Abstract
Performance-based financing (PBF) programs are increasingly implemented in low and middle-income countries to improve health service quality and utilization. In April 2011, a PBF pilot program was launched in Boulsa, Leo and Titao districts in Burkina Faso with the objective of increasing the provision and quality of maternal health services. We evaluate the impact of this program using facility-level administrative data from the national health management information system (HMIS). Primary outcomes were the number of antenatal care visits, the proportion of antenatal care visits that occurred during the first trimester of pregnancy, the number of institutional deliveries and the number of postnatal care visits. To assess program impact we use a difference-in-differences approach, comparing changes in health service provision post-introduction with changes in matched comparison areas. All models were estimated using ordinary least squares (OLS) regression models with standard errors clustered at the facility level. On average, PBF facilities had 2.3 more antenatal care visits (95% CI [0.446–4.225]), 2.1 more deliveries (95% CI [0.034–4.069]) and 9.5 more postnatal care visits (95% CI [6.099, 12.903]) each month after the introduction of PBF. Compared to the service provision levels prior to the interventions, this implies a relative increase of 27.7 percent for ANC, of 9.2 percent for deliveries, and of 118.7 percent for postnatal care. Given the positive results observed during the pre-pilot period and the limited resources available in the health sector, the PBF program in Burkina Faso may be a low-cost, high impact intervention to improve maternal and child health.
Keywords: Performance-based financing, Results-based financing, Health services, Provider incentives, Burkina Faso
Highlights
-
•
PBF increased provision of three key reproductive health services in Burkina Faso.
-
•
Future research should examine the mechanisms through which PBF increases service provision.
-
•
PBF in Burkina Faso may be a low-cost, high impact intervention to improve maternal and child health.
1. Introduction
Reducing maternal and child mortality remains a priority of the international development community as demonstrated by the 2015 launch of the Global Strategy for Women’s, Children’s and Adolescents’ Health (Kuruvilla et al., 2016). Despite recent increases in the use of maternal health services as well as recent improvements in maternal and child health, reaching targeted coverage for key health services such as deliveries or early antenatal care remains challenging in many countries (The World Health Organization & UNICEF, 2014; United Nations, 2014). According to the most recent Demographic and Health Survey data from Sub-Saharan Africa data, only 50% of women received the recommended four ANC visits per pregnancy, and 42% of children were not delivered at a health facility (ICF International, 2012). The situation is similar in rural Burkina Faso, where 69% of women did not receive four or more antenatal visits and almost 40% of women gave birth at home as of 2010 (ICF International, 2012).
The reasons for continued low maternal health service use are complex, but appear to include high user fees and poor quality of care in many settings (Hatt et al., 2013, Nair et al., 2014). A wide-variety of programs have been introduced to address these barriers including interventions focused on changing demand (conditional-cash transfers, vouchers, user-fee exemptions, health insurance) and supply-side interventions (financing, targeted subsidies) (The AIDSTAR-Two Project, 2011). Performance-Based Financing (PBF) has been implemented in an increasingly large number of low- and middle income countries to strengthen health systems and increase service provision (The AIDSTAR-Two Project, 2011). PBF is a form of supply-side Results-Based Financing that uses fee-for-service contracts with a service quality component (Fritsche, Soeters, & Meessen, 2014). PBF aims to improve health service provision and quality by increasing staff motivation, reducing provider absenteeism, and increasing the financial independence of facilities, which can allow them to improve the quality of their services, and also potentially reduce users fees (The World Bank, 2012). Recent PBF programs have introduced additional demand-side interventions such as using household visits by health workers to stimulate demand, referrals by community health workers, and the removal of user and drug fees for the poor and vulnerable. While the term PBF first originated in Rwanda, early programs with some of the same tenants as PBF such as contracting and decentralization emerged in the 1990s in Zambia and Cambodia (Bossert et al., 2003, Soeters and Griffiths, 2003). Since the mid-2000s, and in particular after the positive results from the Rwanda program (Basinga et al., 2010), there has been a rapid increase in the number of countries integrating performance-based financing into their health system. As of 2013, over 40 countries have either planned or begun to implement some form of PBF (Fritsche et al., 2014).
A somewhat controversial Cochrane review published in 2012 analyzed nine studies on PBF, and concluded that the existing evidence base was too weak to draw any general conclusions (Meessen, 2012, Witter et al., 2012). More recent PBF programs have generally incorporated more rigorous evaluation designs and several randomized or quasi-experimental studies published since 2010 have increased the quality of available evidence considerably. While a study conducted in the Democratic Republic of the Congo found no effect of PBF on health service utilization (Huillery and Seban, 2014), studies conducted in Rwanda, the Philippines and Tanzania found that PBF increased several, but not all, of the health services examined in these studies (Basinga et al., 2010, Binyaruka et al., 2015, Peabody et al., 2014). Three studies conducted in Burundi found mixed results with findings differing between studies (Bonfrer et al., 2014, Bonfrer et al., 2014, Falisse et al., 2015). While two of the three studies from Burundi found an increase in institutional deliveries and antenatal care, none of the three studies found an increase in vaccinations and only one of the two studies that examined contraception found an increase in this outcome. Three studies from the Philippines, Haiti and Cambodia found positive results for all health services they examined though one of these studies focused exclusively on institutional deliveries (Gertler and Giovagnoli, 2014, Ir et al., 2015, Zeng et al., 2013). Most of these studies focus on maternal and child health service use and few examine health outcomes or quality of the health services provided.
In this paper we examine the effect of a pilot project that introduced Performance-Based Financing from 2011 to 2013 in Burkina Faso. We focus on provision of maternal health services as a key strategy to improve maternal and child health outcomes in the country and globally (Jones et al., 2003, Rosenfield et al., 2006).
2. Methods
2.1. Study setting
Burkina Faso remains one of the poorest countries in the world, with maternal mortality rates of 400 per 100,000 live births and under-5 mortality rate of 96 per 1000 live births in 2013 (UNICEF, 2013). The health system in Burkina Faso is divided into three levels of care. At the highest level, regional hospitals (Centre Hospitalier Regional – CHR) exist in each of 11 of the 13 regions in Burkina Faso (Direction Generale Ministere de la Sante Burkina Faso, 2014). Below the regional level, Burkina Faso is divided into 63 health districts. In 2012 there were a total of 2495 district level primary care facilities (Centres de Santé et de Promotion Sociale – CSPS), and CSPS staffed with physicians (Centre Medical – CM). Secondary care facilities or district hospitals (Centre médical avec antenne chirurgicale – CMA) exist in each health district as well.
2.2. Study design
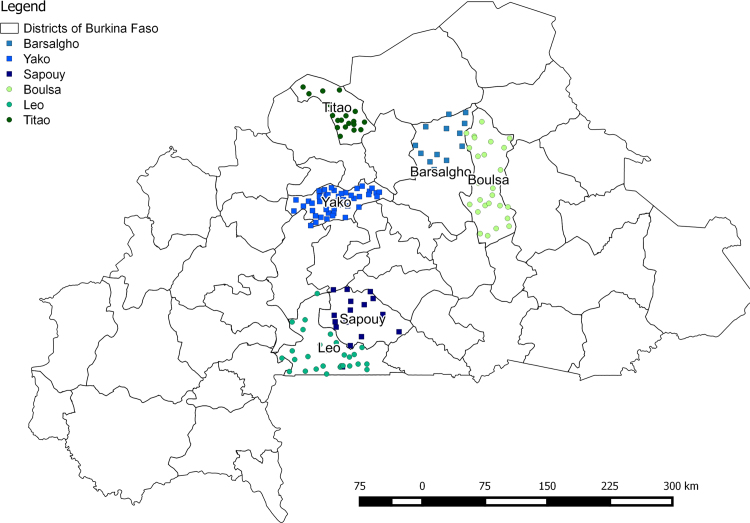
The PBF pilot began in Boulsa, Leo and Titao health districts in April 2011. We use a difference-in-differences design to assess the impact of the PBF program on the provision of essential maternal health services. The three intervention districts were chosen in 2010 by the Ministry of Health (MoH) for the PBF program; these districts were selected based on their health indicators for priority services, their poverty level, their distance from Ouagadougou (<300 km), and their health system characteristics (having a functioning district hospital and having between 15 and 30 primary health care centers). The study area includes three regions in Burkina Faso: North (Titao), Center-North (Boulsa), and Center-West (Leo). For each intervention health district we selected a comparison health district in the same region with comparable health, health system and socio-economic characteristics.
2.3. The intervention package
Before PBF, health facilities in Burkina Faso were financed primarily through funding provided from the Ministry of Health for specific health care resources outlined in annual health facility action plans, and from revenue generated from user fees and drug sales (Robyn et al., 2014). The pilot program changed the previous financing system by defining a package of key health services to be targeted at contracted primary- (CSPS, CM) and secondary-level (CMA) health facilities, and issuing payments based on quantity and quality for these services. Health facilities included in the pilot signed contracts with the central level of the Ministry of Health to provide these packages of services. A checklist which included items such as how well patient documentation was completed, the availability of health supplies equipment, and essential medicines, and adherence to national standards defining quality of care was used to create a quality score. The total payment was determined by multiplying the quality score by the number of each service provided, the payment amount associated with the service, and a measure of health facility characteristics.
The program approach evaluated in the pilot did not include some recommended elements of performance-based-financing including demand side incentives, independent management of the PBF program administration, an increase in health facility autonomy and the introduction of improved management tools. As of 2014, the PBF program approach changed to incorporate several additional design elements that are aligned with PBF guiding principles and best practices such as demand-side incentives and social marketing through household visits (Ministere de la Sante Burkina Faso, 2013). In this paper we evaluate the early PBF program approach in Burkina Faso. Appendix 1 lists the services and their prices for the primary and secondary levels of care. A description of the methods used to determine individual provider payments is provided in Appendix 2.
2.4. Study population
A total of 186 health facilities were included in the study: 168 primary health care centers (Centres de Santé et de Promotion Sociale – CSPS), 5 (Centre médical avec antenne chirurgicale), 2 (Centre Medical – CM), and 10 dispensaries (Fig. 1).
Fig. 1.
Intervention and comparison health facilities.
2.5. Data
All data used for this analysis were obtained from the health management information system (HMIS) of Burkina Faso. The HMIS system is a national database that collects health service delivery information from all public and most private and non-governmental health facilities. Health facilities are responsible for completing a health service use report each month that is transmitted to the district health office. Data from 2009 – 2012 were obtained from district-specific databases. The final database included 8,074 district-month observations. Several verification mechanisms existed in PBF health facilities taking part in the pilot: as a first-stage verification, the number of services declared by the health facility to the HMIS system was checked and verified by agents on a quarterly basis by counting services written in the facility registers. Second, a sample of patients was drawn for each type of service, with sampled patients being visited and interviewed (i) to ensure they received the services declared by the health facility, and (ii) to assess their satisfaction with the services provided.
2.6. Indicators
A wide range of health services were incentivized during the pilot study (Appendix 1). For analytical purposes, we focus on four key maternal health service indicators: the number of antenatal care visits, the proportion of antenatal care visits that occurred during the first trimester of pregnancy, the number of complicated and uncomplicated deliveries at the health facility, and the number of postnatal consultations occurring 42 days after pregnancy provided. Complicated deliveries were defined as pregnancies with abnormal fetal size or position resulting in difficult delivery. Uncomplicated deliveries were defined as spontaneous vaginal deliveries occurring when a pregnant female goes into labor without the use of drugs or techniques to induce labor, and delivers her baby in the normal manner, without forceps, vacuum extraction, or a cesarean section. For antenatal care, we focus on women completing at least 4 visits to capture the proportion of women meeting the WHO ANC standards. We chose to focus on maternal health services in this analysis as they have been identified as priority services for many performance-based financing evaluations, including a large randomized controlled trial planned in Burkina Faso.
2.7. Statistical analysis
The data set extracted covers the period from January 2009 to December 2012; PBF was formally started in April 2011; we therefore divide the overall sample into the pre-period from January 2009 – March 2011, and the post-period from April 2011 – December 2012.
Our empirical analysis compares pre-post differences between treated and comparison areas using a difference-in-differences regression model. The empirical model estimated can be characterized as:
where is number of services of interest provided by facility i of district d in time period t, time trend is a service-specific time trend capturing general trends over time, RBF is an indicator for a facility being in a treated district, post captures general average monthly change compared to the pre-intervention period, RBF*post captures the additional improvements in indicators observed in treated areas, are facility fixed effects and Month are calendar month indicators to control for seasonal fluctuations in service utilization. We assumed dependence of residuals from facility observations over time, and have therefore clustered standard errors at the facility level in all regression models.
To address the concern that more complete data from intervention facilities drives our results, we test whether removing health facilities that report missing data in any month for any of the three health services affects our results. The results from this model are presented in Appendix 3.
3. Results
Table 1 below presents baseline characteristics for intervention and matched control districts in 2010, the year before PBF began. While there are some differences in population size and the number of primary health facilities in matched districts, the number of facilities per 100,000 people was similar in the matched pairs in the pre-intervention period. The matched pairs also have similar literacy rates, and proportions of the population living close to a health facility; however, the poverty rate differs in the matched districts in Centre-Nord and Nord.
Table 1.
Health district characteristics, 2010a.
| Region | District | Treatment | Population | Number of health facilities | Number of health facilities per 100,000 people | Percent of the population less than 5 km from a health facility | Literacy rate | Poverty rate |
|---|---|---|---|---|---|---|---|---|
| Centre-Nord | Boulsa | Intervention | 365,473 | 28 | 7.66 | 0.30 | 87.0 | 0.439 |
| Centre-Nord | Barsalogho | Comparison | 163,320 | 11 | 6.74 | 0.30 | 90.8 | 0.606 |
| Centre-Ouest | Leo | Intervention | 233,315 | 31 | 13.29 | 0.42 | 83.2 | 0.504 |
| Centre-Ouest | Sapouy | Comparison | 199,934 | 17 | 8.50 | 0.34 | 87.8 | 0.578 |
| Nord | Titao | Intervention | 158,356 | 20 | 12.63 | 0.46 | 84.7 | 0.600 |
| Nord | Yako | Comparison | 353,315 | 42 | 11.89 | 0.50 | 88.1 | 0.375 |
Data from the Annuaire Statistique 2010, Ministère de la Santé, Burkina Faso
Table 2 shows the average number of the four health services examined here – 4th and 5th antenatal care visits, the proportion of first antenatal care visits that occurred during the first trimester of pregnancy, deliveries, and postnatal care visits – for health facilities by district during the pre-intervention period from January 2009 through March 2011. The mean facility level number of monthly deliveries ranged from 17 in Titao to 33 in Barsalogho. The monthly mean during the pre-intervention period among all three PBF districts was the same as the monthly mean in the intervention district (22). The mean number of monthly 4th and 5th facility prenatal visits was lowest in Yako, Leo and Titao (6) and highest in Barsalogho (15). Similar to deliveries, the monthly mean during the pre-period was the same for intervention and comparison districts (8). The mean proportion of first ANC visits provided to women in the first trimester of pregnancy ranged from 15% in Yako to 27% Sapouy. The proportion in intervention districts before the start of PBF was 23% compared to 19% in comparison districts. The number of postnatal care visits was lowest in Titao (3) and highest in Barsalogho (19). The monthly mean in the three intervention districts was 8 and the mean in comparison districts was 9 during the pre-period.
Table 2.
Average monthly health facility number of 4th and 5th prenatal visits, deliveries, and postnatal visits by health district during the pre-intervention period, January 2009 – March 2011.
| Region | District | Treatment | Na | Deliveries |
ANC Visits (4 or 5) |
First ANC in the first trimester |
Postnatal visits |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | sd | mean | sd | mean | sd | mean | sd | ||||
| Centre-Nord | Boulsa | Intervention | 31 | 28 | 16 | 12 | 13 | 0.24 | 0.21 | 12 | 18 |
| Centre-Nord | Barsalogho | Comparison | 14 | 33 | 13 | 15 | 10 | 0.21 | 0.18 | 19 | 12 |
| Centre-Ouest | Leo | Intervention | 35 | 19 | 15 | 6 | 6 | 0.20 | 0.20 | 7 | 9 |
| Centre-Ouest | Sapouy | Comparison | 18 | 24 | 18 | 11 | 9 | 0.27 | 0.18 | 9 | 9 |
| Nord | Titao | Intervention | 24 | 17 | 9 | 6 | 5 | 0.26 | 0.22 | 3 | 5 |
| Nord | Yako | Comparison | 51 | 18 | 17 | 6 | 6 | 0.15 | 0.18 | 6 | 8 |
| Intervention | 90 | 22 | 15 | 8 | 10 | 0.23 | 0.22 | 8 | 13 | ||
| Comparison | 83 | 22 | 17 | 8 | 8 | 0.19 | 0.19 | 9 | 10 | ||
The number of functioning health facilities varied over the study period; numbers in the figure represent the total number of health facilities that were open at any point during the study period in each district
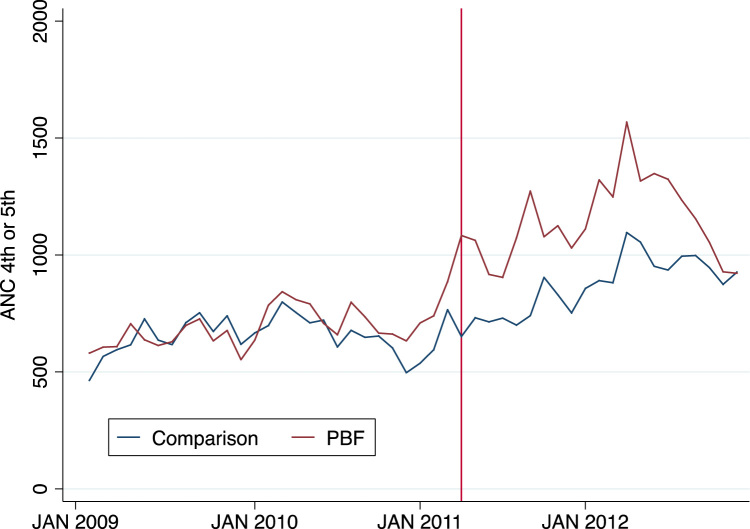
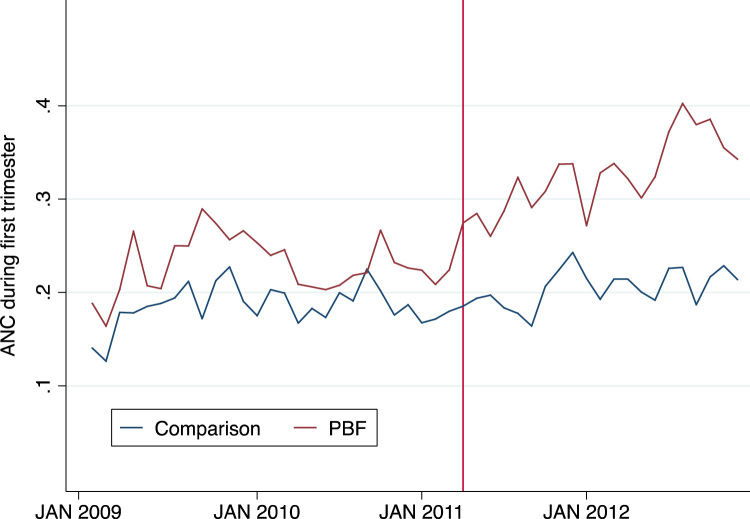
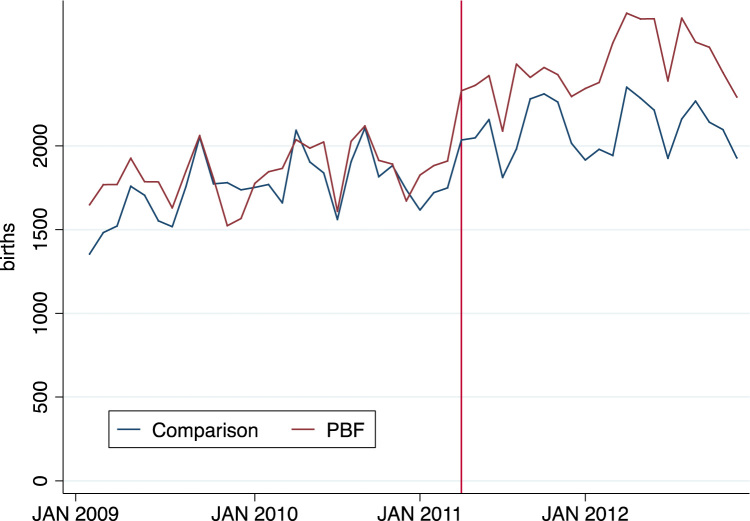
Table 3 presents our main impact estimates. On average, PBF facilities provided approximately two more 4th and 5th antenatal visits per month (2.336, 95% CI 0.446–4.225) compared to comparison facilities after the start of PBF. The proportion of first ANC visits provided to women in the first trimester of pregnancy increased by 8.5 percentage points more in PBF districts than comparison districts (0.085, 95% CI 0.043–0.126), institutional deliveries increased by two births per month (2.052, 95% CI 0.034–4.069) and PBF facilities on average completed 9.5 more postnatal care visits (9.501, 95% 6.099, 12.903) per month.
Table 3.
Post intervention and interaction term coefficients from difference-in-differences models, Burkina Faso January 2009 – December 2012.
| Dependent variable | 95% CI | Relative increase** | ||
|---|---|---|---|---|
| Four or five prenatal care visits | ||||
| PBF*post | 2.336* | [0.446, | 4.225] | =2.336/8.432=0.277 |
| N | 8074 | |||
| Percent of ANC visits occurring in the first trimester | ||||
| PBF*post | 0.085* | [0.043, | 0.126] | =0.085/0.229=0.371 |
| N | 8047 | |||
| Facility births | ||||
| PBF*post | 2.052* | [0.034, | 4.069] | =2.052/22.243=0.092 |
| N | 8074 | |||
| Postnatal visits | ||||
| PBF*post | 9.501* | [6.099, | 12.903] | =9.501/8.005=1.187 |
| N | 8074 | |||
p<0.05
Relative increase was calculated by dividing each indicator's interaction term by the pre-intervention mean in the PBF districts
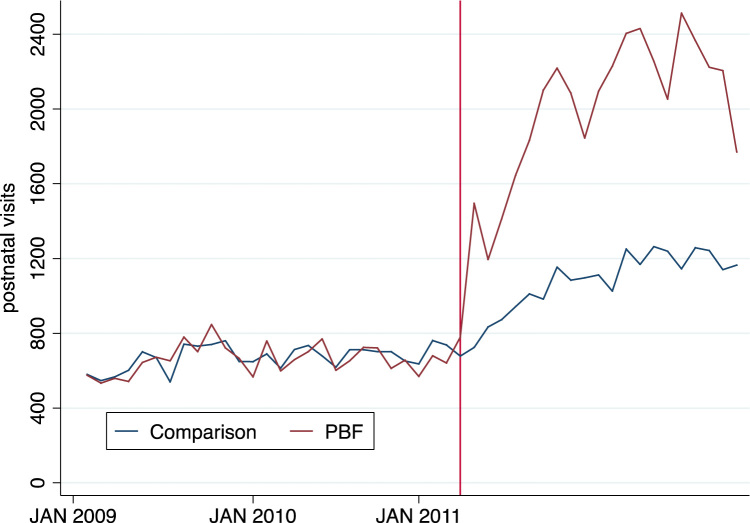
Fig. 2, Fig. 3, Fig. 4, Fig. 5 illustrate these results graphically. For all four indicators, the pre-intervention trends in PBF and comparison districts appear similar from January 2009 through March 2011, and then diverge significantly in the post-period.
Fig. 2.
Number of 4th or 5th antenatal care visits performed by month in PBF and comparison districts, January 2009 – December 2012.
Fig. 3.
Proportion of monthly first ANC visits that occurred in the first trimester of pregnancy in PBF and comparison districts, January 2009 – December 2012.
Fig. 4.
Number of number of institutional deliveries performed by month in PBF and comparison districts, January 2009 – December 2012.
Fig. 5.
Number of postnatal care visits performed by month in PBF and comparison districts, January 2009 – December 2012.
4. Discussion
The results presented in this paper suggest that the PBF program implemented in Burkina Faso led to sizeable increases in the provision of maternal health services. Relative to comparable health facilities, the average number of advanced ANC visits, deliveries and postnatal care visits increased by 27.7%, 9.2%, and 119% percent, respectively. These changes are substantial, and were achieved within a relatively short period, suggesting that the program was highly effective in the setting studied. This paper adds to several other quasi-experimental designs that found mixed and positive results of PBF using measures of health service provision, health service quality, and health provider efficiency. Overall, when considered alongside other evidence that is evolving from the multitude of PBF evaluations that have recently been conducted, this study makes a strong case that PBF can be used to increase the provision of at least some targeted health services.
The use of administrative data for this analysis results in several limitations. The first is that administrative data may be more subject to misreporting than survey data. It is possible that some facilities in both groups were not reporting services before the start of PBF and that the increases shown here are the result of improved reporting in PBF facilities. To investigate this we repeated the same difference-in-differences regression analysis used in the results after dropping all the health facilities that reported missing data for any of our outcomes for any month included in the dataset. As shown in Appendix 3, the results remain similar after dropping facilities missing monthly data on one or more of the outcomes. We can therefore rule out the possibility that improved reporting on the extensive margin can explain our results; however, we cannot rule out the possibility of that the PBF facilities that reported data at baseline increased the completeness of their reporting after the start of the intervention.
In addition to data reliability, our use of aggregated administrative data limited our ability to determine who benefited from the program. Without individual-level data, we were not able to examine whether PBF resulted in disproportionally greater coverage increases among groups with higher socioeconomic status, a concern that has been raised in previous research (Lannes, Meessen, Soucat, & Basinga, 2015). Finally, our reliance on administrative data made it difficult to examine service-specific changes in quality of care.
A second limitation of our study is that did not contain measures that could be used to more closely examine the mechanisms of change. Two important potential mechanisms include the effect of increased overall facility resources, which might affect service use through infrastructure improvement if electricity, more space, or more hospital beds allowed the facilities to serve more patients for longer hours. Other studies have provided comparison facilities with an equivalent amount of financial resources in an effort to isolate the effect of incentives (Basinga et al., 2010). No extra financial resources were provided to comparison facilities in this study; however, funding from the Programme d’Appui au Développement Sanitaire (Program for Health Development) which had previously supported PBF facilities was not provided during the intervention period. A second mechanism is the additional financial resources provided to health facilities and health workers, which can offer motivation and increased flexibility (Basinga et al., 2010). The average monthly amount of the quarterly PBF payment for nurses from April 2011 – March 2012 was 25,787 CFA ($43), which is equivalent to approximately 16% of average government salaries for this category of health worker. In the absence of more data, qualitative research and formal meetings including local stakeholders could be used to shed light on the causal mechanisms explaining the effects observed in this study.
The third limitation is that neither the pilot districts, nor the comparison districts were randomly selected. While we show in our analysis that facilities in treatment and comparison areas look very similar with respect to their pre-intervention trends, it is possible that differential trends would have emerged even in the absence of the intervention. The results in this paper may apply to other regions in Burkina Faso, as the intervention and comparison districts share similar health and economic characteristics as other rural districts in the country.
There are several policy implications for these results. Since 2006 in an attempt to reduce financial barriers, delivery care has been exempt from user fees in Burkina Faso (Ridde, Richard, Bicaba, Queuille, & Conombo, 2011). While user fee reductions have been shown to increase service coverage, many women continued to deliver at home demonstrating that cost was not the only barrier to care seeking (De Allegri et al., 2015, Ganaba et al., 2016). This study shows that in the context of user fee reductions, additional strategies that focus on reinforcing the delivery of essential health services, such as performance-based financing, might be a successful policy tool to further increase coverage by increasing health worker motivation while ensuring quality of care. PBF in Burkina Faso has a relatively low cost for implementation, with an average cost of US$3.00 per capita per year to target the entire package of services at the primary and secondary levels of care. Given the positive results observed during the pre-pilot period and the limited resources available in the health sector, the PBF program in Burkina Faso may be a low-cost, high impact intervention to improve maternal and child health. In-depth cost-benefit analyses of different policies should be conducted to compare the impact of these interventions relative to their cost. Additionally, research investigating how to better target the poor, and how to solve demand side challenges within PBF program approach would be valuable.
5. Conclusion
The PBF pilot program in three districts of Burkina Faso that ran from 2011–2013 resulted in a significant increase in key maternal health indicators for PBF. As the country has embarked since 2014 on a progressive scale-up of PBF that currently covers one-third of the country and includes an embedded experimental impact evaluation, more knowledge and evidence is expected to be produced by the Burkina Faso PBF program in the coming years.
Funding
This work was supported by the World Bank through the Health Results Innovation Trust Fund (HRITF).
Conflict of interest statement
Maria Steenland’s work preparing this manuscript was financed by the World Bank’s Health Results Innovation Trust Fund (HRITF).
Footnotes
The findings, interpretations and conclusions expressed in the paper are entirely those of the authors, and do not represent the views of the World Bank, its Executive Directors, or the countries they represent. We wish to thank our partners in the Ministry of Health in Burkina Faso for helping develop the study methodology and tools, and facilitating data collection.
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2017.01.001.
Appendix A. Supplementary material
Supplementary material
.
References
- Basinga, P., Gertler, P.J., Binagwaho, A., Soucat, A.L.B., Sturdy, J.R., Vermeersch, C.M.J. (2010). Paying primary health care centers for performance in Rwanda. Policy research working papers.
- Binyaruka P., Patouillard E., Powell-Jackson T., Greco G., Maestad O., Borghi J. Effect of paying for performance on utilisation, quality, and user costs of health services in Tanzania: A controlled before and after study. PLoS One. 2015;10(8):e0135013. doi: 10.1371/journal.pone.0135013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonfrer I., Soeters R., Van de Poel E., Basenya O., Longin G., van de Looij F., van Doorslaer E. Introduction of performance-based financing in Burundi was associated with improvements in care and quality. Health Affairs. 2014;33(12):2179–2187. doi: 10.1377/hlthaff.2014.0081. [DOI] [PubMed] [Google Scholar]
- Bonfrer I., Van de Poel E., Van Doorslaer E. The effects of performance incentives on the utilization and quality of maternal and child care in Burundi. Social Science Medicine. 2014;123:96–104. doi: 10.1016/j.socscimed.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Bossert T., Chitah M.B., Bowser D. Decentralization in Zambia: Resource allocation and district performance. Health Policy and Planning. 2003;18(4):357–369. doi: 10.1093/heapol/czg044. [DOI] [PubMed] [Google Scholar]
- De Allegri M., Tiendrebéogo J., Müller O., Yé M., Jahn A., Ridde V. Understanding home delivery in a context of user fee reduction: A cross-sectional mixed methods study in rural Burkina Faso. BMC pregnancy and childbirth. 2015;15(1):1. doi: 10.1186/s12884-015-0764-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Direction Generale Ministere de la Sante Burkina Faso (2014). Annuaire Statistique N.001 2013. Ouagadougou, Burkina Faso
- Falisse J.-B., Ndayishimiye J., Kamenyero V., Bossuyt M. Performance-based financing in the context of selective free health-care: An evaluation of its effects on the use of primary health-care services in Burundi using routine data. Health Policy and Planning. 2015;30(10):1251–1260. doi: 10.1093/heapol/czu132. [DOI] [PubMed] [Google Scholar]
- Fritsche G.B., Soeters R., Meessen B. World Bank Publications; Washington D.C, USA: 2014. Performance-based financing toolkit. [Google Scholar]
- Ganaba R., Ilboudo P.G., Cresswell J.A., Yaogo M., Diallo C.O., Richard F., Witter S. The obstetric care subsidy policy in Burkina Faso: What are the effects after five years of implementation? Findings of a complex evaluation. BMC Pregnancy Childbirth. 2016;16:84. doi: 10.1186/s12884-016-0875-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gertler P.J., Giovagnoli P.I. and Martinez S. Rewarding provider performance to enable a healthy start to life: Evidence from Argentina’s Plan Nacer. World Bank Policy Research Working Paper. 2014;(6884) [Google Scholar]
- Hatt L.E., Makinen M., Madhavan S., Conlon C.M. Effects of user fee exemptions on the provision and use of maternal health services: A review of literature. Journal of Health, Population and Nutrition. 2013;31:67–80. [PubMed] [Google Scholar]
- Huillery, E., & Seban, J. (2014). Performance-Based Financing, Motivation and Final Output in the Health Sector: experimental evidence from the Democratic Republic of Congo. Retrieved from 〈http://econ.sciences-po.fr/sites/default/files/file/elise/paper_DRC_July2014_AER.pdf〉
- ICF International (2012). The DHS Program STATcompiler. Retrieved June 10, 2015, from 〈http://www.statcompiler.com〉
- Ir P., Korachais C., Chheng K., Horemans D., Van Damme W., Meessen B. Boosting facility deliveries with results-based financing: A mixed-methods evaluation of the government midwifery incentive scheme in Cambodia. BMC Pregnancy Childbirth. 2015;15(1):1. doi: 10.1186/s12884-015-0589-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones G., Steketee R.W., Black R.E., Bhutta Z.A., Morris S.S., Group B.C.S.S. How many child deaths can we prevent this year? The Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- Kuruvilla S., Bustreo F., Kuo N., Mishra C., Taylor K., Fogstad H., Thomas J. The Global strategy for women's, children's and adolescents' health (2016–2030): A roadmap based on evidence and country experience. Bulletin of the World Health Organization. 2016;94(5):398–400. doi: 10.2471/BLT.16.170431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lannes L., Meessen B., Soucat A., Basinga P. Can performance‐based financing help reaching the poor with maternal and child health services? The experience of rural Rwanda. The International Journal of Health Planning and Management. 2015;31(3):309–348. doi: 10.1002/hpm.2297. [DOI] [PubMed] [Google Scholar]
- Meessen, B. (2012). An online debate on "Performance-based financing in low- and middle-income countries: still more questions than answers". [DOI] [PMC free article] [PubMed]
- Ministere de la Sante Burkina Faso (2013). Guide de Mise en Oeuvre du Financement Base sur les Resultats dans le secteur de la Sante: Ministere de la Sante Burkina Faso
- Nair M., Yoshida S., Lambrechts T., Boschi-Pinto C., Bose K., Mason E.M., Mathai M. Facilitators and barriers to quality of care in maternal, newborn and child health: A global situational analysis through metareview. BMJ Open. 2014;4(5):e004749. doi: 10.1136/bmjopen-2013-004749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peabody J.W., Shimkhada R., Quimbo S., Solon O., Javier X., McCulloch C. The impact of performance incentives on child health outcomes: Results from a cluster randomized controlled trial in the Philippines. Health Policy Plan. 2014;29(5):615–621. doi: 10.1093/heapol/czt047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V., Richard F., Bicaba A., Queuille L., Conombo G. The national subsidy for deliveries and emergency obstetric care in Burkina Faso. Health Policy Plan. 2011;26(Suppl 2) doi: 10.1093/heapol/czr060. [DOI] [PubMed] [Google Scholar]
- Robyn P.J., Bärnighausen T., Souares A., Traoré A., Bicaba B., Sié A., Sauerborn R. Provider payment methods and health worker motivation in community-based health insurance: A mixed-methods study. Social Science Medicine. 2014;108:223–236. doi: 10.1016/j.socscimed.2014.01.034. [DOI] [PubMed] [Google Scholar]
- Rosenfield A., Maine D., Freedman L. Meeting MDG-5: An impossible dream? The Lancet. 2006;368(9542):1133–1135. doi: 10.1016/S0140-6736(06)69386-0. [DOI] [PubMed] [Google Scholar]
- Soeters R., Griffiths F. Improving government health services through contract management: A case from Cambodia. Health Policy Plan. 2003;18(1):74–83. doi: 10.1093/heapol/18.1.74. [DOI] [PubMed] [Google Scholar]
- The AIDSTAR-Two Project. (2011). The PBF Handbook: Designing and Implementing Effective Performance-Based Financing Programs Version 1.0
- The World Bank. (2012). Concept note for the impact evaluation of a PBF pilot in Cameroon.
- The World Health Organization & UNICEF (2014). Trends in maternal mortality: 1990 to 2013: estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division: executive summary.
- United Nations. (2014). The Millennium Development Goals Report 2014.
- Witter S., Fretheim A., Kessy F.L., Lindahl A.K. Paying for performance to improve the delivery of health interventions in low- and middle-income countries. Cochrane Database Syst Rev. 2012;2:CD007899. doi: 10.1002/14651858.CD007899.pub2. [DOI] [PubMed] [Google Scholar]
- Zeng W., Cros M., Wright K.D., Shepard D.S. Impact of performance-based financing on primary health care services in Haiti. Health Policy and Planning. 2013;28(6):596–605. doi: 10.1093/heapol/czs099. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material