Abstract
Introduction and objective
Studies on telemedicine have shown success in reducing the geographical and time obstacles incurred in the receipt of care in traditional modalities with the same or greater effectiveness; however, there are several barriers that need to be addressed in order for telemedicine technology to spread. The aim of this review is to evaluate barriers to adopting telemedicine worldwide through the analysis of published work.
Methods
The authors conducted a systematic literature review by extracting the data from the Cumulative Index of Nursing and Allied Health Literature (CINAHL) and PubMed (MEDLINE) research databases. The reviewers in this study analysed 30 articles (nine from CINAHL and 21 from Medline) and identified barriers found in the literature. This review followed the checklist from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009. The reviewers organized the results into one table and five figures that depict the data in different ways, organized by: barrier, country-specific barriers, organization-specific barriers, patient-specific barriers, and medical-staff and programmer-specific barriers.
Results
The reviewers identified 33 barriers with a frequency of 100 occurrences through the 30 articles. The study identified the issues with technically challenged staff (11%), followed by resistance to change (8%), cost (8%), reimbursement (5%), age of patient (5%), and level of education of patient (5%). All other barriers occurred at or less than 4% of the time.
Discussion and conclusions
Telemedicine is not yet ubiquitous, and barriers vary widely. The top barriers are technology-specific and could be overcome through training, change-management techniques, and alternating delivery by telemedicine and personal patient-to-provider interaction. The results of this study identify several barriers that could be eliminated by focused policy. Future work should evaluate policy to identify which one to lever to maximize the results.
Keywords: Barriers, adoption, implementation, telemedicine, mHealth
Introduction
Rationale
This review uses the definition of telehealth from the World Health Organization (WHO):
The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.1
For the purposes of our systematic review, this definition defines our topic and identifies the key terms for a literature search. We also follow WHO’s practice of not distinguishing between telemedicine and telehealth, and for this review we use the term ‘telemedicine’ to refer to telemedicine or telehealth.1 WHO identifies some common elements that telemedicine should include: providing some sort of clinical support, overcoming a barrier of proximity, using some sort of information and communications technology, and for the overall benefit of the patient.1
The topic of using telemedicine to address world health issues warrants study, as does the identification of barriers to adoption and possible mechanisms to overcome those barriers. telemedicine increases access to general and specialized healthcare services, delivers care to rural areas, offers providers greater flexibility in scheduling, and saves patients’ time and money in seeking care. A recent study conducted in the US Department of Veterans Affairs found that delivering care through telemedicine saves the patient an average of 145 miles and 142 minutes per visit.2 A teleneurology study showed that patients were saved, on average, two hours of travel time and US$70 per visit.3 An orthopaedic study showed a total savings of US$5,538,120 for 921 patients living in remote areas over 5.5 years.4 Studies in developing countries bridge proximal boundaries through the use of text messages for prenatal and post-partum care in Africa.5,6 Barriers to adopt telemedicine remain in both developed and developing countries and unnecessarily slow its diffusion. Developing countries may also struggle with the implementation of technology, such as high-speed Internet.1 The global diffusion of telemedicine can provide many advantages to both providers and patients, but barriers exist. Other studies have examined barriers in specific countries and regions, but not in the last several years, and not a comparison on an international level.7,8
Objective
The objective of this study is to examine the various challenges faced in implementing telemedicine among several different countries to identify any new trends compared with similar studies from several years past. What are the principal barriers to the adoption of telemedicine? What countries are experiencing barriers? Which barriers are unique to some groups in the healthcare industry? Is there public policy that could help overcome these barriers? Our review aims to record the most frequently faced challenges and the efforts to overcome those challenges.
Methods
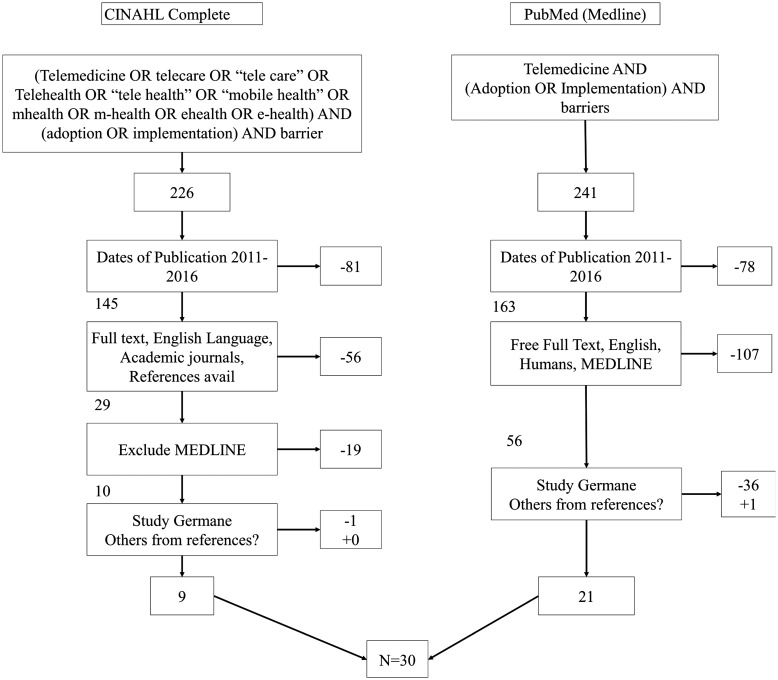
We conducted a systematic review of the literature by extracting data from the Cumulative Index of Nursing and Allied Health Literature (CINAHL) and PubMed (MEDLINE) research databases. Searches were performed between 6 and 10 June 2016. The keywords used for the research in this study were barriers, adoption, implementation, telemedicine, tele care, telecare, tele health, telehealth, mobile health, mHealth, m-Health, eHealth, and e-Health. The terms used in the searches were slightly different between the two databases, primarily because the two databases index differently. Figure 1 illustrates the search process with inclusion and exclusion criteria. As depicted, the exact search phrase in CINAHL was ‘((Barriers) AND (Adoption OR Implementation)) AND (“Telemedicine” OR “Tele care” OR “Mobile health” OR “eHealth” OR “mhealth” OR “m-health” OR “e-health” OR “Telecommunication” OR “telehealth” OR “Self care”)’. In PubMed (MEDLINE), all the sub-terms used in the CINAHL search were already nested under telemedicine in the PubMed Medical Subject Headings (MeSH) of telemedicine. Boolean operators and quotation marks were used in the search process to capture variations in the lexicon and to identify the desired intersection of telemedicine and barriers.
Figure 1.
Literature search with inclusion and exclusion criteria.
When the above-mentioned keywords were used, 226 articles from CINAHL Complete and 241 articles from PubMed were obtained. The articles were filtered using the publication dates ranging from the year 2011 to 2016 to evaluate the most recent barriers in implementing telemedicine and telehealth. The inclusion criteria used for PubMed were: free full-text, English language, and humans, focusing mainly on articles from MEDLINE. The inclusion criteria from the CINAHL-Complete database were: full text, English language, humans, academic journals, and references available. We excluded MEDLINE from CINAHL complete because the search criteria for PubMed included only MEDLINE articles. After applying the filters to both the PubMed and CINAHL Complete databases, the search was narrowed down to 56 and 10 articles, respectively. A literature matrix was created to list all the articles; the articles were then divided between reviewers so that at least two reviewers screened each abstract. Reviewers used a spreadsheet to compile their recommendations on whether the article was germane to this review, and a consensus meeting was called to share notes. Articles deemed not germane by at least two reviewers were excluded, and the articles for which the authors’ recommendations conflicted were discussed to reach consensus. The references from the remaining articles were visually scanned to identify common studies that were not already captured. This process added one additional article. Through our process, 30 articles were selected for the systematic literature review. These 30 articles were divided between the reviewers so that at least two reviewers read each article and made notes to identify barriers. A second consensus meeting was called to compare notes and to reach agreement on the barriers identified. We identified barriers by country and organized them into several bar charts organized by frequency of occurrence in the literature.
Results
We reviewed 30 articles related to the significant barriers to implementing telemedicine around the world.9–38 Our results are tabulated in Table 1. The articles were diverse and originated from a variety of countries, but reviewers identified similarities between barriers listed in multiple countries.
Table 1.
Results of analysis.
| Author(s) | Barriers | Country of origin |
|---|---|---|
| Molfenter et al.9 | Cost, reimbursement, technology-challenged staff, implementation models, confidentiality | USA |
| Petersen and DeMuro10 | Privacy, legal, and technically challenged staff | USA |
| Kontos et al.11 | Age, socioeconomic status, gender, level of education | USA |
| Levine et al.12 | Info overload, poor design, liability issues, cost, uncertain outcomes | USA |
| Adler et al.13 | Resistance to change | USA |
| Kahn et al.14 | Hospital size, profit status, teaching status, rural setting | USA |
| Rutledge et al.15 | Unawareness | USA |
| LeRouge and Garfield16 | Bandwidth, security, state licensing, return on investment (ROI) for providers, resistance to change, technically challenged staff | USA |
| Mohr et al.17 | Cost, availability of tech support, reimbursement, impersonal technology (provider perceptions) | USA |
| Cherney and van Vuuren18 | Licensure, reimbursement, privacy, and confidentiality | USA |
| Silva et al.19 | Bandwidth, resistance to change, legal, licensure, and reimbursement | USA |
| Young et al.20 | Resistance to change | USA |
| Ross et al.21 | Organization: cost, legal, social, and ethical. Individual: unawareness, low e-Health literacy, cost, interoperability | UK |
| Plaete et al.22 | Workflow, resistance to change, poor design, age, level of education | UK |
| Sanders et al.23 | User expectations, computer literacy, and privacy concerns | UK |
| Mair et al.24 | Resistance to change, technically challenged staff, time consuming | UK |
| May et al.25 | Interoperability, uncertainty of outcomes | UK |
| Plaete et al.26 | Level of educational, age | Belgium |
| Ronda et al.27 | Unawareness, apathy, computer literacy | Netherlands |
| Robben et al.28 | Computer literacy, preference for personal communication | Netherlands |
| Van Deursen and van Dijk29 | Age, level of education, poor e-Health literacy | Netherlands |
| Stroetmann et al.30 | Unique patient identifiers, interoperability, reimbursement, loosely defined details surrounding telemedicine, security, legal and regulatory limitations, cost, bandwidth | Europe |
| Schwarz et al.31 | Technically challenged staff, resistance to change | Australia |
| Lycett et al.32 | Outdated hardware, bandwidth, software speed, interoperability | Australia |
| Sinclair et al.33 | Resistance to change, clinician perception of impersonal care, technically challenged staff, cost, time limitations | Australia |
| Medhanyie et al.34 | Technically challenged staff, resistance to change | Ethiopia |
| Bigna et al.35 | Language barrier, some patients do not own mobile phone | Africa |
| Mohammadzadeh et al.36 | Resistance to change, technically challenged staff, cost, interoperability, infrastructure, privacy and data security, quality of health services, battery life | Iran |
| El-Mahalli et al.37 | Unawareness, technically challenged staff, poor design, use of store-and-forward | Saudi Arabia |
| Scholl et al.38 | Poor design, high expectations of users, technically challenged staff | India |
This table enumerates the barriers identified by the authors and the countries of origin from the study.
Table 1 enumerates the barriers identified by the reviewers and the countries of origin from the study. Reviewers used similar terminology across studies to highlight similarities across countries. A total of 33 barriers mentioned a total of 100 times, stemming from studies in seven areas of the world, were identified.9–38
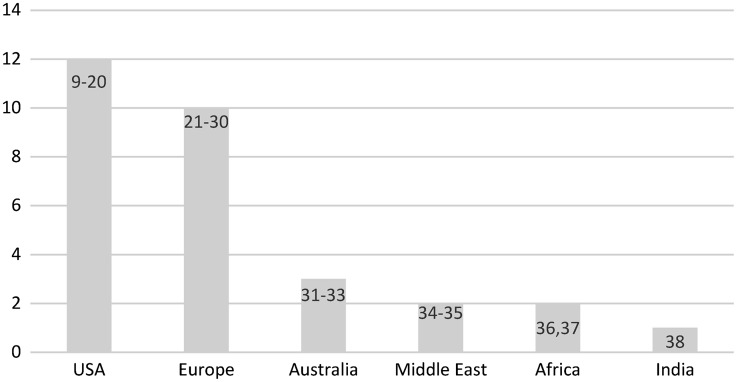
Figure 2 graphically organizes the countries/continents of origin by frequency of occurrence in the literature. A preponderance of the literature stems from the USA (40%),9–20 followed by Europe (33%),21–30 Australia (10%),31–33 Africa (6%),34,35 the Middle East (6%),36,37 and India (3%).38 Numbers do not sum to 100% because of rounding.
Figure 2.
Frequency of barriers by country.
This figure graphically organizes the barriers listed for each country in order of frequency from the literature. The authors categorized these by country or continent. The numbers in each bar correspond to the reference number of the article which also aligns with the order in the References section. A preponderance of the literature stems from the USA (40%), followed by Europe (33%), Australia (10%), Africa (9%), the Middle East (6%), and India (3%).
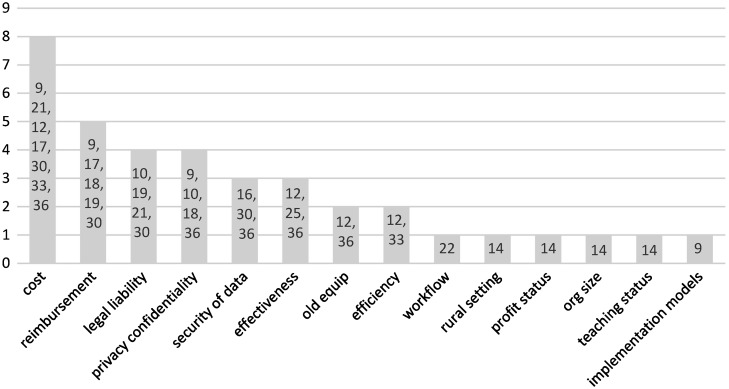
Figure 3 organizes the barriers listed in order of frequency. The authors categorized these as organizational barriers, and across 14 unique barriers they account for 37% of the total frequency of occurrences of barriers listed. Several of the barriers listed were only mentioned once in the literature. The barriers of cost and reimbursement are similar, and together these account for 13% of the barriers listed.9,12,16–19,21,30,33,36 Similarly, the barriers of legal liability, privacy and confidentiality concerns, and security of data are similar, and together these account for 11% of the barriers listed.9,10,16,18,19,21,30,36 The only other barriers that seemed to relate to one another among the organizational barriers were efficiency and workflow.22,24,33 Together, these accounted for 5% of the barriers mentioned. The last 7% of barriers listed were effectiveness, outdated equipment, rural setting, profit status, organization size, teaching status, and lack of implementation models.9,12,14,32,36
Figure 3.
Frequency of barriers for organizations.
This figure graphically organizes the barriers listed in order of frequency. The authors categorized these as organizational barriers to the adoption of telemedicine. The numbers in each bar correspond to the reference number of the article which also aligns with the order in the References section
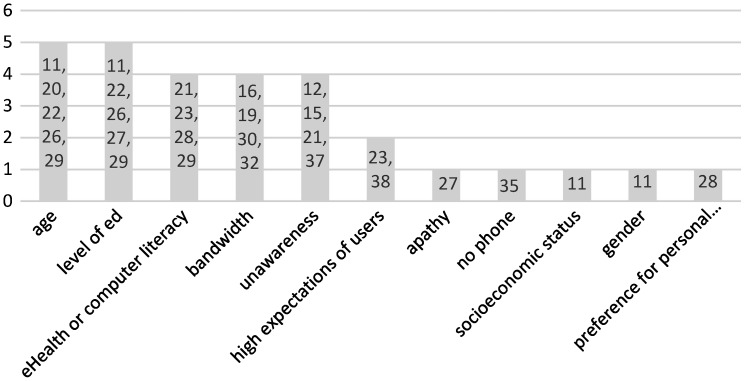
Figure 4 organizes the barriers listed in order of frequency. The authors categorized these as patient barriers, and across 11 unique barriers they account for 29% of the total frequency of barriers listed. The age of the patient and level of education each accounted for five out of the 29 patient barriers (17%).11,20,22,26,27,29 The limit of eHealth or computer literacy, bandwidth of dwelling, and a state of unawareness of the existence of several telemedicine products and services each accounted for four of the 29 patient barriers (14%).12,15,16,19,21,23,28–30,32,37 The high expectation of users accounted for two of the 29 patient barriers (7%).23,38 The remaining five barriers were only mentioned once, but together these account for a total of 17% of the patient barriers listed.11,28,35
Figure 4.
Frequency of barriers for patients.
This figure graphically organizes the barriers listed in order of frequency. The authors categorized these as patient barriers to the adoption of telemedicine. The numbers in each bar correspond to the reference number of the article which also aligns with the order in the References section.
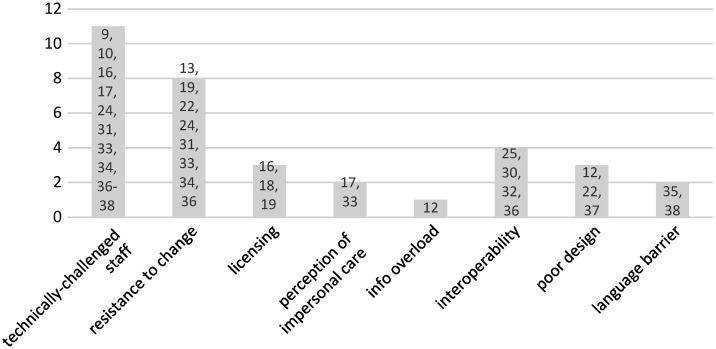
The remaining eight barriers depicted in Figure 5 were categorized by staff (5 out of 8, 62%) and computer programmers (3 out of 8, 38%), and across these eight unique barriers, together, these accounted for 34% of the total frequency of barriers listed. By a wide margin, the barrier most often cited is the limitations of a technically challenged staff (11% of all barriers),9,10,16,17,24,31,33,34,36–38 followed by resistance to change (8% of all barriers).13,19,22,24,31,33,34,36 Licensing issues is a significant barrier because countries and states within countries all require individual licensing requirements. Despite this significant challenge, this barrier only accounted for 3% of all barriers.16,18,19 Perception of impersonal care and information overload were mentioned twice17,33 and once,12 respectively. The last three barriers seemed to be unique to the programmers. Issues of interoperability (4% of all barriers),25,30,32,36 poor application design (3% of all barriers),12,22,37and language barriers (2% of all barriers)35,38 all accounted for 9% of all the occurrences of barriers listed in the literature.
Figure 5.
Frequency of barriers for staff and programmers.
This figure graphically organizes the barriers listed in order of frequency. The authors categorized these as staff and programmer barriers to the adoption of telemedicine. The programmer barriers are the last three on the right. The numbers in each bar correspond to the reference number of the article which also aligns with the order in the References section.
Computer or eHealth literacy were listed as the main barrier to adopting telemedicine in several countries such as the UK and the Netherlands.21–25,27–29 Specifically mentioned in several articles was the lack of available high-speed bandwidth,16,19,30,32 issues with application design,12,22,37 and overall interoperability continues to be a concern because of so many standards adopted at different rates by disparate countries.25,30,32,36 Additionally, having the right equipment was also a significant barrier listed.32,36 Age-related barriers11,20,22,26,29 exist due to lack of exposure to and training in the new technology. Providers’ perceptions that telemedicine would not be personal care28 were complemented by patients’ preferences for personal communication.17,33
Resistance to change was a significant barrier,16,31,34 and this is exacerbated by the high cost9,12,17,21,30,33,36 of the technology and the lack of reimbursements available for care delivered through telemedicine.9,17,18,30 Providers who made the investment in telemedicine were concerned about reimbursement and receiving a return on their investment. Telemedicine requires significant changes to the existing workflows and many staff and providers have to invest time in training new workflows and techniques, and this affects both efficiency24,33 and effectiveness of the care.12,25,36
Confidentiality and privacy issues comprised the barrier topic for 11% of the articles reviewed.9,10,16,18,19,21,30,36 Issues include breach of personal health information that can occur on unsecured networks, as well as unlocked and unencrypted hardware that can be accessed by third parties. Patient’s lack of understanding regarding telemedicine security can make them resistant to adoption. This issue was listed as a concern in the major developed countries such as the US and the UK.
A problem to the US and Canada is state licensing limitations, which prevents an out-of-state physician to treat another patient through telemedicine.16,18
Discussion
Concise summary of main findings
In this review, we identified the common barriers faced by disparate countries at different points on a spectrum of technological maturity, such as convincing leadership that telemedicine is a solid investment, convincing providers that telemedicine is an effective way to treat patients, getting staff to accept the idea and learning strategies, and teaching patients the technological skills required to access telemedicine.
The evidence from this review suggests that the areas where telemedicine has proven to be an effective tool for reaching patient populations in various countries include telemetry, mental health, and diabetes management.14,27,33 We recommend that the policymaking bodies of each country should consider the use of telemedicine to bridge gaps of coverage in all geographical areas, but particularly those in rural settings. The ubiquitous presence of high-speed bandwidth would help bridge a geographical gap of medical access in rural settings. If competitive markets have failed to bring this bandwidth and equipment to these communities, then the respective governments should consider implementing policy to cover the gap. The technology-acceptance gap in older age groups is congruent with the patients’ preferences; therefore, public policy may not be able to help in this area. Providers should accept this preference and wait for new-technology acceptance through the aging population. The countries that listed provider resistance include Ethiopia, UK, Australia, US, and Iran.13,22,31,34 Incentives should be considered to encourage participation in telemedicine modalities of care. Incentives can take the form of monetary rewards, such as the US with its ‘Meaningful Use’ criteria, or disincentives such as fines or less-than-full reimbursement for care. Public information efforts may help overcome this misunderstanding of information-security mechanisms. Finally, the US should consider resolving detriments to inter-state commerce. The US Constitution establishes a supremacy clause that would justify a federal removal of this impediment.
Comparisons to other studies and divergent results
It is not new to observe the use of health information technology for the management of chronic disease, particularly diabetes.39,40 Studies and reviews have identified the effective use of health information technology in this regard, but it is disappointing to encounter apathy on the part of patients for managing their own disease.27 Our review found similar results to other studies, but we added the international comparisons which have not been presented previously in the peer-reviewed literature.
Strengths and limitations to this review
This review adds to a body of knowledge of telemedicine adoption and barriers to the same by comparing the barriers worldwide. This review was structured in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. PRISMA is an international standard for the organization and reporting of randomized control trials, evaluations of interventions, and other types of research. It is endorsed by five editorial organizations and more than 200 journals worlwide.41 Our review also limits the analysis to search results from two well-known research databases, uses key terms registered with MeSH, and uses multiple reviewers to determine the inclusion and exclusion criteria.
The chief limitation of this study is that only five years were examined. An objective assessment of study bias was conducted in this review, but when articles/studies are screened for selection criteria, human judgment can sway the results. We controlled for this limitation through two practices: more than one reviewer examined each article, and we held a series of consensus meetings to ensure we were looking for the same characteristics in studies. We called them consensus meetings because we did not end the meetings until we reached consensus.
We conducted several consensus meetings to specifically address selection bias. As a result, we expect that this review should have a high rate of reliability. We did not control for publication bias.
Recommendations for further research
Public policy could compensate for barriers common in several countries, but it becomes difficult for many nations to act in accord, particularly when monetary incentives can differ between countries. Future research could start with the assembly of a Delphi team to identify possible common ground for international public policy. From the results of the Delphi team, surveys could go out to an international community inviting standards for interoperability and universal acceptance of telemedicine as a means to expand access to care.
Conclusions
Telemedicine is widely used in a majority of the countries discussed as a tool to increase the access to healthcare through the elimination of proximity from the equation of care. However, technology barriers and lack of computer literacy prevailed as a major issue in successfully implementing telemedicine. Our research is successful in identifying the frequency of each barrier for organizations and a variety of stakeholders (patient, medical staff, computer programmer). Although telemedicine shows promise in its ability to increase access and efficiency, ease and acceptance of this modality of care is necessary for its diffusion. This systematic review provides direction for public policy to intervene across international boundaries and reduce the barriers currently experienced.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.World Health Organization (WHO). Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth, Global Observatory for eHealth seires – Volume 2. NLM classification W 26.5. ISBN 9789241564144. ISSN 2220-5462. Geneva: World Health Organization, 2010. [Google Scholar]
- 2.Russo JE, McCool RR, Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E Health 2016; 22(3): 209–215. [DOI] [PubMed] [Google Scholar]
- 3.Hatcher-Martin J, Anderson E, Factor S. Patient acceptance and potential cost-savings of teleneurology in an academic outpatient movement disorders practice (P1.022). Neurology 2016; 86(Suppl 16): P1–022. [Google Scholar]
- 4.Cota A, Tarchala M, Parent-Harvey C, et al. Review of 5.5 years’ experience using e-mail-based telemedicine to deliver orthopedic care to remote communities. Telemed J E Health 2017; 23(1): 37–40. [DOI] [PubMed] [Google Scholar]
- 5.Amoakoh-Coleman M, Borgstein AB, Sondaal SF, et al. Effectiveness of mHealth interventions targeting health care workers to improve pregnancy outcomes in low-and middle-income countries: a systematic review. J Med Internet Res 2016; 18(8): e226–e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hannan J, Brooten D, Youngblut JM, et al. Comparing mothers’ postpartum concerns in two clinical trials 18 years apart. J Am Assoc Nurse Pract 2016; 28(11): 604–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacFarlane A, Murphy AW, Clerkin P. Telemedicine services in the Republic of Ireland: an evolving policy context. Health Policy 2006; 76(3): 245–258. [DOI] [PubMed] [Google Scholar]
- 8.Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med Inform Decis Mak 2012; 12(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Molfenter T, Boyle M, Holloway D, et al. Trends in telemedicine use in addiction treatment. Addict Sci Clin Pract 2015; 10(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petersen C, DeMuro P. Legal and regulatory considerations associated with use of patient-generated health data from social media and mobile health (mHealth) devices. Appl Clin Inform 2014; 6(1): 16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kontos E, Blake KD, Chou WY, et al. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res 2014; 16(7): e172–e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine M, Richardson JE, Granieri E, et al. Novel telemedicine technologies in geriatric chronic non cancer pain: primary care providers’ perspectives. Pain Medicine 2014; 15(2): 206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adler G, Pritchett LR, Kauth MR, et al. A pilot project to improve access to telepsychotherapy at rural clinics. Telemed J E Health 2014; 20(1): 83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn JM, Cicero BD, Wallace DJ, et al. Adoption of intensive care unit telemedicine in the United States. Crit Care Med 2014; 42(2): 362–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutledge CM, Haney T, Bordelon M, et al. Telehealth: preparing advanced practice nurses to address healthcare needs in rural and underserved populations. Int J Nurs Educ Scholarsh 2014; 11(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 16.LeRouge C, Garfield MJ. Crossing the telemedicine chasm: have the US barriers to widespread adoption of telemedicine been significantly reduced? Int J Environ Res Publ Health 2013; 10(12): 6472–6484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohr DC, Burns MN, Schueller SM, et al. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen Hosp Psychiat 2013; 35(4): 332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherney LR, van Vuuren S. Telerehabilitation, virtual therapists, and acquired neurologic speech and language disorders. Semin Speech Lang 2012; 33(3): 243–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silva GS, Farrell S, Shandra E, et al. The status of telestroke in the United States a survey of currently active stroke telemedicine programs. Stroke 2012; 43(8): 2078–2085. [DOI] [PubMed] [Google Scholar]
- 20.Young LB, Chan PS, Cram P. Staff acceptance of tele-ICU coverage: a systematic review. Chest 2011; 139(2): 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross J, Stevenson F, Lau R, et al. Exploring the challenges of implementing e-health: a protocol for an update of a systematic review of reviews. BMJ Open 2015; 5(4): e006773–e006773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plaete J, Verloigne M, Crombez G, et al. What do general practitioners think about an online tailored self-regulation programme for primary prevention. European Health Psychologist 2014; 16(S): 889–889. [Google Scholar]
- 23.Sanders C, Rogers A, Bowen R, et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: a qualitative study. BMC Health Serv Res 2012; 12(1): 220–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mair FS, May C, O’Donnell C, et al. Factors that promote or inhibit the implementation of e-health systems: an explanatory systematic review. B World Health Organ 2012; 90(5): 357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.May CR, Finch TL, Cornford J, et al. Integrating telecare for chronic disease management in the community: what needs to be done? BMC Health Serv Res 2011; 11(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plaete J, Crombez G, DeSmet A, et al. What do general practitioners think about an online self-regulation programme for health promotion? Focus group interviews. BMC Fam Pract 2015; 16(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ronda MC, Dijkhorst-Oei LT, Rutten GE. Reasons and barriers for using a patient portal: survey among patients with diabetes mellitus. J Med Internet Res 2014; 16(11): e263–e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robben SH, Perry M, Huisjes M, et al. Implementation of an innovative web-based conference table for community-dwelling frail older people, their informal caregivers and professionals: a process evaluation. BMC Health Serv Res 2012; 12(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Deursen AJ, van Dijk JA. Internet skills performance tests: are people ready for eHealth? J Med Internet Res 2011; 13(2): e35–e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stroetmann KA, Artmann J, Stroetmann V. Developing national eHealth infrastructures–results and lessons from Europe. AMIA Annu Symp Proc 2011; 2011: 1347–1347. [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarz F, Ward J, Willcock S. E-Health readiness in outback communities: an exploratory study. Rural Remote Health 2014; 14: 2871–2871. [PubMed] [Google Scholar]
- 32.Lycett K, Wittert G, Gunn J, et al. The challenges of real-world implementation of web-based shared care software: the HopSCOTCH Shared-Care Obesity Trial in Children. BMC Med Inform Decis Mak 2014; 14(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sinclair C, Holloway K, Riley G, et al. Online mental health resources in rural Australia: clinician perceptions of acceptability. J Med Internet Res 2013; 15(9): e193–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medhanyie AA, Little A, Yebyo H, et al. Health workers’ experiences, barriers, preferences and motivating factors in using mHealth forms in Ethiopia. Hum Resour Health 2015; 13(2): 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bigna JJ, Noubiap JJ, Plottel CS, et al. Barriers to the implementation of mobile phone reminders in pediatric HIV care: a pre-trial analysis of the Cameroonian MORE CARE study. BMC Health Serv Res 2014; 14(1): 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohammadzadeh N, Safdari R, Rahimi A. Cancer care management through a mobile phone health approach: key considerations. Asian Pac J Cancer Prev 2013; 14(9): 4961–4964. [DOI] [PubMed] [Google Scholar]
- 37.El-Mahalli AA, El-Khafif SH, Al-Qahtani MF. Successes and challenges in the implementation and application of telemedicine in the eastern province of Saudi Arabia. Perspect Health Inf Manag 2012; 9. [PMC free article] [PubMed] [Google Scholar]
- 38.Scholl J, Syed-Abdul S, Ahmed LA. A case study of an EMR system at a large hospital in India: Challenges and strategies for successful adoption. J Biomed Inform 2011; 44(6): 958–967. [DOI] [PubMed] [Google Scholar]
- 39.Benhamou PY. Improving diabetes management with electronic health records and patients’ health records. Diabetes Metab 2011; 37: S53–S56. [DOI] [PubMed] [Google Scholar]
- 40.Kruse CS, Argueta DA, Lopez L, et al. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res 2015; 17(2): e40–e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, et al. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med 2009; 6(7): e1000097. DOI:10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed]