Abstract
We use best–worst scaling to assess two types of concern levels of the adverse consequences of smoking in China. While the smoking cessation policy has worked well in Taiwan, more than 1 million people in mainland China are estimated to die every year from tobacco use. This study compares the preferences of Chinese individuals in the two jurisdictions (mainland versus Taiwan) and explores the possibility of information-based interventions. The relative importance of 13 adverse effects was assessed by conducting a web-based survey on a sample of 480 Chinese participants. The 13 items consist of various adverse effects of tobacco use: from long-term health risk, such as lung cancer and cardiovascular diseases, to reduction of physical capacity and sexual dysfunction, and disturbance to non-smokers. The resulting data suggest possible strategies to curb smoking. Subgroup analysis, focusing on gender, smoking status, and nicotine dependence, was also conducted. Lung cancer, cardiovascular diseases, and chronic obstructive pulmonary disease, in this order, rank highest for both types of respondents. On the other hand, high expenditures (13th) and weight gain after cessation (12th) are the lowest ranked for both. Measuring individual best–worst scores reveals substantial heterogeneity among respondents and that information-based intervention can help curb smoking.
Keywords: Smoking, Information-based interventions, Best–worst scaling method, Chinese preferences
Highlights
-
•
Best-worst scaling (BWS) is used to assess concerns on tobacco adverse effects.
-
•
Adverse effects of tobacco are assessed for mainland and Taiwan residents.
-
•
Lung cancer, cardiovascular diseases, and COPD rank highest for both.
-
•
Information-based interventions are explored for Chinese smokers.
-
•
Comparative results provide insights for a future anti-smoking policy.
Introduction
An anti-tobacco policy is presently one of the most important aspects of health strategy and attracts significant interest around the world (Chen et al., 2015, Pirie et al., 2013, Thun et al., 2013).
China has the largest smoking population in the world (Chen et al., 2015). More than 6 million people are estimated to die annually from tobacco use worldwide (Chen et al., 2015, Jha, 2009, Mathers and Loncar, 2006). Among them, China accounts for more than 1 million deaths annually (Chen et al., 2015). As such, it is very important for China to conduct an effective smoking cessation policy. However, several misunderstandings and “myths” limit such an anti-smoking campaign. Previous research investigates the attitudes of the Chinese towards smoking, finding that these along with certain myths (detailed in the background section) prevent Chinese smokers from quitting smoking. While more than 50% of ever-smokers in high-income countries quit willingly, less than 10% of Chinese ever-smokers quit (Chen et al., 2015, Giovino et al., 2012). These surprising facts indicate that a smoking cessation policy that reduces misunderstandings and myths would be one of the most efficient and cost-effective strategies in China.
The smoking cessation policy has worked incredibly well in Taiwan, whose population has the same racial background as mainland China. The smoking policy in Taiwan is almost the same as in European countries (Bureau of Health Promotion Taiwan, 2014), and the smoking rate here is 18.0% (male: 32.5%, female: 3.3%, 2013), compared to 28.1% (male: 52.9%, female: 2.4%, 2015) in mainland China (World Health Organization, 2015).
In Taiwan, a variety of anti-smoking campaigns have been carried out over the past several decades, such as expanding smoke-free areas, placing health warning illustrations on cigarette packages, prohibiting tobacco advertisements, increasing tobacco taxes, etc. (Bureau of Health Promotion Taiwan, 2014). However, in mainland China, few evidence-based tobacco prevention and intervention strategies have been conducted (Chen et al., 2015; Finch et al., 2010). Promoting the application of Taiwan’s tobacco strategies in mainland China may help reduce the number of smokers and advance the understanding of the negative aspects of tobacco use for more effective tobacco control.
One of our main goals is to reduce the number of smokers in mainland China. This study focuses on two jurisdictions (Taiwan and mainland China), which are culturally similar but have different tobacco control policies. We conducted a web-based survey to comparatively analyze whether the citizens of the two jurisdictions have different preferences on the negative effects of tobacco use.
If so, we consider that the differences are due to (partially) different tobacco control policies. The findings obtained by comparing the two jurisdictions suggest that the success of the tobacco control policies in Taiwan could be useful in identifying policies with the potential to effectively reduce the number of smokers in mainland China.
The analysis results revealed a difference between the two jurisdictions, indicating that the negative effects of passive tobacco exposure are well understood in Taiwan, while this understanding is comparatively poor in mainland China.
The various adverse consequences of tobacco use have gained significant interest worldwide (Chen et al., 2015, Pirie et al., 2013, Thun et al., 2013). Marti (2012) performs a pioneering analysis using best–worst scaling (BWS) to assess the level of concern for the adverse effects of tobacco use. Targeting adolescents in Switzerland, the resulting data and subgroup analysis showed heterogeneity in preferences and the possibility of information-based interventions. We selected items and designed the experiment following Marti (2012), who selected 15 adverse consequences of tobacco use. Before the web-based survey, the pretest was conducted with a sample of 16 smoker and non-smoker Japanese college students to confirm whether items used in this study are appropriate or understandable. After additional discussion with a Chinese specialist in health economics to consider the 15 items, we chose 13 items to investigate Chinese preferences. During the pretest, respondents commented that one of the items (Tobacco industry manipulation) was difficult to understand as an adverse consequence and the other (Endangering relatives) duplicated other effects (Disturbance to non-smokers). Hence, the relative importance of the 13 adverse effects, also used by Marti (2012), was assessed by conducting a web-based survey on a sample of 480 Chinese participants. Therefore, this study focusses on the general population and compares preferences of smoking-related risks between Chinese individuals in the two culturally close jurisdictions but with large differences in terms of tobacco control policies. Following Marti (2012),1 we investigated not only the health risks most commonly cited (i.e., lung cancer and cardiovascular diseases), but also less mentioned health implications (e.g., effects on teeth, appearance, skin, weight, and sexual dysfunction) and other adverse effects that are unrelated to health, such as cost and addiction. Among health risks, some studies found that the population overestimates the risk of cancer (Van Houtven et al., 2008, Marti, 2012, Viscusi et al., 2014). This study also investigates how seriously the Chinese evaluate the risk of cancer.
This study uses the case 1 (or object case) BWS method to assess the relative importance of 13 adverse effects caused by tobacco use. In addition to the health risks of direct smoking, we also focused on passive smoking, which is a serious problem in mainland China (Wang, Chiu, Qiu, Au, & Yu, 2009). In countries with high awareness of anti-smoking, a large portion of the population is concerned about passive smoking and smoking in public places is often prohibited. Comparative results provide insights for future strategies of an anti-smoking policy.
Background
Taiwan versus mainland China
People living in different societies have different viewpoints and preferences. In this section, we compare the smoking culture in two types of societies. The populations of Taiwan and mainland China, although sharing the same racial background, have different attitudes towards tobacco use.
Taiwan
The history of smoking in Taiwan is reported in detail in Taiwan’s tobacco control annual report, which promotes that “tobacco products are the leading killers and destroyers of our health” (Bureau of Health Promotion Taiwan, 2014). Before the 1970s, smoking products were an indispensable part of social life in Taiwan, with the smoking rate among males as high as 60%. In the 1980s, as some smoking hazards became known, the government allocated more funds for tobacco control. The civil society also began to raise awareness about the damage caused by tobacco use and the Tobacco Hazards Prevention Act was implemented in 1997, which provided the basis for smoking control, limited the marketing and advertisement of tobacco products, and mandated the indication of nicotine and tar content on tobacco products. In the 2000s, on each pack of cigarettes, one was required to pay a tobacco health and welfare surcharge, which increased from TWD 5 in 2000 to TWD 10 in 2006 and TWD 20 in 2009. In 2000, Tobacco and Alcohol Tax Act was passed, which required a TWD 5 for each pack, with collection beginning in 2002; it was amended in 2006 to increase the surcharge to TWD 10 per pack and to TWD 20 in 2009 as per the amended Tobacco Hazards Prevention Act.
In 2005, the World Health Organization (WHO) Framework Convention on Tobacco Control came into effect. The Taiwanese government amended the Tobacco Hazards Prevention Act in 2009 in line with these international trends. The 2009 amendment covered a variety of anti-tobacco measures, expanding smoke-free areas to all enclosed workplaces and public places, placing health-warning illustrations on cigarette packages, prohibiting tobacco advertisements, and increasing tobacco taxes. This amended law has had significant impact on decreasing the number of smokers. The annual cessation rate rose significantly from 7.1% in 2007 to 8.9% in 2010. The quit attempt rate also increased significantly from 39.4% to 42.9% (Chang, Sung, Zhu, & Chiou, 2014). Thus, the amended law had a significant positive impact on prevalence of adolescent smoking (Huang, Lin, Chen, & Tsai, 2013).
Mainland China
China is the world’s largest tobacco manufacturer and consumer, with 350 million smokers in 2010 (Li et al., 2011). Moreover, the annual number of deaths from tobacco use reached 1.2 million in 2010, and is estimated to reach 2 million by 2030 and 3 million by 2050 (Chen et al., 2015, Zhang et al., 2011).
There are several striking features of tobacco use in mainland China. First, a large gender distribution gap exists, meaning that men are at risk of death and disease from active smoking and women from passive exposure (Gan, Smith, Hammond, & Hu, 2007). Second, there is a recent trend of smoking initiation at an early age. Compared to older generations, such as those born in the 1930s, younger generations (e.g., those born in the 1970s) started smoking at an average age of around 20, which means that many may have started even before the age of 20 (Chen et al., 2015). Third, few Chinese willingly quit smoking. Compared to many high-income countries, where more than 50% of ever-smokers quit by choice (Giovino et al., 2012), less than 10% of Chinese ever-smokers quit willingly (Chen et al., 2015). Differentiating mainland China’s mortality pattern from western nations is that chronic lung disease rates are relatively higher than coronary heart disease rates, possibly because of indoor air pollution and smoking (Chen et al., 2015). Fourth, there still exist several misunderstandings and “myths” regarding tobacco use: “Tobacco use is an important social and cultural tradition”; “It is not unusual for teachers and doctors to smoke”; “Smoking is not illegal and that is individual freedom”; “Tobacco is a significant contributor to the economy”; etc. (Ma et al., 2008). These myths and attitudes prevent Chinese smokers from quitting smoking.
Method
Data collection
A web-based survey2 was conducted during August 20–29, 2015. A Japanese version of the questionnaire used was translated into Chinese by a bilingual scholar. Two additional bilingual individuals checked both versions of the questionnaire and modified its wording accordingly. Respondents were registered monitors with Searchina Research Co., Ltd., a research firm, to estimate preferences among the public. Subjects were required to provide consent to participate in the survey after reading the objectives and a document explaining the protection of confidentiality on the survey website. Those who consented were given access to a set of screening questions. We screened monitors by age, gender, and smoking status and collected samples reflecting the proportions of the current status for the two jurisdictions. The research firm obtained approval from each respondent and the participation of respondents was voluntary. Ethical approval was not required for conducting the survey. Participants could withdraw from the survey at any time and/or skip any questions they did not want to answer. After respondents finished answering the BWS questions, they were requested to answer personal demographic questions: age, gender, household income, smoking status, etc. Nicotine dependence level questions were based on the Fagerström Test for Nicotine Dependence (FTND) (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) and all participants were categorized into three groups (High, Middle, and Low levels) separately.
The targeted sample size was set at 240 for Taiwan and 240 for mainland China (all participants were recruited from among Shanghai residents; therefore, we refer to mainland China as Shanghai hereafter), reflecting the proportions of age, gender, and current smoking status for the two jurisdictions. With regard to the sample size of the previous studies, for example, the sample size of Marti (2012) is 376, whereas the sample size of our study is 480 (240 in each region). Therefore, we judged that our sample size was comparable to those in previous studies. The recruitment ended when the targeted sample size was collected, resulting in 240 completed questionnaires in each case.
Demographic characteristic
Descriptive statistics of two types of Chinese are presented in Appendix A. Demographic characteristic, such as age and gender show no statistically significant difference, while smoking rate and nicotine dependence are higher in Shanghai participants. Almost one-third (29.6%) of Shanghai respondents are smokers, while this is approximately half in Taiwan (15.8%). Additionally, almost one-third of Shanghai participants are more than middle level in nicotine dependence.
Best–worst scaling method
BWS is a relatively new analysis method developed by Finn and Louviere (1992). It presents multiple choices and then requires the respondents to choose the best and the worst options, respectively. Here, we use the BWS method to analyze the levels of concern about the various adverse effects of tobacco use. The BWS is divided into three types: namely object (case 1), profile (case 2), and multi-profile (case 3) cases (Flynn, 2010). We use object case (case 1), which is suitable for perceiving the relative evaluation of the multiple items the respondents chose, as our purpose is to measure the seriousness of the 13 adverse consequences. Table 1 shows the items used in this analysis.
Table 1.
Items used in the BW scaling.
| Item no. | Adverse consequences |
|---|---|
| 1 | Lung cancer |
| 2 | Cardiovascular diseases |
| 3 | Reduced life expectancy |
| 4 | COPD |
| 5 | Skin problems |
| 6 | Reduction of physical capacity |
| 7 | Oral and dental problems |
| 8 | Sexual dysfunction |
| 9 | Addiction |
| 10 | Weight gain after cessation |
| 11 | Inhalation of chemicals |
| 12 | Disturbance of non-smokers |
| 13 | High expenditures |
BWS method case 1 has the merit for respondents since they can easily choose the extremes as the most important and least important among several items, and for the analysts, who are able to analyze the data by only using the four basic arithmetic operations. On these points, BWS method case 1 is superior to the traditional methods for preference analysis, such as rating scale or ranking, therefore this method is now used in broad fields such as marketing or health economics (Lusk and Briggeman, 2009, Tsuge et al., 2014). For details on the BWS method, see Louviere, Lings, Islam, Gudergan, and Flynn (2013) and Tsuge et al. (2014).
Questionnaire design
Numerous studies use the balanced incomplete block designs (BIBDs) to create a combination of choices, the so-called choice set, which is presented to respondents. Using BIBDs, each choice appears the same number of times through all choice sets, and so does the combination of each choice and the other choices (Auger et al., 2007, Lee et al., 2008). Furthermore, the BIBDs ensure that each choice set includes the same number of items. Some previous studies, including Marti (2012), used the two-level orthogonal main-effect design rather than the BIBD to construct their choice sets (Marti, 2012). However, the BIBD is preferable, as the number of items can vary for each choice set in the two-level orthogonal main-effect design.
Here, we refer to previous studies and construct the choice set using BIBDs. We convert the number of BIBDs into the 13 adverse consequences of tobacco use described earlier, and generate 13 choice sets as shown in Table 2. All choices appeared four times and a combination of each adverse consequence appeared once. We present the 13 choice sets to respondents, who choose the most and the least serious damage from each choice set. Fig. 1 is an example of a choice task.
Table 2.
Balanced incomplete block designs (BIBDs) ― 13 choices & four options’ case.
| Choice set no. | Item no. | |||
|---|---|---|---|---|
| 1 | 1 | 2 | 4 | 10 |
| 2 | 2 | 3 | 5 | 11 |
| 3 | 3 | 4 | 6 | 12 |
| 4 | 4 | 5 | 7 | 13 |
| 5 | 1 | 5 | 6 | 8 |
| 6 | 2 | 6 | 7 | 9 |
| 7 | 3 | 7 | 8 | 10 |
| 8 | 4 | 8 | 9 | 11 |
| 9 | 5 | 9 | 10 | 12 |
| 10 | 6 | 10 | 11 | 13 |
| 11 | 1 | 7 | 11 | 12 |
| 12 | 2 | 8 | 12 | 13 |
| 13 | 1 | 3 | 9 | 13 |
Fig. 1.
Example of a choice task.
Counting analysis
It is common to use counting analysis and the maximum-difference (max-diff) model (logit model) to analyze data obtained by the BWS method. Counting analysis is typically used to analyze BWS data, for it does not need expert knowledge and utilizes only four basic arithmetic operations, as mentioned. First, we count the number of times each choice has been chosen as “the best” and “the worst.” The former is called “total best” and the latter is “total worst.” Subsequently, we subtract “total worst” from “total best” and the result is “B-W score,” which is high when one choice is evaluated more than others. A previous study (Marley & Louviere, 2005) shows that the B-W score is a good approximation of the precision of the maximum likelihood estimate in the logit model.
Maximum-difference model (logit model)
The max-diff model, developed by Finn and Louviere (1992), is an expansion of the conditional logit model and is based on a random utility model used in discrete choice experiments. In the max-diff model, it is assumed that respondents consider the remaining utilities for all possible pairs within the choice sets, and choose one pair that makes the result maximum as “the best” and “the worst.” For J choices, the number of choice pairs containing “the best” and “the worst,” from which respondents can choose is J(J – 1). Here, we have 12 pairs (4 * 3 = 12) of “the best” and “the worst” that can be chosen, as they contain four (J = 4) of 13 adverse consequences in each choice set.
We define as the utility of choice , presents the utility calculated as the difference between choice and choice , and is the error term in Eq. (1):
| (1) |
The probability that respondents choose choice and choice as “the best” and “the worst,” respectively, from J is described as the probability, which means that the difference in utility between choice and choice is bigger than all the other pairs of choices in the choice sets:
Assuming that the error term follows a type I extreme value distribution (Gumbel distribution), we obtain the conditional logit model developed by McFadden (1974). The probability that the respondents choose choice and choice as “the best” and “the worst,” respectively, from J, is described as follows (Lusk & Briggeman, 2009):
| (2) |
Parameter is estimated by maximum likelihood estimation.
Results
Counting analysis
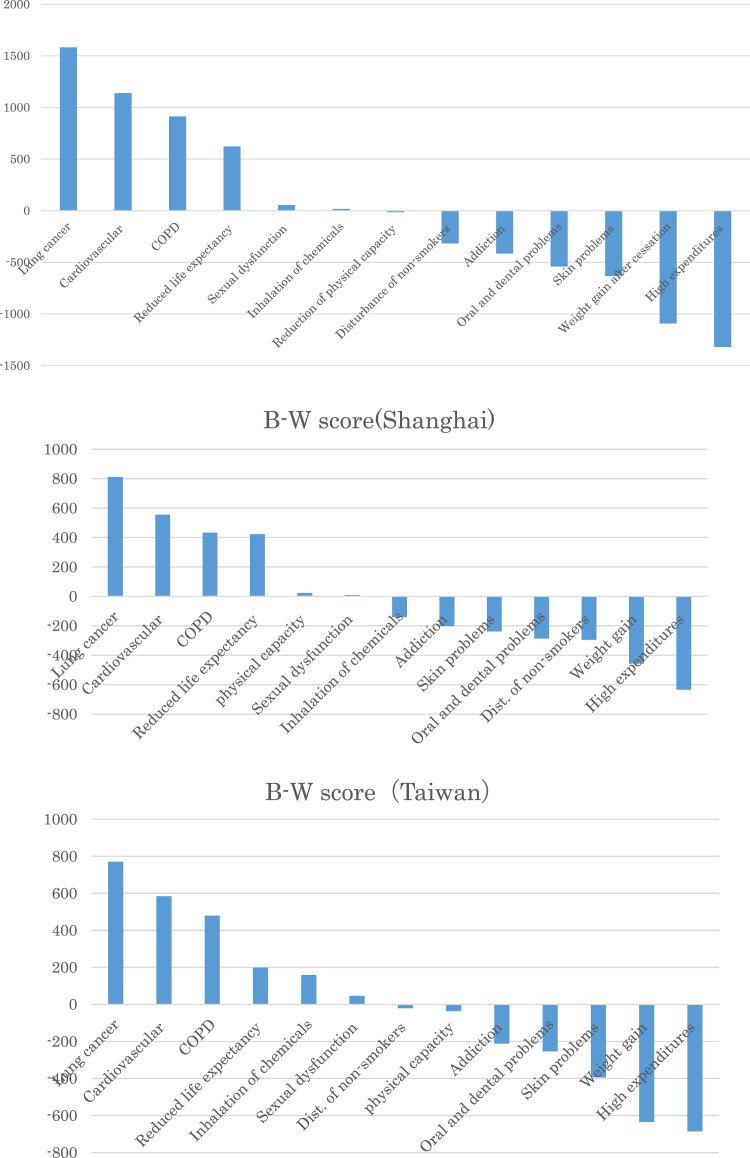
The results of the counting analysis are shown in Fig. 2. The results of the counting analysis for each group (Shanghai and Taiwan) are also shown in Fig. 2. The main results can be summarized as follows:
-
•
As expected, lung cancer is considered the most serious negative outcome, followed by cardiovascular disease, chronic obstructive pulmonary disease (COPD), and reduced life expectancy. This finding is in line with preceding observations focusing on cancer risk (Van Houtven et al., 2008, Viscusi et al., 2014).
-
•
The relative seriousness of disturbance to non-smokers is underestimated in Shanghai.
Fig. 2.
Results of the counting analysis.
“Disturbance to non-smokers” is ranked the seventh most important factor in Taiwan, while it is 11th in Shanghai. This finding is in line with our intuition that most people in mainland China, especially male smokers are insensitive to adverse effects of smoking on others, while successful anti-smoking campaigns make the Taiwanese more sensitive to others by recognizing that smoking is a great risk factor, not only for themselves, but also for others.
Maximum-difference analysis
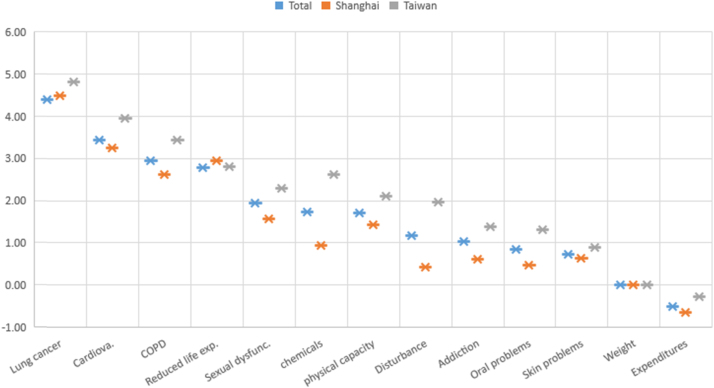
Table 3 shows the estimation results of the max-diff analysis. For each item, we summarized the results by group (total, Shanghai, and Taiwanese) in Fig. 3. The main results can be summarized as follows:
-
•
Lung cancer is regarded as the most serious negative outcome, followed by cardiovascular disease, COPD, and reduced life expectancy.
-
•
The differences in preferences vary by items in each group.
Table 3.
Estimation results of Maximum-difference model.
|
Total |
Shanghai |
Taiwan |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | St. dev. | p value | Coefficient | St. dev. | p value | Coefficient | St. dev. | p value | |
| Lung cancer | 4.41 | 0.089 | < 0.001 | 4.49 | 0.1018 | < 0.001 | 4.83 | 0.1070 | < 0.001 |
| Cardiovascular | 3.44 | 0.089 | < 0.001 | 3.25 | 0.1007 | < 0.001 | 3.95 | 0.1037 | < 0.001 |
| Reduced life expectancy | 2.79 | 0.080 | < 0.001 | 2.95 | 0.0920 | < 0.001 | 2.81 | 0.0918 | < 0.001 |
| COPD | 2.95 | 0.087 | < 0.001 | 2.63 | 0.0983 | < 0.001 | 3.44 | 0.1000 | < 0.001 |
| Skin problems | 0.73 | 0.076 | < 0.001 | 0.64 | 0.0802 | < 0.001 | 0.89 | 0.0920 | < 0.001 |
| Reduction of physical capacity | 1.72 | 0.082 | < 0.001 | 1.42 | 0.0905 | < 0.001 | 2.11 | 0.0987 | < 0.001 |
| Oral and dental problems | 0.85 | 0.077 | < 0.001 | 0.48 | 0.0845 | < 0.001 | 1.31 | 0.0962 | < 0.001 |
| Sexual dysfunction | 1.94 | 0.079 | < 0.001 | 1.58 | 0.0890 | < 0.001 | 2.29 | 0.0966 | < 0.001 |
| Addiction | 1.04 | 0.077 | < 0.001 | 0.62 | 0.0873 | < 0.001 | 1.39 | 0.0927 | < 0.001 |
| Inhalation of chemicals | 1.73 | 0.078 | < 0.001 | 0.94 | 0.0872 | < 0.001 | 2.63 | 0.0991 | < 0.001 |
| Disturbance of non-smokers | 1.18 | 0.072 | < 0.001 | 0.43 | 0.0849 | < 0.001 | 1.97 | 0.0844 | < 0.001 |
| High expenditures | -0.51 | 0.079 | < 0.001 | -0.65 | 0.0899 | < 0.001 | -0.27 | 0.0882 | 0.002 |
| Weight gain after cessation | – | – | – | – | – | – | – | – | – |
| n | 480 | 240 | 240 | ||||||
| Log-likelihood | -6537.69 | -4991.51 | -4837.64 | ||||||
| Akaike Information Crit. | 6549.69 | 5003.51 | 4849.64 | ||||||
Fig. 3.
Graphical representation of the estimation results of Maximum-difference model.
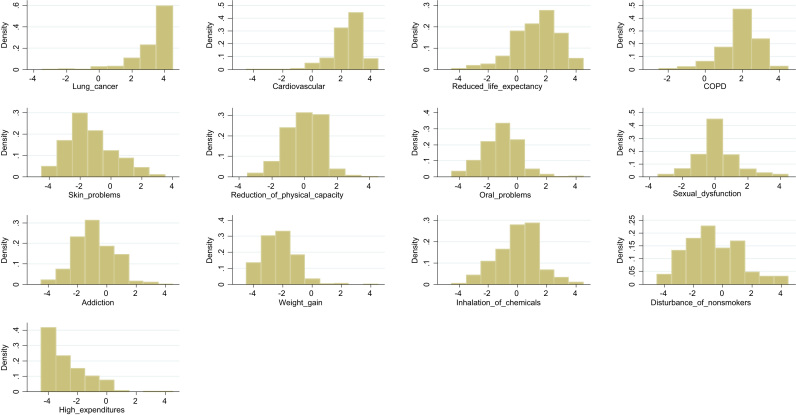
Distributions of preferences for each item
For all 13 items, we counted individual B-W scores, which lie in the possible range of -4 to 4. Fig. 4 shows the distributions of individual B-W scores. The individual B-W scores for each item exhibit substantial heterogeneities. To investigate these, we compare the mean B-W scores by subgroups: Shanghai and Taiwan, males and female, smokers and non-smokers, and individuals with “high,” “middle,” and”low” nicotine addiction (measured in line with questions in the FTND (Heatherton et al., 1991). We used a similar classification as Marti (2012) to conduct the subgroup analyses (gender, smoking status, etc.). As the main objective of this study is to contribute in reducing the number of smokers in mainland China, comparisons have been made between not only Shanghai and Taiwan, but also using subgroups by sex, smoking history, and level of nicotine addiction. By comparing subgroups instead of only the comparison between Shanghai and Taiwan, it is possible to obtain knowledge helpful in reducing smoking in China.
Fig. 4.
Distributions of B-W scores for each adverse effect.
In his comparative analysis between subgroups, Marti (2012) indicates differences in preferences between subgroups, such as males and females, which is effective in providing information related to the harm tobacco use can cause.
This study also compares and analyzes the subgroups based on the level of nicotine addiction. If a difference in preference according to the addiction level is confirmed, it would be effective to provide information in accordance with those preferences. Table 4 shows comparison results by each subgroup.
Table 4.
Results by subgroups.
| Adverse effect | Shanghai vs. Taiwan | Male vs. female | Smoking vs. non-smoking | High+middle vs. Low nicotine addiction | ||||
|---|---|---|---|---|---|---|---|---|
| Lung cancer | 0.17 | * | -0.08 | -0.34 | *** | -0.35 | *** | |
| Cardiovascular | -0.12 | 0.18 | * | -0.13 | -0.16 | |||
| Reduced life expectancy | 0.93 | *** | 0.21 | -0.20 | -0.20 | |||
| COPD | -0.20 | ** | -0.09 | -0.22 | * | -0.23 | ** | |
| Skin problems | 0.65 | *** | 0.59 | 0.31 | * | 0.34 | ** | |
| Reduction of physical capacity | 0.25 | *** | -0.06 | 0.09 | 0.10 | |||
| Oral and dental problems | -0.13 | 0.33 | *** | 0.33 | ** | 0.31 | ** | |
| Sexual dysfunction | -0.15 | -0.21 | * | -0.02 | 0.00 | |||
| Addiction | 0.04 | -0.12 | 0.23 | 0.25 | * | |||
| Inhalation of chemicals | -1.25 | *** | -0.58 | *** | -0.18 | -0.20 | ||
| Disturbance of non-smokers | -1.15 | *** | -0.37 | ** | -0.49 | ** | -0.44 | ** |
| High expenditures | 0.22 | * | 0.23 | * | 0.34 | ** | 0.33 | ** |
| Weight gain after cessation | 0.74 | *** | -0.04 | 0.28 | ** | 0.27 | ** | |
Significant: 1%***, 5%**, 10%*.
We collected a variety of comments during the pretest, such as female respondents expressing that appearance is one of their biggest concerns, and non-smoking respondents expressing concerns of long-term, smoking-related health issues and disturbance to non-smokers. As for appearance and long-term variables, Marti (2012) has analyzed the difference in them between subgroups and obtained useful results. As for smoking-related health status and disturbance to non-smokers, useful implications were expected from the comparisons. We then focus on the following four variables: appearance, smoking-related health status, long-term, and disturbance to non-smokers.
The main results can be summarized as follows:
-
•
Some groups weigh variables related to appearance highly. In this instance, skin problems, oral and dental problems, and weight gain after cessation, are identified as variables relating to appearance.
Excluding the importance that Shanghai residents assign to oral and dental problems, smokers, Shanghai residents, and individuals with high to moderate nicotine addiction place greater importance on variables related to appearance.
-
•
Some subgroups assign lower importance to smoking-related health status. Here, COPD and inhalation of chemicals are identified as aspects of smoking-related health status.
Except for the importance for inhalation of chemicals by smokers and individuals with high to moderate nicotine addiction, Shanghai residents, smokers, and individuals with high to moderate nicotine addiction assign lower importance to smoking-related health status. These two findings suggest that the preferences of Shanghai residents, smokers, and individuals with high to moderate nicotine addiction are highly homogeneous.
-
•
Some groups assign a lower importance to long-term variables. Lung cancer, cardiovascular disease, and reduced life expectancy are identified as long-term variables in this instance.
Smokers and individuals with high to moderate nicotine addiction assign a lower importance to lung cancer. The other variables are not statistically significant. However, it is unexpected and even noteworthy that Shanghai residents assign a higher importance to reduced life expectancy.
-
•
Some groups assign a low importance to variables of disturbance to non-smokers. Shanghai residents, males, smokers, and individuals with high to moderate nicotine addiction assign a lower importance to problems caused to others.
The four results summarized here show that Shanghai residents, smokers, and individuals with high to moderate nicotine addiction have significantly similar preferences. Furthermore, that these groups’ preferences are similar to preferences associated with smoking may enable the acquisition of further knowledge from prior research, showing that smokers place a low emphasis on health status and problems caused to other people, as well as prior research showing that smokers have a strong status quo bias.
Implications for intervention and policy
Analysis of the preferences of residents from Shanghai and Taiwan on the negative outcomes of tobacco use revealed several findings. First, the personal preferences of individuals for the 13 negative outcomes of tobacco use are significantly heterogeneous.
Our analysis revealed different preferences for “Disturbance to non-smokers” and “Inhalation of chemicals” between the two jurisdictions, possibly due to their different tobacco policies. In Taiwan, the negative effects of passive tobacco exposure are well understood, while this understanding is comparatively poor in mainland China.
In Taiwan, anti-smoking campaigns have been carried out steadily over the past several decades, such as the increase in tobacco prices, educating the youth about the negative effects of tobacco use, and anti-tobacco pictures on cigarette packaging. It is believed that the understanding of the negative effects of passive tobacco exposure can be improved in mainland China by implementing steady tobacco control policies similar to those in Taiwan, leading to a decrease in the number of smokers.
It was found that Shanghai residents and smokers assign a lower importance to passive smoking. It is well known that schooling has an impact on curbing smoking (Becker and Murphy, 1988, Chaloupka, 1991, Farrell and Fuchs, 1982, Grossman, 1972). Individuals with a higher level of schooling are less likely to smoke and more likely to quit smoking. Grossman (1972) suggests that education increases the production of health by individuals and increases the ability to understand information on the negative effects of smoking.
For instance, between 1966 and 1987, in the United States, while the smoking rate among those who had not graduated high school dropped only marginally, from 36.5% to 35.7%, the rate among college graduates fell dramatically, from 33.7% to 16.3% (Sander, 1995). Therefore, messages that evoke concerns of passive smoking should be considered. Subgroup analysis (Table 4) indicates that Shanghai residents are unaware of the seriousness of passive smoking. Therefore, it is necessary to educate them of these risks.
Additionally, smokers show a tendency to underestimate long-term health consequences, such as lung cancer. In other words, it is likely that smokers are not cognizant of the fact that these long-term health consequences will shorten their lives. Previous literature indicates that smokers exhibit a high rate of time preference and a low rate of risk aversion (Anderson and Mellor, 2008, Ida and Goto, 2009). Smokers show little interest in investments leading to gains in the distant future, and tend to act according to their immediate impulses or with a strong present bias (Khwaja, Sloan, & Salm, 2006), while showing little concern about long-term health consequences, such as lung cancer (Anderson & Mellor, 2008).
Consequently, a campaign informing people that smoking leads to a higher risk of health problems, including cancer and high blood pressure, as well as shortened life expectancy, combined with increased education and targeted messages, is likely to be effective.
Conclusion
China has the largest population of smokers in the world. Assessing Chinese preferences for smoking provides valuable information in promoting anti-tobacco campaigns.
Using BWS, this study analyzed how two types of Chinese (residents of Shanghai and Taiwan) evaluate 13 adverse consequences of tobacco use. This study is the first empirical analysis conducted using case 1 BWS for the health assessment of Chinese residents. The analysis focused on the target groups’ evaluations of 13 negative effects of tobacco. These 13 effects, as applied in the research by Marti (2012), include long-term negative health effects such as lung cancer and heart disease; causal factors of short-term ill health; costs relating to health impacts; and issues of physical appearance not directly connected to health. The resulting data showed that lung cancer is evaluated as the most serious effect, followed by heart disease and COPD. A comparison between Shanghai and Taiwanese residents showed that the former are more likely to place a low emphasis on the problems caused by smoking to other people.
Additionally, subgroup analysis showed that Shanghai residents, smokers, and individuals with high to moderate nicotine addiction have significantly similar preferences. We believe that information on public preferences towards the adverse effects of tobacco use is valuable and information-based interventions will help enact anti-tobacco policies in mainland China.
This study has several limitations. It is based on a web-based survey. Web-based samples tend to be biased towards higher income and higher education populations. Indeed, most of our observations come from individuals with higher education background. However, our main goal is to compare the preferences of individuals in the two culturally close jurisdictions but with large differences in tobacco control policies. From this perspective, our sample biases do not undermine our goal. For a more precise investigation of public preferences in future, we will conduct experiments with samples that reflect the proportions of the current status of the two jurisdictions.
Funding
The Asia Pacific Institute of Research, Japan.
Ethical approval
This project was helped by Searchina Research Co., Ltd. for conducting the web-based survey. http://www.insightsresearch.cn/ Respondents were registered monitors with Searchina Research Co., Ltd., a research firm. Subjects were required to provide consent to participate in the survey after reading the objectives and a document explaining the protection of confidentiality on the survey website.
Conflict of interest
None.
Acknowledgements
This project was funded by the Asia Pacific Institute of Research. We would like to thank Ma Xinxin for translating questionnaires into Chinese and Searchina Research Co., Ltd. for conducting the web-based survey, and gratefully thank two anonymous referees for their helpful comments and suggestions.
Footnotes
The questionnaire used here follows Marti (2012) and the results of the survey have not been published elsewhere.
The questionnaire (both the Japanese and Chinese versions) is available upon request from the corresponding author.
Contributor Information
Takeshi Mori, Email: uhh03905@nifty.com.
Takahiro Tsuge, Email: tsuge@center.konan-u.ac.jp.
Appendix A. Sample characteristics
Descriptive statistics ― whole sample (N = 480)
| Mainland | Taiwan | ||
|---|---|---|---|
| n = 240 | n = 240 | ||
| Mean age | 39.15 | 39.22 | |
| Female (%) | 47.5 | 47.5 | |
| Level of education (%) | Junior high school | 0.4 | 0.0 |
| High school | 0.4 | 6.3 | |
| 2-year or 4-year university | 43.3 | 32.1 | |
| Graduate school | 55.8 | 28.8 | |
| Household income (%) | < $50,000 | 27.1 | 37.9 |
| $50,000 to $60,000 | 22.5 | 23.3 | |
| $60,000 to $70,000 | 15.8 | 13.3 | |
| $70,000 to $80,000 | 12.9 | 9.6 | |
| > $80,000 | 21.6 | 15.8 | |
| Nicotine dependence (%) | Low | 70.4 | 85.0 |
| Middle | 22.1 | 11.7 | |
| High | 7.5 | 3.3 | |
| Current smoker (%) | 29.6 | 15.8 |
References
- Anderson L.R., Mellor J.M. Predicting health behaviors with an experimental measure of risk preference. Journal of Health Economics. 2008;27:1260–1274. doi: 10.1016/j.jhealeco.2008.05.011. [DOI] [PubMed] [Google Scholar]
- Auger P., Devinney T.M., Louviere J.J. Using best–worst scaling methodology to investigate consumer ethical beliefs across countries. Journal of Business Ethics. 2007;70:299–326. [Google Scholar]
- Becker G.S., Murphy K.M. A theory of rational addiction. Journal of Political Economy. 1988;96:675–700. [Google Scholar]
- Bureau of Health Promotion Taiwan . Taiwan tobacco control 2014 annual report. 2014. [Google Scholar]
- Chaloupka F. Rational addictive behavior and cigarette smoking. Journal of Political Economy. 1991;99:722–742. [Google Scholar]
- Chang F.C., Sung H.Y., Zhu S.H., Chiou S.T. Impact of the 2009 Taiwan tobacco hazards prevention act on smoking cessation. Addiction. 2014;109:140–146. doi: 10.1111/add.12344. [DOI] [PubMed] [Google Scholar]
- Chen Z., Peto R., Zhou M., Iona A., Smith M., Yang L. Contrasting male and female trends in tobacco-attributed mortality in China: Evidence from successive nationwide prospective cohort studies. The Lancet. 2015;386:1447–1456. doi: 10.1016/S0140-6736(15)00340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell P., Fuchs V.R. Schooling and health: The cigarette connection. Journal of Health Economics. 1982;1:217–230. doi: 10.1016/0167-6296(82)90001-7. [DOI] [PubMed] [Google Scholar]
- Finch K., Novotny T.E., Ma S., Qin D., Xia W., Xin G. Smoking knowledge, attitudes, and behaviors among rural-to-urban migrant women in Beijing China. Asia Pacific J. Pub. Health. 2010;22:342–353. doi: 10.1177/1010539509335034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn A., Louviere J.J. Determining the appropriate response to evidence of public concern: The case of food safety. Journal of Public Policy Marketing. 1992:12–25. [Google Scholar]
- Flynn T.N. Valuing citizen and patient preferences in health: Recent developments in three types of best–worst scaling. Expert Review of Pharmacoeconomics Outcomes Research. 2010;10:259–267. doi: 10.1586/erp.10.29. [DOI] [PubMed] [Google Scholar]
- Gan Q., Smith K.R., Hammond S.K., Hu T.-w. Disease burden of adult lung cancer and ischaemic heart disease from passive tobacco smoking in China. Tobacco Control. 2007;16:417–422. doi: 10.1136/tc.2007.021477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovino G.A., Mirza S.A., Samet J.M., Gupta P.C., Jarvis M.J., Bhala N. Tobacco use in 3 billion individuals from 16 countries: An analysis of nationally representative cross-sectional household surveys. The Lancet. 2012;380:668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- Grossman M. On the concept of health capital and the demand for health. Journal of Political Economy. 1972;80:223–255. [Google Scholar]
- Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerstrom K.O. The Fagerström test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Huang S.L., Lin I., Chen C.Y., Tsai T.I. Impact of tobacco control policies on adolescent smoking: Findings from the global youth tobacco survey in Taiwan. Addiction. 2013;108:1829–1835. doi: 10.1111/add.12259. [DOI] [PubMed] [Google Scholar]
- Ida T., Goto R. Simultaneous measurement of time and risk preferences: Stated preference discrete choice modeling analysis depending on smoking behavior. International Economic Review. 2009;50:1169–1182. [Google Scholar]
- Jha P. Avoidable global cancer deaths and total deaths from smoking. Nature Reviews Cancer. 2009;9:655–664. doi: 10.1038/nrc2703. [DOI] [PubMed] [Google Scholar]
- Khwaja A., Sloan F., Salm M. Evidence on preferences and subjective beliefs of risk takers: The case of smokers. International Journal of Industrial Organization. 2006;24:667–682. [Google Scholar]
- Lee J.A., Soutar G., Louviere J. The best–worst scaling approach: An alternative to Schwartz’s values survey. Journal of Personality Assessment. 2008;90:335–347. doi: 10.1080/00223890802107925. [DOI] [PubMed] [Google Scholar]
- Li Q., Hsia J., Yang G. Prevalence of smoking in China in 2010. New England J. of Medicine. 2011;364:2469–2470. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- Louviere J., Lings I., Islam T., Gudergan S., Flynn T. An introduction to the application of (case 1) best–worst scaling in marketing research. International Journal of Research in Marketing. 2013;30:292–303. [Google Scholar]
- Lusk J.L., Briggeman B.C. Food values. American Journal of Agricultural Economics. 2009;91:184–196. [Google Scholar]
- Ma S., Hoang M.-A., Samet J.M., Wang J., Mei C., Xu X. Myths and attitudes that sustain smoking in China. Journal of Health Communication. 2008;13:654–666. doi: 10.1080/10810730802412222. [DOI] [PubMed] [Google Scholar]
- Marley A.A., Louviere J.J. Some probabilistic models of best, worst, and best–worst choices. Journal of Mathematical Psychology. 2005;49:464–480. [Google Scholar]
- Marti J. A best–worst scaling survey of adolescents' level of concern for health and non-health consequences of smoking. Social Science Medicine. 2012;75:87–97. doi: 10.1016/j.socscimed.2012.02.024. [DOI] [PubMed] [Google Scholar]
- Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFadden D. Conditional logit analysis of qualitative choice behavior. In: Zarembka P., editor. Frontiers in Econometrics. Academic Press; New York: 1974. pp. 105–142. [Google Scholar]
- Pirie K., Peto R., Reeves G.K., Green J., Beral V., Collaborators M.W.S. The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. The Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander W. Schooling and smoking. Economics of Education Review. 1995;14:23–33. [Google Scholar]
- Thun M.J., Carter B.D., Feskanich D., Freedman N.D., Prentice R., Lopez A.D. 50-year trends in smoking-related mortality in the United States. New England Journal of Medicine. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuge T., Nakamura S., Usio N. Assessing the difficulty of implementing wildlife-friendly farming practices by using the best–worst scaling approach. Social-Ecological Restoration in Paddy-Dominated Landscapes. 2014:223–236. (Springer) [Google Scholar]
- Van Houtven G., Sullivan M.B., Dockins C. Cancer premiums and latency effects: A risk tradeoff approach for valuing reductions in fatal cancer risks. Journal of Risk and Uncertainty. 2008;36:179–199. [Google Scholar]
- Viscusi W.K., Huber J., Bell J. Assessing whether there is a cancer premium for the value of a statistical life. Health Economics. 2014;23:384–396. doi: 10.1002/hec.2919. [DOI] [PubMed] [Google Scholar]
- Wang X.-R., Chiu Y.-L., Qiu H., Au J., Yu I.-S. The roles of smoking and cooking emissions in lung cancer risk among Chinese women in Hong Kong. Annals of Oncology. 2009 doi: 10.1093/annonc/mdn699. (mdn699) [DOI] [PubMed] [Google Scholar]
- World Health Organization . Vol. 2015. World Health Organization; 2015. (WHO report on the global tobacco epidemic 2015: Raising taxes on tobacco). [Google Scholar]
- Zhang J., Ou J.X., Bai C.X. Tobacco smoking in China: Prevalence, disease burden, challenges and future strategies. Respirology. 2011;16:1165–1172. doi: 10.1111/j.1440-1843.2011.02062.x. [DOI] [PubMed] [Google Scholar]