. Jackson et al48 compared the effectiveness of Active Cognitive Therapy and Befriending in reduction of psychosis symptoms and functional improvement in people with first episode of psychosis. They reported equal effectiveness of the 2 treatments, which is suggestive of a significant role of befriending in psychosis recovery. This finding is congruent with findings of Roe et al25 who reported that patients’ subjective recovery from psychosis was significantly associated with a decrease in loneliness. It therefore appears that increased loneliness may play a role in the maintenance of psychosis, but also that a decrease in loneliness may be related to subsequent recovery. However, the results of the Adult Psychiatric Morbidity Survey in England15 suggest that traditional approaches to reducing loneliness, such as increased social support and participation, had only a limited effect on subjective loneliness. This raises the possibility that these strategies, which are often applied in order to reduce loneliness in people with psychotic disorders, might not be very effective. Badcock et al38 reported that loneliness amongst people with psychotic disorders was particularly associated with thought disturbance and reduced sense of pleasure. Thus, increasing possibilities for social interaction might not always be effective; if one does not derive pleasure from social contact or has negative cognitions related to social participation, then a positive outcome of the intervention is unlikely. In addition, having a confidante has been associated with lower levels of loneliness49 which would be suggestive of the importance of the quality of interaction rather than the quantity. It thus seems essential that in clinical practice particular attention is given to loneliness and the maintaining role it might have in psychotic experiences. It is important to consider that patients with psychosis are often longing for social contact but lacking resources to build them and maintain. Consequently, treatment options might involve changing maladaptive cognitions,50 while at the same time providing high quality social contact. Indeed, this may be one reason why the therapeutic relationship has been found to be such a crucial factor in ensuring effective and safe psychological therapy for psychosis.51
Strengths and Limitations
We decided, a priori, to adopt a deliberately inclusive approach for this meta-analysis. Although this is recommended52 and although it ensures we made the best use of the limited studies available, the cost is inevitably considerable heterogeneity among studies in terms of population (including stage of illness), methodological design and quality. It may be argued that limiting the analysis to studies that look at one particular type of psychotic disorder, or at one particular population (eg, late onset only, first episode only) may have increased the homogeneity of the results—thus giving us confidence that any residual heterogeneity was not attributable to these factors. However, an inclusive approach to meta-analysis is arguably more transparent and informative. Unlike a more restrictive meta-analysis, this approach minimizes the number of a priori assumptions we have to make about moderating factors, and instead allows us to produce empirical data on the effect of excluding such subgroups. Indeed, we found no evidence that stage of illness acted to moderate the overall effect, which suggests the observed relationship between psychosis and loneliness is a robust one.
Studies of various types of psychotic disorders were included in our meta-analysis. This reflects our decision to operate with a broad definition of psychosis, rather than focus on specific symptoms. However, we note that negative symptoms such as withdrawal or loss of pleasure are significantly different from positive symptoms such as hallucinations and delusions. For example, Badcock and colleagues38 reported data on 12 specific symptoms, including delusions, hallucinations, thought disorder, passivity etc. and found significant correlations with loneliness only for 2 of them (thought disorder and loss of pleasure). Given our broad inclusion criteria which included bipolar disorder and schizoaffective disorder (both of which entail periods of mania or hypomania, which may involve heightened/lowered social activities) it is possible that breaking the sample up into different diagnosis would reveal different strengths of the relationship. However, there were not enough studies to do this.
Although our meta-analysis provides important data on the nature of the psychosis-loneliness relationship, future meta-analyses may benefit from adopting a symptom-specific approach. Their results may present less heterogeneity as a consequence, and the value of such work for understanding the onset and maintenance of specific psychotic symptoms may be high.
It is also important to consider that our quality assessment relates very much to the hypothesis we are testing. Although we criticized the quality of several of the included studies, we did this simply so that we could form a view as to the reliability of the estimate. We fully recognize that many of the studies did not set out to examine the link between psychosis and loneliness, and often only reported loneliness data as a secondary outcome.
Some of the included studies reported adjusted OR only15 which further complicates the analysis, for various authors adjust for different parameters and this leads to difficulty in interpreting the synthesized results. Nonetheless, there was no evidence that the overall effect was moderated by these individual studies.
Although tests of publication bias were not significant, it is possible that this was due to a limited number of studies included in this analysis.53 A visual inspection of the funnel plot did suggest that small studies reporting limited or no relationship between psychosis and loneliness may be lacking. Publication bias is of course an endemic problem54 and, as with clinical trials, pre-registration of empirical research could help to reduce—or at least measure—non-publication of nonsignificant results.54
Six studies that appeared relevant for the current analysis were not included due to difficulty in obtaining usable data. In addition, we did not include studies that were not published in English. Noninclusion of studies is of particular concern in systematic reviews of observational studies as there is inevitably a greater threat of publication bias with this sort of research than, eg, treatment effectiveness research.55 On the other hand, we were not completely unsuccessful in acquiring unpublished data or information; in fact, 3 authors replied to our queries meaning we were able to include data from 13 studies, instead of 10.
A particular strength of our review and meta-analysis is that we sought to pre-register the hypotheses and methodology in the public domain.56,57 As noted elsewhere,56,58 systematic reviews and meta-analysis are far from immune from risks of selective reporting bias and hypothesizing after the results are known. Although we made some changes to our protocol after registering it (largely to reduce scope), pre-registration ensures complete transparency about these, thus allowing readers to judge for themselves whether they are driven by issues relating to feasibility, new information, or bias.
Conclusion
This review and meta-analysis has provided clear evidence that there is a significant relationship, moderate in magnitude, between loneliness and psychotic symptoms in people with psychosis. Although there was high heterogeneity across different studies, the overall relationship was robust. Such a finding is congruent with other evidence, as well as recent theoretical accounts of psychosis.41,59 This finding should be considered in clinical practice and treatment provision for those with psychotic disorders. However further studies are needed to test the hypothesis that loneliness may cause psychosis. In particular, studies examining the effect of experimentally manipulating loneliness on psychotic symptoms are essential for understanding the causal status and direction of the relationship we have observed here.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Supplementary Material
Acknowledgments
We would like to thank Prof David Roe, Dr Krystal Ludwig, and Dr Piotr Switaj for providing us with additional information about their studies. We would also like to thank all other authors who contacted us with information on any unpublished studies. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Morgan VA, Waterreus A, Jablensky A, et al. People living with psychotic illness in 2010: the second Australian national survey of psychosis. Aust N Z J Psychiatry. 2012;46:735–752. [DOI] [PubMed] [Google Scholar]
- 2. Stain HJ, Galletly CA, Clark S, et al. Understanding the social costs of psychosis: the experience of adults affected by psychosis identified within the second Australian National Survey of Psychosis. Aust N Z J Psychiatry. 2012;46:879–889. [DOI] [PubMed] [Google Scholar]
- 3. Norman RM, Malla AK, Manchanda R, Harricharan R, Takhar J, Northcott S. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. 2005;80:227–234. [DOI] [PubMed] [Google Scholar]
- 4. Beels CC. Social support and schizophrenia. Schizophr Bull. 1981;7:58–72. [DOI] [PubMed] [Google Scholar]
- 5. Møller P, Husby R. The initial prodrome in schizophrenia: searching for naturalistic core dimensions of experience and behavior. Schizophr Bull. 2000;26:217–232. [DOI] [PubMed] [Google Scholar]
- 6. van der Werf M, van Winkel R, van Boxtel M, van Os J. Evidence that the impact of hearing impairment on psychosis risk is moderated by the level of complexity of the social environment. Schizophr Res. 2010;122:193–198. [DOI] [PubMed] [Google Scholar]
- 7. Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol Psychiatr Sci. 2013;22:131–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hawkley LC. Loneliness and Social Embeddedness in Old Age. Encyclopedia of Geropsychology Singapore: Springer; 2015. [Google Scholar]
- 9. Macdonald EM, Jackson HJ, Hayes RL, Baglioni AJ, Jr, Madden C. Social skill as determinant of social networks and perceived social support in schizophrenia. Schizophr Res. 1998;29:275–286. [DOI] [PubMed] [Google Scholar]
- 10. Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin Psychol Rev. 2006;26:695–718. [DOI] [PubMed] [Google Scholar]
- 11. Schumaker JF, Shea JD, Monfries MM, Groth-Marnat G. Loneliness and life satisfaction in Japan and Australia. J Psychol. 1993;127:65–71. [DOI] [PubMed] [Google Scholar]
- 12. Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21:152–164. [DOI] [PubMed] [Google Scholar]
- 13. Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience–cortisol associations in a population-based sample of older adults. Proc Natl Acad Sci. 2006;103:17058–17063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cacioppo JT, Hawkley LC, Berntson GG. The anatomy of loneliness. Curr Dir Psychol Sci. 2003;12:71–74. [Google Scholar]
- 15. Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48:5–13. [DOI] [PubMed] [Google Scholar]
- 16. Myin-Germeys I, Nicolson NA, Delespaul PA. The context of delusional experiences in the daily life of patients with schizophrenia. Psychol Med. 2001;31:489–498. [DOI] [PubMed] [Google Scholar]
- 17. Freeman D, Pugh K, Antley A, et al. Virtual reality study of paranoid thinking in the general population. Br J Psychiatry. 2008;192:258–263. [DOI] [PubMed] [Google Scholar]
- 18. Riggio HR, Kwong WY. Social skills, paranoid thinking, and social outcomes among young adults. Pers Indiv Diff. 2009;47:492–497. [Google Scholar]
- 19. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Freeman D, Garety PA. Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behav Res Ther. 2003;41:923–947. [DOI] [PubMed] [Google Scholar]
- 21. Epley N, Akalis S, Waytz A, Cacioppo JT. Creating social connection through inferential reproduction: loneliness and perceived agency in gadgets, gods, and greyhounds. Psychol Sci. 2008;19:114–120. [DOI] [PubMed] [Google Scholar]
- 22. Hutton P, Morrison AP, Taylor H. Brief cognitive behavioural therapy for hallucinations: can it help people who decide not to take antipsychotic medication? A case report. Behav Cogn Psychother. 2012;40:111–116. [DOI] [PubMed] [Google Scholar]
- 23. Świtaj P, Grygiel P, Anczewska M, Wciórka J. Loneliness mediates the relationship between internalised stigma and depression among patients with psychotic disorders. Int J Soc Psychiatry. 2014;60:733–740. [DOI] [PubMed] [Google Scholar]
- 24. Peplau LA. Loneliness: A Sourcebook of Current Theory, Research, and Therapy. Vol 36 New York, NY: John Wiley & Sons Inc; 1982. [Google Scholar]
- 25. Roe D, Mashiach-Eizenberg M, Lysaker PH. The relation between objective and subjective domains of recovery among persons with schizophrenia-related disorders. Schizophr Res. 2011;131:133–138. [DOI] [PubMed] [Google Scholar]
- 26. Borge L, Martinsen EW, Ruud T, Watne O, Friis S. Quality of life, loneliness, and social contact among long-term psychiatric patients. Psychiatr Serv. 1999;50:81–84. [DOI] [PubMed] [Google Scholar]
- 27. Cohen CI, Talavera N, Hartung R. Predictors of subjective well-being among older, community-dwelling persons with schizophrenia. Am J Geriatr Psychiatry. 1997;5:145–155. [PubMed] [Google Scholar]
- 28. Pješčić KD, Nenadović MM, Jašović-Gašić M, Trajković G, Kostić M, Ristić-Dimitrijević R. Influence of psycho-social factors on the emergence of depression and suicidal risk in patients with schizophrenia. Psychiatr Danub. 2014;26:226–230. [PubMed] [Google Scholar]
- 29. Young S, Snyder M, Schactman L. Early recovery from Psychotic Spectrum Disorder within a therapeutic community: significance and effects. Psychosis. 2015;7:37–47. [Google Scholar]
- 30. Tylova V, Ptáček R, Kuželová H. 2301–Emotional and social loneliness in etiology and therapy of mental illness. Eur Psychiatry. 2013;28:1.21920709 [Google Scholar]
- 31. Borenstein MH, Higgins L, Rothstein JHR. Introduction to Meta-analysis. Chichester, UK: Wiley; 2009. [Google Scholar]
- 32. Williams JW, Plassman BL, Burke J, Holsinger T, Benjamin S. Preventing Alzheimer’s Disease and Cognitive Decline. Evidence Report/Technology Assessment No. 193 Rockville, MD: Agency for Healthcare Research and Quality; 2010. [PMC free article] [PubMed] [Google Scholar]
- 33. Taylor PJ, Hutton P, Wood L. Are people at risk of psychosis also at risk of suicide and self-harm? A systematic review and meta-analysis. Psychol Med. 2015;45:911–926. [DOI] [PubMed] [Google Scholar]
- 34. Group GW. Grading of Recommendations, Assessment, Development, and Evaluation: Obtenido de 2007. http://www.gradeworkinggroup.org. Accessed December 10, 2015.
- 35. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 36. Sündermann O, Onwumere J, Bebbington P, Kuipers E. Social networks and support in early psychosis: potential mechanisms. Epidemiol Psychiatr Sci. 2013;22:147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 38. Badcock JC, Shah S, Mackinnon A, et al. Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophr Res. 2015;169: 268–273. [DOI] [PubMed] [Google Scholar]
- 39. van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population?Schizophr Res. 2000;45:11–20. [DOI] [PubMed] [Google Scholar]
- 40. Yung AR, Phillips LJ, Yuen HP, et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr Res. 2003;60:21–32. [DOI] [PubMed] [Google Scholar]
- 41. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 42. Trower P, Chadwick P. Pathways to defense of the self: a theory of two types of paranoia. Clin Psychol. 1995;2:263–278. [Google Scholar]
- 43. Kinderman P, Bentall RP. Self-discrepancies and persecutory delusions: evidence for a model of paranoid ideation. J Abnorm Psychol. 1996;105:106–113. [DOI] [PubMed] [Google Scholar]
- 44. Freeman D, Garety P, Fowler D, et al. The London-East Anglia randomized controlled trial of cognitive-behaviour therapy for psychosis. IV: self-esteem and persecutory delusions. Br J Clin Psychol. 1998;37:415–430. [DOI] [PubMed] [Google Scholar]
- 45. Close H, Garety P. Cognitive assessment of voices: further developments in understanding the emotional impact of voices. Br J Clin Psychol. 1998;37:173–188. [DOI] [PubMed] [Google Scholar]
- 46. Boyda D, McFeeters D, Shevlin M. Intimate partner violence, sexual abuse, and the mediating role of loneliness on psychosis. Psychosis. 2015;7:1–13. [Google Scholar]
- 47. Angell B, Test MA. The relationship of clinical factors and environmental opportunities to social functioning in young adults with schizophrenia. Schizophr Bull. 2002;28:259–271. [DOI] [PubMed] [Google Scholar]
- 48. Jackson HJ, McGorry PD, Killackey E, et al. Acute-phase and 1-year follow-up results of a randomized controlled trial of CBT versus Befriending for first-episode psychosis: the ACE project. Psychol Med. 2008;38:725–735. [DOI] [PubMed] [Google Scholar]
- 49. Green LR, Richardson DS, Lago T, Schatten-Jones EC. Network correlates of social and emotional loneliness in young and older adults. Pers Soc Psychol Bull. 2001;27:281–288. [Google Scholar]
- 50. Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10:238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Goldsmith LP, Lewis SW, Dunn G, Bentall RP. Psychological treatments for early psychosis can be beneficial or harmful, depending on the therapeutic alliance: an instrumental variable analysis. Psychol Med. 2015;45:2365–2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Berman NG, Parker RA. Meta-analysis: neither quick nor easy. BMC Med Res Methodol. 2002;2:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176:1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Joober R, Schmitz N, Annable L, Boksa P. Publication bias: what are the challenges and can they be overcome?J Psychiatry Neurosci. 2012;37:149–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867–872. [DOI] [PubMed] [Google Scholar]
- 56. Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L. An international registry of systematic-review protocols. Lancet. 2011;377:108–109. [DOI] [PubMed] [Google Scholar]
- 57. Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–1020. [DOI] [PubMed] [Google Scholar]
- 58. Quintana DS. From pre-registration to publication: a non-technical primer for conducting a meta-analysis to synthesize correlational data. Front Psychol. 2015;6:1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hoffman RE. A social deafferentation hypothesis for induction of active schizophrenia. Schizophr Bull. 2007;33:1066–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.