Abstract
Adult studies have reported associations of low 25-hydroxyvitamin D (25OHD) with dyslipidemia and cardiovascular disease; however, there are scarce pediatric data regarding relationships between vitamin D status and specific lipid markers affecting cardiovascular risk. In this cross-sectional study of children evaluated at university-based pediatric endocrinology clinics, 178 patients meeting criteria for overweight or obesity had 25OHD levels assessed over a 2-year period; 60 of 178 had non-HDL (high-density lipoprotein) cholesterol and fasting lipid parameters performed. Patients with 25OHD <20 ng/mL had significantly higher non-HDL cholesterol (134.76 ± 47.32 vs 108.85 ± 31.14, P < .03), triglyceride (TG)/HDL ratio (3.09 ± 2.26 vs 1.82 ± 1.18, P = .03), total cholesterol (TC)/HDL ratio (4.23 ± 1.23 vs 3.40 ± 1.05, P < .01), TC (184.15 ± 40.19 vs 158.89 ± 30.10, P < .01), and TG (134.76 ± 47.32 vs 78.93 ± 37.46, P < .03) compared with 25OHD ≥20 ng/mL. Vitamin D deficiency was significantly associated with increase in atherogenic lipids and markers of early cardiovascular disease. These findings suggest that vitamin D deficiency may have negative effects on lipid parameters with increase in cardiovascular risk.
Keywords: vitamin D, obesity, dyslipidemia, non-HDL cholesterol, cardiovascular disease
Introduction
The childhood obesity rate has more than tripled over the past 30 years, with obesity affecting 17% of children and adolescents ages 2 to 19 years in the United States.1 Obesity is a risk factor for vitamin D deficiency with serum 25-hydroxyvitamin D (25OHD) levels documented to be inversely related to body mass index (BMI). Vitamin D plays an essential role in calcium absorption and skeletal health. Studies have also reported nonskeletal associations of vitamin D deficiency, with low 25OHD found to be directly correlated with a variety of cardiometabolic risk factors including insulin resistance, hypertension, and dyslipidemia, as well as progression to diabetes mellitus.2,3
Adults with high lipoprotein ratios have increased risk of cardiovascular disease (CVD), and elevated non–high-density lipoprotein (non-HDL) cholesterol in childhood is shown to be related to cardiovascular risk in adulthood.4,5 Serum non-HDL cholesterol is the universal screening test recommended by the National Heart, Lung, and Blood Institute, in childhood, for dyslipidemia as it is considered a predictor for atherosclerosis in children and adolescents.6,7
Studies in adults have reported associations of low 25OHD with dyslipidemia and CVD.8,9 However, there are lack of data regarding the relationship between vitamin D status and specific lipid markers affecting cardiovascular risk during childhood. This is particularly important as low vitamin D status may be a modifiable risk factor for CVD. The objective of the study was to investigate the relationship between vitamin D status and cardiovascular risk, specifically using serum lipid markers, during childhood and adolescence. Our hypothesis was that non-HDL cholesterol, as well as total cholesterol (TC)/HDL and triglyceride (TG)/HDL lipoprotein ratios, would vary inversely with serum 25OHD levels.
Methods
Participants
In this cross-sectional study, children and adolescents ages 6 to 17 years were evaluated at the pediatric endocrinology outpatient clinics at Weill Cornell Medicine between April 2013 and May 2015 with vitamin D levels obtained at time of visit. Exclusion criteria included hepatic, renal, or malabsorptive disease, active vitamin D supplementation, metabolic bone disease, or primary hyperparathyroidism. Age, sex, pubertal status, 25OHD levels, and fasting lipid parameters (TC, TG, HDL, low-density lipoprotein [LDL], and non-HDL cholesterol) were collected. Vitamin D deficiency was defined as a vitamin D <20 ng/mL. Prepubertal status was defined as Tanner 1 breasts in females and a testicular volume of ≤3 mL in males. TC/HDL and TG/HDL ratios were calculated. This study was approved by the Weill Cornell Medical College Institutional Review Board.
Assays
Serum 25OHD measurements were performed by direct competitive chemiluminescence immunoassay using the DiaSorin LIASON kit. Lipid profiles were performed at the laboratory of New York Presbyterian Hospital. Only laboratory data performed at our institution were collected for review.
Statistical Analysis
Analyses were performed in SAS version 9.4 (SAS institute Inc, Cary, NC). Two-sided P values <.05 were considered to indicate statistical significance. Data are presented as mean ± standard deviation (SD), except where otherwise noted. Analysis of variance and χ2 test were used to compare groups of patients by demographic characteristics, as appropriate. Two-sample t tests or Wilcoxon rank sum tests were used to evaluate differences in metabolic parameters between the vitamin D deficient group (<20 ng/mL) and nondeficient group (≥20 ng/mL) and prepubertal versus pubertal groups, as appropriate. Multivariable linear regression models (ie, analysis of covariance models) were also used to compare metabolic parameters between the vitamin D deficient and nondeficient groups after adjustment for age, gender, and BMI SDS (SD score).
Results
A total of 178 patients (61 males and 117 females; age 12.1 ± 3.3 years) met criteria for overweight and obesity (BMI > 85th percentile). Sixty of 178 patients had fasting lipid parameters available. The clinical characteristics of the cohort are summarized in Table 1. Mean serum 25OHD was 20.7 ± 9.2 ng/mL, and more than half of all patients (55%) were vitamin D deficient. There was no significant difference between BMI and BMI percentile between vitamin D deficient (<20 ng/mL) and nondeficient patients, and mean BMI was at the 97th percentile in both groups.
Table 1.
Baseline Participant Characteristics.a
| All Subjects BMI >85th Percentile | Vitamin D <20 ng/mL | Vitamin D ≥20 ng/mL | P | |
|---|---|---|---|---|
| N | 60 | 33 | 27 | |
| Age, years | 12.28 (3.21) | 12.85 (3.26) | 11.59 (3.06) | .133 |
| Female sex, n (%) | 38 (63.33%) | 21 (63.64%) | 17 (62.96%) | .957 |
| 25OHD, ng/mL | 20.73 (9.22) | 15.20 (3.58) | 27.49 (9.54) | — |
| Height, cm | 155.01 (15.43) | 156.23 (15.35) | 153.51 (15.68) | .502 |
| Weight, kg | 75.38 (31.30) | 81.84 (34.68) | 67.48 (25.00) | .077 |
| Weight, SDS | 2.33 (0.74) | 2.35 (0.81) | 2.29 (0.64) | .752 |
| BMI, kg/m2 | 31.34 (7.38) | 32.92 (8.49) | 29.40 (5.28) | .066 |
| BMI, SDS | 2.18 (0.46) | 2.21 (0.48) | 2.14 (0.43) | .542 |
| BMI percentile | 97.52 (3.17) | 97.58 (3.17) | 97.46 (3.23) | .886 |
Abbreviations: BMI, body mass index; 25OHD, 25-hydroxyvitamin D; SDS, standard deviation score.
Data are means ± SD unless otherwise specified.
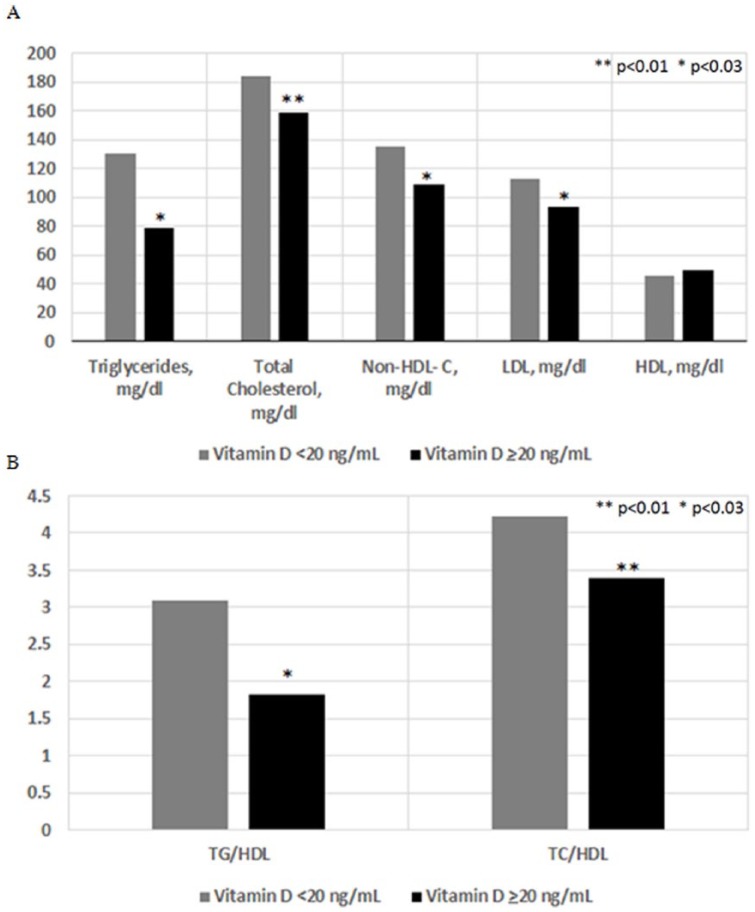
When laboratory results were analyzed according to vitamin D status, patients with vitamin D deficiency (25OHD <20 ng/mL) were found to have significantly higher non-HDL cholesterol, TC, TG, and LDL levels (P < .03) compared with patients with 25OHD ≥20 ng/mL (Table 2). In addition, significantly higher TG/HDL and TC/HDL ratios (P ≤ .03) were found in vitamin D deficient patients compared with nondeficient patients (Figure 1). After adjustment for BMI SDS, age, and gender, the effect of vitamin D status on lipid abnormalities remained significant (LDL, P = .042; non-HDL cholesterol, P = .010; TG, P = .041; total cholesterol, P = .022; TG/HDL ratio, P = .041; TC/HDL ratio, P = .021). Pubertal children with vitamin D deficiency showed significantly higher TC/HDL levels (4.26 ± 1.18 vs 3.42 ± 0.8, P < .02) than those with vitamin D status ≥20 ng/mL, while TC (P = .06), non-HDL cholesterol (P = .07), and TG/HDL (P = .09) approached significance.
Table 2.
Results of Lipid Parameters According to 25-Hydroxyvitamin D Statusa.
| All Subjects BMI >85th Percentile | Vitamin D <20 ng/mL | Vitamin D ≥20 ng/mL | P | |
|---|---|---|---|---|
| N | 60 | 33 | 27 | |
| Triglycerides, mg/dL | 107.15 (77.45) | 130.24 (93.26) | 78.93 (37.46) | .029 |
| Total cholesterol, mg/dL | 172.78 (37.90) | 184.15 (40.19) | 158.89 (30.10) | .009 |
| Non-HDL cholesterol, mg/dL | 125.35 (39.86) | 138.85 (41.53) | 108.85 (31.14) | .012 |
| TG/HDL | 2.52 (1.95) | 3.09 (2.26) | 1.82 (1.18) | .032 |
| TC/HDL | 3.86 (1.22) | 4.23 (1.23) | 3.40 (1.05) | .009 |
| LDL, mg/dL | 103.93 (32.36) | 112.53 (34.26) | 93.74 (26.89) | .025 |
| HDL, mg/dL | 47.43 (12.20) | 45.30 (8.94) | 50.04 (15.05) | .136 |
Abbreviations: BMI, body mass index; HDL, high-density lipoprotein; TG, triglycerides; TC, total cholesterol; LDL, low-density lipoprotein.
Data are means ± SD unless otherwise specified.
Figure 1.
Lipid parameters (A) and lipoprotein ratios (B) in vitamin D deficient versus nondeficient groups.
Discussion
This is one of the first studies to assess the relationship of vitamin D deficiency with both lipoprotein ratios and non-HDL cholesterol in children and adolescents with obesity or overweight status. In our study, over one half of children and adolescents were found to be vitamin D deficient, and vitamin D deficiency was found to be significantly associated with an increase in atherogenic lipids and known markers of early CVD. Non-HDL cholesterol, TC/HDL, TG/HDL, TC, and TG levels were all significantly higher in the vitamin D deficient patients compared with patients without vitamin D deficiency. These findings suggest that vitamin D deficiency may have negative effects on lipid markers, with an increase in cardiovascular risk among children and adolescents with low vitamin D levels.
Non-HDL cholesterol has been demonstrated to be more predictive of persistent dyslipidemia compared with other lipid parameters, as well as recognized as a better index than LDL cholesterol for identifying high-risk patients.6,10 In published guidelines for cardiovascular health and risk reduction in children and adolescents, serum non-HDL cholesterol is currently the universal dyslipidemia screening test recommended by the National Heart, Lung, and Blood Institute and supported by the American Academy of Pediatrics in childhood.6,7 In addition, several studies in adults have reported that lipid-related ratios such as TC/HDL and TG/HDL may be better predictors of cardiovascular risk than other markers used independently.4,11-14 In particular, TG/HDL has been strongly associated with predicting coronary artery disease and cardiovascular death in adults.13,15,16
Although there is no consensus regarding the definition of vitamin D deficiency in adults, it has been defined in the literature as a 25OHD level of <20 ng/mL.3,17 Cross-sectional analyses in adults have confirmed an association between optimal vitamin D status and a favorable lipid profile.8,9,18 However, there are very few pediatric studies in patients with overweight or obesity that have specifically evaluated the relationship of vitamin D status with serum non-HDL cholesterol or lipoprotein ratios. In a study by Nwosu et al, the authors analyzed vitamin D status and early markers of CVD in a prepubertal cohort of 45 patients including 20 patients with normal BMI status. In this study, vitamin D levels were found to vary inversely with non-HDL cholesterol, TC/HDL, and LDL.19 The authors reported a 25OHD level of 30 ng/mL to be associated with optimal cardioprotection in children. Although both lipoprotein ratios and non-HDL cholesterol were evaluated in the study by Nwosu et al, the authors looked specifically at prepubertal children of varying BMI status.
In a cross-sectional study of healthy children ages 1 to 5 years with a BMI >85th percentile in 25% of patients, the authors reported each 10 nmol/L increase in 25OHD to be associated with a decrease in non-HDL cholesterol concentration of 0.89 mg/dL, total cholesterol of 1.08 mg/dL, and triglycerides of 2.34 mg/dL. Associations between 25OHD and LDL and HDL were not found to be statistically significant; however, the laboratory studies were performed in a nonfasting state and in a younger cohort of patients during early childhood.7 Another study specifically evaluating African American adolescents (n = 24) found that 25OHD levels were inversely correlated with total cholesterol and non-HDL cholesterol levels.20 However, 19/24 patients in this study had a BMI <85th percentile. Lastly, in a cross-sectional study of children with obesity (n = 209; age 6-19 years) utilizing age, race/ethnicity, season, and BMI adjusted models, the authors reported that total cholesterol, non-HDL cholesterol, and oxidized LDL were inversely associated with log-transformed 25OHD.21 In this study, the relationship of lipoprotein ratios TG/HDL and TC/HDL with vitamin D status was not assessed.
To our knowledge, our study is the largest to date examining the association between 25OHD and both lipoprotein ratios and non-HDL cholesterol as markers of cardiovascular risk in children and adolescents with overweight and obesity. This study adds to the sparse pediatric literature on these particular predictors of cardiovascular risk. Our study’s limitations include its cross-sectional design, which prevents the ability to assess temporal associations between vitamin D levels and risk factors for CVD. Another limitation is the lack of data regarding race and ethnicity of our subjects. Despite these limitations, the study provides valuable insight into the relationship of vitamin D status and cardiometabolic risk through novel lipid indices in a pediatric cohort with overweight and obesity status. It emphasizes the need for further research to determine the short- and long-term risks in children and adolescents with vitamin D deficiency and dyslipidemia, and whether repletion of vitamin D leads to a decreased incidence of dyslipidemia with reduction in cardiovascular risk.
Conclusion
In conclusion, we found a high prevalence of vitamin D deficiency in our pediatric patients with overweight or obesity. Low vitamin D status was significantly associated with an increase in several atherogenic lipids and may be a modifiable risk factor for CVD. Given that children with obesity are already at higher risk for several comorbidities including metabolic syndrome, insulin resistance, hypertension, and hyperlipidemia, these results are particularly important and support screening children and adolescents with overweight or obesity for vitamin D deficiency. Our study highlights the role of monitoring vitamin D levels in children and adolescents with overweight or obesity, and the potential benefits of improving vitamin D status to reduce cardiometabolic risk.
Acknowledgments
We thank Dr. Oksana Lekarev for her review of this article.
Footnotes
Author Contributions: MC: Contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
HTM: Contributed to design; contributed to analysis and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
PJC: Contributed to design; contributed to analysis and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
TS: Contributed to conception and design; contributed to acquisition, analysis, and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Paul J. Christos and Hoda Hammad were partially supported by the following grant: Clinical and Translational Science Center at Weill Cornell Medical College (UL1-TR000457-06). The funding organization had no role in the study design; collection, analysis, and interpretation of data; or in the preparation, review, and submission of the manuscript.
ORCID iD: Marisa Censani  https://orcid.org/0000-0002-0247-3237
https://orcid.org/0000-0002-0247-3237
References
- 1. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307:483-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842-856. [DOI] [PubMed] [Google Scholar]
- 3. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281. [DOI] [PubMed] [Google Scholar]
- 4. Millan J, Pintó X, Muñoz A, et al. Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag. 2009;5:757-765. [PMC free article] [PubMed] [Google Scholar]
- 5. Srinivasan SR, Frontini MG, Xu J, Berenson GS. Utility of childhood non-high-density lipoprotein cholesterol levels in predicting adult dyslipidemia and other cardiovascular risks: the Bogalusa Heart Study. Pediatrics. 2006;118:201-206. [DOI] [PubMed] [Google Scholar]
- 6. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213-S256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Birken CS, Lebovic G, Anderson LN, et al. ; TARGet Kids! Collaboration. Association between vitamin D and circulating lipids in early childhood. PLoS One. 2015;10:e0131938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jorde R, Grimnes G. Vitamin D and metabolic health with special reference to the effect of vitamin D on serum lipids. Prog Lipid Res. 2011;50:303-312. [DOI] [PubMed] [Google Scholar]
- 9. Al Mheid I, Quyyumi AA. Vitamin D and cardiovascular disease: controversy unresolved. J Am Coll Cardiol. 2017;70:89-100. [DOI] [PubMed] [Google Scholar]
- 10. Brunzell JD, Davidson M, Furberg CD, et al. Lipoprotein management in patients with cardiometabolic risk: consensus conference report from the American Diabetes Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2008;51:1512-1524. [DOI] [PubMed] [Google Scholar]
- 11. Kinosian B, Glick H, Garland G. Cholesterol and coronary heart disease: predicting risks by levels and ratios. Ann Intern Med. 1994;121:641-647. [DOI] [PubMed] [Google Scholar]
- 12. Kastelein JJ, van der Steeg WA, Holme I, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation. 2008;117:3002-3009. [DOI] [PubMed] [Google Scholar]
- 13. Wen J, Zhong Y, Kuang C, Liao J, Chen Z, Yang Q. Lipoprotein ratios are better than conventional lipid parameters in predicting arterial stiffness in young men. J Clin Hypertens (Greenwich). 2017;19:771-776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hsia SH, Pan D, Berookim P, Lee ML. A population-based, cross-sectional comparison of lipid-related indexes for symptoms of atherosclerotic disease. Am J Cardiol. 2006;98:1047-1052. [DOI] [PubMed] [Google Scholar]
- 15. Frohlich J, Dobiásová M. Fractional esterification rate of cholesterol and ratio of triglycerides to HDL-cholesterol are powerful predictors of positive findings on coronary angiography. Clin Chem. 2003;49:1873-1880. [DOI] [PubMed] [Google Scholar]
- 16. Barzi F, Patel A, Woodward M; Asia Pacific Cohort Studies Collaboration. A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region. Ann Epidemiol. 2005;15:405-413. [DOI] [PubMed] [Google Scholar]
- 17. Holick MF, Binkley NC, Bischoff-Ferrari HA; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. [DOI] [PubMed] [Google Scholar]
- 18. Ponda MP, Huang X, Odeh MA, Breslow JL, Kaufman HW. Vitamin D may not improve lipid levels: a serial clinical laboratory data study. Circulation. 2012;126:270-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nwosu BU, Maranda L, Cullen K, Ciccarelli C, Lee MM. Vitamin D status is associated with early markers of cardiovascular disease in prepubertal children. J Pediatr Endocrinol Metab. 2013;26:1067-1075. [DOI] [PubMed] [Google Scholar]
- 20. Sriram S, Croghan I, Lteif A, Donelan-Dunlap B, Li Z, Kumar S. Relationship between 25(OH)D levels and circulating lipids in African American adolescents. J Pediatr Endocrinol Metab. 2016;29:1165-1172. [DOI] [PubMed] [Google Scholar]
- 21. Lee M, Ebert JR, Kadakia MP, Zhang J, Czerwinski SA. Inverse associations between cardiometabolic risk factors and 25-hydroxyvitamin D in obese American children and adolescents. Am J Hum Biol. 2016;28:736-742. [DOI] [PubMed] [Google Scholar]