Abstract
Death certificate data from the Multiple Cause of Death (MCOD) files were analyzed to better understand the drug categories most responsible for the increase in fatal overdoses occurring between 1999 and 2014. Statistical adjustment methods were used to account for the understatement in reported drug involvement occurring because death certificates frequently do not specify which drugs were involved in the deaths. The frequency of combination drug use introduced additional uncertainty and so a distinction was made between any versus exclusive drug involvement. Many results were sensitive to the starting and ending years chosen for examination. Opioid analgesics played a major role in the increased drug deaths for analysis windows starting in 1999 but other drugs, particularly heroin, became more significant for recent time periods. Combination drug use was important for all time periods and needs to be accounted for when designing policies to slow or reverse the increase in overdose deaths.
Keywords: Drug fatalities, Fatal overdoses, Drug poisoning deaths, Drug deaths, Drug mortality, Overdose deaths, Drug cocktails
Highlights
-
•
The number of drug poisoning deaths rose in every year between 1990 and 2014.
-
•
The specific drugs involved in fatal overdoses are understated on death certificates.
-
•
The drugs responsible for the secular increase in fatal overdoses vary over time.
-
•
Nevertheless, the majority of drug deaths involve multiple classes of drugs.
1. Introduction
Fatal drug overdoses have reached epidemic levels in the United States, increasing 137% from 2000–2014 (Rudd, Aleshire, Zibbell, & Gladden, 2016). Growth in poisoning deaths, around 90% of which are now caused by drugs (Warner, Chen, Makuc, Anderson, & Miniño, 2011), were the most important source of the rise in the all-cause mortality rates of 45–54-year-old non-Hispanic whites occurring between 1999 and 2013 (Case & Deaton, 2015). The involvement of opioid analgesics (hereafter referred to as “opioids”) and, more recently, heroin have received particular attention (Centers for Disease Control and Prevention, 2011, Centers for Disease Control and Prevention, 2012, Jones et al., 2015, Rudd et al., 2016, Volkow et al., 2014), including a White House Summit in August 2014 (Hardesty, 2014).
Concerted efforts to lessen the severity of the opioid epidemic include establishing prescription drug monitoring programs, restricting the ability of pain clinics and online pharmacies to dispense oxycodone and other controlled substances, and developing abuse-deterrent formulations of some prescription drugs (Centers for Disease Control and Prevention, 2013, Finklea et al., 2013, Rannazzisi, 2013, Kirschner et al., 2014). The federal Comprehensive Addiction and Recovery Act of 2016 (S. 524) supports expansions of drug diversion programs (reducing the criminality of low-level drug violations), medication assisted treatments, and the availability of naloxone administration for opioid overdoses.
However, there remain significant barriers to formulating effective policies to reverse or slow the rise in drug fatalities. One is that deadly overdoses frequently involve combinations of drugs in ways that are not fully understood (Jones et al., 2013, Paulozzi et al., 2014).1 Second, we lack reliable knowledge of the specific drugs involved in poisoning fatalities because the drugs responsible are frequently left unspecified on death certificates. As a result, the contributions of specific drug categories or of drug combinations are understated.
Misunderstanding about these issues results in frequent erroneous statements being made about the nature of drug poisoning fatalities. In a typical example, Olsen (2016) states: “In 2014, nearly 20,000 deaths due to overdose of prescription opioids occurred in the United States”. This is incorrect. An accurate characterization is that a prescription opioid was mentioned on the death certificates of around 20,000 fatalities classified as drug poisonings in that year. However, the actual number of cases involving opioids was certainly larger than this, because the drugs involved in these deaths were frequently not recorded. Conversely, prescription opioids may have caused either more or fewer fatalities because other drugs (particularly sedatives and psychotropic medications) were also implicated in many of these deaths. These issues become even more problematic when considering trends in fatal drug overdoses, since patterns of drug reporting and combination use have changed over time.
This analysis provides a first step in addressing several of these shortcomings and is innovative in three ways. First, statistical adjustment procedures recently developed by Ruhm (2016a) are extended and applied here to provide more accurate information on the drugs and drug combinations involved in fatal overdoses. These methods raise estimates of the involvement of specific drugs by 30% to >50% and emphasize the importance of drug “cocktails”. Second, the adjusted estimates are used to examine which drug categories are responsible for the rapid rise in fatal overdoses. The frequency of multiple drug-taking introduces uncertainty, so a distinction is made between any versus exclusive drug involvement. Third, the investigation highlights the sensitivity of the findings to the choice of starting and ending years, revealing a key role of prescription opioids early in the data period but with other drugs, particularly heroin, and drug combinations being more important later.
2. Methods
2.1. Data
The primary outcomes are counts of drug poisoning deaths to US residents, using death certificate data from the 1999–2014 Multiple Cause of Death files (MCOD). The MCOD provide information on: a single underlying cause of death (UCD), up to twenty additional causes and some demographic data (Centers for Disease Control and Prevention, 2016). Cause-of-death was categorized using four-digit International Classification of Diseases, Tenth Revision (ICD-10) codes with details also provided on place of residence, age, race/ethnicity, sex, year, and weekday of death. The public use files lack geographic identifiers but restricted data on the state and county of residence were obtained for use in this study.
Poisoning deaths were defined using ICD-10 UCD codes, where the underlying cause is the “disease or injury that initiated the chain of morbid events that led directly and inevitably to death” (Centers for Disease Control and Prevention, 2014).2 In cases of drug overdoses, the death certificate lists one or more drugs involved as immediate or contributory causes of death. These were included as ICD-10 “T-codes” and referred to here as drug involvement or mentions. The specific drug categories examined were: narcotics, sedatives, psychotropics, other specified drugs and unspecified drugs. Important subcategories were also analyzed. Narcotics were subdivided into opioid analgesics, heroin, cocaine and other narcotics, and psychotropics into antidepressants, antipsychotics and stimulants.3 “Other specified” drugs included anesthetics, antiallergic and immunosuppressive drugs, histamine and anti-gastric secretion medications, cardiac drugs, antibiotics and many others. Poisoning by unspecified drugs, medicaments and biologicals (ICD-10 T-code, T50.9) is important because no specific drug was identified for 20–25% of fatal overdoses. Combination drug use was defined as the involvement of two or more of the drug categories: opioids, heroin, cocaine, other narcotics, sedatives, psychotropics or other drugs. This classification does not capture the use of multiple types of drugs within classes.4
The primary analysis began in 1999 because ICD-9 codes, used earlier, were not fully comparable to ICD-10 categories (Anderson, Miniño, Hoyert & Rosenberg, 2001). However, frequencies of drug poisoning deaths (but the not the specific drugs involved) could be compared using ICD-9 and ICD-10 codes, so public-use MCOD files for years before 1999 were used to conduct a descriptive investigation of broad trends in overdose fatalities from 1982–2014.
2.2. Analytic approach
The first step in determining which drug categories were responsible for the rise in overdose mortality involved accounting for fatalities where the death certificates did not specify the drugs involved. To do so, the analysis was limited to drug deaths and a dichotomous variable was constructed indicating if at least one drug type was mentioned on the death certificate, rather than only the unspecified category (ICD-10 T-code, T50.9). County-year averages of this variable were calculated and denoted as .
A series of probit models were next estimated to predict the determinants of specific drug mentions on death certificates. These models were run separately for each year and drug category (e.g. opioids in 2014) and also for drug combinations (more than one drug category reported). The specifications took the form:
| (1) |
where was a binary dependent variable indicating if the overdose death for individual i in county j was reported to involve the specified drug (based on ICD-10 T-codes) or more than one category (i.e. a drug combination). Estimating separate models for each drug type and year allows the predicted effects of , and the other explanatory variables, to vary across drug classes and time periods. This could occur if, for example, some drug categories were reported more completely than others in areas with low rates of reporting, or if the reporting patterns changed over time.
In addition to the models included supplementary covariates ( for: sex, two race indicators (black, other nonwhite), currently married (versus never married, separated/divorced, widowed, or status not reported), four educational categories (less than high school graduate, high school graduate, some college, college graduate), eight age groups (≤20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, >80), nine census regions (New England, Mid-Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain and Pacific) and seven day of the week indicators.5 is an error term.
Predicted values of the dependent variables were calculated, for each drug poisoning death in the given year, and then averaged, to obtain mean predicted prevalences,
| (2) |
for Φ(⊡) the cumulative distribution function of the standard normal distribution. Since these predictions were based on actual values of the explanatory variables, the estimated prevalences were expected to be close to the sample mean values. This was tested for and confirmed.
A second set of predicted values was obtained after setting to one for all drug deaths in the year. The average expected value, hereafter referred to as the “adjusted prevalence”, , and estimated as:
| (3) |
indicates the involvement rate predicted for the specified drug category if at least one drug had been mentioned on all overdose death certificates. A key assumption for the adjusted prevalences to provide unbiased estimates of true prevalences is that the explanatory variables were related to drug involvement in the same way for deaths with no drug reported on the death certificate (only ICD-10 T-code, T50.9) as for those where at least one drug was mentioned. Robust standard errors and associated 95 percent confidence intervals (95% CI) were calculated with observations clustered by county.
The predicted number of deaths involving a specific class of drugs, , was calculated as the product of the adjusted prevalence and number of drug poisoning deaths in the year (:
| (4) |
Corresponding estimates for exclusive drug involvement (e.g. opioids without the involvement of heroin, cocaine, sedatives, psychotropics or other drugs) were also obtained. Sensitivity of the results to alternative sets of covariates or estimating linear probability, rather than probit, models was examined.
The calculations just described represent “in-sample” estimates but two indications of the success of the adjustment procedures were considered. The first compared reported and adjusted prevalences of exclusive unspecified drug involvement. As mentioned, the reported prevalence was 20–25% in most years. Completely successful adjustment procedures would reduce this to zero. The second test reversed the first by calculating adjusted prevalences assuming that drug types were never specified on the death certificates (i.e. =0), with perfect adjustment implying exclusive unspecified drug prevalences of 100%.6 Note that predicted probabilities from probit models can never reach zero or one, so that complete adjustment is not possible.
The adjusted prevalences were then used to calculate the contributions of specific drug categories to the growth in fatal overdoses. Changes in prevalences between an earlier and a later period, denoted using the subscripts 0 and 1, respectively, were:
| (5) |
and the change in deaths involving a specified drug category was:
| (6) |
for Finally, the percentage of the change in all drug deaths due to the specific drug category was estimated as: These percentages were calculated for both any and exclusive drug involvement. Since previous investigations have typically focused on any mentions, they correspond to the first set of estimates, except without adjusting for undercounting due to incomplete drug reporting. Contributions to overdose mortality trends based on any involvement double-count cases where multiple drugs were implicated and so overstate the role of specific drug categories. Conversely, estimates based on exclusive involvement understate the contributions, since no attribution was made when the deaths involve drug cocktails.
The 1999–2014 analysis period was dictated by data availability (using ICD-10 codes), rather than a theoretical justification. Two related strategies were implemented to examine sensitivity of the results to the choice of starting and ending years of analysis. In the first, the starting year was always 1999 and estimates were obtained for all possible ending years between 2003 and 2014. For the second, the final year was 2014 and the beginning year ranged from 1999–2010.7
3. Results
3.1. Trends in fatal overdoses and drug specification rates
Fatal overdoses rose 622% between 1982–2014, from 6518 to 47,055 deaths. In 1982, motor vehicle fatalities were seven times more common than drug deaths but by 2014, there were 33% more overdose deaths than vehicle fatalities, and drugs accounted for 91% of all poisoning mortality. Seventy-five percent of the rise in fatal overdoses from 1982–2014 occurred since 1999, the starting year of the primary analysis. Some of the increase in drug deaths reflects population growth, but the overdose mortality rate rose 425% (from 2.81 to 14.75 per 100,000) between 1982–2014.8 Fatal overdoses grew more over time for males than females and, since 2000, for whites than blacks. In 2014, persons aged 35–54 had the highest risk of dying from drugs; death rates were lowest in the West North Central region of the US and much of the South, except for Oklahoma and Louisiana, while being relatively high in Alaska, most Mountain and Appalachian states (except Idaho), the rust belt and parts of New England. However, there were pockets of high mortality in otherwise relatively low drug death states such as California and Texas.
The percentage of fatal overdoses with at least one drug type reported on the death certificate ranged from 74.1% in 2008 to 80.4% in 2014, with relatively low specification rates during the great recession (2007–2009) and its aftermath, and rapid increases near the end of the sample period. County-level drug specification and mortality rates also appeared to be related, raising the possibility that differential reporting patterns could influence the calculated fatal overdose rates.
Details on these patterns are provided in Figures A1-A5 of the online Supplement.
3.2. Drug poisoning deaths in 2014
Table 1 shows the drugs involved in 2014 fatal overdoses, based on reported and adjusted prevalences. The first column indicates the drug category, with corresponding ICD-10 codes in parentheses (ChiroCode Institute, 2014). The second and third columns display numbers and shares of deaths, based on death certificate reports. The last two columns show adjusted prevalences, estimated using the procedures described above, and percentage differences between these and reported prevalences, with 95% confidence intervals in brackets. As discussed, any versus exclusive involvement, as well as multiple drug use, were evaluated.
Table 1.
Reported and adjusted drug involvement in 2014 drug poisoning deaths.
| Drug mentions | Reported # of Deaths | Prevalence (%) | Adjusted prevalence (%) | % Difference |
|---|---|---|---|---|
| Any Involvement (T-Codes) | ||||
| Narcotics (40.0–40.9) | 30,731 | 65.3 | 82.2 [81.3–83.2] | 25.9 [24.4–27.4] |
| Opioid Analgesics (40.2–40.4) | 18,893 | 40.2 | 52.6 [50.7–54.6] | 31.1 [26.3 – 35.9] |
| Heroin (40.1) | 10,574 | 22.5 | 30.0 [28.0 –32.0] | 33.4 [24.5–42.3] |
| Cocaine (40.5) | 5415 | 11.5 | 15.2 [13.8 –16.5] | 31.7 [20.3–43.1] |
| Other Narcotics (40.0, 40.6–40.9) | 2822 | 6.0 | 7.5 [6.2–8.8] | 24.7 [2.9–46.5] |
| Sedatives (42.0–42.8) | 9308 | 19.8 | 29.2 [27.5–30.9] | 47.6 [39.0–56.1] |
| Psychotropics (43.0–43.9) | 9614 | 20.4 | 27.3 [25.5–29.1] | 33.5 [24.8–42.3] |
| Antidepressants (43.0–43.2) | 4768 | 10.1 | 14.9 [13.9–15.8] | 46.6 [37.1–56.1] |
| Antipsychotics (43.3–43.5) | 1588 | 3.4 | 5.2 [4.7–5.7] | 53.9 [38.6–69.2] |
| Psychostimulants (43.6) | 4298 | 9.1 | 11.0 [9.7–12.3] | 20.0 [5.9–34.2] |
| Other Specified (36.0–38.9, 41.0, 41.9 | 3573 | 7.6 | 10.3 [9.6–10.9] | 35.5 [26.8–44.1] |
| 44.0–48.7, 49.0–50.8) | ||||
| Unspecified (50.9) | 23,347 | 49.6 | 38.4 [35.2–41.6] | −22.6 [−29.0– −16.2] |
| Exclusive Involvement | ||||
| Opioid Analgesics | 7769 | 16.5 | 19.3 [18.1–20.5] | 17.1 [9.8–24.5] |
| Heroin | 5067 | 10.8 | 13.4 [11.9–14.8] | 24.2 [10.6–37.7] |
| Cocaine | 1747 | 3.7 | 4.3 [3.7–4.9] | 16.1 [0.7–31.5] |
| Sedatives | 814 | 1.7 | 2.1 [1.9–2.3] | 22.4 [11.6–33.2] |
| Psychotropics | 3390 | 7.2 | 7.9 [7.1–8.8] | 10.2 [-1.8−22.3] |
| Other Specified | 1476 | 3.1 | 3.5 [3.3–3.8] | 12.3 [4.0−20.6] |
| Unspecified | 9201 | 19.6 | 3.5 [3.2–3.7] | -82.2 [-83.5– −81.0] |
| >1 Drug Category | 16,187 | 34.4 | 49.3 [47.5–51.1] | 43.2 [38.0–48.4] |
Note: Data are from the Multiple Cause of Death files. Drug poisoning deaths include ICD-10 Underlying Cause of Death Codes: X40-44, X60-64, X85, Y10-14, Y35.2, *U01.6 and *U01.7) Entries in parentheses refer to ICD-10 T codes for drug mentions. >1 Drug Category refers to drug mentions of two or more of the following drug types: opioid analgesics, heroin, cocaine, other narcotics, sedatives, psychotropics and other specified drugs. Exclusive drug involvement indicates deaths where only the specified class of drugs is mentioned (but unspecified drugs could also be involved). Reported numbers of deaths and prevalences are from death certificates and indicate the percentage of drug poisonings where the specified type of drug is mentioned. Adjusted prevalences are average predicted values from probit models, where at least one specific drug is assumed to be mentioned for all poisoning deaths in the county (SPECIFY=1). Models also control for: sex, race (black, other), Hispanic origin, currently married, education (high school dropout, high school graduate, some college, college graduate), age (≤20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, >80), day of the week of death, and census region. % Difference refers to the percentage difference between the adjusted and reported prevalences. These are calculated using more significant digits than are shown in the table, so some differences may appear due to rounding error. 95 percent confidence intervals, shown in brackets, are computed using robust standard errors with clustering at the county level.
Narcotics were mentioned on the death certificates of 65% of fatal overdoses, with reported prevalences of 40%, 23% and 12% for opioids, heroin and cocaine. However, involvement of other drugs was also common, with sedatives and psychotropic drugs each listed around one-fifth of the time. No drug was specified in 20% of deaths, with multiple drug classes reported in 34%.9 One implication is that it will be hard to assign the responsibility of the death to any specific drug category. For example, prescription opioid use was mentioned in 40% of drug poisoning deaths but was the only drug category in just 17%. Exclusive involvement of other drug types was reported only one-fifth to one-half as often as any mention, in most cases, except that sedatives were almost never the only drug reported.10
Adjusted prevalences were higher than reported prevalences for all specific drug categories. For example, the adjusted opioid analgesic prevalence was 52.6% (95% CI, 50.7%-54.6%), or 31% (95% CI, 26%-36%) higher than the reported 40.2% rate. For other major drug categories, the difference between adjusted and reported prevalences ranged from 32%-48%, and for multiple drug use it was 43% (95% CI, 38%-48%). Disparities between adjusted and reported prevalences were generally smaller and more varied for exclusive (than any) drug involvement, but still important, ranging from a statistically non-significant 10% for psychotropics to 24% (95% CI, 11%-38%) for heroin.11
The adjustment procedures worked well, but not perfectly. Specifically, the adjusted prevalence of only unspecified drug involvement was less than one-fifth as large as the reported prevalence: 3.5% (95% CI, 3.2–3.7%) versus 19.6%. Calculating adjusted prevalences under the assumption that drug types were never specified on the death certificates (by predicting probabilities with =0) yielded a predicted prevalence of exclusively unspecified drug involvement of 96.3% (95% CI, 95.8%-96.9%), where perfect adjustment would imply a prevalence of 100%. Thus, to the extent the adjustments remain incomplete, there may be a small remaining understatement of specific drug involvement.
The adjustment procedures were also robust to a variety of alternative specifications including: 1) estimating linear probability rather than probit models; 2) excluding all covariates other than ; 3) adding supplementary covariates for manner of death (intentional, accidental, or undetermined intent) and whether an autopsy was performed (see Supplement table A3 for results).12 Examination of subsamples stratified by manner of death revealed some differences in patterns of drug involvement. Table A4 of the supplement provides details. Finally, Ruhm (2016b) investigated whether adjusted prevalences continued to be understated because the procedure did not account for cases where both specified and unspecified drugs were listed on the death certificate. Some support for this possibility was provided for sedatives, psychotropic medications and combination drug use, but less so for prescription opioids, heroin or cocaine.
3.3. Fatal drug poisonings: 1999–2014
Using the previously described methods, reported and adjusted prevalences, as well as the corresponding numbers of deaths involving specific drug categories, were compared for all sample years (1999–2014). Adjusted prevalences were calculated as , from Eq. (3), and the number of deaths as from (4). Full results are detailed in Supplement figures A6 through A9. The primary findings are as follows.
First, adjusted prevalences and numbers of deaths exceeded the reported counterparts for all years and drug categories. Second, psychotropic and combination drug prevalence rose fairly steadily throughout the analysis period, as did sedative and opioid involvement through 2010 and 2011. Conversely, cocaine prevalence decreased sharply until 2010 and then leveled out while heroin involvement declined through 2006 but increased thereafter, and dramatically beginning in 2011. However, since the number of fatal overdoses grew rapidly over time, from 16,849 in 1999 to 47,055 in 2014, deaths involving particular drugs could rise even with flat or declining prevalences. For instance, drug fatalities involving cocaine grew 40% (from 5076 to 7131) between 1999 and 2014, even while prevalence fell from 30% to 15%. Conversely, rising prevalences reinforce this effect so that, for example, deaths involving psychotropic drugs more than tripled (from 3577 to 12,837) while the prevalence rose “just” 28% (from 21.2% to 27.3%). Particularly noteworthy is the recent explosion of fatal heroin overdoses: the estimated number of deaths rose 18% (from 2342 to 2757) between 1999 and 2006, by an additional 53% (to 4214) in 2010, and another 235% (to 14,103) in 2014. Finally, while growth has not been particularly rapid, opioids remained the most common category involved in fatal overdoses – growing from 5390 deaths in 1999 to 24,769 in 2014.13
Third, in relative terms, death certificate reports understated prevalences most severely for sedatives, combination drug use and, to a lesser extent, psychotropic medications, but with the greatest growth over time in this disparity for heroin. An important consequence of this last result is that the rapid recent rise in heroin-related deaths is understated using death certificate reports. The largest absolute (rather than relative) disparity between adjusted and reported prevalences or numbers of deaths occurred for opioids and multiple drug involvement – reaching 7354 and 7535 deaths respectively, in 2011, before declining to 5876 and 6996 in 2014 – but also with substantial gaps for sedatives and psychotropics (5351 and 3528 deaths in 2011) and, recently, for heroin (3529 fatalities in 2014).14
3.4. Drugs responsible for the increase in fatal overdoses
The adjusted prevalences were next used to provide information on the drug categories most responsible for the rise in fatal drug poisonings. Table 2 summarizes results for 1999–2014. To illustrate, there were 16,894 fatal drug poisonings in 1999 and 47,055 in 2014, a growth of 30,206. Opioids were estimated to be involved in 5390 of these deaths in 1999 and 24,769 in 2014, an increase of 19,380 (95% CI, 18,459–20,301). Thus, based on “any” involvement, opioids were estimated to be “responsible” for 64.2% (19,380/30,206) of the rise in fatal overdoses (95% CI, 61.1%-67.2%). This method attributes to opioids all of the growth in deaths that involve them in some way. However, as mentioned, the sum of all “any involvement” contributions exceeds 100%. The lower panel of Table 2 therefore focuses on exclusive use. For example, 2300 drug poisoning deaths only involved opioids in 1999 versus 9099 in 2014, a difference of 6800 (95% CI, 6,187–7,412) or 22.5% (95% CI, 20.5–24.5%) of the total increase in overdose fatalities over the period.
Table 2.
Estimated changes of drug involvement in drug poisoning deaths: 1999 to 2014.
| Drug Category | Δ in # Deaths |
% of total Δ Explained |
||
|---|---|---|---|---|
| Estimate | 95% Confidence interval | Estimate | 95% Confidence interval | |
| Any Involvement | ||||
| Opioid Analgesics | 19,380 | [18,459–20,301] | 64.2 | [61.1 - 67.2] |
| Heroin | 11,760 | [10,666–12,855] | 38.9 | [35.3 - 42.6] |
| Cocaine | 2055 | [1441–2669] | 6.8 | [4.8 - 8.8] |
| Other Narcotics | -967 | [−2030 −96] | -3.2 | [-6.7- 0.3] |
| Sedatives | 11,173 | [10,452–11,893] | 37.0 | [34.6 - 39.4] |
| Psychotropics | 9,260 | [8529–9991] | 30.7 | [28.2 - 33.1] |
| Antidepressants | 4,321 | [3882–4759] | 14.3 | [12.9 - 15.8] |
| Antipsychotics | 1,915 | [1666–2164] | 6.3 | [5.5 - 7.2] |
| Psychostimulants | 4,440 | [3919–4961] | 14.7 | [13.0 - 16.4] |
| Other Specified | 3,271 | [2934–3608] | 10.8 | [9.7 - 11.9] |
| Unspecified | 12,209 | [10,797–13,622] | 40.4 | [35.7 - 45.1] |
| Exclusive Involvement | ||||
| Opioid Analgesics | 6800 | [6187–7412] | 22.5 | [20.5 - 24.5] |
| Heroin | 5388 | [4653–6122] | 17.8 | [15.4 - 20.3] |
| Cocaine | 42 | [-210 - 294] | 0.1 | [-0.7 - 1.0] |
| Sedatives | 367 | [240 - 495] | 1.2 | [0.8 - 1.6] |
| Psychotropics | 2181 | [1790 – 2572] | 7.2 | [5.9–8.5] |
| Antidepressants | -13 | [-173 - 147] | 0.0 | [-0.6 -0.5] |
| Antipsychotics | 114 | [57 - 170] | 0.4 | [0.2 - 0.6] |
| Psychostimulants | 1937 | [1621–2254] | 6.4 | [5.4–7.5] |
| Other Specified | 707 | [519 - 895] | 2.3 | [1.7 - 3.0] |
| Unspecified | 1004 | [900–1109] | 3.3 | [3.0 - 3.7] |
| >1 Drug Category | 16,778 | [15,914–17,641] | 55.5 | [52.7 - 58.4] |
Note: See note on Table 1. Estimates are based on adjusted prevalences. Δ in # Deaths is the difference between 2014 and 1999 deaths involving the specified drug. % of Total Δ Explained is Δ in # Deaths divided by 30,206 (the increase in drug poisoning deaths between 2014 and 1999). Confidence intervals are based on robust standard errors calculated with clustering at the county level.
Based on any involvement, opioids played the most important role in accounting for 64% of the rise in drug fatalities from 1999–2014 (95% CI, 61%-67%). Even with the adjustment procedures, unspecified drugs explained 40% of the growth (95% CI, 36%-45%), while heroin, sedatives and psychotropic drugs each accounted 28% to 43% of the trend.
Corresponding calculations using exclusive involvement revealed much lower contributions but also important differences in the patterns. Opioids continued to be responsible for the largest portion of the growth (23%; 95% CI, 21%-25%) but only slightly more than heroin (18%; 95% CI, 15–20%). Exclusive involvement of sedatives explained almost none of the change, while lone use of psychotropics accounted for 7% (95% CI, 6–9%), almost all due to psychostimulants. The key role of drug cocktails in being responsible for 56% of the rise in drug deaths (95% CI, 53–58%) is reiterated in the last row of the table, again emphasizing the importance of better understanding such cases.
Lower estimates were generally obtained when basing the calculations on reported rather than adjusted prevalences. For instance, any opioid or heroin involvement were estimated to account for 49% and 29%, and combination drug use for 40%, of the overall growth in fatal overdoses, between 1999 and 2014, based on death certificate reports, versus 64%, 39% and 56% when using adjusted prevalences (see Supplement table A6 for details). This was expected since attribution, based on death certificate mentions, would be understated due to cases where no specific drug was identified.
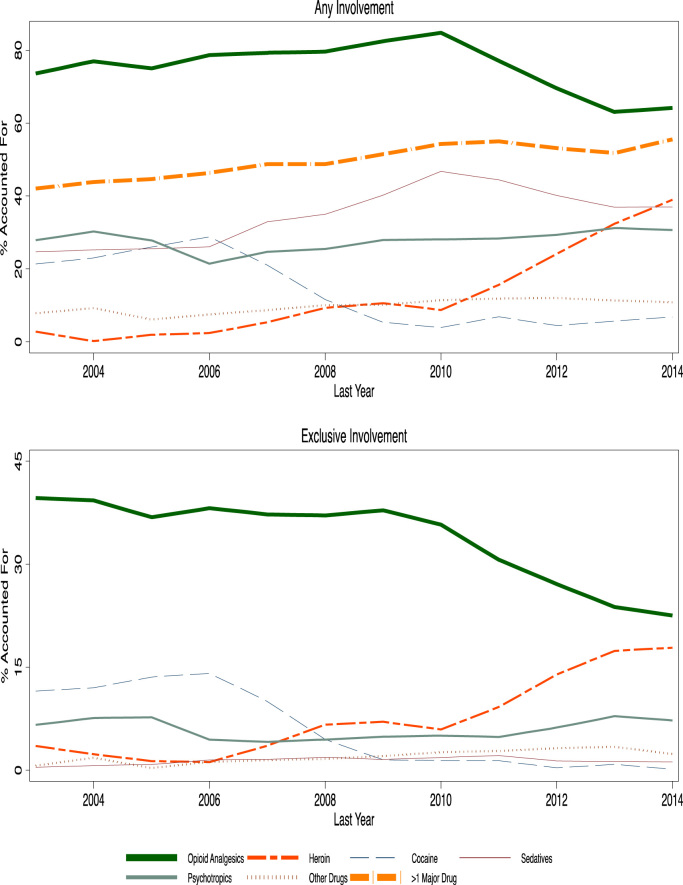
Examination of the 1999–2014 period reflects data availability rather than any theoretical justification. Therefore sensitivity of the results to the use of alternative analysis windows was evaluated. Fig. 1 summarizes estimated effects for periods that start in 1999 and end in the year specified on the X-axis. For instance, the left-most entry is for 1999–2003 while that farthest to the right covers the full 1999–2014 period.
Fig. 1.
: Change in overdose deaths accounted For: 1999 through Stated Year.
Opioids were most important for all sub-periods, but less so for those that included the recent years: any opioid involvement “explained” 74%-85% of the growth in deaths for windows ending between 2003 and 2010, compared to 64% for the full (1999–2014) period.15 The role of exclusive opioid analgesic involvement fell virtually monotonically with the addition of later years, from 40% for 1999–2003 to 23% for 1999–2014. This occurred because the importance of combination drug use rose fairly steadily, from 42% for 1999–2003 to 56% for 1999–2014.
The other notable results in Fig. 1 relate to illicit narcotics, with the role for cocaine falling and of heroin rising as more recent years were included. Specifically, any cocaine involvement “explained” 21%-29% of the rise in overdose deaths for periods ending between 2003–2007, and exclusive mentions accounted for 10%-14%, but they were of almost no importance when the final year is 2009 or later. By contrast, heroin played little role for periods concluding before 2007 but became more consequential with the inclusion of subsequent years, particularly those after 2010: any heroin involvement accounted for 9% of the total change from 1999–2010 but 39% from 1999–2014, with exclusive involvement responsible for 6% and 18% respectively. Results for the other drug classes were less sensitive to the choice of periods, except for the continued rise in the explanatory power of sedative involvement over time. However, sedatives were almost never exclusively responsible for drug deaths.
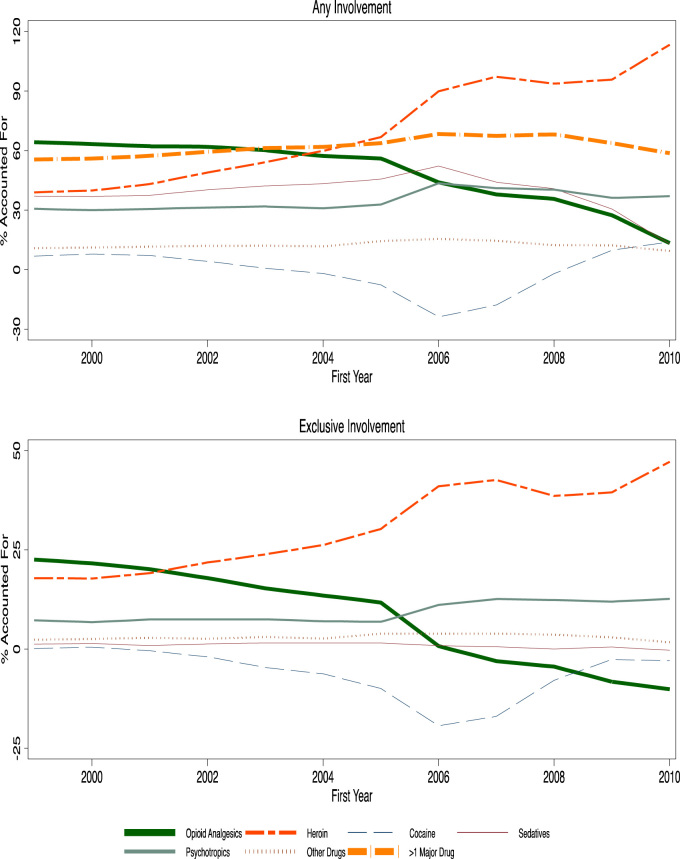
Fig. 2 summarizes an alternative way of examining the data, where the ending year was always 2014 but the starting year varied. Doing so yielded remarkable changes. In particular, any opioid involvement became less important for more recent starting years and accounted for less of the growth in overdose deaths than heroin, sedatives, and psychotropics when the first year analyzed was later than 2003, 2004 and 2005 respectively. Conversely, heroin made the largest contribution for analyses starting after 2003 and exclusive heroin involvement explained more of the rise than lone use of opioids for all periods beginning after 2001: any (exclusive) heroin involvement accounted for 60%, 97% and 113% (26%, 43% and 47%) of the growth in drug deaths for analysis windows starting in 2004, 2007 and 2010.
Fig. 2.
Change in overdose deaths accounted for: stated year through 2014.
Multiple drug use was always important, being responsible for 56% of the rise in drug deaths from 1999–2014 and 62%, 67% and 59% of the increase when starting the analysis in 2004, 2007 and 2010. The contribution of psychotropic medications also rose when focusing on more recent years, from 31% for any involvement for 1999–2014 to 44% for 2006–2014, with exclusive involvement contributing 7% and 11%. The patterns were more variable for other drugs, which usually also had less explanatory power.
Table 3 further details these differences by showing results for the equal length sample sub-periods 1999–2006 and 2007–2014. During the earlier timespan, any opioid involvement accounted for 79% (95% CI, 74%-83%) of the rise in drug deaths and exclusive use for 38% (95% CI, 35–41%). Conversely, in the later period, heroin played the dominant role with any involvement accounting for 97% (95% CI, 89%-106%) of the change and exclusive use for 43%, (95% CI, 36%-49%). Combination drug use also became more important in the later period, accounting for 67% (95% CI, 60%-74%) of the increase from 2007–2014 vs. 46% (95% CI, 43%-50%) from 1999–2006, as did psychotropic medications, particularly psychostimulants, whereas the role of cocaine involved deaths declined sharply. The contribution of sedatives grew over time, but only in combination with other drugs.
Table 3.
Percent of change in drug poisoning deaths explained, 1999 to 2006 and 2007 to 2014.
| Drug category | 2006 vs. 1999 |
2014 vs. 2007 |
||
|---|---|---|---|---|
| Estimate | 95% Confidence Interval | Estimate | 95% Confidence Interval | |
| Any Involvement | ||||
| Opioid Analgesics | 78.7 | [74.4 - 83.0] | 37.9 | [31.7 - 44.1] |
| Heroin | 2.4 | [-0.5 - 5.3] | 97.2 | [88.6 - 105.9] |
| Cocaine | 28.8 | [26.1 - 31.5] | -17.8 | [-22.7 - -12.9] |
| Other Narcotics | 1.3 | [-2.5 - 5.1] | -6.5 | [-14.6 - 1.6] |
| Sedatives | 26.0 | [22.6 - 29.5] | 44.1 | [37.2 - 50.9] |
| Psychotropics | 21.4 | [18.9 - 23.9] | 41.0 | [34.6 - 47.5] |
| Antidepressants | 11.8 | [9.7 - 14.0] | 13.2 | [8.8 - 17.7] |
| Antipsychotics | 5.9 | [4.8 - 7.0] | 5.1 | [2.4 - 7.7] |
| Psychostimulants | 6.0 | [4.6 - 7.4] | 30.5 | [26.8 - 34.2] |
| Other Specified | 7.5 | [5.8 - 9.2] | 14.6 | [11.7 - 17.5] |
| Unspecified | 32.8 | [28.0 - 37.5] | 48.5 | [38.5 - 58.4] |
| Exclusive Involvement | ||||
| Opioid Analgesics | 38.2 | [34.9 - 41.4] | -3.0 | [-8.3 - 2.3] |
| Heroin | 1.2 | [.0 - 2.4] | 42.6 | [36.1 - 49.1] |
| Cocaine | 14.1 | [12.3 - 15.9] | -17.0 | [-19.8 - -14.1] |
| Sedatives | 1.5 | [0.8 - 2.1] | 0.6 | [-0.5 - 1.7] |
| Psychotropics | 4.4 | [3.0 - 5.9] | 12.6 | [9.7 - 15.5] |
| Antidepressants | 0.3 | [-.6 - 1.2] | -0.4 | [-1.7 - .9] |
| Antipsychotics | 0.9 | [.6 - 1.2] | -0.4 | [-0.9 - .2] |
| Psychostimulants | 2.7 | [1.8 - 3.6] | 13.1 | [11.0 - 15.2] |
| Other Specified | 1.2 | [0.4 - 2.0] | 3.9 | [2.4 - 5.4] |
| Unspecified | 3.7 | [3.2 - 4.3] | 2.2 | [1.2 - 3.3] |
| >1 Drug Category | 46.3 | [42.6 - 50.1] | 67.4 | [60.4 - 74.4] |
4. Discussion
This study investigated which drug categories were responsible for the growth in fatal overdoses between 1999 and 2014 or sub-periods. Three challenges were encountered when attempting to answer this seemingly simple question. First, current death certificate data are problematic for understanding the drug poisoning epidemic, with a particular issue being the frequency that no specific drug was identified (Slavova et al., 2015). Second, combinations of drugs were often involved. This makes it difficult to assign responsibility to individual drug categories, or possibly meaningless to do so if the effects were interactive. It also implies that the contributions of drug categories, based on “any mentions”, will sum to more than 100% of the total number or change over time in drug deaths. Third, the contributions of different drugs depend on the time period analyzed.
Each of these issues was addressed above. Predictive methods previously developed by Ruhm (2016a) were extended and implemented to deal with the incompleteness of reporting. The involvement of drug combinations was carefully examined, with a distinction made between any versus exclusive drug involvement. Finally, a thorough investigation of the sensitivity of the results to the choice of analysis periods was provided.
The findings have important implications. The number of U.S. residents dying from drug poisonings rose from 16,849 in 1999 to 47,055 in 2014. In all years analyzed, opioids were the most common class of drugs involved, justifying ongoing actions to reduce the negative consequences associated with their use. These efforts have met with some success: the number of fatal overdoses involving opioids declined 7% from 2011–2013 (from 24,271 to 22,501), before rising in 2014 (to 24,769). However, the total number of drug poisoning deaths has continued to grow, from 41,340 in 2011 to 47,505 in 2014, and fatal overdoses increased in every year since 1990, even as the involvement of specific drugs changed.16 For example, deaths involving cocaine fell 30% (from 10,133 to 7,131) from 2006–2014 whereas heroin-involved fatalities skyrocketed by 498% (from 2,360 to 14,103) between 2004–2014, with most of this growth since 2010.
A key finding is that a majority of overdose fatalities involved multiple drug classes, complicating the attribution of the secular increase to specific drugs. Combination drug use itself is likely to be a risk factor. For example, sedatives were estimated to be involved in 11,843 deaths in 2014 versus just 1,847 in 1999, but were virtually never the only drug implicated. While the health risks of using benzodiazepines and opioids together are almost certainly greater than of either in isolation (Jones et al., 2012, Park et al., 2015), the effects of interactions between drug types more generally remains poorly understood. This is an important area for future research. In addition, although the modest decline since 2011 in opioid-related mortality has been accompanied by an enormous increase in deaths involving heroin, the evidence is mixed on whether these are substitutes (Cicero et al., 2012, Markon and Crites, 2014, Powell et al., 2015) or complements (Rudd et al., 2014, Compton et al., 2016).
Attribution of the secular increase in fatal overdoses to specific drug categories also depended on the time period analyzed. Because deaths involving opioids rose extremely rapidly at the start of the 21st century (from 5,275 in 1999 to 22,015 in 2009), they were “responsible” for a large percentage of growth in drug poisoning fatalities for any period beginning at or near 1999, regardless of the ending year. Conversely, heroin played the most important role for periods starting after 2003, and even earlier when basing the calculations on exclusive drug involvement. This reflects the very rapid growth in heroin-related fatalities since the mid-2000s. However, the role of combination drug use is again worth emphasizing. It explained 40%-60% of the growth in drug deaths and became more important in recent years. The design of effective policies to reduce fatal drug poisonings therefore needs to reflect for the important role of drug cocktails.
These findings should be interpreted in light of several limitations. First, the adjustment procedures used to account for overdose deaths where no drug was specified on the death certificate work well but not perfectly. This would raise particular concern if patterns of drug involvement varied across cases with and without specific drug mentions in ways not captured by the explanatory variables. However, county-year average drug specification rates were by far the most important predictor. These vary depending on whether coroners or medical examiners complete the death certificates and if there is centralized oversight of the process by a Chief Medical Examiner (Warner, Paulozzi, Nolte, Davis & Nelson, 2013). However, they are unlikely to be strongly influenced by unobserved individual determinants of drug involvement.17 Second, some overdose deaths might be misclassified as being due to non-drug causes or vice versa. Third, death certificates may be incomplete, even when drugs are specified. For example, there is some indication that more detailed reporting would raise the estimated involvement of sedatives, psychotropics and combination drug use by more than for opioids, heroin or cocaine (Ruhm, 2016b). Fourth, there may be inaccuracies even when specific drugs are reported. For instance, heroin metabolizes into morphine and codeine and so its use may sometimes be attributed to those drugs (Mertz, Janssen & Williams, 2014).
Finally, the ICD-10 codes provide limited information on the specific drugs involved in fatal overdoses with, for example, oxycodone, hydrocodone and morpehene all being placed in the same category (ICD-10 code, T40.2). This has led to recommendations to add detail to death certificates on the drugs involved, toxicology levels, ICD categories, as well as more carefully distinguishing between cases where a given drug is the cause of mortality versus those where it was detected but not a major contributor to the death (Webster and Dasgupta, 2011, Goldberger et al., 2013). Recent research using textual information on death certificates, rather than ICD codes (Ossiander, 2014, Warner et al., 2016), confirms the importance of poly-drug use and can more fully identify the use of multiple drug types within classes (e.g. combined involvement of oxycodone and hydrocodone). However, these studies cover a relatively short time period and do not account for fatalities where no specific drug is identified on the death certificate.
Notwithstanding these qualifications, this analysis highlights the key role of drug “cocktails” in accounting for the rise in fatal overdoses – emphasizing the importance of better understanding the risk factors associated with such combined drug use – as well as the explosive recent growth in drug deaths involving heroin.
Acknowledgement
I thank participants of the Southeastern Health Economics Study Group, Caribbean Health Economics Symposium, Tulane University Innovation and Behavior in Health Markets Conference, Emory University and University of North Carolina at Greensboro for helpful comments on earlier versions of this research.
Footnotes
The term “overdoses” is used for convenience, while recognizing that some drug poisoning deaths are intentional.
Poisoning deaths included ICD-10 UCD codes X40-X49, X60-X69, X85-X90 Y10-Y19, Y35.2, *U01(.6–.7); UCD codes for drug poisoning deaths were X40-X44, X60-X64, X85, Y10-Y14, Y35.2, *U01(.6–.7), (World Health Organization, 2014).
Common opioid analgesics are oxycodone, methadone, hydrocodone and fentanyl. Antipsychotic medications include drugs such as: Thorazine (chlorpromazine), Compazine (prochlorperazine) and Haldol (haoperidol). Pschostimulants include methamphetamines, amphatamine salts (e.g. Adderall) and methylphenidates such as Ritalin and Concerta. Benzodiazepines, such as Valium (diazepam) and Xanax (alprazolam), are the most important subclass of sedatives, accounting for 84% of sedative-involved fatal overdoses in 2012 (Ruhm, 2016a).
Psychotropics may be most important in this regard, since this category includes heterogeneous types of drugs. Warner, Trinidad, Bastian, Minino, and Hedegaard (2016) provide evidence that multiple types of opioids are frequently involved in fatal drug poisonings.
Education was sometimes reported in years rather than specific thresholds. In these cases, ≤11, 12, 13–15 and ≥16 years were classified as less than high school graduate, high school graduate, some college and college graduate.
Thus, the estimated prevalence in this case is: .
Shorter analysis periods were not examined since such estimates would be dominated by noise.
Population data (the denominator in the mortality rate calculations) came from the National Cancer Institute's Surveillance Epidemiology and End Results (SEER) program and were designed to supply more accurate population estimates for intercensal years than standard census projections. See http://www.seer.cancer.gov/data for details.
The characteristics of deaths where no drug was specified differed substantially from those where ≥1 drug was mentioned. As expected, mean values of were much lower in the former cases (52.5% vs. 87.2%). In addition, lack of specificity was relatively common for males, non-Hispanic whites and those residing in the Mid-Atlantic, East South Central or West South Central census regions, while being relatively uncommon for those in the New England or South-Atlantic regions. Full details are provided in Supplement Table A1.
Drug involvement for the 4911 non-drug poisoning deaths occurring in 2014 was also examined. A drug was mentioned on the death certificate in 236 (4.8%) of these cases, with most (118) being an unspecified drug and with a specific drug mentioned just 2.9% of the time (143 deaths).
Reported Drug involvement rates for 2014 fatal overdoses were also compared across low- and high-diagnosis counties, defined as those where was ≤68.4% and ≥98.2% (the bottom and top quartiles of the population-weighted distribution). Differences in reported prevalences, displayed in Supplement table A2, were dramatic. For example, opioids were mentioned 2.7 times as often in high- versus low-diagnosis counties (52.8% vs. 19.5%), with even larger relative differences for heroin, cocaine, and sedative mentions, and with multiple drug use prevalence being almost four times greater. No drug was specified in 54% of fatal overdoses in low-diagnosis but in <1% of high-diagnosis counties. This comparison does not account for potential confounders, which could be important since deaths in low-diagnosis counties were more likely to involve females, whites and married individuals.
Manner of death or use of autopsies could be endogenous (e.g. if the latter were more commonly performed in high diagnosis counties). Information on autopsies first became available on death certificates in 2003.
The patterns described in this paragraph and the next refer to point estimates, rather than 95% confidence intervals.
Patterns of exclusive and combination drug use were also examined, using adjusted prevalences, for 1999, 2006 and 2014. Full results are provided in Supplement table A5. This investigation further emphasizes the importance of drug “cocktails”. Exclusive drug involvement occurred less than half the time for all categories and years and was particularly rare for sedatives. The specific drug combinations varied considerably across years. For instance, the percentage of opioid analgesic-involved deaths where sedatives were also implicated rose from 18.1% in 1999 to 38.1% in 2014 while simultaneous cocaine use became less frequent. Patterns for heroin differed somewhat, with much of the dramatic recent increase reflecting exclusive use – rising from 39% in 1999 to 45% in 2014 – while the fraction with combined involvement of opioids fell from 30% in 1999 to 22% in 2006, and that also involving cocaine declined from 38% in 2006 to 21% in 2014.
The fatality numbers in this section, other than the total number of drug deaths, are based on adjusted prevalences and so are measured with error.
As evidence of the central importance of SPECIFY, adjusted prevalence estimates quite similar to those presented above were obtained using a prediction model where it was the only explanatory variable (see Supplement Table A3).
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2017.01.009.
Appendix A. Supplementary material
Supplementary material
.
References
- Anderson R.N., Miniño A.M., Hoyert D.L., Rosenberg H.M. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep. 2001;49(2):1–32. [PubMed] [Google Scholar]
- Case A., Deaton A. (2015). Rising morbidity and mortality in midlife among white non-hispanic Americans in the 21st Century. PNAS 2015; published ahead of print November 2, doi:10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed]
- Centers for Disease Control and Prevention Vital Signs: Overdoses of prescription opioid pain relievers – United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Risk for overdose from methadone used for pain relief – United States, 1999-2010. MMWR. Morb Mortal Wkly Rep. 2012 July 6; 61(26):493-497. [PubMed]
- Centers for Disease Control and Prevention (2013). Opioids drive continued increase in drug overdose deaths February 20. 〈http://www.cdc.gov/media/releases/2013/p0220_drug_overdose_deaths.html〉.
- Centers for Disease Control and Prevention (2014). National Center for Health Statistics. Instructions for Completing the Cause-of-Death Section of the Death Certificate. 〈http://www.cdc.gov/nchs/data/dvs/blue_form.pdf〉. Accessed 22.08.17.
- Centers for Disease Control and Prevention (2016). Multiple Cause of Death 1999–2014. 〈http://wonder.cdc.gov/help/mcd.html〉, Accessed 15.06.17.
- ChiroCode Institute (2014). ICD-10-CM (ICD10) Diagnosis Codes – T Codes. 〈http://www.chirocode.com/medical-codes/icd-10-cm/icd-10-cm-diagnosis-T-codes.html〉.
- Cicero T.J., Ellis M.S., Surratt H.L. Effect of abuse-deterrent formulation of OxyContin. N Engl J Med. 2012;367(2):187–189. doi: 10.1056/NEJMc1204141. [DOI] [PubMed] [Google Scholar]
- Compton W.M., Jones C.M., Baldwin G.T. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finklea K.M., Bagalman E., Sacco L.N. Library of Congress, Congressional Research Service; Washington, DC: 2013. Prescription drug monitoring programs. [Google Scholar]
- Hardesty C. Office of National Drug Policy; Washington DC: 2014. White House Summit on the Opioid Epidemic.〈http://www.whitehouse.gov/blog/2014/06/19/white-house-summit-opioid-epidemic〉 (June 19) [Google Scholar]
- Goldberger B.A., Maxwell J.C., Campbell A., Wilford B.B. Uniform standards and case definitions for classifying Opioid-related deaths: Recommendations by a Samhsa consensus panel. J Addict Dis. 2013;32(3):231–243. doi: 10.1080/10550887.2013.824334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C.M., Logan J., Gladden R.M., Bohm M.K. Demographic and substance use trends among heroin users – United States, 2002–2013. Morb Mortal Wkly Rep. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- Jones C.M., Mack K.A., Paulozzi L.J. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–659. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- Jones J.D., Mogali S., Comer S.D. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125(1-2):8–18. doi: 10.1016/j.drugalcdep.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschner N., Ginsburg J., Sulmasy L.S. Health and Public Policy Committee of the American College of Physicians.Prescription drug abuse: Executive summary of a policy position paper from the American College of Physicians. Annals of Internal Medicine. 2014;160(3):198–200. doi: 10.7326/M13-2209. [DOI] [PubMed] [Google Scholar]
- Markon J., Crites A. Experts: Officials missed signs of prescription drug crackdown's effects on heroin use. Washington Post. 2014 (Mar 6) [Google Scholar]
- Mertz K.J., Janssen J.K., Williams K.E. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J Forensic Sciences. 2014;59(6):1583–1585. doi: 10.1111/1556-4029.12541. [DOI] [PubMed] [Google Scholar]
- Olsen Y. The CDC guideline on opioid prescribing: Rising to the challenge. JAMA. 2016;315(15):1577–1579. doi: 10.1001/jama.2016.1910. [DOI] [PubMed] [Google Scholar]
- Ossiander E.M. Using textual cause-of-death data to study drug poisoning deaths. American Journal of Epidemiology. 2014;179(7):884–894. doi: 10.1093/aje/kwt333. [DOI] [PubMed] [Google Scholar]
- Park T.W., Saitz R., Ganoczy D., Ilgen M., Bohnert A.S. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ. 2015;350:h2698. doi: 10.1136/bmj.h2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi L.J., Mack K.A., Hockenberry J.M. Vital signs: Variation among States in prescribing of opioid pain relievers and benzodiazepines – United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):563–568. [PMC free article] [PubMed] [Google Scholar]
- Powell D., Pacula R., Jacobson N. (2015). Do Medical Marijuana Laws Reduce Addictions and Deaths Related to Pain Killers?. National Bureau of Economic Research Working Paper 21345. [DOI] [PMC free article] [PubMed]
- Rannazzisi J. (2013). Testimony for “Curbing Prescription Drug Abuse in Medicare”. Hearing before the Committee on Homeland Security and Governmental Affairs, United States Senate, 113th Congress, June 24, retrieved from: 〈http://www.gpo.gov/fdsys/pkg/CHRG-113shrg82571/pdf/CHRG-113shrg82571.pdf〉.
- Rudd R.A., Aleshire N., Zibbell J.E., Gladden R.M. Increase in drug and opioid overdose deaths – United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50/51):1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Rudd R.A., Paulozzi L.J., Bauer M.J., Burleson R.W., Carlson R.E., Dao D. Increase in Heroin Overdose Deaths – 28 States, 2010 to 2012. MMWR Morb Mortal Wkly Rep. 2014;63(39):849–854. [PMC free article] [PubMed] [Google Scholar]
- Ruhm C.J. Drug Poisoning Deaths in the United States, 1999–2012: A statistical adjustment analysis. Popul Health Metr. 2016;14(2) doi: 10.1186/s12963-016-0071-7. (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm C. Taking the measure of a fatal drug epidemic. National Bureau of Economic Research Working Paper No. 22504, August 2016. (2016b).
- Slavova S., O’Brien D.B., Creppage K., Dao D., Fondario A., Haile E., Hume B., Largo T.W., Nguyen C., Sabel J.C., Wright D. Members of the Council of State and Territorial Epidemiologists Overdose Subcommittee. Drug overdose deaths: Let's get specific. Public Health Rep. 2015;130(4):339–342. doi: 10.1177/003335491513000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Frieden T.R., Hyde P.S., Cha S.S. Medication-assisted therapies – Tackling the opioid overdose epidemic. N Engl J Med. 2014;370(22):2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Warner M., Chen L.H., Makuc D.M., Anderson R.N., Miniño A.M. National Center for Health Statistics; Hyattsville, MD: 2011. Drug poisoning deaths in the United States, 1980–2008. (NCHS data brief, no 81) [PubMed] [Google Scholar]
- Warner M., Paulozzi L.J., Nolte K.B., Davis G.G., Nelson L.S. State variation in certifying manner of death and drugs involved in drug intoxication deaths. Acad Forensic Pathol. 2013;3(2):231–237. [Google Scholar]
- Warner M., Trinidad J.P., Bastian B.A., Minino A.M., Hedegaard H. Drugs Most Frequenlty Involved in Drug Overdose Deaths: United States, 2010–2014. Natl Vital Stat Rep. 2016;65(10):1–15. [PubMed] [Google Scholar]
- Webster L.R., Dasgupta N. Obtaining adequate data to determine causes of opioid-related overdose deaths. Pain Med. 2011;12(Suppl 2):S86–S92. doi: 10.1111/j.1526-4637.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2014). International Classification of Diseases (ICD). 〈http://www.who.int/classifications/icd/en/〉.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material