Abstract
Background
There is evidence for a group of nonclinical individuals with full-blown, persistent psychotic experiences (PEs) but no need-for-care: they are of particular importance in identifying risk and protective factors for clinical psychosis. The aim of this study was to investigate whether reasoning biases are related to PEs or need-for-care.
Method
Two groups with persistent PEs (clinical; n = 74; nonclinical; n = 92) and a control group without PEs (n = 83) were compared on jumping-to-conclusions (JTC) and belief flexibility. A randomly selected subset of interviews (n = 104) was analyzed to examine differences in experiential and rational reasoning.
Results
As predicted JTC was more common in the clinical than the other 2 groups. Unexpectedly no group differences were observed between clinical and nonclinical groups on measures of belief flexibility. However, the clinical group was less likely to employ rational reasoning, while the nonclinical group was more likely to use experiential reasoning plus a combination of both types of reasoning processes, compared to the other 2 groups.
Conclusions
Reasoning biases differ in groups with PEs with and without need-for-care. JTC is associated with need-for-care rather than with PEs. The ability to invoke rational reasoning processes, together with an absence of JTC, may protect against pathological outcomes of persistent PEs. However, marked use of experiential reasoning is associated with the occurrence of PEs in both clinical and nonclinical groups. Implications for theory development, intervention and further research are discussed.
Keywords: jumping-to-conclusions, psychotic experiences, need-for-care, experiential and rational reasoning, cognitive models of psychosis
Introduction
There is growing evidence for the existence of a group of nonclinical individuals with full-blown, persistent psychotic experiences (PEs) but no need-for-care.1 These are individuals with persistent, nondistressing PEs, and they show few signs of distressing delusions or paranoia.1 They also show a flexible range of benign (typically normalizing, often spiritual) appraisals of their anomalous experiences2,3; they do not show the threat-related, maladaptive appraisals commonly seen in clinical groups.4,5 As such this group is of particular importance in identifying risk and protective factors for clinical psychosis.
One protective factor that may distinguish this unique group is an absence of the reasoning biases associated with maladaptive appraisals of anomalous experience. Individuals with distressing delusions, specifically, make decisions on the basis of limited evidence in probabilistic reasoning tasks: the so-called “jumping-to-conclusions” (JTC) data-gathering bias.6 JTC is exacerbated in acute states, and may represent a trait vulnerability7 and a prognostic marker.8 Work on JTC has led to investigations into belief flexibility, defined as the metacognitive ability to reflect on one’s own beliefs,6 and the related bias against disconfirmatory evidence (BADE),9,10 defined as the neglect of counterarguments for decision-making. Lack of belief flexibility is commonly reported in people with clinical delusions, with typical rates ranging between 50% and 75%,6 and is a related but distinct process to JTC and belief conviction.11 To date, belief flexibility has been studied almost exclusively in the context of clinical delusions. The flexible range of benign explanations of experiences observed in individuals with persistent nonclinical PEs, make JTC and belief flexibility constructs of interest for understanding the absence of threat appraisals in this group.4,5
The definition of belief flexibility (ie, an ability to step back, consider the possibility of being mistaken and reflect on alternative explanations) overlaps with the analytic, controlled “type 2” reasoning identified in dual-process models of cognition.12 Recent investigations of reasoning and psychosis have drawn on Epstein’s cognitive-experiential self-theory (CEST) and associated nomenclature of “experiential/ intuitive” (emotion based) and “rational” systems.13 Modest positive correlations have been found between experiential reasoning and paranormal and superstitious beliefs and schizotypy, with rational reasoning showing the converse relationship.14–16 Freeman et al16 also found that a perceived reliance on experiential reasoning is associated with paranoid thinking in the general population, while reliance on deliberation (rational reasoning) is associated with fewer paranoid thoughts. These studies point to the relevance of dual-process models to the psychosis continuum; in particular suggesting that rational reasoning may be associated with reduced paranoia while over-reliance on experiential (emotion-based) reasoning may be associated with unusual beliefs and paranoia across the psychosis continuum.
In summary, studying individuals with persistent nondistressing PEs with no need-for-care can illuminate protective factors mitigating the risk of transition to clinical psychosis. It is important to distinguish this group from individuals with an “at risk mental state” (ARMS) and those in the general population scoring highly on measures of delusion-proneness, on the lower end of the continuum of risk of psychosis, where elevated paranoia would be expected and evidence of reasoning biases would be predicted.7,17,18 We hypothesize that these groups will differ with respect to reasoning biases; and more specifically that the absence of the clinically established biases in JTC and belief flexibility, together with differences in dual-process reasoning may help to explain the adaptive meaning-making in this unique group.
Aims
The primary aim was to investigate whether JTC and belief flexibility are associated with need-for-care rather than PEs alone: individuals with persistent PEs, with and without need-for-care, and a control group without PEs, were compared on responses to standardised assessments of JTC and belief flexibility. A secondary aim was to compare how the three groups reason about their PEs/a personally meaningful belief, applying a dual-process framework (detailed in the “Methods” section).
Hypotheses
The clinical group will be more likely to show JTC than nonclinical and control groups, who will not differ from each other.
The nonclinical and the control groups will be more likely to demonstrate belief flexibility about their own beliefs and a control belief, than the clinical group.
JTC will be associated with belief inflexibility (possibility of being mistaken) across the sample (replicating6).
The nonclinical group will score more highly than the clinical group on rational reasoning. Group differences in experiential reasoning will be explored.
Methods
This was a planned study within the UNIQUE study.1
Participants
Three groups were recruited across 2 sites (Urban—South London; Rural—North Wales): (1) patients with PEs (diagnoses F20–F39) (clinical group; n = 74); (2) individuals with PEs without need-for-care (nonclinical group; n = 92); (3) controls with no PEs (n = 83), matched to nonclinical group in age, gender, ethnicity, and education.
Exclusion (all groups): (1) age <18; (2) insufficient English; (3) neurological history, head injury, epilepsy; (4) primary substance dependence; (5) estimated IQ <70 (10 individuals otherwise meeting criteria for the clinical group had estimated IQ below 70 and were excluded on the basis that reasoning task performances may not be valid.)
Main inclusion criterion for clinical/nonclinical groups was evidence of current PEs (past month/ in clear consciousness), scoring ≥2 (“occasional”) on at least one item of the Scale for the Assessment of Positive Symptoms (SAPS19). Specific inclusion criteria for nonclinical group: (1) experiences started ≥5 years previously (avoiding possibly prodromal individuals); (2) did not score 2 (“unmet need”) on basic self-care and “psychological distress” items (relating to PEs) of Camberwell Assessment of Need Short Appraisal Schedule (CANSAS20); (3) no previous contact with mental health services/general practitioner (GP) regarding PEs (nor anyone on their behalf); (4) no previous contact with specialist mental health provision not available through general/family practitioner; (5) judged by research worker to not be in need-of-care for PEs. A specific exclusion criterion for controls was endorsement of any unusual experience item at screening; see1 and online supplement.
Measures
Appraisals of Anomalous Experiences Interview (AANEX2).
A semi-structured interview, eliciting current PEs, and associated emotional/cognitive correlates. Part one (AANEX-Inventory, short form21) comprises 17 anomalous experiences (including hearing voices, somatic experiences, experiences of reference, thought/mind permeability), rated on a 3-point scale (1 = not present; 2 = unclear; 3 = present; range 17–51) over lifetime, and currently (past month). Inter-rater reliabilities (IRR; N = 35; 16 clinical, 19 nonclinical) indicated almost perfect agreement (intra-class correlation coefficient (ICC) > .8): total (ICC = .995); current (ICC = .997); lifetime (ICC = .998). Experiences elicited by AANEX-Inventory anchored Part two (AANEX-CAR; context, appraisals and response), including belief flexibility items.
JTC Bias—The Beads Task.
JTC was assessed using a computerised (difficult; 60:40) version of the data-gathering beads task.6 Number of beads drawn prior to decision (maximum 20) was recorded. JTC has been operationalised as a decision made after ≤2beads.6 Decision conviction and accuracy were recorded.
Belief Flexibility.
Assessed using 2 standardized, widely used items6,11: (1) possibility of being mistaken22 and (2) alternative explanations.23 Both are scored yes/no indicating presence/absence of flexibility. For clinical and nonclinical groups the anchor was the main belief about the cause of PEs (ie, flexibility was assessed in the context of explanations of experiences rather than specific delusions, as in earlier studies). Illness/biological attributions were treated in an identical fashion to other explanations, that is, individuals were asked whether they might be mistaken/to generate alternative beliefs. Controls were presented with five beliefs in order to identify a comparable personally significant belief24 about a fundamental issue (God exists; There is an afterlife; The climate is changing due to human factors; Everything happens for a reason; There is a higher force at work in the world). They were asked to select the item that was “...most important to the way in which you think about the world- you can either agree or disagree with the statement you choose- the important thing is that the statement is one that matters personally to you.” If no item reached a 70% personal significance threshold, they were asked to generate their own belief (relating to the physical or metaphysical nature of the world or the functioning of society; purely value-based judgments/opinions were excluded given methodological issues identified in a previous study (Belief flexibility data were only available for 45 of the control group. This comprised 18 males (40.0%) and 27 females; mean age of 47.4 years (range 21–73); 40 (88.9%) self-identified as “white” background; 35 (77.9%) were in employment/education/training. There were no significant differences between those that provided belief flexibility data compared to those that did not on any key demographic or JTC reasoning variable.).24
Belief flexibility was also assessed in all groups in relation to a control belief: “the sun will rise tomorrow.”24,25 IRR for main belief items (n = 45; 16 clinical, 19 nonclinical, 10 control) demonstrated at least substantial agreement (ie, kappas >.6 following Landis and Koch26; “Possibility of being mistaken” = 0.77; “Alternative Explanations” = 0.86.)
Ratings of Experiential Vs Rational Reasoning Processes.
A novel method of rating dual-process reasoning was developed. Responses to belief flexibility and AANEX-CAR2 appraisal (“what sense do you make of your experiences?”) items were transcribed for analysis, since they elicited statements reflecting reasoning processes. Definitions of rational and experiential reasoning were developed using Epstein’s CEST framework,13,27 following Freeman et al.16 Definitions (see Appendix) were closely tied to recent integrative dual-process theories.28 Interviews were scored 0–2 (0 = no evidence of reasoning process; 1 = questionable/possible use; 2 = clear and spontaneous use). Ratings (clinical and nonclinical groups) were based on explanations of PEs. In the clinical group these included (in addition to de facto delusions), biological/biomedical explanations and spiritual explanations that showed clear overlap with the nonclinical group. The focus on the process of reasoning rather than belief content mitigates concerns over tautology in particular given that ratings could not be blind to belief content. IRR was conducted on 21 (20% of analysed sample) transcripts (6 clinical, 7 nonclinical, 8 control) with an independent blinded rater; agreement for rational (kappa = 0.67) and experiential (kappa = 0.71) reasoning fell into the “substantial agreement” (0.6–0.8) range.26
Wechsler Adult Intelligence Scale 3rd Edition—Short Form (WAIS-III29).
One subtest of each index was administered: information (verbal comprehension), block design (perceptual organization), arithmetic (working memory), and digit symbol (processing speed). Scores were prorated to estimate IQ.
Procedures
Ethical Approval.
NRES Committee London–Westminster (Ref: 12/LO/0766), South London & Maudsley/Institute of Psychiatry (SLAM/IoP) R&D Office (Ref: R&D2012/047), and BCUHB R&D Office (Reference: Jackson/LO/0766). Participants were screened over the phone or in person. Eligible participants completed all assessments, plus other measures and experimental tasks (not reported in this article), and given an honorarium.
Statistical Analysis
Data were analyzed using SPSS version 20. Normally distributed continuous variables were analyzed using t-tests and 1-way ANOVAs. Where deviations from a normal distribution could not be corrected by transforming, nonparametric testing was conducted. Group differences in JTC (beads drawn) were analyzed using Mann–Whitney (individual group comparisons) and Kruskall–Wallis (3-group comparisons) tests. χ2 tests were conducted on dichotomised variables: JTC extreme responding (decision after ≤2 beads), flexible versus nonflexible responses to belief flexibility items and, for experiential/rational ratings, “clear and spontaneous use of specific reasoning processes” (a maximum rating of 2) vs “no” or only “questionable evidence” (a rating of 0 or 1).
The view that ANCOVA (analysis of covariance, commonly employed in psychological research) or equivalent methods should be used to achieve the goal of “controlling for” real group differences has been condemned.30 We therefore report the group differences on our hypothesized variables without including as covariates in the analysis established risk factors for psychosis, on which the groups differ (such as IQ, ethnicity, and gender) or those inherent to need-for-care status (eg, impaired functioning, anxiety, depression, etc).
Results
Demographics and Clinical Data
The groups did not differ in age (table 1). In line with previous research, the nonclinical group was more likely to be female, and nonclinical and control groups were less likely to belong to black or minority ethnic groups, had higher IQ, and were more likely to be in education/employment/training. The nonclinical group had a younger age of onset of their PEs than the clinical group, with 77.2% reporting voices during their lifetime. Overall they were less symptomatic than the clinical group on the SAPS19 and SANS,31 although not significantly different on the AANEX,2 a measure designed to assess anomalous experiences across the psychosis continuum. The nonclinical group experienced hallucinations in all modalities as well as first-rank symptoms, but scored lower on global delusions (with minimal endorsement of paranoid or grandiose delusions). Ideas of reference were the most commonly rated delusion in the nonclinical group, but these were still less common than in the clinical group. The nonclinical group also reported fewer cognitive difficulties and negative symptoms (see1 for further information).
Table 1.
Demographic and Clinical Data by Group
| Clinical (n = 74) | Nonclinical (n = 92) | Controls (n = 83) | Significance tests | |
|---|---|---|---|---|
| London:Bangor | 35:39 | 51:41 | 43:40 | |
| Female (%) | 25 (33.8%) | 67 (72.8%) | 57 (68.7%) | χ2(2) = 30.1, P < .001 |
| Mean age (range) | 43 (20–78) | 46 (18–80) | 46 (21–76) | F(2,246) = 1.142, P = .321 |
| Ethnicity | χ2(2) = 11.2, P = .004 (white vs BME) | |||
| White | 71.6% | 87.0% | 90.4% | |
| Black | 21.6% | 6.5% | 3.6% | |
| Dual Heritage | 2.7% | 3.3% | 2.4% | |
| Asian | 2.7% | 2.2% | 2.4% | |
| Other | 1.4% | 1.1% | 1.2% | |
| In education/training/employment | 18.9% | 69.6% | 78.3% | χ2(2) = 65.2, P < .001 |
| Mean IQ (SD) | 89e (11.7) | 105b (14.0) | 112a (16.5) | F (2,225.5) = 54.2, P < .001 |
| Median psychiatric admissions (range) | 4d (0–20) | N/A | N/A | |
| On anti-psychotic medication | 89% | N/A | N/A | |
| Typical | 10% | |||
| Atypical | 55% | |||
| Clozapine | 24% | |||
| >1 antipsychotic | 16% | |||
| % maximum daily dose; median (range) | 50 (12–100)g | |||
| Mean age at start of psychotic experiences (SD) | 22 (10.8) | 15 (12.3) | N/A | t (164) = 3.8, P < .001 (C>NC) |
| Lifetime voices | 87.8% | 77.2% | N/A | χ2(1) = 3.150, P = .08 |
| SAPS total | 26.4 (15.4)a | 12.2 (7.2)a | N/A | *P < .001 |
| SAPS hallucinations global rating | 3.1 (1.9) | 2.4 (1.3) | N/A | *P = .001 |
| SAPS delusions global rating | 3.6 (1.2) | 2.3 (1.4) | N/A | *P < .001 |
| Frequency scoring ≥3 (global delusions) | 59/73 | 37/92 | N/A | |
| Frequency scoring ≥3 (persecutory delusion) | 29/73 | 1/92 | ||
| SAPS bizarre behaviour global | 0.8 (1.2) | 0.1 (0.4) | N/A | *P < .001 |
| SAPS thought disorder global rating | 0.9 (1.2) | 0.1 (0.3) | N/A | *P < .001 |
| SANS total | 20.2 (11.8)f | 3.0 (3.3)c | N/A | *P < .001 |
| SANS global ratings total (sum of 5 global ratings) | 8.5 (3.7) | 1.5 (1.7)a | N/A | *P < .001 |
| SAPS somatic/tactile hallucinations | 1.4 (1.8) | 2.1 (1.7) | N/A | P = .005 |
| SAPS delusions of reference | 2.7 (1.7) | 1.7 (1.7) | N/A | P < .001 |
| SAPS visual hallucinations | 1.2 (1.7) | 1.6 (1.7) | N/A | P = .094 |
| SAPS thought insertion | 1.8 (1.9) | 1.6 (1.7) | N/A | P = .551 |
| SAPS auditory hallucinations | 2.7 (2.2) | 1.4 (1.4) | N/A | P < .001 |
| SAPS mind reading | 1.7 (1.9) | 1.1 (1.4) | N/A | P = .047 |
| SAPS olfactory hallucinations | 0.5 (1.1) | 0.7 (1.2) | N/A | P = .096 |
| SAPS feelings of being controlled | 0.9 (1.7) | 0.5 (1.1) | N/A | P = .093 |
| SAPS voices commenting | 1.6 (2.1) | 0.3 (1.0) | N/A | P < .001 |
| SAPS thought broadcast | 1.5 (2.0) | 0.2 (0.6) | N/A | P < .001 |
| SAPS voices conversing | 1.1 (1.8) | 0.2 (0.6) | N/A | P < .001 |
| SAPS grandiose delusions | 0.7 (1.4) | 0.2 (0.7) | N/A | P = .007 |
| SAPS thought withdrawal | 0.7 (1.4) | 0.1 (0.5) | N/A | P < .001 |
| SAPS religious delusions | 0.7 (1.4) | 0.1 (0.4) | N/A | P < .001 |
| SAPS persecutory delusions | 1.9 (1.6) | 0.1 (0.4) | N/A | P < .001 |
| SAPS inappropriate affect | 0.3 (0.9) | 0.03 (0.3) | N/A | P = .006 |
| SAPS delusions of jealousy | 0.3 (0.7) | 0.01 (0.1) | N/A | P < .001 |
| SAPS delusions of sin/ guilt | 0.7 (1.3) | 0.01 (0.1) | N/A | P < .001 |
| SAPS somatic delusions | 0.3 (0.9) | 0.01 (0.1) | N/A | P = .001 |
| AANEX total current | 30.1 (6.2)b | 28.6 (5.1) | N/A | t (135.0) = 1.327, P = .19 |
| AANEX total lifetime | 36.6 (6.6)a | 34.8 (4.9) | N/A | t (130.3) = 1.935, P = .06 |
Superscript letters represent the number of missing participants as follows: a = 1, b =2, c=3, d = 5, e = 6, f = 7, and g = 10.
*Mann–Whitney tests (all SAPS and SANS scores).
Hypothesis 1: The clinical group will be more likely to show the JTC bias than nonclinical and control groups, who will not differ from each other.
As predicted the clinical group was significantly more likely to demonstrate JTC, both in terms of number of beads drawn and percentage showing extreme responding, compared to the other 2 groups, with small to medium effect sizes (table 2).
Table 2.
Number of Beads Drawn, Extreme JTC Responding, Conviction and Accuracy on the Beads Task in the 3 Groups
| Clinical (n = 74) | Nonclinical (n = 92) | Controls (n = 83) | Significance Test | Effect sizes/odds ratios (95% CIs) | |
|---|---|---|---|---|---|
| Mean number of beads drawn (SD); median (IQR) | 7.01 (6.06); 5 (1–11)a | 10.36 (6.60); 10 (5–15)b | 11.19 (6.09); 11 (8–16) | H(2) = 17.41, P < .001 | |
| C < NC; U = 2312.5, P = .002 | r = −.246 | ||||
| NC = CON; U = 3467, P = .345 | r = −.072 | ||||
| C< CON; U = 1844.0, P < .001 | r =−.325 | ||||
| Mean of conviction in final choice (SD); median (IQR) | 63.45 (27.21); 60 (50–80)a | 61.02 (25.67); 60 (50–80)a | 51.83 (27.27); 60 (40–70)b | H(2) = 6.175, P = .046 | |
| C = NC; U = 3003.50, P = .588 | r = .043 | ||||
| NC > CON; U = 3019.00, P = .049 | r = −.150 | ||||
| C > CON; U = 2297.50, P = .024 | r = −.183 | ||||
| N (%) extreme responders (≤2) | 26 (35.1%) | 17 (18.5%) | 9 (10.8%) | χ2(2) = 14.48, P = .001 | |
| C > NC; χ2(1) =5.928, P = .015 | OR = 2.390 (1.174, 4.864) | ||||
| NC = CON; χ2(1) = 2.011, P = .156 | OR = 1.864 (0.781, 4.446) | ||||
| C > CON; χ2(1) = 13.326, P < .001 | OR = 4.454 (1.922, 10.322) | ||||
| N (%) incorrect | 16a (22.5%) | 12a (13.5%) | 9b (10.8%) | χ2(2) = 4.38, P = .112 |
The effect size, r, is calculated following (Rosenthal, 1991) by the equation , where Z is the z-score and N is number of observations on which z is based. For r as an effect size .1 = small, .3 = medium, .5 = large.
aThree missing data points.
bOne missing data point.
Hypothesis 2: The nonclinical and the control groups will be more likely to demonstrate belief flexibility about their own beliefs and a control belief, than the clinical group.
The hypothesis was not supported, with no differences between the clinical and nonclinical groups on belief flexibility items on either the main or control belief (table 3). For the main belief, there was a trend (P = .057) toward the nonclinical group showing less flexibility on the “possibility of being mistaken” item compared to the control group.
Table 3.
Belief Flexibility Items for Main Belief and Control Belief
| Main belief | Clinical (n = 71) | Nonclinical (n = 92) | Controls (n = 401) | Significance Tests | Odds Ratio (95% CIs) |
|---|---|---|---|---|---|
| Personal significance (SD) | N/A | N/A | 85.63 (9.62) | H(2) = 4.015, P = .134 | |
| Mean of conviction (SD); Median (IQR) | 75.65a (25.14); 80 (60–99) | 82.76 (21.24); 90 (76–100) | 80.52 (19.55); 85 (70–99) | ||
| PM? | Overall: χ2(2) = 3.689, P = .158 | ||||
| No | 32 | 44 | 12 | C vs NC; χ2(1) = .186, P = .666 | 1.145 (0.617, 2.128) |
| Yes | 40 | 48 | 28 | CON vs NC; χ2(1) = 3.627, P = .057 | 2.139 (0.970, 4.714) |
| % Yes | 55.6 | 52.2 | 70.0 | CON vs C; χ2(1) = 2.249, P = .139 | 1.867 (0.822, 4.241) |
| AE? | Overall: χ2(2) = 3.033, P = .219 | ||||
| No | 35 | 38 | 13 | NC vs C; χ2(1) = 1.035, P = .309 | 1.382 (0.741, 2.577) |
| Yes | 36 | 54 | 27 | CON vs NC; χ2(1)=.912, P = .340 | 1.462 (0.669, 3.192) |
| % Yes | 50.7b | 58.7 | 67.5 | CON vs C; χ2(1) = 2.941, P = .086 | 2.019 (0.899, 4.534) |
| Control belief | Clinical (n = 73) | Nonclinical (n = 92) | Controls (n = 45) | ||
| Mean of conviction (SD); Median (IQR) | 89.04 (23.14); 100 (98.5–100) | 93.92 (16.16); 100 (99–100) | 97.15 (9.50); 100 (99–100) | H(2) = 0.268, P = .874 | |
| PM? | Overall: χ2(2) = 0.461, P = .794 | ||||
| No | 37 | 45 | 20 | C vs NC; χ2(1) = 0.025, P = .875 | 1.051 (0.567, 1.945) |
| Yes | 36 | 46 | 25 | CON vs NC; χ2(1) = 0.302, P = .582 | 1.223 (0.597, 2.506) |
| % Yes | 49.3 | 50.5b | 55.6 | CON vs C; χ2(1) = 0.434, P = .510 | 1.285 (0.609, 2.708) |
PM, “possibility of being mistaken”; AE, “alternative explanations.”
15/45 were excluded because no belief was rated above the 70% threshold.
aTwo missing data points.
bOne missing data point.
cThree missing data points.
Hypothesis 3: JTC will be associated with belief inflexibility (possibility of being mistaken) across the sample.
The hypothesis was not supported: people with JTC (extreme responding) were not more likely to show belief inflexibility on either main (χ2(1) = 0.585, P = .445; OR [95% CI] = 1.288 [0.673, 2.466]) or control (χ2(1) = 0.464, P = .496; OR [95% CI] = 1.249 [0.658, 2.372]) beliefs.
Hypothesis 4: The nonclinical group will score more highly than clinical group on rational reasoning.
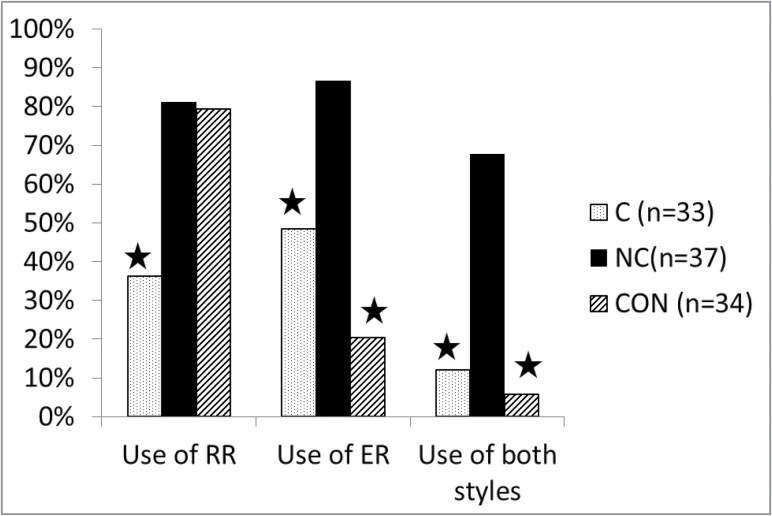
The nonclinical group was more likely than the clinical group to receive a maximum rating (“clear consistent evidence”) for rational reasoning, while the nonclinical and control group did not differ (table 4 and figure 1). The nonclinical group was more likely to show experiential reasoning than the clinical group, who in turn was more likely to employ it than the control group. Finally in terms of use of a combination of both styles of reasoning, the nonclinical group was more likely to show “clear consistent evidence” of a combination of both styles of reasoning than the other 2 groups.
Table 4.
Group Differences in Use of Rational Reasoning (RR), Experiential Reasoning (ER), and Both Styles of Reasoning
| C (n = 33) | NC (n = 37) | CON (n = 34) | Significance Tests | Effect Sizes/Odds Ratios (95% CIs) | |
|---|---|---|---|---|---|
| Use of RR? n (%) | 12/33 = 36.4% | 30/37 = 81.1% | 27/34 = 79.4% | χ2(2) = 19.484, P < .001 | |
| C vs NC; χ2(1) = 14.533, P < .001 | OR = 7.500 (2.531, 22.223) | ||||
| NC vs. CON; χ2(1) =.031, P = .860 | OR = 0.900 (0.279, 2.899) | ||||
| CON vs C; χ2(1) = 12.757, P < .001 | OR = 6.750 (2.263, 20.132) | ||||
| Use of ER? n (%) | 16/33 = 48.5% | 32/37 = 86.5% | 7/34 = 20.6% | χ2(2) = 31.256, P < .001 | |
| C vs NC; χ2(1) = 11.688, P = .001 | OR = 6.800 (2.124, 21.774) | ||||
| NC vs CON; χ2(1) =31.079, P < .001 | OR = 24.390 (7.042, 83.333) | ||||
| CON vs C; χ2(1) =.781, P = .016 | OR = 3.636 (1.238, 10.638) | ||||
| Use of ER and RR? n (%) | 4/33 = 12.1% | 25/37 = 67.6% | 2/34 = 5.9% | χ2(2) = 39.450, P < .001 | |
| C vs NC; χ2(1) =22.099, P < .001 | OR = 15.104 (4.320, 52.805) | ||||
| NC vs CON; χ2(1) =28.608, P < .001 | OR = 33.333 (6.849, 166.666) | ||||
| CON vs C; χ2(1) = 0.799, P = .371 | OR = 2.208 (0.376, 12.987) |
Fig. 1.
Percentage in each group showing clear evidence of rational reasoning (RR), experiential reasoning (ER) and both ER and RR (stars indicate differences at P ≤ .001 between adjacent groups). C, clinical; NC, nonclinical; CON, controls.
Additional Exploratory Analysis
Individuals showing clear evidence of rational reasoning were more likely to show higher belief flexibility on both the “possibility of being mistaken” (χ2(1) = 4.234, P = .040; OR [95% CI] = 2.375 [1.033, 5.459]) and “alternative explanations” items (χ2(1) = 6.936, P = .008; OR [95% CI] = 3.048 [1.311, 7.083]). This was expected given definitional overlap and use of belief flexibility items for ratings of rational reasoning. Individuals showing extreme JTC responding were less likely, at trend level, to use rational reasoning (χ2(1) = 3.339, P = .068; OR [95% CI] = 2.417 [0.924, 6.322]). Individuals showing clear evidence of experiential or “both rational and experiential” reasoning did not show significant differences on any of the other reasoning variables (see supplementary material).
For reference, additional analysis involving IQ and the key reasoning variables are presented in supplementary materials. Overall, IQ (when entered alongside group) significantly predicted JTC and some (but not all) of the other reasoning variables; correlation with beads drawn was low (r = .260, P < .01) indicating a small effect. Gender was not a significant predictor of any dependent variable and the addition of gender to regression models had no effect on the results.
Discussion
This study investigated whether the established reasoning biases of JTC and belief flexibility are associated with presence of PEs or with need-for-care status, by comparing individuals with persistent PEs, with and without need-for-care. It also applied, for the first time, a dual-process framework to investigate the process of explaining (reasoning about) PEs. Reasoning biases were found to differ in people with persistent PEs with and without need-for-care. The results suggest that an ability to invoke rational reasoning processes, together with an absence of limited data gathering (JTC), may protect against the development of need-for-care when persistent PEs are present, while marked use of experiential reasoning is associated with the presence of PEs.
The novel finding that JTC is not associated with the presence of full-blown PEs in the absence of a need-for-care, offers a new perspective on the causal role of this reasoning bias in the context of PEs. Consistent with the hypothesized role of reasoning biases in cognitive models of psychosis,32,33 we suggest that absence of JTC reduces the likelihood of developing maladaptive threat appraisals and the resultant characteristic paranoia observed in clinical populations.4,5 While the specificity of JTC to delusions remains subject to debate, a recent well-conducted meta-analysis has concluded that there is evidence for specificity of JTC to delusions.34 Since the unique nonclinical group in this study is characterized by persistent nondistressing PES in the absence of paranoia/distressing delusions, the absence of JTC is consistent with specificity to distressing delusions and not hallucinations.35,36
As also hypothesized, the clinical group was less likely than the other 2 groups to employ rational reasoning when explaining their PEs. Thus, those whose PEs were associated with a need-for-care, employed less “type 2,” reflective reasoning; this type of reasoning assists with generating alternative, less distressing, appraisals of these experiences. In contrast, the nonclinical group (with PEs but without need-for-care) did not differ from controls in rational reasoning, and was equally likely to be reflective; consistent with the association between rational reasoning and reduced paranoia in the general population, suggesting an adaptive role for such reasoning.16 However, the nonclinical group did also show higher levels of experiential, “gut” reasoning: over 60% showed clear evidence of both reasoning processes. Consistent with these findings, Daalman and colleagues37 found that healthy voice-hearers showed high levels of “emotional reasoning” (a bias showing clear overlap with experiential reasoning) and Wolfradt and colleagues14 reported that a preference for both intuitive (“type 1”) and rational (“type 2”) thinking styles leads to stronger paranormal beliefs.
Belief flexibility findings were less clear-cut. While there was some evidence of the nonclinical group being less likely to accept the possibility of being mistaken than controls, there were no differences between the clinical and nonclinical group on any item. The rates of flexibility reported on the “possibility of being mistaken” item are comparable with previous studies6,11; however the focus on explanations of experiences rather than delusional beliefs per se, may account for the higher than expected flexibility in the clinical group on the “alternative explanation” item compared to earlier studies.11,23 The only previous study comparing delusions with personally significant beliefs24 reported no differences in flexibility on the main belief between deluded, remitted, and control groups (consistent with current findings), but found evidence of greater flexibility in controls on the control/standard belief. The current study may be considered an improvement in terms of larger sample size and more stringent criteria for selection of comparison belief for controls.
The dual-process ratings, developed for this study, offer a novel way of assessing “online” reasoning in an ecologically valid manner. Rational reasoning was associated with belief flexibility and, at trend level, with absence of JTC, providing some evidence of convergent validity. However, the apparent disparity between explicit belief flexibility responses and the use of rational reasoning in the nonclinical group (evidenced by the dual-process ratings) suggests that while responses to standard belief flexibility questions can predict positive engagement with psychological therapy,11,38,39 these items may be less successful in elucidating subtle real-world reasoning processes.
The study findings need to be interpreted in the context of certain methodological limitations. The cross-sectional nature of the study means the possibility cannot be excluded that associations, for example, between JTC and need-for-care, may be epiphenomenal to, or a consequence of, need-for-care, or relate only to specific aspects (eg, presence of delusions or other variables, such as IQ, on which the groups differ). The current study did not set out to examine the role of neurocognition in need-for-care status and its contribution to these reasoning biases. In future, using a comprehensive battery, we would recommend further examination of the relationship between IQ, neurocognitive deficits, and belief flexibility (and dual-process reasoning), as has been done previously with the JTC bias.40 The novel dual-process findings should also be considered preliminary since ratings were conducted on only a subset of the overall sample and they require replication in a larger, fully-blinded sample. Future work should take into account the possibility that clinical groups may engage in less reasoning overall (regardless of type) when compared to other groups41 although this issue was mitigated in the current study by ratings being conducted in terms of presence of one clear example of experiential or rational reasoning rather than frequency of use. The fact that some differences on belief flexibility did not reach statistical significance may be attributable to reduced power given the relatively small sample size for these analyses specifically.
In summary, this study has found that reasoning biases differ in groups with PEs with and without need-for-care. People with persistent PEs but without need-for-care did not JTC and made more use of rational reasoning than those with need-for-care. Therefore, absence of JTC and an ability to invoke rational reasoning represent plausible protective factors within this unique group. In contrast, a high use of experiential reasoning, common to both PE groups, may play a role in the occurrence of both benign and clinically distressing PEs. It is notable that dual-process models of reasoning are starting to inform a new generation of targeted reasoning interventions, focused on constructs such as “fast” and “slow” thinking, with promising results.39,42–45 The dynamic nature of real-world reasoning is likely to involve a complex interplay of processes competing and combining to produce observed behavior.28 Gaining a more nuanced understanding of how individuals with PEs, with and without a need-for-care, reason about their experiences will assist in refining future developments in clinical interventions for distressing psychosis.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Funding
This study was supported by Medical Research Council (Reference: G1100568).
Supplementary Material
Acknowledgments
T.W. acknowledges support by National Institute for Health Research (NIHR) collaboration for Leadership in Applied Health Research and Care South London at King’s College Hospital NHS Foundation Trust. The views expressed are the author(s) and not necessarily the NHS, NIHR or Department of Health. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Appendix 1: Definitions of Reasoning Processes
Experiential reasoning scoring
Type 1 process: fast, high capacity, independent of working memory and cognitive ability
Reasoning processes to be rated as experiential in cases of:
(Main criteria)—Reasoning clearly tied to affect (feeling, hunches, gut-feelings, vibes, etc) that is, reasoning on basis of internal subjective states.
-
Where there is evidence of judgements being made in a rapid, nondeliberative manner
For example, “flashes of understanding/ insight,” “sudden revelations,” “sudden shifts in understanding.”
-
Where the person expresses the view that their way of understanding cannot easily be reduced into words/logic.
Where the individual states something akin to “I just know”
Where the individual states something akin to “I don’t know if I can describe what I mean”
Where an individual states limitations to rationality, logic (“some things science can’t understand,” etc).
Rational reasoning processes
Type 2 process: slow, low capacity, heavily dependent on working memory and related to individual differences in cognitive ability].
Reasoning processes to be rated as rational reasoning on the basis of:
-
Evidence of slower, deliberative processing
describing a process of reflection/analyzing over a period of time
For example, “I have thought long and hard about this”
-
Where the person acknowledges applying a logical, rational approach to developing their understanding.
Examples such as “I thought about this, considered other possibilities, checked “x” out, asked others,” etc.
Where the person draws on evidence collected from or (or at least available to) other people, that is, third-person proof/evidence.
-
Where the person acknowledges how they were (at any stage) “not certain/ in doubt” about belief.
For example, “I wasn’t sure, it was hard to work out what was going on at the start,” “I’m still not sure.”
-
Specific use of any of the following
Hypothetical reasoning (“if . . . then”)—consistent with a logical reasoning process.
Spontaneous use of “cognitive simulation,” that is, the person showing an ability to “decouple” from their own understanding to acknowledge other ways of understanding the same experiences.
Explicit use of probability estimates on the basis that this stands opposed to the idea of “just knowing.”
References
- 1. Peters E, Ward T, Jackson M, et al. Clinical, socio-demographic and psychological characteristics in individuals with persistent psychotic experiences with and without a “need for care”. World Psychiatry. 2016;15:41–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brett CMC, Peters EP, Johns LC, Tabraham P, Valmaggia LR, McGuire P. Appraisals of Anomalous Experiences Interview (AANEX): a multidimensional measure of psychological responses to anomalies associated with psychosis. Br J Psychiatry Suppl. 2007;191:S23–S30. [DOI] [PubMed] [Google Scholar]
- 3. Heriot-Maitland C, Knight M, Peters E. A qualitative comparison of psychotic-like phenomena in clinical and non-clinical populations. Br J Clin Psychol. 2012;51:37–53. [DOI] [PubMed] [Google Scholar]
- 4. Ward TA, Gaynor KJ, Hunter MD, Woodruff PW, Garety PA, Peters ER. Appraisals and responses to experimental symptom analogues in clinical and nonclinical individuals with psychotic experiences. Schizophr Bull. 2014;40:845–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Underwood R, Kumari V, Peters E. Cognitive and neural models of threat appraisal in psychosis: a theoretical integration. Psychiatry Res. 2016;239:131–138. [DOI] [PubMed] [Google Scholar]
- 6. Garety PA, Freeman D, Jolley S, et al. Reasoning, emotions, and delusional conviction in psychosis. J Abnorm Psychol. 2005;114:373–384. [DOI] [PubMed] [Google Scholar]
- 7. Garety PA, Freeman D. The past and future of delusions research: from the inexplicable to the treatable. Br J Psychiatry. 2013;203:327–333. [DOI] [PubMed] [Google Scholar]
- 8. Dudley R, Daley K, Nicholson M, et al. ‘Jumping to conclusions’ in first-episode psychosis: a longitudinal study. Br J Clin Psychol. 2013;52:380–393. [DOI] [PubMed] [Google Scholar]
- 9. Moritz S, Woodward TS. A generalized bias against disconfirmatory evidence in schizophrenia. Psychiat Res. 2006;142:157–165. [DOI] [PubMed] [Google Scholar]
- 10. Woodward TS, Moritz S, Cuttler C, Whitman JC. The contribution of a cognitive bias against disconfirmatory evidence (BADE) to delusions in schizophrenia. J Clin Exp Neuropsychol. 2006;28:605–617. [DOI] [PubMed] [Google Scholar]
- 11. So SH, Freeman D, Dunn G, et al. Jumping to conclusions, a lack of belief flexibility and delusional conviction in psychosis: a longitudinal investigation of the structure, frequency, and relatedness of reasoning biases. J Abnorm Psychol. 2012;121:129–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kahneman D. Thinking, Fast and Slow. New York, NY: Farrar, Straus and Girouz; 2011. [Google Scholar]
- 13. Epstein S, Pacini R, Denes-Raj V, Heier H. Individual differences in intuitive-experiential and analytical-rational thinking styles. J Pers Soc Psychol. 1996;71:390–405. [DOI] [PubMed] [Google Scholar]
- 14. Wolfradt U, Oubaid V, Straube ER, Bischoff N, Mischo J. Thinking styles, schizotypal traits and anomalous experiences. Pers Indiv Differ. 1999;27:821–830. [Google Scholar]
- 15. Lindeman M, Aarnio K. Superstitious, magical, and paranormal beliefs: An integrative model. J Res Pers. 2007;41:731–744. [Google Scholar]
- 16. Freeman D, Evans N, Lister R. Gut feelings, deliberative thought, and paranoid ideation: a study of experiential and rational reasoning. Psychiatry Res. 2012;197:119–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Colbert SM, Peters ER. Need for closure and jumping-to-conclusions in delusion-prone individuals. J Nerv Ment Dis. 2002;190:27–31. [DOI] [PubMed] [Google Scholar]
- 18. Lim MH, Gleeson JF, Jackson HJ. The jumping-to-conclusions bias in new religious movements. J Nerv Ment Dis. 2012;200:868–875. [DOI] [PubMed] [Google Scholar]
- 19. Andreasen N. Scale for the Assessment of Positive symptoms (SAPS). Iowa City IA: University of Iowa; 1984. [Google Scholar]
- 20. Slade M, Loftus L, Phelan M, Thornicroft G, Wykes T. The Camberwell Assessment of Need. London: Gaskell; 1999. [Google Scholar]
- 21. Lovatt A, Mason O, Brett C, Peters E. Psychotic-like experiences, appraisals, and trauma. J Nerv Ment Dis. 2010;198:813–819. [DOI] [PubMed] [Google Scholar]
- 22. Wessely S, Buchanan A, Reed A, et al. Acting on delusions. 1: Prevalence. Br J Psychiatry. 1993;163:69–76. [DOI] [PubMed] [Google Scholar]
- 23. Freeman D, Garety PA, Fowler D, Kuipers E, Bebbington PE, Dunn G. Why do people with delusions fail to choose more realistic explanations for their experiences? An empirical investigation. J Consult Clin Psychol. 2004;72:671–680. [DOI] [PubMed] [Google Scholar]
- 24. Colbert SM, Peters ER, Garety PA. Delusions and belief flexibility in psychosis. Psychol Psychother. 2010;83:45–57. [DOI] [PubMed] [Google Scholar]
- 25. Garety P. Delusions—problems in definition and measurement. Br J Med Psychol. 1985;58:25–34. [DOI] [PubMed] [Google Scholar]
- 26. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 27. Epstein S. Integration of the cognitive and the psychodynamic unconscious. Am Psychol. 1994;49:709–724. [DOI] [PubMed] [Google Scholar]
- 28. Evans JS, Stanovich KE. Dual-process theories of higher cognition: advancing the debate. Perspect Psychol Sci. 2013;8:223–241. [DOI] [PubMed] [Google Scholar]
- 29. Wechsler D. Wechsler Adult Intelligence Scale—Third Edition. San Antonio, TX: The Psychological Corporation; 1997. [Google Scholar]
- 30. Miller GA, Chapman JP. Misunderstanding analysis of covariance. J Abnorm Psychol. 2001;110:40–48. [DOI] [PubMed] [Google Scholar]
- 31. Andreasen N. Scale for the Assessment of Negative Symptoms (SANS). Iowa City, IA: University of Iowa; 1984. [Google Scholar]
- 32. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 33. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. [DOI] [PubMed] [Google Scholar]
- 34. Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the “jumping to conclusions” reasoning bias: a systematic review and meta-analysis Schizophrenia Bull. 2016;42:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bristow E, Tabraham P, Smedley N, Ward T, Peters E. Jumping to perceptions and to conclusions: specificity to hallucinations and delusions. Schizophr Res. 2014;154:68–72. [DOI] [PubMed] [Google Scholar]
- 36. Lincoln TM, Ziegler M, Mehl S, Rief W. The jumping to conclusions bias in delusions: specificity and changeability. J Abnorm Psychol. 2010;119:40–49. [DOI] [PubMed] [Google Scholar]
- 37.Daalman K, Sommer IEC, Derks EM, Peters ER. Cognitive biases and auditory verbal hallucinations in healthy and clinical individuals. Psychol Med. 2013;43:2339–2347. [DOI] [PubMed] [Google Scholar]
- 38. Garety P, Fowler D, Kuipers E, et al. London East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis. 2. Predictors of outcome. Br J Psychiatry. 1997;171:420–426. [DOI] [PubMed] [Google Scholar]
- 39. Waller H, Freeman D, Jolley S, Dunn G, Garety P. Targeting reasoning biases in delusions: a pilot study of the Maudsley Review Training Programme for individuals with persistent, high conviction delusions. J Behav Ther Exp Psychiatry. 2011;42:414–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Garety P, Joyce E, Jolley S, et al. Neuropsychological functioning and jumping to conclusions in delusions. Schizophr Res. 2013;150:570–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Freeman D, Lister R, Evans N. The use of intuitive and analytic reasoning styles by patients with persecutory delusions. J Behav Ther Exp Psychiatry. 2014;45:454–458. [DOI] [PubMed] [Google Scholar]
- 42. Garety P, Waller H, Emsley R, et al. Cognitive mechanisms of change in delusions: an experimental investigation targeting reasoning to effect change in paranoia. Schizophr Bull. 2015;41:400–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Waller H, Emsley R, Freeman D, et al. Thinking well: a randomised controlled feasibility study of a new CBT therapy targeting reasoning biases in people with distressing persecutory delusional beliefs. J Behav Ther Exp Psychiatry. 2015;48:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Moritz S, Veckenstedt R, Bohn F, et al. Complementary group Metacognitive Training (MCT) reduces delusional ideation in schizophrenia. Schizophr Res. 2013;151:61–69. [DOI] [PubMed] [Google Scholar]
- 45. Moritz S, Andreou C, Schneider BC, et al. Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin Psychol Rev. 2014;34:358–366. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.