Supplemental digital content is available in the text.
Key Words: PHYSICAL ACTIVITY, METs, SEDENTARY ACTIVITY, LIGHT ACTIVITY, MODERATE ACTIVITY, VIGOROUS ACTIVITY, CHILDREN, ENERGY COST
ABSTRACT
Purpose
A Youth Compendium of Physical Activities (Youth Compendium) was developed to estimate the energy costs of physical activities using data on youth only.
Methods
On the basis of a literature search and pooled data of energy expenditure measurements in youth, the energy costs of 196 activities were compiled in 16 activity categories to form a Youth Compendium of Physical Activities. To estimate the intensity of each activity, measured oxygen consumption (V˙O2) was divided by basal metabolic rate (Schofield age-, sex-, and mass-specific equations) to produce a youth MET (METy). A mixed linear model was developed for each activity category to impute missing values for age ranges with no observations for a specific activity.
Results
This Youth Compendium consists of METy values for 196 specific activities classified into 16 major categories for four age-groups, 6–9, 10–12, 13–15, and 16–18 yr. METy values in this Youth Compendium were measured (51%) or imputed (49%) from youth data.
Conclusion
This Youth Compendium of Physical Activities uses pediatric data exclusively, addresses the age dependency of METy, and imputes missing METy values and thus represents advancement in physical activity research and practice. This Youth Compendium will be a valuable resource for stakeholders interested in evaluating interventions, programs, and policies designed to assess and encourage physical activity in youth.
Physical activity is a major component of daily energy expenditure, and the most variable among young individuals. An understanding of its relationship to growth and development is of paramount importance to the health and well-being of children (1). Physical activity is a complex construct often classified qualitatively into major categories based on function (occupation, recreation, sports, locomotion, and self-care) or quantitatively based on intensity of effort (sedentary, light, moderate, and vigorous) (2). Knowing the intensity level of the physical activities in which youth participate can help researchers and practitioners understand patterns of physical activity and prescribe and encourage an amount of activity for optimal health.
Assessment of physical activity and estimation of its energy costs in children has many applications for clinical practice, public health, and applied research. Valid methodology is needed to assess compliance with physical activity guidelines and test effectiveness of programs and interventions. In epidemiologic studies and clinical practice, self-report questionnaires, direct observation, and monitoring devices are common tools to assess physical activity (3,4). In these approaches, reported or observed physical activity data are converted to energy expenditure using previously determined METs.
MET values are available from the adult compendium of physical activities (Adult Compendium) that classifies activities by function, specific type of activity, and intensity (5). METs are used to express the energy costs of physical activities as multiples of resting metabolic rate (RMR) (6). By convention, in adults, 1 MET is taken to be an oxygen uptake of 3.5 mL·kg−1·min−1 or 1 kcal·kg−1·h−1. The Adult Compendium has 21 major activity categories and 821 specific activities (6,7). In the Adult Compendium, 68% of the MET values are based on referenced measurements and the remainder on expert opinion.
Adult MET values, however, are not applicable to children (8–10). Children have higher basal metabolic rates (BMR) per unit body mass than adults that decline gradually as children grow and mature. Sex-specific developmental changes in organ weights, organ-specific metabolic rates, muscle mass, and adiposity differentially affect BMR and are responsible for the decline in BMR (11,12). BMR averages ~6.5 mL·kg−1·min−1 or 1.9 kcal·kg−1·min−1 in a typical 6-yr-old and approaches the adult value of 3.5 mL·kg−1·min−1 or 1 kcal·kg−1·min−1 in a typical 18-yr-old. Use of the standard adult MET equivalency would underestimate BMR of children.
Also, young children compared with adolescents or adults have disproportionately higher energy expenditure per unit body mass for physical activities. The energy cost of performing submaximal activities increases with age when expressed as kilocalories per minute but decreases with age when expressed relative to body mass (kcal·kg−1·min−1) (10). In addition to the developmental changes in body size and composition discussed above, children become more skilled and efficient at performing certain activities. Consequently, the energy costs of physical activities are not constant throughout childhood.
To address these problems, Ridley and colleagues (13) developed a compendium of energy expenditures for youth in 2008 (Ridley Compendium) that provided MET values for 244 activities, 38% of which were based on METs measured in children. The range of the number of data points used to assign an energy cost to an activity was 8 to 510. The remainder of the MET values was taken from the Adult Compendium (7), with the recommendation to multiply METs by child BMR when calculating total energy cost. Also, prediction equations for the energy costs of walking and running based on age and speed were provided. This was an important first step forward, especially in light of the available literature on youth energy expenditure at the time. However, the Ridley Compendium had several limitations: 1) small sample sizes in many studies, 2) a limited number of physical activities assessed, 3) only 19 pediatric published sources, and 4) a constant MET value for each activity provided for all children 5–17 yr old. As with the Adult Compendium, the Ridley Compendium had 1) limited ability to precisely estimate energy expenditure of individuals and 2) inherent errors for activities that can be performed at varying intensities.
To address these limitations, the Youth Energy Expenditure Workshop was convened by the Centers for Disease Control and Prevention, the National Cancer Institute, and the National Collaborative for Childhood Obesity Research on April 19–20, 2012, in Atlanta, GA. The Expert Panel agreed that an updated, expanded, and web-accessible compendium (named Youth Compendium of Physical Activities, henceforth called Youth Compendium) would be a valuable contribution to the field and that two tasks would be necessary to accomplish this objective. The first was to conduct a systematic literature review to locate studies published since 2007 (the latest date covered in the Ridley Compendium). This search would broaden the scope of the Ridley Compendium by widening the age range and expanding the databases used to search for relevant studies. The second task was to commission a workgroup of the Expert Panel to review and analyze existing data on the energy costs of physical activity in children.
The workgroup arrived at the conclusion that youth MET (METy) presented by age-groups was the preferred metric for presentation of the energy costs of physical activities in this Youth Compendium after a thorough evaluation of several options (9). Metrics of absolute oxygen uptake (mL·min−1), oxygen uptake per kilogram body mass (V˙O2 in mL·kg−1·min−1), net oxygen uptake (V˙O2, RMR), allometric scaled oxygen uptake (V˙O2 in mL·kg−0.75·min−1), and METy (V˙O2·[resting V˙O2]−1) were evaluated based on pooled data of 947 children ages 5 to 18 yr, who engaged in 14 different activities. No metric completely eliminated the influence of age, height, body mass, or sex for all 14 activities. Of the metrics examined, the METy displayed the least age dependency for sedentary and low-intensity activities. V˙O2ALLOMETRIC was the best for reducing age dependency for moderate-to-vigorous intensity activities. Although V˙O2ALLOMETRIC seemed to work well for ambulatory activities, it did not work as well for activities that require additional equipment or more skills such as playing basketball. V˙O2ALLOMETRIC coefficients are complex to calculate, and a different mass exponent may be required for each activity, making it challenging to directly compare activities. On the basis of these findings and considerations, the workgroup recommended the use of the METy.
Consistent with observations by Harrell et al. (14) and Trost et al. (15), the age dependency of METy values was a function of the type and intensity of the activity (9). METy values for sedentary and light-intensity standing activities were not statistically influenced by age. For moderate-to-vigorous activities, METy was positively correlated with age (r = 0.28 to 0.59). To account for the age dependency in this Youth Compendium, METy values are presented for short, discrete age-groups: 6–9, 10–12, 13–15, and 16–18 yr. The errors in using a constant METy value versus age-groups or specific ages were evaluated in a separate article by Pfeiffer et al. (16). The percent error reduction ranged from −0.2% to 21.7% for age-groups and from −0.23% to 18.2% for age in years compared with a constant METy value.
This article describes the development of a Youth Compendium, which presents the energy costs of 196 physical activities derived from pediatric data only, expressed in terms of METy for age categories 6–9, 10–12, 13–15, and 16–18 yr. This Youth Compendium, which will be housed on the National Collaborative for Childhood Obesity Research website at www.nccor.org/nccor-tools/youthcompendium, will be a valuable resource for researchers and practitioners interested in improving the health of children and adolescents through physical activity.
METHODS
Data sources for this Youth Compendium included:
Systematic reviews of the literature (Ridley 2013, 2016 at www.nccor.org/nccor-tools/youthcompendium): (a) energy costs of physical activities excluding walking and running in children from 90 studies and (b) energy costs of walking and running in children from 75 studies (some studies overlap)
Pooled data set: energy costs of physical activities, including walking and running derived from four publications (14,17–19)
2016 JPAH supplement: energy costs of physical activities in children, including walking and running from 12 studies (20)
In these three data sources, BMR was predicted using age-, sex-, and mass-specific Schofield equations (21) for calculation of METy values. Schofield equations (21) were based on 2060 children, ages 3–18 yr, from 44 published studies. Experimental conditions used for study inclusion stipulated true basal metabolism: 1) absence of gross muscular activity, 2) ≥12-h post absorptive state, 3) thermoneutrality, 4) emotional repose, and 5) stable nutritional status. No departure from goodness of fit was found when the equations were tested on a validation data set. For ages 3–18 yr, height did not contribute significantly to BMR, once weight had been taken into account.
The Schofield equations for boys, ages 3–10 and 10–18 yr, are as follow:
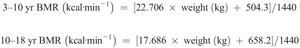
The Schofield equations for girls, ages 3–10 and 10–18 yr, are as follows:
The development of this Youth Compendium involved five steps 1) classification of the physical activities into 16 major categories, 2) profile plots constructed for 16 major categories, 3) multiple imputation of missing METy values, 4) review of the observed and imputed METy values, 5) smoothing observed and imputed METy values, and 6) development of a coding scheme for this Youth Compendium.
Data Sources
Systematic reviews of the literature
Ridley and colleagues conducted two systematic literature reviews of the energy cost of physical activities in children (www.nccor.org/nccor-tools/youthcompendium). Study eligibility criteria included the following: full-text article, thesis/dissertation, or data provided from authors from a published conference abstract; data on children and adolescents; energy cost/expenditure of specific physical activities measured; energy cost/expenditure of walking and running measured at specific set speeds; and energy cost data measured using indirect calorimetry or direct calorimetry. Study exclusion criteria were systematic reviews or meta-analysis and participant enrollment based on illness, except overweight and obesity. If studies compared a control of healthy participants with a sample based on a specific pathology, data were extracted for the control sample only. The aim of the first search, completed in 2013, was to locate pediatric studies where the energy cost of specific physical activities excluding walking and running was measured. The aim of the second search, completed in 2016, was to locate pediatric studies where the energy cost of walking and running at selected speeds was measured. The following databases were searched: CINAHL, Cochrane library, EMBASE, Medline, Proquest, PsychINFO, SCOPUS, SportDiscus, and Web of Science. Where multiple metrics were provided for the energy cost of the activity, the following hierarchy was used to extract data: 1) V˙O2, 2) energy expenditure (kJ), 3) energy expenditure (kcal), and 4) METy calculated using the child’s BMR. Where possible, energy cost data not provided as V˙O2 (mL·kg−1·min−1) were converted to this base metric for comparative purposes. Data not provided per unit mass were converted using the mean mass provided. Data presented in kcals were first converted to kilojoules using the conversion factor of 1 kcal = 4.18 kJ and then converted to V˙O2 using a standard energy equivalent for oxygen uptake (20.9 kJ·L−1 O2). The METy cost was calculated by dividing the measured energy cost by the estimated mean BMR calculated using the age-, sex-, and mass-specific Schofield prediction equations (21). The extracted data set contained sampling schemes, methodology, and mean data for participant descriptive variables (sample size, age, weight, and height) and energy costs of the activity (see Table, Supplemental Digital Content 1, Activity-specific references for METy values, http://links.lww.com/MSS/B54).
Pooled data set
To supplement the literature review, METy values for specific activities were compiled from a pooled data set of energy costs of physical activities in 933 children, ages 5 to 18 yr (9). On the basis of participant characteristics (age, sex, and body mass) and activity-related oxygen uptake (mL O2·min−1), BMR was estimated by the Schofield prediction equation (21) and used to compute METy values. Studies by Crouter et al. (19), Trost et al. (17), and Harrell et al. (14) were located in the Ridley literature reviews; it should be noted, however, that METy values from these studies were not duplicated in this Youth Compendium.
2016 JPAH supplement
Energy costs of physical activities were extracted from recent publications in JPAH (22–33). BMR was estimated by the Schofield prediction equation (21) and used to compute METy values. Data from Ridley et al. (34) were included in the 2013 literature review, and the study by Trost et al. (15) was included in the pooled data set and therefore not duplicated in this Youth Compendium.
Development of this Youth Compendium
Step 1: classification of the physical activities into 16 major categories
Specific activities from the literature review, the pooled data set, and the JPAH supplement were classified into 16 major categories taking into consideration body position (sitting, standing, and lying down), upper or lower body movement, locomotion, weight or non-weight bearing, and intensity of effort. Because of the differences in child development and age dependency of METy (9), the observations were then classified into one of four a priori–defined age-groups, 6–9, 10–12, 13–15, and 16–18 yr, based on the study mean age (median age when the mean was not provided).
Step 2: profile plots constructed for 16 major categories
Age-group-specific mean METy values were calculated for each specific activity. Profile plots were constructed for each of the 16 activity categories to show the missing data pattern for the different activities within the category. For the profile plots, each specific activity in a category was treated as a single observation, which meant one line per activity in each plot. In addition, the percent of missing observations was calculated for each activity category within each age-group.
Step 3: multiple imputation of missing METy values
Multiple imputation of missing METy values was performed to maximize the utility and comprehensiveness of the Youth Compendium by providing METy values across all age-groups for each activity. First, linear and quadratic regression models were computed to study the structure of the relationship between age and METy cost for each activity with a sufficient number of observations using Proc GLM in SAS. Adjusted R2 was used to compare the fits of the linear and quadratic models to determine which model should be used to impute METy cost in age ranges without observations. The linear component was significant for all specific activities, and therefore the linear not the quadratic term was used in the imputations.
Next, a multiple imputation mixed model was used to impute missing values for age ranges in which there were no observations for a given activity. To take advantage of similar types of movement, a mixed model was used to properly account for the clustering in the data by specific activity within each activity category. The mixed model “borrowed” data from similar activities within a major category allowing for imputation of activities that had fewer observations. A previously published macro was used to perform the multiple imputation (35). A different imputation model was fit for each activity category to predict METy values from a linear age term and included random intercepts for the different activities in a category. Each missing value was imputed 20 times. The midpoint of each age range was used to calculate the imputed values. After the imputed values were generated, they were bounded with a lower bound of 1 and an upper bound of 3 SD above the mean for the category. These bounds replaced any imputed values that were outside the predetermined range (1.1% of imputed METy values were below 1.0 and 0.8% were above 3 SD, with no apparent clustering). Both the upper and the lower bound adjustments took place after all imputations were performed, meaning that no imputations were skipped. Any abnormal imputed value that was changed was flagged in the imputed data set.
Step 4: review of the observed and imputed METy values
From the completed data set, a table of the average METy values of each activity for each age-group was generated, showing both observed and imputed values. Profile plots for each major activity category were created using the mean observed and imputed values. The table and plots of the average METy values were reviewed for consistency among activities within the major activity categories and across age-groups within each specific activity. Similar to the criterion for the imputed values, outlying values were defined as values 3 SD above or below the mean for the category or contrary trends across age-groups. A total of 4.6% of the mean METy values were replaced by linear regression based on the age coefficient from the mixed model.
Step 5: smoothing observed and imputed METy values
To smooth the observed and imputed METy values, mixed models for each of the major activity categories were conducted from the completed data set to obtain model-based parameter estimates predicting METy from age treated as a continuous variable. The activity- and age-group-specific METy values were predicted using the fixed and random coefficients for the intercept and slope at the midpoint for each of the age-groups. Profile plots for each major activity category were created using the model-based values. Similar to adjustments of the age-specific observed and imputed mean METy values, approximately 6% of model-based METy values were adjusted to be consistent within the major activity categories and across age-groups within each specific activity.
Step 6: development of a coding scheme for the Youth Compendium
To facilitate data coding, a six-digit coding scheme was developed for METy values in this Youth Compendium. In the coding scheme, the first two digits (1–16) represent the major activity category, the next three digits represent the specific activity, and the last digit represents the age-group (1, reserved for 2–5 yr; 2, for 6–9 yr; 3, for 10–12 yr; 4, for 13–15 yr; and 5, for 16–18 yr). In Tables 1–4, the age-group is designated by the placeholder X. For example, the activity codes for Aerobic Dance are 601002, 601003, 601004, and 601005 for the age-groups 6–9, 10–12, 13–15, and 16–18 yr, respectively. The corresponding METy values are 3.3, 3.8, 4.8, and 4.0.
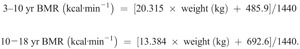
TABLE 1.
Model-based METy values for activities while lying and sitting for the Youth Compendium of Physical Activities.
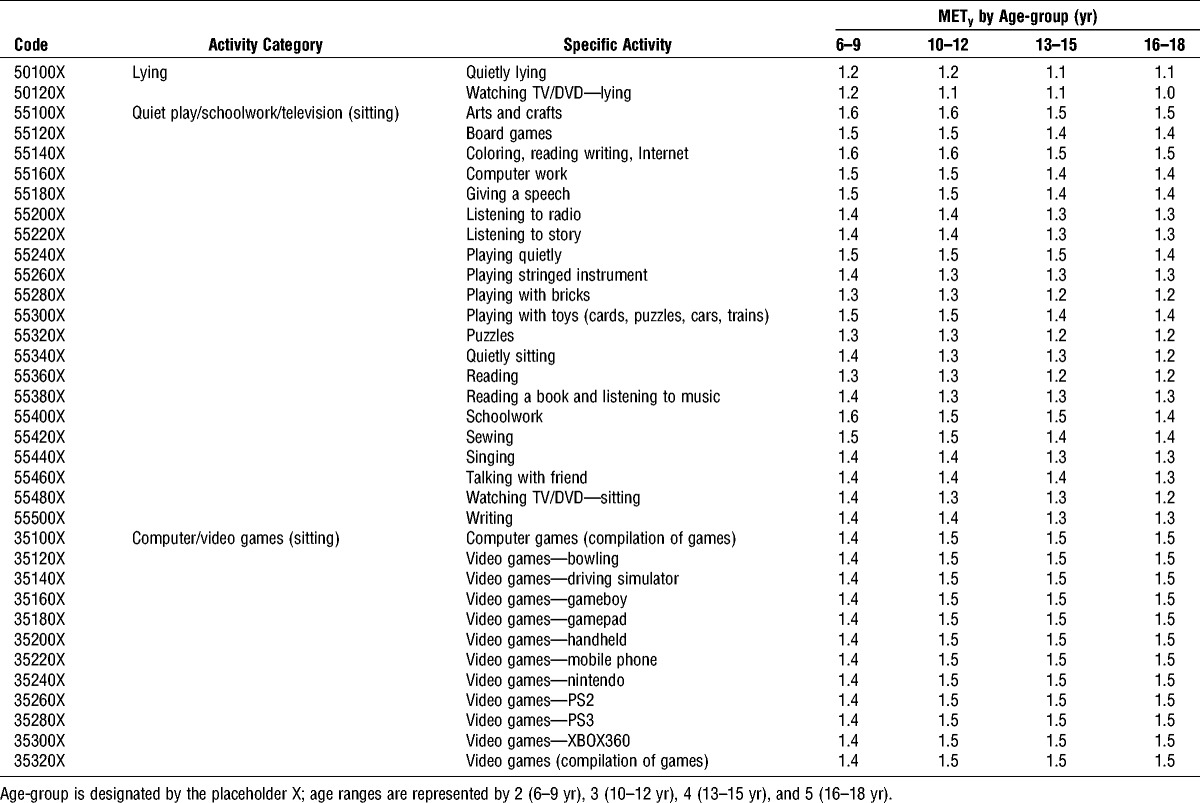
TABLE 4.
Model-based METy for walking and running activities for the Youth Compendium of Physical Activities.
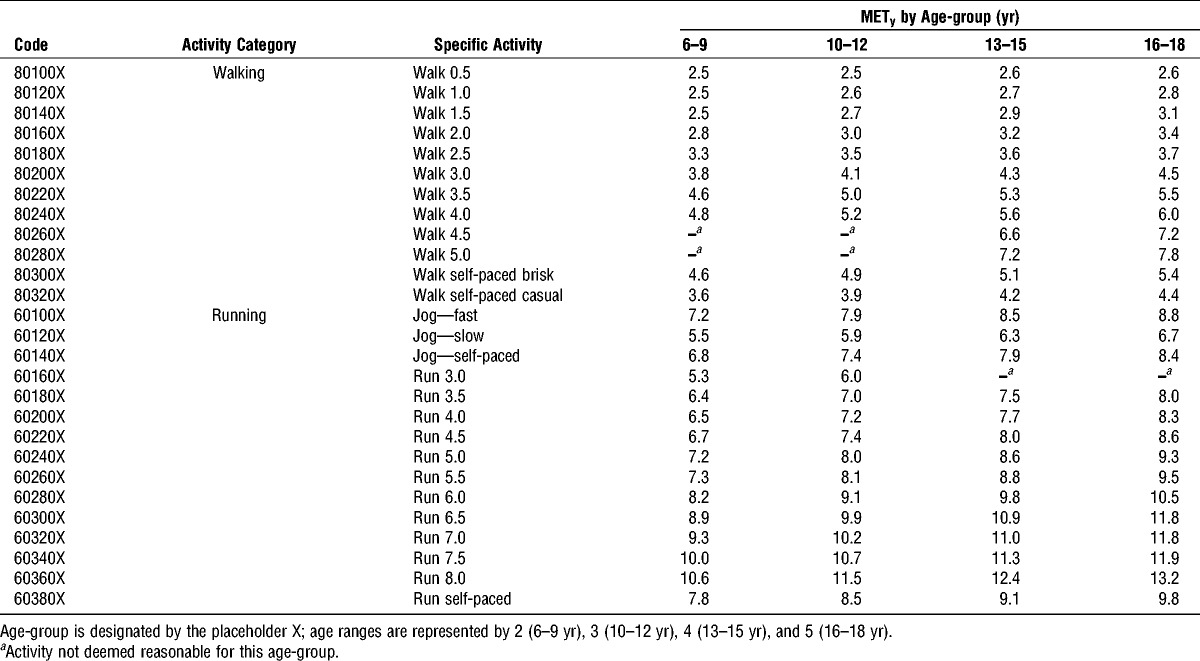
TABLE 2.
Model-based METy for activities while standing, doing housework, and playing active video games for the Youth Compendium of Physical Activities.
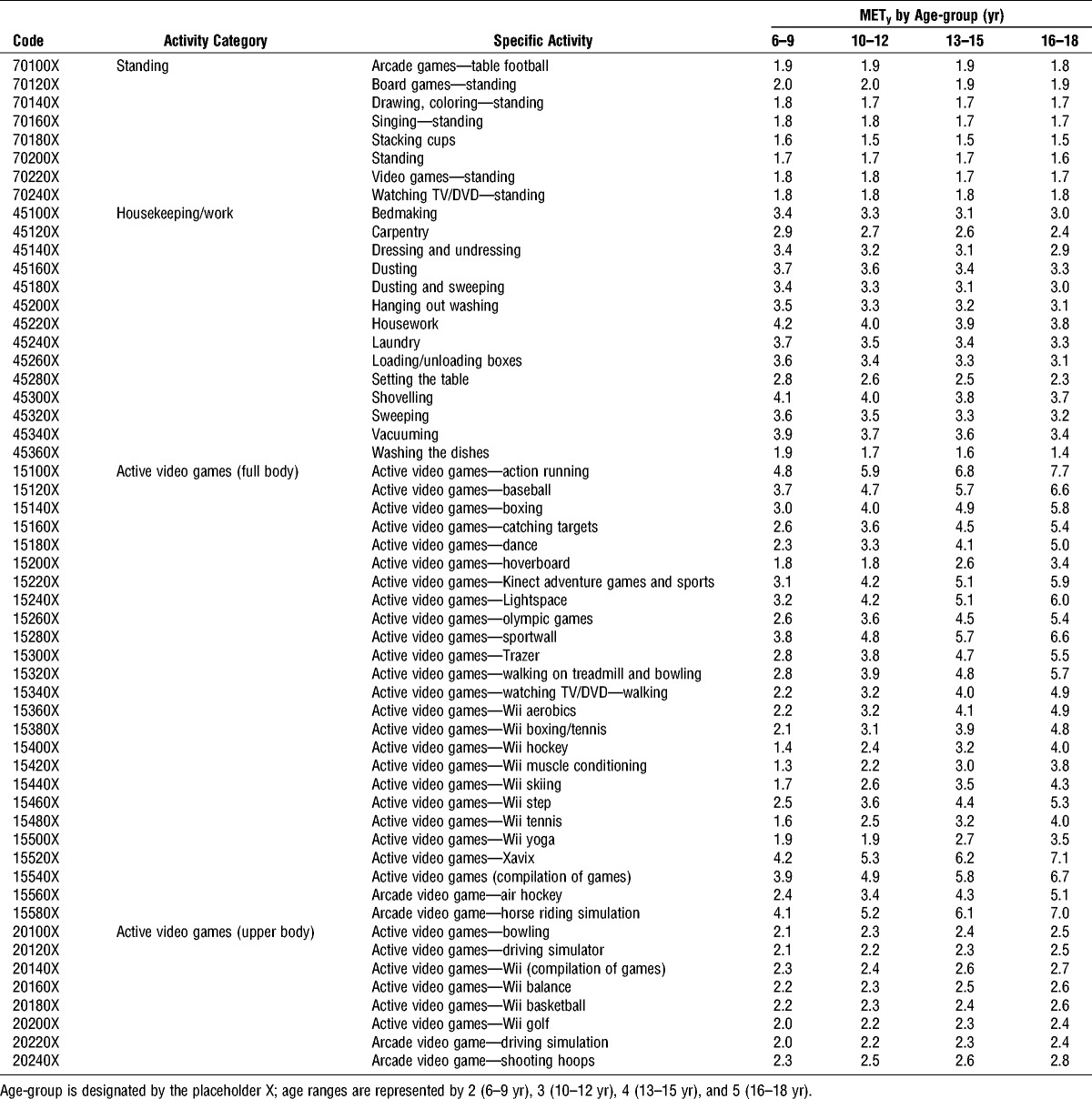
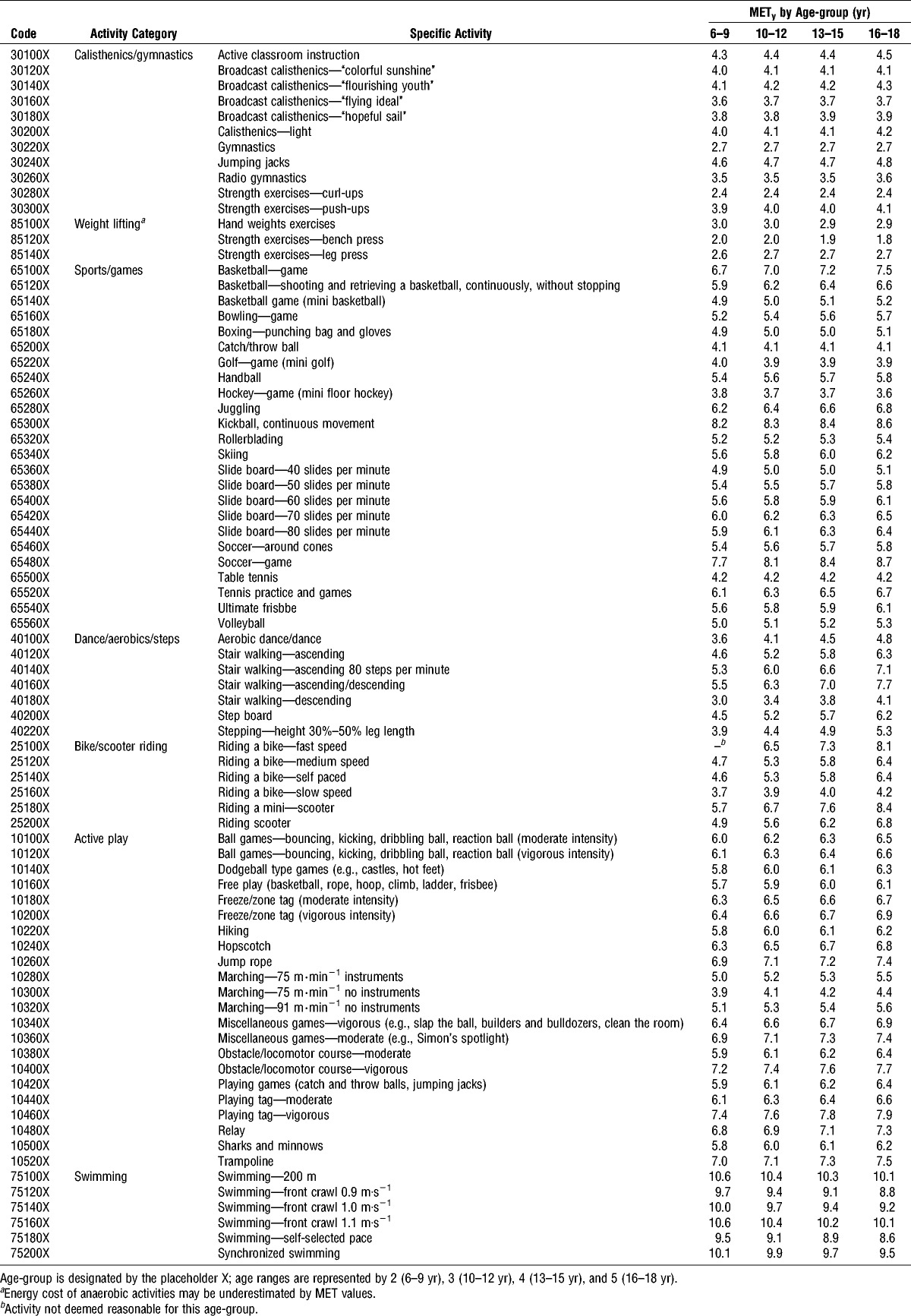
TABLE 3.
Model-based METy for play and sports activities for the Youth Compendium of Physical Activities.
RESULTS
In total, energy costs of 196 physical activities were extracted from 137 pediatric studies representing more than 37,000 observations on children, 11.5 ± 2.6 yr old, with mean weight 44.8 ± 14.4 kg and height 146.1 ± 21.6 cm (see Table, Supplemental Digital Content 1, Activity-specific references for METy values, http://links.lww.com/MSS/B54). The literature review yielded energy cost values for 121 specific activities for children 6 yr and older, excluding walking and running. The pooled data set of 36 activities provided mean energy cost data of 14 additional activities and the JPAH supplement data of 78 activities provided mean energy costs of 34 additional activities. For walking and running activities, the mean energy costs of walking (12 levels) and running (15 levels) at various speeds available from all three sources were grouped by 0.5 mph increments (walking, 0.5–5.0 mph; running, 3.0–8.0 mph) where available. When speed was not provided, walking and running activities were classified by effort (e.g., slow, fast, and self-paced).
The 196 specific activities were classified into 16 major categories. Most sports games were simulated and self-paced, in the sense that they were modified games imitating the typical movement patterns of the game (i.e., dribbling a soccer ball through cones to simulate movements in a soccer game). The Computer/Video Games (sitting) category reflected sedentary behaviors such as computer games, mobile phone games, Nintendo, and PS2 and 3, which do not require children to stand or do much movement other than moving a joystick or pushing controls with hands or fingers. For the active video games, the children performed some sort of movement, whether it was standing and imitating a sport such as swinging a tennis racket or performing a dance movement. The energy costs for active video games varied substantially and therefore were split into active video games (full body) and active video games (upper body) to distinguish the energy costs.
Youth Compendium database resulted in 397 observed mean METy values (51%) and 380 imputed mean METy values (49%) in the four age-groups for 196 specific activities (see Table, Supplemental Digital Content 2, Table of observed and imputed METy values by activity and age-group, http://links.lww.com/MSS/B55). The imputed and observed METy values for the specific activities within each major category were graphically examined to identify inconsistencies (see Figure, Supplemental Digital Content 3, Activity-specific METy values by age-groups for each major activity category, http://links.lww.com/MSS/B56).
The final model-based METy values in the four age-groups for 196 specific activities are presented in Tables 1–4 and as a supplemental file (see Table, Supplemental Digital Content 4. Table of model-based METy values by activity and age-group, http://links.lww.com/MSS/B57). The tables display the activity code, major activity category, specific activity, and model-based METy values for the four age-groups. The model-based METy values are graphically illustrated for the specific activities within four of the major categories (Fig. 1). Figure 1 shows that the METy values for quiet play/schoolwork/television and housekeeping/work that are independent of age, in contrast to dance/aerobics/steps and running, where the age dependency for METy values and wider range of METy intensities are evident. In general, the METy values of the more sedentary activities were similar across age-groups, and the METy values of the more intense activities increased with age.
FIGURE 1.
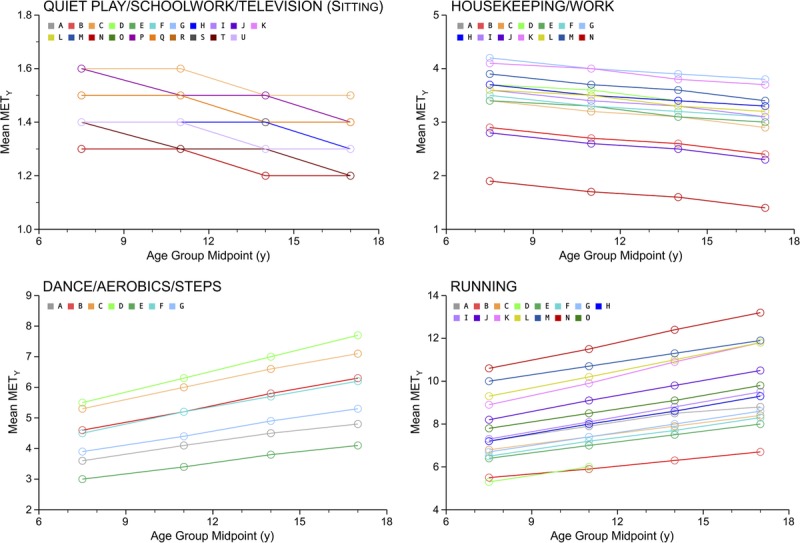
METy values are plotted by age-groups—midpoint (y) for the following activity categories: quiet play/schoolwork/television (sitting), including the specific activities: A = arts and crafts; B = board games; C = coloring, reading, writing, Internet; D = computer work; E = giving a speech; F = listening to radio; G = listening to story; H = playing quietly; I = playing stringed instrument; J = playing with bricks; K = playing with toys (cards, puzzles, cars, trains); L = puzzles; M = quietly sitting; N = reading; O = reading a book and listening to music; P = schoolwork; Q = sewing; R = singing; S = talking with friend; T = watching TV/DVD; U = writing; housekeeping/work, including the specific activities: A = bed making; B = carpentry; C = dressing and undressing; D = dusting; E = dusting and sweeping; F = hanging out washing; G = housework; H = laundry; I = loading/unloading; j = setting the table; J = setting the table; K = shoveling; L = sweeping; M = vacuuming; N = washing the dishes; Dance/Aerobics/Step, including the specific activities: A = aerobic dance/dance; B = stair walking-ascending; C = stair walking—ascending 80 steps per minute; D = stair walking—ascending/descending; E = stair walking—descending; F = step board; G = stepping—height 30%–50% leg length; Running, including the specific activities: A = jog-fast; B = jog-slow; C = jog self-paced; D = run 3.0 mph; E = run 3.5 mph; F = run 4.0 mph; G = run 4.5 mph; H = run 5.0 mph; I = run 5.5 mph; J = run 6.0 mph; K = run 6.5 mph; L = run 7.0 mph; M = run 7.5 mph; N = run 8.0 mph; O = run self-paced.
An estimate of the energy cost of a physical activity can be computed based on the METy value from the Youth Compendium, a measured or computed BMR, and duration of the specific activity, as follows:

where the BMR for boys and girls is predicted using age-, sex-, and mass-specific Schofield equations (21).
DISCUSSION
This article describes a Youth Compendium of Physical Activities based completely on empirical energy expenditure measurements in children. This Youth Compendium consists of METy values for 196 specific activities classified into 16 major categories for four age-groups: 6–9, 10–12, 13–15, and 16–18 yr. The methods used in formulating this Youth Compendium sought to address the unique developmental challenges in determining the energy costs of physical activities in children. First, all METy values were measured or derived from pediatric data only. Second, missing METy data were predicted using a specific imputation mixed model for each major activity category. Third, METy values for each activity were provided for the four age-groups to address the age dependency of METy values (9).
Past studies have shown that the age dependency of METy values is a function of the type and intensity of the activity. In our study, the METy values for sedentary and light-intensity standing activities were not appreciably influenced by age, whereas for moderate-to-vigorous activities, METy values were positively correlated with age (9). These observations were reinforced by the profile plots of this Youth Compendium, which showed consistent overall trends within major activity categories. In general, the low-intensity categories display no slope, and the higher intensity categories a positive slope across age-groups.
The energy costs of many specific activities were not available from the literature search for all age-groups. Therefore, we used a specific multiple imputation mixed model for each major activity category to fill-in missing data, resulting in 49% of the METy values in the database. This approach maximized the use of all the data and simultaneously considered linear trends across age-groups and patterns within age-groups for similar activities. Presentation of the imputed values in the Supplemental Digital Content allowed for identification of gaps in the literature that may be filled with future research on the energy costs of physical activities in youth.
In the compilation and profile plots of the measured and imputed data on the energy cost of physical activities, variability within specific activities was evident. Variability in the measured values across physical activities and age-groups can be attributed to different study designs, participant characteristics, procedures and equipment among studies, developmental changes in body size and composition, age-dependent levels of skill and efficiency, and participant self-selected pace and effort for uncontrolled activities. Some activities were controlled (e.g., walking and running at set speeds on a treadmill), whereas others were performed at self-selected intensities. These volitional activities would be expected to have greater variation in METy values among children because of differences in 1) the fitness level of the child, 2) the child’s perceptions of intensity, 3) the child’s motivation, 4) previous experience with the activity, and 5) experimental conditions and instructions given.
To reconcile the irregularities in METy values within the major activity categories and across age-groups within each specific activity, the observed and imputed values were smoothed producing more physiologically consistent METy values. Although these values may be refined and expanded with future research, they currently represent the best estimates of the energy costs of physical activities in youth.
The comprehensive tables of model-based METy values can serve as a valuable resource for estimating energy costs of physical activities in research and clinical studies from self-report questionnaires, direct observation, and monitoring devices. This Youth Compendium also may assist in assessing physical activity guidelines such as the 2008 Physical Activity Guidelines for Americans (www.health.gov/paguidelines) and estimating physical activity levels for applications that estimate energy requirements of children such as Choose My Plate (https://www.choosemyplate.gov/) or Dietary Reference Intakes (https://www.nal.usda.gov/fnic/dietary-reference-intakes). Because application of METy values requires tailoring to the child’s BMR computed based on age, sex, and body weight, the METy values presented here can be applied to a wide range of children and adolescents, thus making them generalizable to healthy pediatric populations, ages 6 to 18 yr.
Caveats of this Youth Compendium are not unlike the limitations acknowledged for the Ridley Compendium (13) and the Adult Compendium (5–7). In all cases, the MET values are averages and, therefore, do not reflect individual variability due to body composition, fitness, effort, mechanical efficiency, or environmental conditions under which the activity is performed. Some activities in this Youth Compendium can be performed at varying intensities and therefore are inherently more variable than prescribed activities such as walking and running at set speeds. METy values will be more accurate at the group than the individual level. In cases where individual estimation is desired, users should realize that energy expenditure can be influenced by many factors not captured by the mean METy values presented here. Users should appreciate that these values are estimates and are not recommended to be used for precise estimation of energy balance.
In calculating METy values, the denominator BMR is computed based on age, sex, and body weight. Although incorporation of BMR greatly reduces the weight dependency, METy values are not completely independent of body weight, especially for locomotive activities. Average METy values can underestimate energy costs in children with obesity and overestimate them in children with underweight (36). Factors such as body composition, body shape, cross-sectional area of the primary muscles, leg length, and efficiency of body movement may influence the relationship of energy expenditure to body weight (9). For this Youth Compendium, data were not excluded on the basis of weight status. In fact, many studies did not provide information on the BMI status of their participants. Therefore, the average METy values in this Youth Compendium are applicable to all healthy children with the caveat that overestimation or underestimation of energy costs of some activities may occur with subgroups of children based on BMI status.
The breadth of child and adolescent activities in this Youth Compendium is incomplete. The majority of METy values were measured in mid-childhood, and therefore more data are needed in very young children and older adolescents. The energy costs of specific activities such as transport, gardening, and certain sports (e.g., kayaking, sailing, ice skating, skateboarding, water polo, horseback riding, martial arts, lacrosse, rugby, rock climbing, and softball) are not available. Particularly lacking in the current Youth Compendium are METy values for occupational work, self-care, and lawn and garden activities. We envisage this Youth Compendium will be updated and refined over time as more measured values are published. Future research efforts could solicit certain types of activities in specific age-groups to fill the gaps. In addition, this Youth Compendium is not applicable to children with illnesses or disabilities that alter movement or mechanical efficiency and thereby the energy cost of activities. Research is needed to fill the paucity of energy expenditure data in special populations.
In conclusion, this Youth Compendium of Physical Activities presents METy values for 196 activities across four age-groups: 6–9, 10–12, 13–15, and 16–18 yr. The new Youth Compendium can be used to standardize the scoring and interpretation of youth physical activity data in research and public health surveillance applications. It will be a valuable resource to standardize the scoring and interpretation of youth physical activity data in research and public health surveillance applications.
Supplementary Material
Acknowledgments
The Working Group on Youth Energy Expenditure consists of Barbara Ainsworth, Ph.D., M.P.H. (Arizona State University); David Bassett, Ph.D. (University of Tennessee); David Berrigan, Ph.D. (NCI); Nancy Butte, Ph.D. (Baylor College of Medicine); Scott Crouter, Ph.D. (University of Tennessee); Janet Fulton, Ph.D. (CDC); Stephen Herrmann, Ph.D. (Sanford Health/Research); Kate Ridley, Ph.D. (Flinders University, Australia); Robert McMurray, Ph.D. (University of North Carolina); Karin Pfeiffer, Ph.D. (Michigan State University); Stewart Trost, Ph.D. (Queensland University of Technology); and Kathleen Watson, Ph.D. (CDC).
The authors acknowledge the valuable contributions of those who attended the initial Youth Energy Expenditure Workshop: Bridget Borgogna (CDC); David Brown, Ph.D. (CDC); Susan Carlson, Ph.D. (CDC); Dianna Carroll, Ph.D. (CDC); Kong Chen, Ph.D. (NIDDK); Joan Dorn, Ph.D. (CDC); Ginny Frederick, M.S. (CDC Foundation); Deb Galuska, Ph.D. (CDC); Carmen Harris, M.P.H. (CDC); Kristin lssacs, Ph.D. (US Environmental Protection Agency); Sarah Lee, Ph.D. (CDC); Robert Malina, Ph.D. (Tarleton State University); Mindy Millard-Stafford, Ph.D. (Georgia Institute of Technology); Don Morgan, Ph.D. (Middle Tennessee State University); Chantelle Owens, MS (CDC); Prabasaj Paul, Ph.D. (CDC); Russell R. Pate (University of South Carolina); Anne Rodgers (Science Writer); Tom Rowland, MD (Baystate Children’s Hospital); MinKyoung Song, Ph.D. (CDC); Andrea Torres, M.P.H. (CDC). In addition, we thank Natasha Schranz, Ph.D.; Gavin Tempest, Ph.D.; Sam Chalmers, Ph.D.; David Bentley, Ph.D.; Reegan Knowles; Kyle Sprow; and Penny Randal-Levy for excellent assistance with the literature review.
This project has been funded by the National Cancer Institute (NCI), the Office of Disease Prevention, Centers for Disease Control and Prevention (CDC), and the National Collaborative on Childhood Obesity Research (NCCOR)—a public–private partnership among NCI, CDC, the Robert Wood Johnson Foundation (RWJF), and the U.S. Department of Agriculture. This project also has been funded with federal funds from the U.S. Department of Agriculture (USDA)/Agricultural Research Service (ARS) under Cooperative Agreement No. 58-6250-0-008.
None of the authors has conflicts or potential conflicts of interest, including relevant financial interests, activities, relationships, and affiliations related to this research. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
The results of the present study do not constitute endorsement by the American College of Sports Medicine. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC. The contents of this publication do not necessarily reflect the views or policies of the USDA, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.acsm-msse.org).
REFERENCES
- 1.U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 2.Butte NF, Ekelund U, Westerterp KR. Assessing physical activity using wearable monitors: measures of physical activity. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S5–12. [DOI] [PubMed] [Google Scholar]
- 3.Dollman J, Okely AD, Hardy L, Timperio A, Salmon J, Hills AP. A hitchhiker’s guide to assessing young people’s physical activity: deciding what method to use. J Sci Med Sport. 2009;12(5):518–25. [DOI] [PubMed] [Google Scholar]
- 4.Montoye HJ, Kemper HCG, Saris WHM, Washburn RA. Measuring Physical Activity and Energy Expenditure. Champaign, IL: Human Kinetics; 1996. pp. 1–191. [Google Scholar]
- 5.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80. [DOI] [PubMed] [Google Scholar]
- 6.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81. [DOI] [PubMed] [Google Scholar]
- 7.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. [DOI] [PubMed] [Google Scholar]
- 8.Torun B. Energy cost of various physical activities in healthy children. In: Schürch B, Scrimshaw NS, eds. Activity, Energy Expenditure and Energy Requirements of Infants and Children. Lausanne: International Dietary Energy Consultancy Group; 1990. pp. 139–83. [Google Scholar]
- 9.McMurray RG, Butte NF, Crouter SE, et al. Exploring metrics to express energy expenditure of physical activity in youth. PLoS One. 2015;10(6):e0130869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rowland TW. Children’s Exercise Physiology. Champaign, IL: Human Kinetics; 2005. pp. 80–4. [Google Scholar]
- 11.Gallagher D, Belmonte D, Deurenberg P, et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol. 1998;275:E249–58. [DOI] [PubMed] [Google Scholar]
- 12.Muller MJ, Bosy-Westphal A, Kutzner D, Heller M. Metabolically active components of fat-free mass and resting energy expenditure in humans: recent lessons from imaging technologies. Obes Rev. 2002;3(2):113–22. [DOI] [PubMed] [Google Scholar]
- 13.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. Int J Behav Nutr Phys Act. 2008;5:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrell JS, McMurray RG, Baggett CD, Pennell ML, Pearce PF, Bangdiwala SI. Energy costs of physical activities in children and adolescents. Med Sci Sports Exerc. 2005;37(2):329–36. [DOI] [PubMed] [Google Scholar]
- 15.Trost SG, Drovandi CC, Pfeiffer K. Developmental trends in the energy cost of physical activities performed by youth. J Phys Act Health. 2016;13:S35–40. [DOI] [PubMed] [Google Scholar]
- 16.Pfeiffer KA, Watson KB, McMurray RG, et al. Energy cost expression for a Youth Compendium of Physical Activities: rationale for using age groups. Pediatr Exerc Sci. 2017;8:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–8. [DOI] [PubMed] [Google Scholar]
- 18.Butte NF, Wong WW, Adolph AL, Puyau MR, Vohra FA, Zakeri IF. Validation of cross-sectional time series and multivariate adaptive regression splines models for the prediction of energy expenditure in children and adolescents using doubly labeled water. J Nutr. 2010;140(8):1516–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crouter SE, Horton M, Bassett DR., Jr Validity of ActiGraph child-specific equations during various physical activities. Med Sci Sports Exerc. 2013;45(7):1403–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrmann SD, Pfeiffer KA. New data for an updated Youth Energy Expenditure Compendium. J Phys Act Health. 2016;13:S1–83. [DOI] [PubMed] [Google Scholar]
- 21.Schofield WN, Schofield C, James WPT. Basal metabolic rate—review and prediction, together with an annotated bibliography of source material. Hum Nutr Clin Nutr. 1985;39C:1–96. [PubMed] [Google Scholar]
- 22.Barkman J, Pfeiffer K, Diltz A, Peng W. Examining energy expenditure in youth using XBOX Kinect: differences by player mode. J Phys Act Health. 2016;13:S41–3. [DOI] [PubMed] [Google Scholar]
- 23.Clevenger KA, Aubrey AJ, Moore RW, et al. Energy cost of children’s structured and unstructured games. J Phys Act Health. 2016;13:S44–7. [DOI] [PubMed] [Google Scholar]
- 24.Gao Y, Sun H, Zhuang J, et al. Metabolic equivalents of selected sedentary and physical activities in chinese youth. J Phys Act Health. 2016;13:S48–52. [DOI] [PubMed] [Google Scholar]
- 25.Honas JJ, Willis EA, Herrmann SD, Greene JL, Washburn RA, Donnelly JE. Energy expenditure and Intensity of classroom physical activity in elementary school children. J Phys Act Health. 2016;13:S53–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Innerd AL, Azevedo LB. The energy expenditure of free-living physical activities in primary schoolchildren. J Phys Act Health. 2016;13:S57–61. [DOI] [PubMed] [Google Scholar]
- 27.Mackintosh KA, Ridley K, Stratton G, Ridgers ND. Energy cost of free-play activities in 10- to 11-year-old children. J Phys Act Health. 2016;13:S71–4. [DOI] [PubMed] [Google Scholar]
- 28.Ondrak KS, McMurray RG. Comparison of energy expenditure of youth playing tennis during practice and match settings. J Phys Act Health. 2016;13:S21–3. [DOI] [PubMed] [Google Scholar]
- 29.Sasaki JE, Howe C, John D, et al. Energy expenditure for 70 activities in children and adolescents. J Phys Act Health. 2016;13:S24–8. [DOI] [PubMed] [Google Scholar]
- 30.Schuna JM, Jr, Barreria TV, Hsia DS, Johnson WD, Tudor-Locke C. Youth energy expenditure during common free-living activities and treadmill walking. J Phys Act Health. 2016;13:S29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lau M, Wang L, Acra S, Buchowski MS. Energy expenditure of common sedentary activities in youth. J Phys Act Health. 2016;13:S17–20. [DOI] [PubMed] [Google Scholar]
- 32.Lee JE, Stodden DF, Gao Z. Young children’s energy expenditure and moderate-to-vigorous physical activity on weekdays and weekends. J Phys Act Health. 2016;13(9):1013–6. [DOI] [PubMed] [Google Scholar]
- 33.van Loo CM, Okely AD, Batterham M, et al. Predictive validity of a thigh-worn accelerometer METs algorithm in 5- to 12-year-old children. J Phys Act Health 2016;13:S78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ridley K, Olds T. The energy cost of household chores, rollerblading, and riding scooters in 9- to 14-year-old children. J Phys Act Health. 2016;13:S75–7. [DOI] [PubMed] [Google Scholar]
- 35.Mistler, Stephen A. A SAS macro for applying multiple imputation to multilevel data. Paper 438. 2013. San Francisco (CA): Proceedings of the SAS Global Forum. 4-28-0013.
- 36.Spadano JL, Must A, Bandini LG, Dallal GE, Dietz WH. Energy cost of physical activities in 12-y-old girls: MET values and the influence of body weight. Int J Obes Relat Metab Disord. 2003;27(12):1528–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


