Abstract
Accessory ossicles are developmental variants which are often asymptomatic. When incidentally picked up on imaging, they are often inconsequential and rarely a cause for concern. However, they may cause pain or discomfort due to trauma, altered stress, and over-activity. Nuclear scintigraphy may play a role in the diagnosis and localizing pain generators. 18F-Sodium Fluoride (NaF) is a PET imaging agent used in bone imaging. Although commonly used in imaging patients with cancer imaging malignancy, 18F-NaF may be useful in the evaluation of benign bone and joint conditions. In this article, we would like to present a spectrum of clinical cases and review the potential diagnostic utility of 18F-NaF in the assessment of symptomatic accessory ossicles in patients referred for staging cancers.
Keywords: 18F-NaF PET/CT, accessory ossicles, hybrid imaging
Introduction
Bone and joint pain is a common presentation in both primary and secondary practice. First line investigation is commonly plain radiograph which allows for detection of fractures, and soft tissue swelling to a lesser extent. Often, small fragments of ossification may be mistaken for fractures on plain radiograph, altering patient management erroneously [1].
Ossification refers to the process of bone formation or remodeling. Bones in the human body start ossification in about the third month of fetal life into late adolescence. The process is started by osteoblasts in areas known as primary centers of ossification and is normally completed in our mid-20s. Long bones can have secondary ossification centers in the epiphysis, where it fuses with the metaphysis. Occasionally, extra bones can be formed from an unfused primary or secondary ossification centers. They often develop to be small, well-corticated structures close to a joint. They are common developmental variants which are often asymptomatic, and their function is not fully understood [1,2].
Accessory ossicles are developmental variants which are often asymptomatic. When incidentally picked up on imaging, they are often inconsequential, and rarely a cause for concern. They can occur in many areas, with almost forty variations identified in the feet alone. Prevalence is variable depending on the area of involvement. They may be mistaken for fractures on plain radiographs, which could alter patient management. While most of them are asymptomatic, they have potential to cause discomfort or pain if involved in trauma, infection or degeneration. However, they may cause pain or discomfort due to trauma and over activity. When picked up in the asymptomatic patient on the radiograph, the accessory ossicles are frequently misdiagnosed as fractures. Occasionally, the ossicles may also suffer fractures which cause pain [2]. MRI can provide excellent soft-tissue detail, and detect bone marrow edema and surrounding soft tissue involvement if there is pathology related to the accessory ossicle. While MRI is a common second-line investigation if plain radiographs are inconclusive in investigating bone pain, while anatomic imaging techniques, in particular, MRI, offer exquisite soft-tissue detail, bone scintigraphy may play a role also be useful in the diagnosis and localization of pain generators. Indeed, increased bone turnover (high activity) may correlate better with sites of active pathology [3].
Bone scintigraphy is used to help diagnose conditions such as malignancy, inflammation and fracture. It provides functional imaging to visualize bone metabolism which radiograph and CT cannot pick up. Its ability to pick up areas of increased bone turnover may correlate better with sites of active pathology [4]. However, the intrinsic anatomic resolution of the technique is limited. Even though the introduction of multi-modality SPECT/CT has improved the sensitivity and specificity of bone scintigraphy. 18F-NaF PET/CT currently offers the highest image and is reported to be superior to conventional 99mTc-MDP [5]. In this review article, we would like to present a spectrum of cases and the potential diagnostic utility of 18F-NaF in the assessment of symptomatic accessory ossicles, which was picked up as an incidental finding in patients referred for staging cancers.
Limited anatomical resolution may be a disadvantage of using bone scintigraphy, but hybrid imaging involving CT provides the tool to give both functional and anatomical detail in a single study and also increases the specificity of 18F-NaF PET [4]. This modality is also may be useful in patients with contraindications for MRI and can be used as an adjunct to investigate causes of musculoskeletal pain. In this review article, we would like to present a spectrum of cases and the potential diagnostic utility of 18F-NaF in the assessment of symptomatic accessory ossicles, which was picked up as incidental findings on patients referred for staging cancers.
Findings
Os naviculare accessorium or accessorium or os tibiale externum
The os naviculare accessorium is an accessory ossicle adjacent to the medial aspect of the navicular bone. One of the most common accessory bones of the foot, it has a reported incidence of up to 28% [4]. It is present in about 10% of the population, with a bilateral prevalence of approximately 70%. It can present with medial side foot pain that worsens, worsening with weight-bearing exercises (Figure 1). If the os is large, it can protrude medially to cause friction against footwear. It can be classified using the Geist classification into three types [5]. Type 1 accessory os navicular is a 2-3 mm sesamoid bone within the distal aspect of the posterior tibial tendon with no attachment to the navicular tuberosity; Type 2 usually measures 12 mm, and is connected to the navicular tuberosity by hyaline cartilage or fibrocartilage, this is the most common variant of os naviculare (50%) [4]; Type 3 is a prominent tuberosity known as cornuate navicular-this is thought to be a fused Type 2 os navicular, resulting in bony protuberance. Type II is more likely to cause symptoms, and studies suggest simple excision to be beneficial for symptomatic type 2 os naviculare [6]. Surgery may also involve the reshaping of the area and repair posterior tibial tendon to restore function.
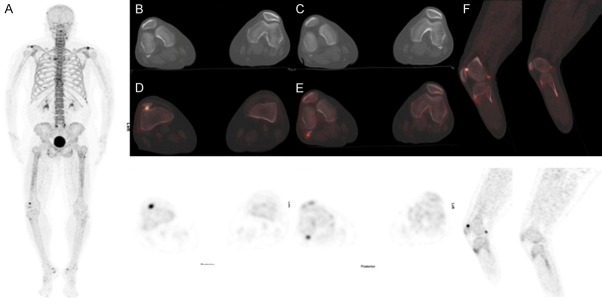
Figure 1.
54-year old female diagnosed with breast cancer presented with left foot pain of 3 months. A. 18F-NaF PET/CT was performed for staging. MIP images demonstrate increased radiotracer uptake in the anteromedial aspect of left mid foot region and right distal femur (bone infarct). B. 18F-NaF PET/CT images show increased radiotracer uptake in the anteromedial aspect of left mid foot. C. Axial CT images demonstrate a bilateral osseous density medial to the navicular bone which was suggestive of a Type II accessory navicular bone. D-F. Fused 18F-NaF PET/CT shows increased tracer uptake in the articulation with sclerosis between the medial border of the left navicular and an os naviculare. Scan appearances are suggestive of left painful accessory os syndrome.
Os fabella
Fabella translates to “little bean” in Latin. This accessory ossicle is typically found in the lateral head of gastrocnemius, as a sesamoid bone in the posterolateral capsule of the knee joint (Figure 2). Occasionally they are found in the medial head of gastrocnemius. Fibrocartilaginous in nature, they can articulate with the respective femoral condyle. Previous studies have suggested it occurs in 20-87% of the population, with a higher incidence in the Asian population [7-10]. Patients can present with posterolateral knee pain, often known as the fabella syndrome [11]. Pain increases with the extension of the knee as the fabella are pressed upon the femoral condyle [12]. It can also cause compression on the common fibular nerve, causing a peroneal nerve palsy [13,14]. Usually, symptoms resolve with conservative management but can recur with high levels of activity. Surgical excision can be carried out with minimal risk [12].
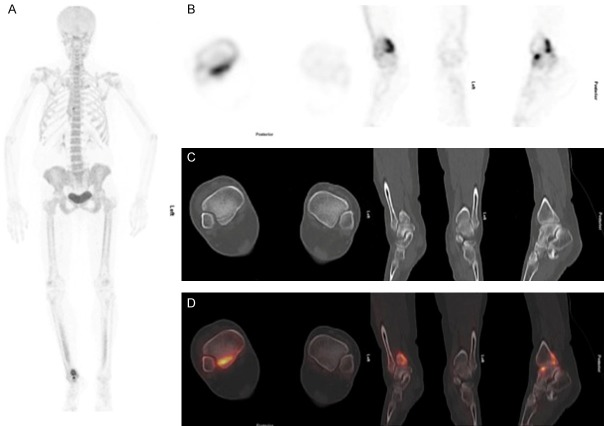
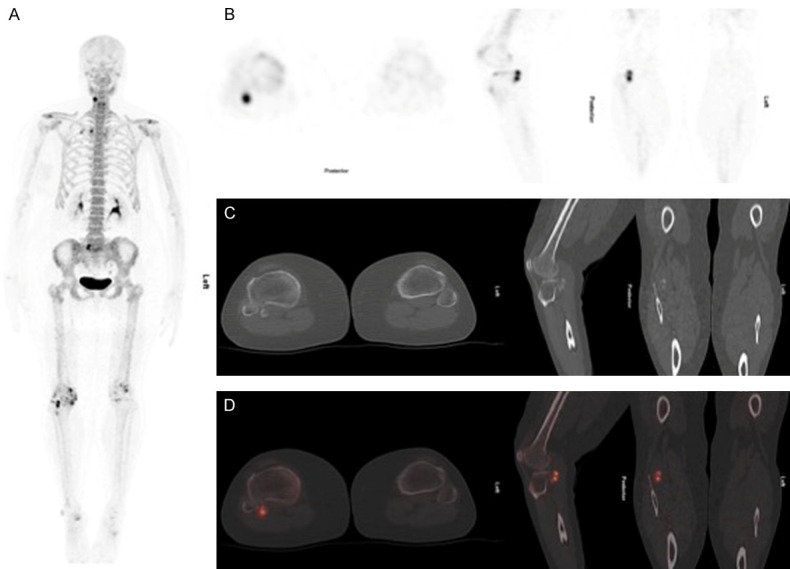
Figure 2.
64-year old female with breast cancer and right posterolateral knee pain underwent 18F-NaF PET/CT for staging. A. MIP images show increased tracer activity in both acromioclavicular joints, the facet joints of L5/S1, the right knee as well as in the bones of both feet. B, C. Axial CT images demonstrate bilateral osseous density posterolateral to the femoral condyle. D-F. Fused 18F-NaF PET/CT show increased tracer uptake in the right patellofemoral joint and articulation of right gastrocnemius muscle with fabella. The tracer uptake within the left fabella is relatively normal. The scan findings are suggestive of right painful fabella syndrome and patellofemoral joint arthritis.
Os subfibulare
Os subfibulare is located at the tip of the lateral malleolus between the tip of the lateral malleolus and the talus (Figure 3). The secondary center of ossification of the lateral malleolus starts in the first year of life and usually fuses by age of 15 [15]. Very rarely do they enlarge and become symptomatic. The ossicles can be fractured, with the injury extending through a segment of the malleolus. It can also be avulsed, which if not adequately diagnosed and treated, can lead to delayed union, non-union, or chronic pain of the ankle [16]. When symptomatic, it can be treated conservatively, but if presented with refractory symptoms, surgery is indicated. Symptoms can be relieved with excision of the ossicle and reconstitution of the collateral ligament [17].
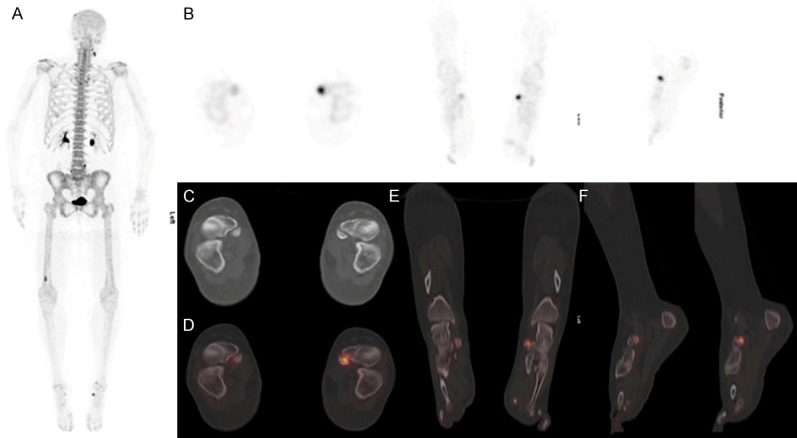
Figure 3.
66-year old female with left sided breast cancer complains of generalized bone pain. A. 18F-NaF PET/CT MIP images show increased tracer activity in the sternum, the left 1st and 2nd rib. Increased tracer uptake is also seen in both knees and the distal right leg. B. Transaxial NaF images show increased tracer uptake in the right ankle. C. CT shows a bifid appearance of the tip of the lateral malleolus of the right fibula, representing an accessory ossicle. D, E. Fused 18F-NaF PET/CT images show increased tracer uptake at the articulation site. Findings are consistent with a symptomatic os subfibulare.
Os subtibiale
The os subtibiale is a rare accessory ossicle has an incidence of 0.2-1.2% [18], and it is results from the failure of the failure of fusion of separate ossification centers of the medial malleolus in childhood (Figure 4). It is a rare accessory bone, and a study found that it was present in about 1% of the population. In the reported cases, os subtibiale were reported to be bilateral [18]. Patients may present with swelling over the medial aspect of the ankle with tenderness over the deltoid ligament. Commonly misdiagnosed as a malleolar injury, it can lead to unnecessary surgery. It is differentiated from a fractured malleolus on x-ray as it has a smooth edge, is often bilateral, and has maximum tenderness over the ligaments rather than over the medial malleolus. Initial treatment is conservative with compression bandage and anti-inflammatories, but it has also been reported that excision with open surgery provides complete resolution of symptoms [19].
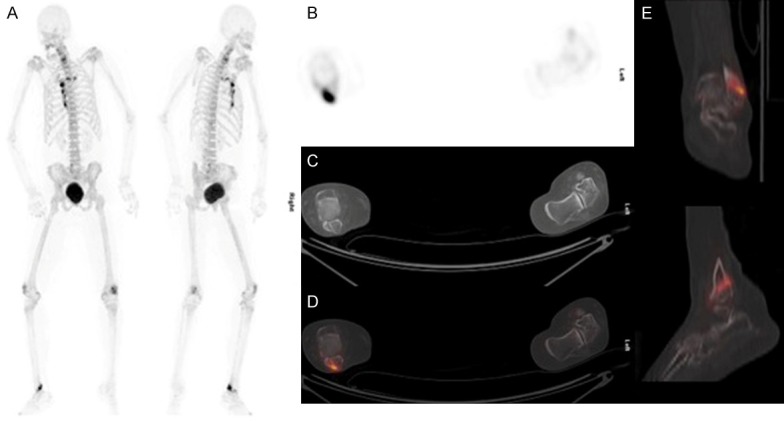
Figure 4.
44-year old female complained of right distal leg pain for 4 months. A. 18F-NaF MIP images shows increased tracer activity in distal right tibia. B. Transaxial PET images show increased tracer uptake at tip of medial malleolus. C. CT shows an unfused medial malleolus ossification center of the right tibia representing an accessory ossicle. D. Fused 18F-NaF PET/CT images show increased tracer uptake at the articulation site. These findings are consistent with a painful os subtibiale.
Os cyamella
An os cyamella is common in primates, but rare in humans. It is a sesamoid bone, usually located on the lateral aspect of the distal femur, in the popliteal grove (Figure 5). It is a normal variant within the popliteus tendon [20] and usually presents as with posterolateral knee pain and intermittent swelling and locking. Other differentials include osteochondral flakes, osteophytes, a fabella, and periosseous calcifications [19].
Figure 5.
55-year old female has left breast cancer and liver metastases receiving 18F-NaF PET/CT because of right leg pain. A. MIP images show increased tracer activity in both acromioclavicular joints, the right sternoclavicular and knee joints. B. PET images show focally increased tracer uptake at the posterior aspect of the proximal tibia on the right. C. On CT there is a round bone density posterior of right proximal tibia, a finding compatible with an accessory sesamoid ossicle of the popliteus known as cyamella. D. Fused 18F-NaF-PET/CT images show increased tracer uptake at this site, consistent with painful cyamella syndrome.
Os acromiale
There are normally three acromial ossification centers which fuse by the age of 25. An os acromiale is the result of a failed fusion of the one of three acromial ossification centers, and is present in about 8% of people [21]. They can be classified into subtypes, based on the fusion pattern of the three ossification centrescenters. Painful shoulder can be due to impingement of rotator cuff muscles with the unfused fragments causes impingement symptoms (Figure 6). Motion movement at the unfused sites can lead to arthritic changes, and there can also be concomitant rotator cuff tear. Amongst elite swimmers, it commonly presents as a painful shoulder or shoulder discomfort, and is a cause of “swimmer’s shoulder” [22]. An os acromiale is commonly misdiagnosed as muscle fatigue or rotator cuff overload.
Figure 6.
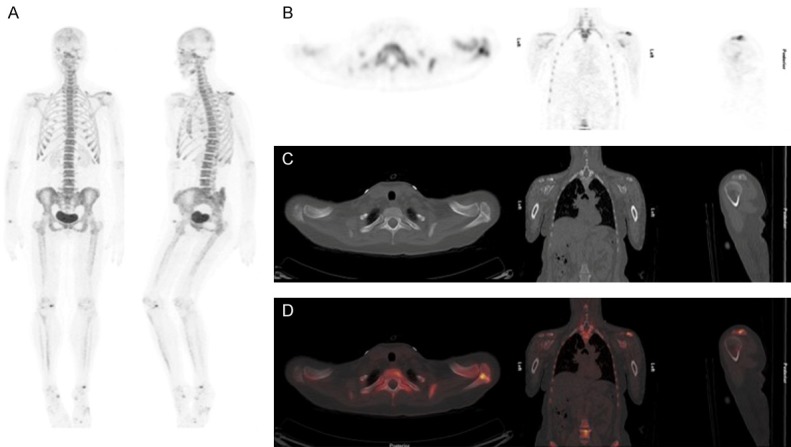
42-year old female with right sided breast cancer and severe left shoulder pain. A. MIP images show increased tracer activity in the left acromioclavicular region, right knee and both mid foot regions. B. PET images show increased tracer activity at the left acromioclavicular joint. C. CT images shows unfused left anterior acromial ossification center (os acromiale) with sclerosis of on the articular surface. D. Fused 18F-NaF PET/CT axial, coronal and sagittal images show increased tracer uptake at the articulation site. These findings are consistent with painful os acromiale.
Discussions
Accessory bones are common anatomical variants. A broad knowledge of the location of accessory bones will aid history taking, physical examination, and diagnosis. Unfortunately, there are limited publications on the various os, most of which are case reports. An increased knowledge is important to raise awareness of accessory bones as a differential diagnosis when assessing imaging studies obtained for the musculoskeletal pain of unknown origin. When identified, these bones may not be clinically significant but may lead to unnecessary investigations if mistaken for a fracture. Our cases have demonstrated the use of 18F-NaF in evaluating accessory ossicles as incidental findings.
99mTc is widely used in bone scintigraphy, but there has been resurging interest in the use of 18F-NaF for use of PET/CT. It is a validated imaging tool for bone imaging with favorable pharmacokinetics compared to 99mTc. Araz et al. demonstrated the superior ability of 18F-NaF PET/CT in visualizing small lesions due to better resolution and higher target/background ratio [23]; this would be particularly useful as os fragments may be small. With increasing popularity of 18F-NaF, we would be able to use it to demonstrate diverse disease spectrum and is a promising tool for diagnostic use in patients with pain of multiple locations.
While MRI is deemed superior in its anatomical detail, PET imaging allows functional imaging, and our examples show that they can be diagnostic in identifying symptomatic ossicles. In our patients, there was no need for further imaging to confirm the diagnosis, and use of this modality can also be used for patients with contraindications to MRI.
Conclusion
While not yet widely used, 18F-NaF will be increasingly used in diagnosing skeletal pain which is otherwise not identified on radiographs. Its diagnostic ability would be useful, especially in patients who are already undergoing bone scintigraphy, and in patients who report pain of multiple locations. Its promising use needs to be further explored from case reports and its further studies.
Acknowledgements
Dr. Abduredha Esmail, Dr. Fareeda Alkandari and Dr. Najeeb Ahmed.
Disclosure of conflict of interest
None.
References
- 1.Miller TT. Painful accessory bones of the foot. Semin Musculoskelet Radiol. 2002;6:153–161. doi: 10.1055/s-2002-32361. [DOI] [PubMed] [Google Scholar]
- 2.Mellado JM, Ramos A, Salvado E, Camins A, Danus M, Sauri A. Accessory ossicles and sesamoid bones of the ankle and foot: imaging findings, clinical significance and differential diagnosis. Eur Radiol. 2003;13(Suppl 6):L164–177. doi: 10.1007/s00330-003-2011-8. [DOI] [PubMed] [Google Scholar]
- 3.Even-Sapir E, Mishani E, Flusser G, Metser U. 18F-Fluoride positron emission tomography and positron emission tomography/computed tomography. Semin Nucl Med. 2007;37:462–469. doi: 10.1053/j.semnuclmed.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF 3rd, Roemer FW, Malguria N, Guermazi A. Sesamoids and accessory ossicles of the foot: anatomical variability and related pathology. Insights Imaging. 2013;4:581–593. doi: 10.1007/s13244-013-0277-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geist E. Supernumerary bone of the foot: a roentgen study of the feet of 100 normal individuals. Am J Orthop Surg. 1914;12:403. [Google Scholar]
- 6.Rietveld AB, Diemer WM. Surgical treatment of the accessory navicular (os tibiale externum) in dancers: a retrospective case series. J Dance Med Sci. 2016;20:103–108. doi: 10.12678/1089-313X.20.3.103. [DOI] [PubMed] [Google Scholar]
- 7.Pritchett JW. The incidence of fabellae in osteoarthrosis of the knee. J Bone Joint Surg Am. 1984;66:1379–1380. [PubMed] [Google Scholar]
- 8.Minowa T, Murakami G, Kura H, Suzuki D, Han SH, Yamashita T. Does the fabella contribute to the reinforcement of the posterolateral corner of the knee by inducing the development of associated ligaments? J Orthop Sci. 2004;9:59–65. doi: 10.1007/s00776-003-0739-2. [DOI] [PubMed] [Google Scholar]
- 9.Kawashima T, Takeishi H, Yoshitomi S, Ito M, Sasaki H. Anatomical study of the fabella, fabellar complex and its clinical implications. Surg Radiol Anat. 2007;29:611–616. doi: 10.1007/s00276-007-0259-4. [DOI] [PubMed] [Google Scholar]
- 10.Zeng SX, Dong XL, Dang RS, Wu GS, Wang JF, Wang D, Huang HL, Guo XD. Anatomic study of fabella and its surrounding structures in a Chinese population. Surg Radiol Anat. 2012;34:65–71. doi: 10.1007/s00276-011-0828-4. [DOI] [PubMed] [Google Scholar]
- 11.Weiner DS, Macnab I. The “fabella syndrome”: an update. J Pediatr Orthop. 1982;2:405–408. [PubMed] [Google Scholar]
- 12.Driessen A, Balke M, Offerhaus C, White WJ, Shafizadeh S, Becher C, Bouillon B, Hoher J. The fabella syndrome - a rare cause of posterolateral knee pain: a review of the literature and two case reports. BMC Musculoskelet Disord. 2014;15:100. doi: 10.1186/1471-2474-15-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takebe K, Hirohata K. Peroneal nerve palsy due to fabella. Arch Orthop Trauma Surg. 1981;99:91–95. doi: 10.1007/BF00389743. [DOI] [PubMed] [Google Scholar]
- 14.Patel A, Singh R, Johnson B, Smith A. Compression neuropathy of the common peroneal nerve by the fabella. BMJ Case Rep. 2013:2013. doi: 10.1136/bcr-2013-202154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shands AJ. Accessory bones of foot: x-ray study of feet of 1,054 patients. South Med Surg. 1931;93:326–334. [Google Scholar]
- 16.Pai MV. Os subfibulare: a case report of painful fibular accessory ossicle. FAOJ. 2010;3:3. [Google Scholar]
- 17.Berg EE. The symptomatic os subfibulare. Avulsion fracture of the fibula associated with recurrent instability of the ankle. J Bone Joint Surg Am. 1991;73:1251–1254. [PubMed] [Google Scholar]
- 18.Madhuri V. Accessory os subtibiale: a case report of misdiagnosed fracture. FAOJ. 2009;2:3. [Google Scholar]
- 19.Iliev AA, Georgiev GP, Landzhov BV, Slavchev SA, Dimitrova IN, Ovtscharoff Wcapital AC. Symptomatic os subtibiale associated with chronic pain around the medial malleolus in a young athlete. Folia Med (Plovdiv) 2016;58:60–63. doi: 10.1515/folmed-2016-0009. [DOI] [PubMed] [Google Scholar]
- 20.Benthien JP, Brunner A. A symptomatic sesamoid bone in the popliteus muscle (cyamella) Musculoskelet Surg. 2010;94:141–144. doi: 10.1007/s12306-010-0083-6. [DOI] [PubMed] [Google Scholar]
- 21.Papatheodorou A, Ellinas P, Takis F, Tsanis A, Maris I, Batakis N. US of the shoulder: rotator cuff and non-rotator cuff disorders. Radiographics. 2006;26:e23. doi: 10.1148/rg.e23. [DOI] [PubMed] [Google Scholar]
- 22.Bedi A, Rodeo SA. Os acromiale as a cause for shoulder pain in a competitive swimmer: a case report. Sports Health. 2009;1:121–124. doi: 10.1177/1941738108326705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Araz M, Aras G, Kucuk ON. The role of 18F-NaF PET/CT in metastatic bone disease. J Bone Oncol. 2015;4:92–97. doi: 10.1016/j.jbo.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]