Supplemental digital content is available in the text.
Key Words: Transition to residency, Medical student education, Clinical skills, Assessment, Standardized nurse, Standardized patient, OSCE, Clinical reasoning
Abstract
Introduction
“Transitions to residency” programs are designed to maximize quality and safety of patient care, as medical students become residents. However, best instructional or readiness assessment practices are not yet established. We sought to study the impact of a screen-based interactive curriculum designed to prepare interns to address common clinical coverage issues (WISE OnCall) on the clinical skills demonstrated in simulation and hypothesize that performance would improve after completing the module.
Methods
Senior medical students were recruited to participate in this single group prestudy/poststudy. Students responded to a call from a standardized nurse (SN) and assessed a standardized patient (SP) with low urine output, interacted with a 45-minute WISE OnCall module on the assessment and management of oliguria, and then evaluated a different SP with low urine output of a different underlying cause. Standardized patients assessed clinical skills with a 37-item, behaviorally anchored checklist measuring clinical skills (intraclass correlation coefficient [ICC], 0.55–0.81). Standardized nurses rated care quality and safety and collaboration and interprofessional communication using a 33-item literature-based, anchored checklist (ICC, 0.47–0.52). Standardized patient and SN ratings of the same student performance were correlated (r, 0.37–0.62; P < 0.01). Physicians assessed clinical reasoning quality based on the students’ patient encounter note (ICC, 0.55–0.68), ratings that did not correlate with SP and SN ratings. We compared pre-post clinical skills performance and clinical reasoning. Fifty-two medical students (31%) completed this institutional review board –approved study.
Results
Performance as measured by the SPs, SNs, and the postencounter note all showed improvement with mostly moderate to large effect sizes (range of Cohen’s d, 0.30–1.88; P < 0.05) after completion of the online module. Unexpectedly, professionalism as rated by the SP was poorer after the module (Cohen’s d, −0.93; P = 0.000).
Discussion
A brief computer-based educational intervention significantly improved graduating medical students' clinical skills needed to be ready for residency.
Within weeks of graduating from medical school, newly minted graduates in all specialties must be ready to perform as interns. This transition can be challenging and daunting. A task force of the American College of Surgeons surveyed 12% of US interns in surgery programs in 2009 and found that they feel “only moderately prepared to perform most of the common intern level responsibilities in the domains of medical knowledge and patient care.”1 In the same study, “clinical management of (predictable) postoperative conditions” seemed to be a source of anxiety during intern year. Program directors and hospital leadership are equally concerned and have invested heavily in orientation programs and increased supervision to mitigate the “July effect”—in which patient care quality and safety are endangered as new trainees acclimate to their new roles.2,3 July of internship may be particularly challenging for graduates who do not have rigorous clinical rotations scheduled throughout their final year of medical school and focus instead on nonclinical activities. Regaining forgotten or eroded knowledge, skills, and attitudes, which had been previously acquired, has been the focus of “intern orientation.”
Recently, medical school programs have attempted to better prepare their students by implementing transitions to residency programs or boot camps.4–6 These programs are typically 1 week to 1 month in duration; focus on skills, attitudes, and formative assessment; and are usually face-to-face and resource intensive. Generally, they do not include baseline or summative assessments of their trainees' readiness such as performance-based assessment with documented feedback to the candidate or an educational handoff to future program directors. Barriers to conducting performance assessments at the end of medical school include lack of measures as well as costly resources such as simulation center space and time and faculty availability. Despite these efforts, leaders in the academic and hospital-based community are asking: are medical school graduates as ready as possible for residency?
In the interest of patient safety and quality of care, policy makers have advocated for new national standards to assure that residents are prepared to manage critical situations. The Accreditation Council for Graduate Medical Education guidelines, for example, stipulate that direct supervision is required for interns managing common conditions (eg, low urine output, hypertension, change in neurologic status, etc) until competence is demonstrated and documented by the program director.7 The Association of American Medical Colleges similarly stipulated a set of common standards through their document, the core Entrustable Professional Activities for Entering Residency.8 In truth, little is known about the capacity of graduating medical students,2 to function safely in residency. It is important to understand this gap quantitatively and qualitatively to inform transition to residency programs going forward.
For this study, we designed a program to assess and address readiness for residency of graduating medical students and focused on a single clinical coverage issue. We defined readiness for residency as demonstration of the following clinical skills—responding to a page while on call, assessing a patient complaint, and documenting the encounter—based on sound clinical reasoning, as reflected by the content of the medical record. We addressed readiness for residency using WISE OnCall.
WISE OnCall
We developed “WISE OnCall,” a series of instructional case-based multimedia modules designed to address readiness for internship. The theoretical framework for WISE OnCall is cognitive apprenticeship,9,10 an instructional model in which an expert guides an “apprentice” to be able to experience common medical/surgical “coverage” situations, through modeling, coaching, scaffolding, and ultimately fading of instructional guidance. This design of the modules is based on our experience building and researching the use of WISE MD for clinical clerkship education.11–16 To date, 8 WISE OnCall modules have been completed with plans to build at least 5 more in the next 2 years (https://www.wisemed.org/wise-oncall/). Each module provides a sequential approach to a common clinical issue. First, there is an overview of the problem including underlying diagnostic and management approaches. This is followed by a video simulation illustrating the assessment of a clinical situation emphasizing collection of information from the medical record, the nursing staff, the patient, and medical tests. The case reinforces the importance of effective interprofessional communication and professionalism. The final section includes 3 practice cases that enable the learner to interact by applying diagnostic skills and obtaining feedback. This digital strategy is designed to help transitioning medical students or novice residents develop more advanced diagnostic schemas or cognitive illness scripts, which then become the basis of the development of their clinical reasoning.13
For this study, we chose the oliguria (low urine output) module because it is a topic that all students are likely to have basic familiarity with by the end of medical school and it is a condition interns in medical and surgical disciplines can expect to encounter during a typical night on hospital call. The objectives for the module are listed in Figure 1. We hypothesized that on average, the clinical skills required to safely care for a patient with low urine output would be demonstrably strengthened through interacting with WISE OnCall.
FIGURE 1.
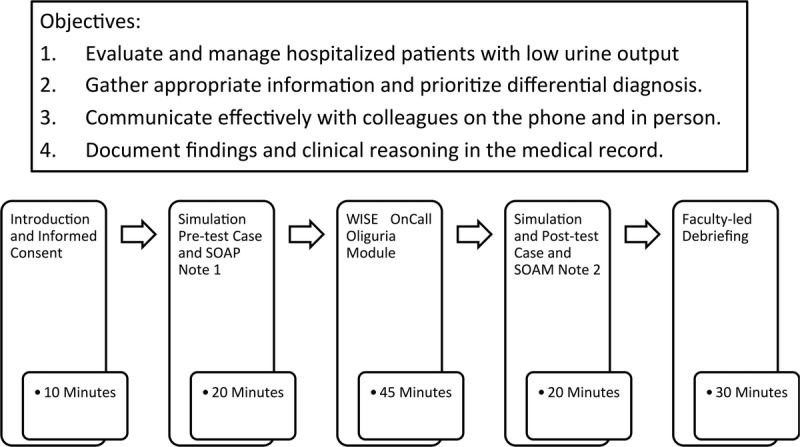
Objectives, sequence, and timeline of the readiness for internship experience.
METHODS
Subjects and Setting
All senior-year medical students (n = 164) at our medical school in the North Eastern United States received an e-mail toward the second half of the academic year from the principal investigators inviting them to participate in a 3-hour “readiness for internship” event held in our simulation center. Our students have extensive experience with performance-based assessment involving standardized patients (SPs) and are also accustomed to the assessment framework used in this study. There are 18 formative and summative required interactions spread throughout the 4-year curriculum. In the letter, we explained that 1 purpose of this event was to study the effectiveness of WISE OnCall—a series of Web-based modules designed to prepare them to care for patients with common clinical coverage issues—and that they would also be able to debrief their experience with a clinical faculty member. Fifty-two senior medical students out of a class of 164 (31%) volunteered to participate, and all completed the study protocol. They received 100 US dollars for completing all study materials. No academic credit was given for participation in this activity, and it was not required for graduation. The institutional review board at our medical school reviewed and approved this study after a full protocol review. We choose not to collect any demographic information to ensure the confidentiality of our students, some of whom would remain at our institution for residency training.
Standardized Patient/Nurse Scenarios
We assessed ability to evaluate and manage oliguria in the acute care setting before and after they completed the WISE OnCall module using the SP/standardized nurse (SN) simulation cases. We developed 2 interprofessional simulated scenarios, both involving an SP and an SN. In both cases, the intern was asked to evaluate an otherwise clinically stable, hospitalized patient with low urine output. The cases were designed to be of equivalent difficulty for senior medical students who were familiar with the differential diagnosis of new onset oliguria. Accompanying instruments were developed to assess students' clinical reasoning and clinical skills after standard case design methodology.17
Procedures
Figure 1 illustrates the sequence of activities and timing for the readiness of internship experience. After a brief orientation and informed consent discussion, participants entered a simulated encounter in which they participated as the covering intern on a surgical service. The scenario began with a page from an SN calling them to assess a postoperative patient with oliguria (simulation pretest/case no. 1).
Upon entering the examination room, the students were expected to engage with both an SP and the SN to assess the clinical situation and to make a plan for management and follow-up. The students were told that they could request laboratory results, electrocardiograms, and imaging results and order and receive the results from simple bedside procedures (eg, Foley catheter insertion, bladder scan with ultrasound, intravenous fluid administration) from the SN.
After the 15-minute encounter, the participants exited the room and were given 5 minutes to type a “coverage” note summarizing their findings (subjective and objective), clinical reasoning (assessment), and plan in the common subjective, objective, assessment, plan (SOAP) format into a word processing program on a computer.
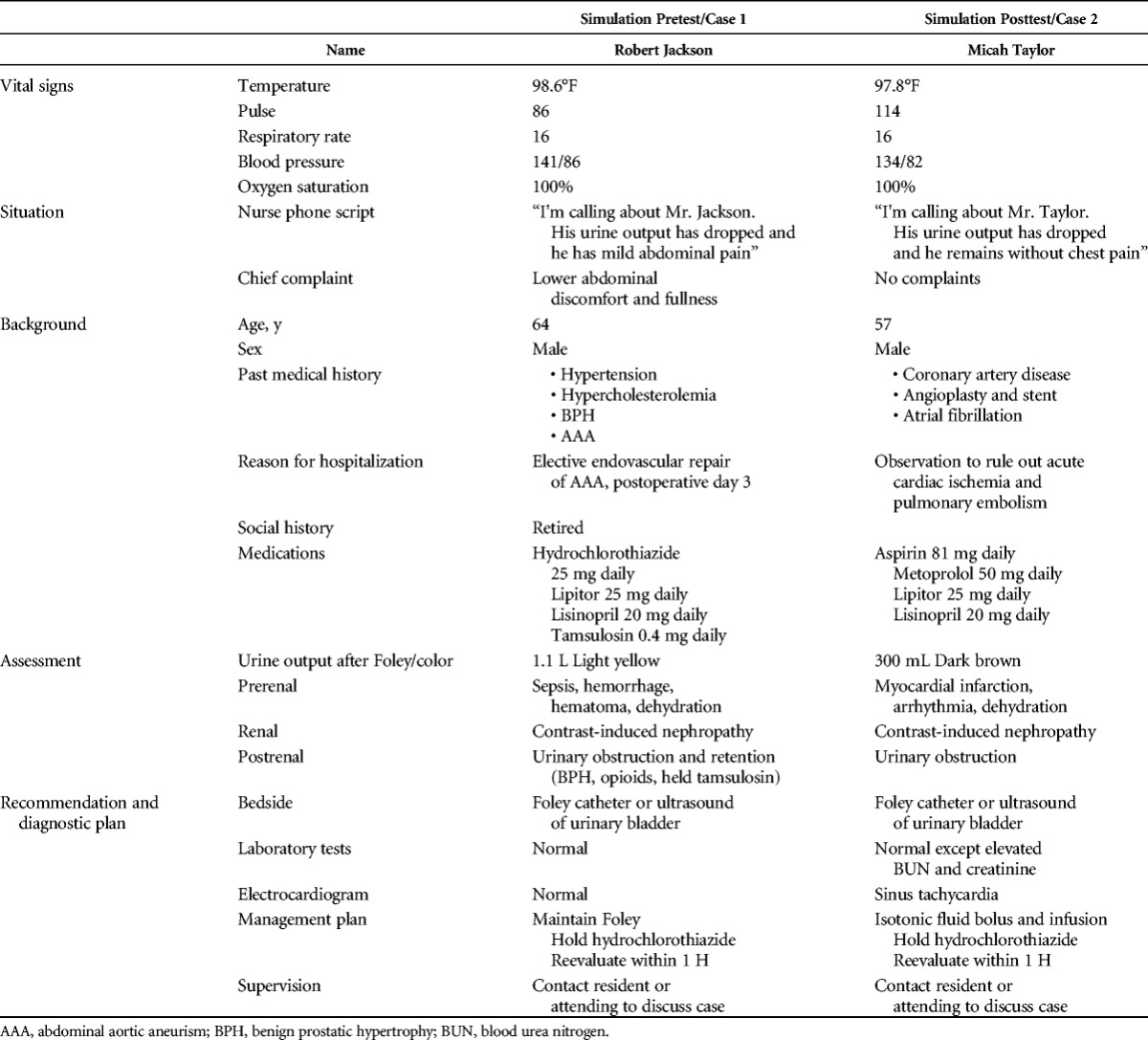
The primary intervention is the WISE OnCall oliguria module. Participants were given 45 minutes to view the module in a private space with a proctor. After viewing the module, participants had a second simulation encounter (simulation posttest/case no. 2). The encounter lasted 15 minutes, and they had 5 minutes to complete the associated SOAP note. To maintain realism and decrease rater bias, a different SP and SN pair was used for the second case. The characteristics of the case and level of difficulty were similar, but the root cause of oliguria was different (Table 1).
TABLE 1.
Simulation Case Descriptors
Finally, students participated in a 30-minute debriefing session with a member of the clinical faculty where all aspects of the exercise were discussed. The main purpose of this debriefing was to answer students' questions. To protect the privacy of students who may have been matched for residency within our institution, the faculty member did not view the student's actual performance. Therefore, the debriefing addressed only student self-reported concerns about their performance.
Simulation Cases and Clinical Skills Assessment
Experienced SPs were recruited and underwent 3 hours of case portrayal and rater training to prepare them to reliably assess clinical skills performance using a 37-item behaviorally anchored checklist measuring communication skills in 3 subdomains-data gathering (6 items), rapport building (6 items), patient education (3 items), history gathering (10 items), and physical examination skills (9 items) (interrater intraclass correlation coefficient [ICC], 0.55–0.81) previously validated for use as a measure of core clinical skills.17 Experienced SPs were recruited to participate as SNs and were trained by an experienced nurse educator (G.N.) to portray a nurse in the simulation and to rate the student's competence. The SN used a 33-item literature-based, behaviorally anchored checklist to rate the student's performance.18 The checklist was modified from an instrument developed for OSCE-based assessment of interprofessional communication including aspects of care quality and safety, collaboration and teamwork, role clarity, and relationship development tailored to the specific clinical case requirements.19 After the behaviorally anchored items, at the end of the SP and SN checklists, raters completed 2 global items each on a 4-point scale. They were asked separately if they would recommend this student based on medical competence (not recommend, recommend with reservations, recommend, or highly recommend), and then they were asked to rate the student's professionalism (not at all, somewhat, professional, and highly professional). Although both SP and SN were in the same room viewing the same student performance, they completed their checklists independently without conferring with each other. A 10% random sample of interactions was reviewed and rerated on videotape by a member of the study team (G.N.) (ICC, 0.47–0.52). Standardized patient and SN checklists for both cases are included as supplemental materials (see PDF, Supplementary Digital Content #1, http://links.lww.com/SIH/A340; SP Checklist Oliguria Case 1), (see PDF, Supplementary Digital Content #2, http://links.lww.com/SIH/A341; SP Checklist Oliguria Case 2), (see PDF, Supplementary Digital Content #3, http://links.lww.com/SIH/A342; SN Checklist Case 1), (see PDF, Supplementary Digital Content #4, http://links.lww.com/SIH/A343; SN Checklist Case 2).
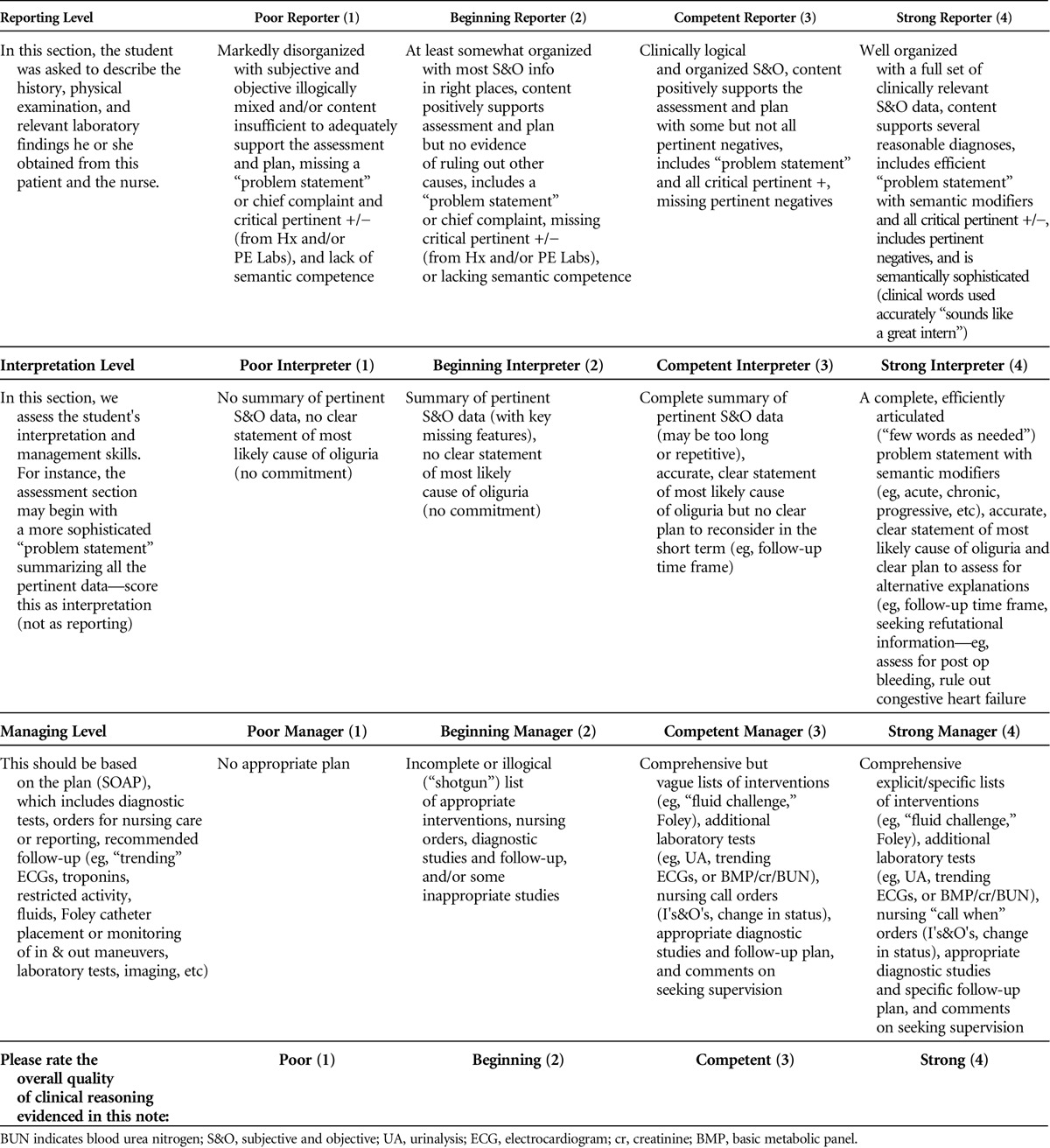
Clinical Reasoning Assessment
Clinical reasoning was assessed based on the SOAP note and scored by 2 experienced clinicians (K.U., D.S.) using a rubric that we developed based on Pangaro's Reporter-Interpreter-Manager-Educator framework.20 We selected this framework because it is how we teach students clinical reasoning and patient note writing and is reinforced in the WISE OnCall Module (Table 2). Each student's notes were scored on 4 characteristics—reporter, interpreter, manager, and overall clinical reasoning—each on a 4-point scale using a rubric with detailed case specific anchors. Twenty percent of the SOAP notes were rated independently by both raters (ICC, 0.55–0.68).
TABLE 2.
Scoring Rubric for Assessing Oliguria SOAP Note
Data Analysis
Standardized patients and SNs rated students on 3-level behaviorally anchored (not done, partially done, well done) checklist items. For analysis, we reduce item scores to a dichotomous variable (not done/partially done, well done) and summarize these for each subdomain as percent well done (%WD). This is the SP checklist data analysis and reporting strategy we have developed over 15 years for both educational and research purposes because we obtain the highest inter- and intrarater reliability, have established consistently high checklist internal validity (Cronbach α for subdomains range, 0.79–0.90), pass/fail cutoffs (which are determined based on multiple factors), and hover around 2 SDs below the mean, which is typically between 55% and 60%. We find this approach to be most transparent and educationally meaningful to students and educators. This is because it reflects the percentage of items in each subdomain the individual student did well, standardizing the scores across subdomains with uneven number of items. When we are working individually with a student to understand the subtleties of his or her performance, we use the data from the “partially done” category.
Clinical reasoning was summarized as mean scores on the 4 Reporter-Interpreter-Manager-Educator characteristics on a 1 to 4 scale and SD. We examine whether WISE OnCall improves the participants' clinical performance and reasoning using paired samples t tests. A priori α level was set as 0.05 for all estimations and β = 0.20. The magnitude of the effect of the module on clinical skills is measured by Cohen's d, which is the difference between the means divided by the pooled SD. Cohen's d is a unit-less ratio allowing comparison of intervention effects across domains measured in different ways and across studies. It is interpreted qualitatively. In general, an effect size of 0.2 to 0.3 is interpreted as a “small” effect, around 0.5 a “medium” effect, and 0.8 to infinity a “large” effect.21,22 Interrater agreement on each measure was calculated as an ICC for pairs of raters within domains.
To assess the concurrent validity of our measures in this small sample, we hypothesized that observers of the same performance would correlate, and, based on our experience measuring clinical skills in this manner, the clinical reasoning as reflected in writing the patient note would not correlate with observed skills performance. We generated a correlation matrix among the comparable domains on the SP (communication skills, recommendation-medical competence, recommendation-professionalism) and SN checklists (interprofessional communication, recommendation-medical competence, recommendation-professionalism), and the faculty member assessed overall clinical reasoning based on the patient notes by each SP/SN case. Because some of the variables are ordinal, we conducted both Pearson and Spearman correlation coefficients, which yielded nearly the same results. We report Pearson r for ease of interpretation.
RESULTS
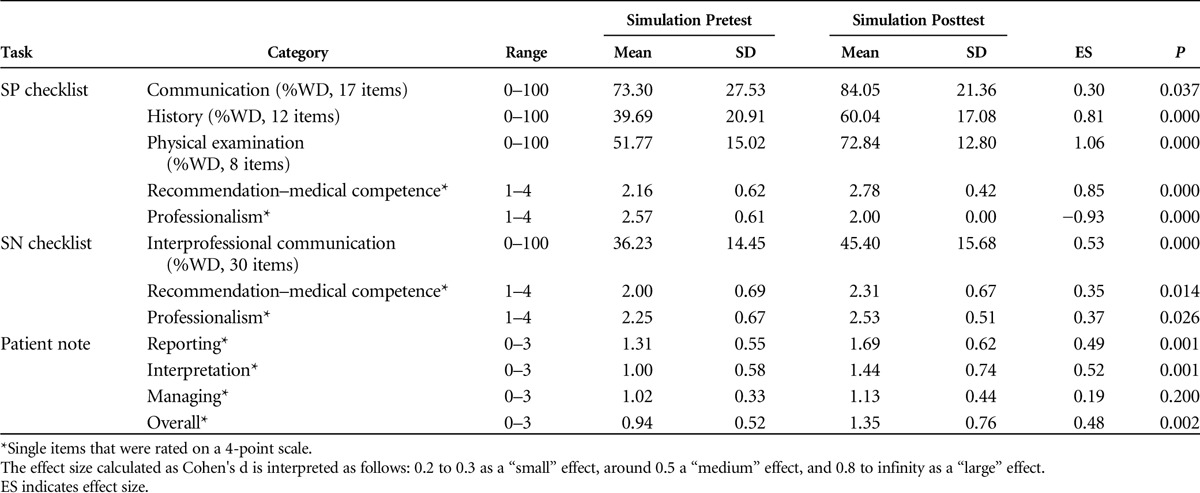
Group Performance and Clinical Reasoning at Baseline and After WISE OnCall
Table 3 shows the potential range, mean scores, and SDs on the categories of simulation pretest and posttest. As hypothesized, all categories measured improved a moderate to large amount after viewing the module, except for professionalism as rated by the SP, which declined, and the “managing” item based on the patient note, which remained the same from the pre- to postsimulation. Comparable SP and SN ratings within the same case were correlated (case no. 1: all 9, r = 0.50 [P < 0.001]; case no. 2: range for 9, r = 0.37–0.62 [P < 01]), and none of the SP and SN ratings correlated with the overall clinical reasoning.
TABLE 3.
Clinical Skills and Clinical Reasoning Performance Before and After WISE OnCall Module
DISCUSSION
WISE OnCall significantly improved the ability to perform key clinical skills expected of a covering intern. We observed moderate to large gains in all clinical competency areas measured supporting both the immediate educational impact of WISE OnCall on performance and the sensitivity and responsiveness of our measures to instruction. The decrease in the global professionalism rating by the SPs after the module is intriguing. It is possible that some students, after being reminded by the WISE OnCall module to be more clinically systematic and thorough, did this at the expense of the other aspects of professional communication, such as rapport building in this time-bounded patient care task. We will be exploring this potentially unintended negative phenomenon in future studies.
It is not surprising that medical students learned in response to instruction. However, given the consistency and magnitude of the improvement and the fact that these were senior medical students, it is likely that this reflects that WISE OnCall's benefit is in reminding students of previous knowledge and ability rather than de novo learning.23,24 Medical students develop basic cognitive schema for oliguria during both preclinical and clinical training. With regular practice during the clinical clerkship curriculum, we assume that students automate more sophisticated thinking patterns and store complex schemas in long-term memory. However, during the fourth and final year of medical school, this material is probably not frequently accessed because our students spend 12 weeks on a scholarly activity, complete only 6 required clinical weeks (critical care and subinternship), and spend a significant amount of time focused on the residency selection process.25–27 We believe that this supports the importance of focused learning experiences, such as WISE OnCall, in critical competency domains as part of transition to internship.
The good news is that at the end of medical school, many students are ready for basic clinical tasks and most are primed and easily reminded of what they have learned. The WISE OnCall module is potentially an efficient method to both remind students of what they already know and boost their capacity to “put it all together.”
Of course, aggregate data mask important individual patterns of response to this learning experience. Most students had improvements in their pre– to post–WISE OnCall clinical skills and clinical reasoning, but a significant minority demonstrated a deterioration of performance over the course of this study. Because participation in the study was anonymous, we could not interview individual students to explore reasons for this pattern. However, it suggests that this type of readiness for internship experience may be useful in identifying individuals in need of further attention and/or remediation before undertaking clinical responsibilities without supervision as an intern.
The evidence to support the validity of our measurement approach to assessing the impact of the WISE OnCall module on core clinical coverage skills needed in internship includes that (1) the constructs measured were performance based and aligned with expert sources on readiness for residency7,8 and the explicit objectives in the WISE OnCall module; (2) the observation and scoring of student skills were made in the rich context of 2 clinical content concordant cases from 3 important perspectives—the patient, nurse, and attending physician—using established rater training and materials, suggesting this was an authentic response process28; (3) experienced and calibrated SPs reported if students collected the available clinical data accurately and completely using appropriate skills, the SN observed and reported on the content and quality of the interprofessional communication and clinical management at the bedside, and an experienced clinician scored the patient note as an ecologically valid manifestation of the students clinical reasoning; and (4) relationship among the measured variables is as hypothesized with correlation between raters observing the same performance and lack of correlation among those direct observers and assessment based on a written note. Unfortunately, rater reliability continues to be a major threat to the internal validity of this study. It remains to be seen if these measures track individual development over time or predict educational or clinical outcomes. We will be exploring our ability to provide meaningful educational handoffs to trainees and residency program directors.
Limitations
The major threat to the validity of our findings is the lack of a control group. We did not include one because we were concerned that we would not be able to recruit enough volunteers for an adequate sample size. Now that we have reason to expect hardy effect sizes, we will be able to randomly assign students to a condition without the WISE OnCall module even with relatively small numbers of participants. It is possible that the findings can be explained simply by the training effect of engaging in 2 sequential simulations. Even if valid, there are several aspects of this study, which limit generalizability of the findings and will be addressed in the future. Subjects were self-selected volunteers and may not reflect the general population of graduating medical students. The performance data are based on a single pre- and postmodule case in a single clinical domain and may not reflect clinical competence in general. Interrater reliability was moderate for SN and clinical reasoning measure. Although we carefully sought to design 2 equally difficult cases, we did not randomly alternate the cases to ensure our findings were not biased. For purely pragmatic reasons, all students received the same cases in the same order. Therefore, it is possible that, independent of the impact of the module, our findings are explained by the second case being significantly easier than the first.
FUTURE DIRECTIONS
Boosting skills and knowledge at the end of medical school and at the beginning of residency remains important to protect patients during the first few months of residency. Future studies should evaluate various strategies to accomplish this and consider long-term retention of learning, potential negative implications for professionalism, cost, and effectiveness measured by educationally and patient-relevant outcomes. We are in the process of studying the longer-term impact of WISE OnCall by following some of our study subjects into residency, experimenting to identify the best sequence of SP/SN cases and WISE OnCall to enhance readiness for residency, and exploring the case specificity of the learning from a particular WISE OnCall module.
CONCLUSIONS
Not all graduating medical students are ready for assessing and managing low urine output, a common on-call situation. As we have shown, it may be possible to assess and improve their readiness through individualized, clinically meaningful measurements and interval training sessions at the end of medical school. Such efforts may have a significant role in ensuring patient safety, especially early on in the residency year. We are currently engaged in refining this approach and expanding the clinical coverage issues addressed in the hopes that we can produce measures of readiness for internship suitable for meaningful educational handoffs of trainees from undergraduate to graduate medical education settings. This work could lead to both benchmarked, clinically meaningful measures and methods to assess readiness for internship and an efficient educational approach to addressing performance gaps.29,30 WISE OnCall was designed to be used in this way addresses predictable, level-appropriate just-in-time learning needs.
Supplementary Material
Footnotes
WISE onCall was developed at NYU School of Medicine. D.S. is the Executive Director for both WISE-MD, which produces and distributes WISE onCall, and the New York Simulation Center. Both are not-for-profit entities. M.W.N. is a member of the Program for Medical Education and Technology at the NYU School of Medicine and Technical Director for WISE-MD and WISE onCall. The other authors declare no conflict of interests.
D.S. is an Emergency Medicine physician at the Brigham and Women's Hospital Emergency Department and is the Senior Director of the Institute for Medical Simulation at the Center for Medical Simulation in Boston. At the time of the study, he was an Assistant Professor in the Department of Emergency Medicine at NYU School of Medicine and the Medial Director and Fellowship Director at The New York Simulation Center for Health Sciences (NYSIM). K.U. at the time of the study was a Fellow in Simulation and Education at NYU and NYSIM and is currently a Fellow in Maternal Fetal Medicine at the University of Southern California. B.R.G. at the time of the study was a Fellow in Simulation and Education at NYU and NYSIM and is currently an Assistant Professor in the Department of Emergency Medicine at The Ohio State University. S.D.Y. is an Assistant Professor of Journalism at Central Connecticut State University, a PhD Candidate in the Educational Communication and Technology program at NYU/Steinhardt, and a Research Assistant at the NYU School of Medicine. H.S. is an Assistant Professor of Education at Georgian Court University, NJ, and a consultant of WISE OnCall project at NYU School of Medicine. M.W.N. is a member of the Program for Medical Education and Technology at the NYU School of Medicine and Technical Director for the WISE MD initiative. G.N. is the Nursing Director and the NYSIM-Hearst Foundations Nursing and Allied Health Fellowship Director at The New York Simulation Center for the Health Sciences. M.V.P. is the Director of the Division of Learning Analytics in the NYU School of Medicine Institute for Innovations in Medical Education and Assistant Professor of Emergency Medicine. T.S.R. is the Frank C. Spencer Professor of Surgery and currently Associate Dean, Medical Education and Technology, Director of the Office On Continuing Medical Education, New York University School of Medicine, Executive Director of WISE-MD and WISE OnCall, and the Executive Director of the New York Simulation Center for the Health Sciences. A.K. is the Arnold P. Gold Professor of Humanism and Professionalism, Professor of Medicine and Surgery and Director of Research on Medical Education and Outcomes (ROMEO) unit of the Division of General Internal Medicine and Clinical Innovations (DGIMCI), and Director Research Program on Medical Education and Technology (PMET).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.simulationinhealthcare.com).
REFERENCES
- 1.Minter RM, Amos KD, Bentz ML, et al. Transition to surgical residency: a multi-institutional study of perceived intern preparedness and the effect of a formal residency preparatory course in the fourth year of medical school. Acad Med 2015;90:1116–1124. [DOI] [PubMed] [Google Scholar]
- 2.Lyss-Lerman P, Teherani A, Aagaard E, Loeser H, Cooke M, Harper GM. What training is needed in the fourth year of medical school? Views of residency program directors. Acad Med 2009;84:823–829. [DOI] [PubMed] [Google Scholar]
- 3.Sachdeva AK, Loiacono LA, Amiel GE, Blair PG, Friedman M, Roslyn JJ. Variability in the clinical skills of residents entering training programs in surgery. Surgery 1995;118:300–308. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 4.Fisher JW, Thompson BM, Garcia AD. Integrative clinical experience: an innovative program to prepare for internship. Teach Learn Med 2007;19:302–307. [DOI] [PubMed] [Google Scholar]
- 5.Laack TA, Newman JS, Goyal DG, Torsher LC. A 1-week simulated internship course helps prepare medical students for transition to residency. Simul Healthc 2010;5:127–132. [DOI] [PubMed] [Google Scholar]
- 6.Teo AR, Harleman E, O'Sullivan PS, Maa J. The key role of a transition course in preparing medical students for internship. Acad Med 2011;86:860–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education (ACGME). Specialty-Specific Duty Hour Definitions. Available at: https://www.acgme.org/Portals/0/PDFs/DH_Definitions.pdf. Accessed February 26, 2017.
- 8.Association of American Medical Colleges (AAMC). The Core Entrustable Professional Activities for Entering Residency. Available at: https://www.aamc.org/initiatives/coreepas. Accessed February 26, 2017. [DOI] [PubMed]
- 9.Collins A, Brown JS, Newman SE. Cognitive apprenticeship: teaching the crafts of reading, writing, and mathematics, learning and instruction: essays in honor of Robert Glaser. In: Resnick LB, ed. New Jersey: Lawrence Erlbaum Associates; 1989:453–494. [Google Scholar]
- 10.Stalmeijer RE, Dolmans DH, Snellen-Balendong HA, van Santen-Hoeufft M, Wolfhagen IH, Scherpbier AJ. Clinical teaching based on principles of cognitive apprenticeship: views of experienced clinical teachers. Acad Med 2013;88:861–865. [DOI] [PubMed] [Google Scholar]
- 11.Kalet AL, Coady SH, Hopkins MA, Hochberg MS, Riles TS. Preliminary evaluation of the web initiative for surgical education (wise-md). Am J Surg 2007;194:89–93. [DOI] [PubMed] [Google Scholar]
- 12.Kalet AL, Song HS, Sarpel U, et al. Just enough, but not too much interactivity leads to better clinical skills performance after a computer assisted learning module. Med Teach 2012;34:833–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song HS, Kalet AL, Plass JL. Assessing medical students' self-regulation as aptitude in computer-based learning. Adv Health Sci Educ Theory Pract 2011;16:97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song HS, Kalet AL, Plass JL. Interplay of prior knowledge, self-regulation and motivation in complex multimedia learning environments. J Comput Assist Learn 2016;32:31–50. [Google Scholar]
- 15.Song HS, Pusic M, Nick MW, Sarpel U, Plass JL, Kalet AL. The cognitive impact of interactive design features for learning complex materials in medical education. Comput Educ 2014;71:198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yavner SD, Pusic MV, Kalet AL, et al. Twelve tips for improving the effectiveness of web-based multimedia instruction for clinical learners. Med Teach 2015;37:239–244. [DOI] [PubMed] [Google Scholar]
- 17.Zabar S, Kachur E, Kalet A, Hanley K. Objective Structured Clinical Examinations: 10 Steps to Planning and Implementing Osces and Other Standardized Patient Exercises. New York, NY: Springer Science & Business Media; 2012. [Google Scholar]
- 18.Zabar S, Adams J, Kurland S, et al. Charting a key competency domain: understanding resident physician interprofessional collaboration (IPC) skills. J Gen Intern Med 2016;31:846–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gillespie C, Adams J, Hanley K, et al. ‘We might as well be speaking different languages’: an innovative interprofessional education tool to teach and assess communication skills critical to patient safety. BMJ STEL 2015;1:54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med 1999;74:1203–1207. [DOI] [PubMed] [Google Scholar]
- 21.Cohen J. Statistical Power Analysis for the Behavioural Sciences. rev. ed Hillsdale, NJ: Lawrence Erlbaum Associates; 1977. [Google Scholar]
- 22.Magnusson K. Interpreting Cohen's d Effect Size: An Interactive Visualization. Available at: http://rpsychologist.com/d3/cohend/. Accessed February 27, 2017.
- 23.Pusic MV, Boutis K, Hatala R, Cook DA. Learning curves in health professions education. Acad Med 2015;90:1034–1042. [DOI] [PubMed] [Google Scholar]
- 24.Pusic MV, Kessler D, Szyld D, Kalet A, Pecaric M, Boutis K. Experience curves as an organizing framework for deliberate practice in emergency medicine learning. Acad Emerg Med 2012;19:1476–1480. [DOI] [PubMed] [Google Scholar]
- 25.Benson NM, Stickle TR, Raszka WV., Jr Going "fourth" from medical school: fourth-year medical students' perspectives on the fourth year of medical school. Acad Med 2015;90:1386–1393. [DOI] [PubMed] [Google Scholar]
- 26.Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard medical school. Acad Med 2007;82:452–457. [DOI] [PubMed] [Google Scholar]
- 27.Wu EH, Elnicki DM, Alper EJ, et al. Procedural and interpretive skills of medical students: experiences and attitudes of fourth-year students. Acad Med 2008;83:S63–S67. [DOI] [PubMed] [Google Scholar]
- 28.Cook DA, Beckman TJ. Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med 2006;119:166.e7–166.e16. [DOI] [PubMed] [Google Scholar]
- 29.Ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ 2013;5:157–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lypson ML, Frohna JG, Gruppen LD, Woolliscroft JO. Assessing residents' competencies at baseline: identifying the gaps. Acad Med 2004;79:564–570. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


