Abstract
In the United States, associations between attained education and adult health typically are larger for those from disadvantaged childhood backgrounds. However, it remains unclear how specific key childhood indicators contribute to these adult health patterns, especially outside the United States. Drawing on the 2014 European Social Survey (20 countries; N=31544), we investigate the key childhood and adolescent indicators of parental education, childhood financial strain, and any serious household conflict growing up, given how these early exposures are known to correlate strongly with both educational attainment and adult health. In regressions with country fixed effects, we find across Europe that higher levels of education are more strongly linked to lessened adult depressive symptoms when childhood disadvantage is present in terms of lower levels of parental education or higher childhood financial strain specifically. However, adjusted predictions reveal that childhood financial strain contributes to this heterogeneity in educational returns far more strongly than parental education. For self-rated health, only childhood financial strain enhances estimated educational health benefits when considering all key childhood social and economic factors jointly. Similarly, childhood financial strain in particular enhances educational protection against overall rates of disease in adulthood. Overall, our findings support prior work on United States data revealing higher educational health returns given childhood disadvantage. At the same time, our findings across three distinct adult health indicators suggest the particular importance of childhood financial strain to understanding heterogeneity in educational health returns.
Keywords: Depression, Self-rated health, Morbidity, Educational attainment, Childhood, Europe
Around the world, individuals with higher levels of education enjoy better health, as marked by their lower rates of depression, inflammation, and major disease, and by their enhanced longevity (Beckfield et al., 2013, Elo, 2009). To help shed light on what produces these health advantages seen with higher levels of education, recent work has illuminated how associations between higher education and better health vary according to childhood or adolescent resources (Bauldry, 2014, Bauldry, 2015, Conti and Heckman, 2010, Ross and Mirowsky, 2011, Schaan, 2014, Schafer et al., 2013). These recent studies test the general hypothesis that educational health gains are concentrated among those with specific childhood or adolescent backgrounds. To the extent that this is true, observed educational health disparities may actually reflect heterogeneous treatment effects of education, with those who are disadvantaged during childhood perhaps benefitting more from schooling. Knowing how health returns to education vary by childhood background provides new information about potential causal mechanisms linking education to health, by revealing whether health gains linked to education are distributed evenly across segments of the general population (Montez & Friedman, 2015).
Evidence is accumulating in the United States that educational health returns are heterogeneous across family socioeconomic origins, with higher education being substantially less predictive of adult health among those who come from advantaged families (Andersson, 2016, Bauldry, 2015, Ross and Mirowsky, 2011, Schafer et al., 2013). Some US studies find the opposite, such that observed educational health returns are higher among those with greater parental socioeconomic resources (Andersson, 2016, Bauldry, 2014). However, existing work has not made clear how distinct key childhood and adolescent life exposures contribute to these heterogeneous returns. Specifically, by focusing either on singular childhood factors like parental education or social class (Andersson, 2016; Ross & Mirowsky, 2016; Schaan, 2014) or on complex vectors of educational determinants (Bauldry, 2014, Bauldry, 2015, Conti and Heckman, 2010, Schafer et al., 2013), work on educational health disparities in the United States leaves unclear intermediate mechanisms, by which key childhood or adolescent factors might jointly shape these disparities. Namely, parental social class, childhood financial strain, and abuse or maltreatment growing up all make distinct and well-established contributions to both final educational attainment and adult health (Carroll et al., 2013, Ross and Mirowsky, 2011, Schafer and Ferraro, 2012, Schafer et al., 2013, Wagmiller et al., 2006, Ziol-Guest et al., 2012). Yet, how each of these key factors contributes uniquely to health returns to education remains unclear. Also, existing work on heterogeneous educational health gradients has focused on the United States. Because socioeconomic health inequality differs substantially across advanced nations (Elo, 2009; Murray, Vos, Lozano, Naghavi & Flaxman, 2012), it is important to examine patterns of heterogeneous educational health returns outside the United States.
Therefore, in this study, we move forward existing work on three fronts. First, we offer an illustrative test of how key childhood and adolescent life exposures jointly contribute to adult educational health disparities. Second, we draw on national data from 20 European countries to offer a first representative test of heterogeneous educational health returns in Europe. Finally, we examine three distinct general health outcomes in adulthood, to evaluate any potential health outcome dependency in educational health returns.
Background
Although the association between higher education and better health is one of the most robust in the population health literature, ample evidence now exists for the presence of heterogeneous associations between education and health. Childhood or adolescent advantages, in terms of higher social and economic resources while growing up, may ultimately make attained education less important to adult health. Specifically, educational attainment may correlate less strongly with adult health given childhood advantage, and childhood disadvantage may enhance the value of education for predicting adult health. This mutual compensation mechanism linking educational attainment and childhood conditions often is termed “resource substitution” (Ross and Mirowsky, 2011, Schafer et al., 2013). Researchers who propose resource substitution generally make the argument that human capital acquisition through schooling on the one hand and childhood factors or advantages separate from schooling on the other hand essentially provide the same basic kinds of cognitive, noncognitive, psychosocial, or material resources correlated with physical health throughout the life course. Thus, educational and extra-educational resources are essentially substitutable in the production of adult health or well-being (e.g., Cutler & Lleras-Muney, 2010; Ross & Mirowsky, 2011; Schafer et al., 2013).
Other studies obtain results consistent with an opposing mechanism, in which education favors those with advantaged childhood backgrounds. Namely, a “resource multiplication” perspective usually posits that educational systems tend to favor individuals from privileged childhood backgrounds, thus amplifying rather than reducing health inequality present during childhood (Andersson, 2016, Bauldry, 2014, Schafer et al., 2013). This perspective highlights how pre-educational resources and active parental guidance dramatically increase the odds of educational engagement, success, and attainment, beginning as early as preschool and carrying through high school and college graduation (Conti & Heckman, 2010). Individuals who begin life in an advantaged socioeconomic position are more likely to obtain higher levels of schooling and more likely to obtain higher-quality schooling (Hout, 2012). However, still unclear is whether these patterns of educational inequality also result in health inequality by level of education; namely, whether these differences in educational experiences linked to childhood factors also result in differing health returns to higher levels of education once obtained.
Overall, the opposing frameworks of resource substitution and resource multiplication take differing stances on how educational attainments and experiences on the one hand, and childhood and adolescent social and economic resources separate from schooling on the other hand, may powerfully interact to either narrow or widen health disparities.
Limitations of existing work on heterogeneous educational health returns
Relevant studies of national US data usually find adult health disparities that are consistent with resource substitution across educational attainment and childhood and adolescent resources (Bauldry, 2015, Ross and Mirowsky, 2011, Schaan, 2014, Schafer et al., 2013), though occasionally they find patterns consistent with resource multiplication (Andersson, 2016, Bauldry, 2014). However, existing work leaves unclear how specific key childhood and adolescent factors contribute to these patterns, and this work also does not resolve whether similar patterns hold outside the United States – or across diverse physical health measures in adulthood.
Investigating key childhood social and economic exposures
Existing work has yet to establish the unique contributions of key childhood social and economic factors to heterogeneous educational returns. In one typical approach, education-health correlations are analyzed across different levels of singular childhood factors such as parental education or socioeconomic class (e.g., Andersson, 2016; Ross & Mirowsky, 2011; Schaan, 2014). In another common approach, researchers specify rich and complex vectors of childhood social and economic factors; these vectors then are used as a basis of forming statistical groups or categories for comparing differences in education-health correlations (e.g., Bauldry, 2014, Bauldry, 2015; Conti & Heckman, 2010; Schafer et al. 2013).
Focusing on singular childhood factors or on complex vectors of factors both are valuable techniques, as they both provide answers to the guiding question of whether observed educational health returns are higher or lower given approximate levels of childhood disadvantage or privilege. However, the answers provided are limited ones, as they leave unclear how certain key childhood and adolescent life exposures may matter jointly to educational health returns. Conti and Heckman (2010) isolate vectors of childhood cognitive, noncognitive, and health factors and show how they contribute separately to observed health returns to education. Because their analysis focuses on how estimated educational health returns vary across percentile scores of endowment factors observed prior to finishing school, it leaves unclear whether or how this effect heterogeneity linked to endowments is based in key childhood life exposures. Cognitive, noncognitive, and health factors are bundled within individuals, and they carry shared origins in specific key childhood social and economic exposures. Vector-based analyses of educational health returns overlook this emphasis on critical life exposures by instead focusing on summative propensity or percentile scores calculated across groups of variables that represent highly intermingled childhood processes, leaving basic structural antecedents unclear (see also Bauldry, 2014, Bauldry, 2015; Schafer et al., 2013).
Adult health disparities carry multifaceted roots in distinct key childhood social and economic conditions. Therefore, it is valuable to analyze these childhood exposures as distinct factors, in terms of how they contribute distinctly to observed educational health returns. As key examples, childhood social class, financial strain, and abuse or maltreatment are three distinct childhood exposures linked to schooling and health across life course. Research on heterogeneous health returns to education has yet to show that parental education in particular modifies educational health returns net of other key childhood exposures such as childhood household conflict or financial strain. This is a vital oversight, given extensive evidence that maltreatment by parents or childhood financial hardship, while they correlate with parental education, still carry consequences for life-course health that are separate and distinct from those of parental education or social class more generally (Ferraro et al., 2016, Hertzman and Boyce, 2010, Johnson and Schoeni, 2011, Schafer and Ferraro, 2012, Ziol-Guest et al., 2012). Meanwhile, existing work also has shown that parental education, childhood financial hardship, and childhood abuse or maltreatment all are linked notably and separately to odds of obtaining higher levels of education (e.g., Bauldry, 2014, Bauldry, 2015; Ross & Mirowsky, 2011; Schafer et al., 2013; Wagmiller et al., 2006).
Despite these well-established links, it remains unclear whether or to what extent these key childhood factors contribute to health returns to education among adults. Because childhood socioeconomic status, financial hardship, and abuse or maltreatment all are related strongly to accumulating vectors of cognitive, noncognitive, psychosocial, and health resources during childhood and adolescence (Conti and Heckman, 2010, Schafer and Ferraro, 2012, Schafer et al., 2013, Ziol-Guest et al., 2012), it is reasonable to expect that these key childhood factors would each make separate and powerful contributions to heterogeneous health returns to education. Indeed, several studies conducted in the US have employed a propensity scoring method in which individuals sort into college on the basis of these key childhood socioeconomic factors, and have revealed substantial heterogeneity in health returns to college across levels of propensity scores (e.g., Bauldry, 2014, Bauldry, 2015; Schafer et al., 2013). However, because the strategy is vector-based, it does not shed light on how specific key childhood factors contribute to heterogeneity in health by level of education.
Analyses of heterogeneous educational health returns outside the United States
A second limitation of existing research on heterogeneous educational health returns is that it draws mostly on United States data. To a large extent, patterns obtained in the US may be predicted to apply in non-US contexts, given basic parallels among rich Western democracies in terms of levels of educational attainment and economic development and in terms of shared civic institutions and globalization influences, for example (Beckfield & Krieger, 2009). Yet, at the same time, European nations differ from the US in a number of respects, in terms of histories of educational institutions (e.g., timing and extent of educational expansion across European nations), the structure of schooling processes (e.g., pathways to academic qualifications or higher degrees), and patterns of social mobility (i.e. differences in parent-child educational correlations across Europe) (Breen & Jonsson, 2005). In addition, Europe also contrasts with the US in terms of key institutional health processes, such as institutionalized social support for citizen well-being and the availability, ease, and affordability of health care (Beckfield et al., 2013).
Limited work to date on non-US data has been limited to non-representative samples. Conti & Heckman’s (2010) analysis drew on a specific British birth cohort. Schaan (2014) analyzed depressive symptoms among middle- and older-aged individuals in thirteen European nations, finding support for resource substitution across parental social class and educational attainment. However, this study drew on a non-probability sample and it did not address distinct childhood conditions.
Outcome dependency in heterogeneous educational health returns
A third limitation of existing work is that it has yet to firmly establish whether processes of resource substitution or multiplication depend on the specific health outcomes under investigation. A serious treatment of differences across health outcomes is important, given how distinct outcomes provide separate windows into biological, physical and mental well-being. For instance, depressive symptoms tap hopelessness and frustrated life expectations, self-rated health captures positive aspects of physical functioning such as energy and vitality independently of illness or morbidity, and overall morbidity provides a useful objective index of number of health problems during adulthood. While Schafer et al. (2013) find consistent evidence for resource substitution across major morbidity and premature mortality, Andersson (2016) finds support for resource multiplication for self-rated health and resource substitution for mortality across multiple decades of US data. Similarly, drawing on a national sample of young adults in the US, Bauldry, 2014, Bauldry, 2015 also finds support for resource multiplication for self-rated health while finding evidence for resource substitution for depressive symptoms. Evidence obtained from Europe is mixed, depending on the health outcome being considered and the way childhood or adolescent resources is operationalized (Conti and Heckman, 2010, Schaan, 2014). Overall, evidence to date on outcome dependency draws mostly on US data, with inconclusive findings; thus possible outcome dependency in European countries remains overlooked.
Overview of the current study
In this study, we draw on a probability dataset of health indicators based in European countries to help move forward existing research on educational health returns. Using representative data from across Europe, we isolate specific key aspects of childhood social and economic conditions: parental education, childhood financial hardship, and potential childhood maltreatment or abuse. Meanwhile, we focus on three distinct adult health outcomes: depression, self-rated health, and morbidity count. Across these three general health outcomes, we analyze whether and to what extent educational health disparities vary by key childhood social and economic indicators.
Materials and methods
Participants and procedure
The 2014 European Social Survey (ESS) provides cross-national, cross-sectional data on childhood social and economic background, educational attainment, and adult mental and physical health. The 2014 wave of the ESS is unique in that it queries adult health measures alongside different indicators of childhood social and economic factors. In the ESS, random probability sampling is used to build representative samples (Eikemo, Bambra, Huijts, & Fitzgerald, 2016). Sample sizes of over 1000 were achieved in each of the 21 nations. After dropping Hungary, in which parental education was not queried, and after restricting the analysis to respondents aged 25 or older (a reasonable age by which to complete college education), our sample is N=34025 across 20 countries. Within this sample, missing data on relevant variables is slight (0 to 5% missing). Thus, analytic samples herein range from N=31497 (depressive symptoms) to N=31503 (self-rated health). For chronic health conditions, N=29364 because Estonia is excluded from the analysis (EE did not submit proper morbidity data; see ESS manual).
Measures
Depressive symptoms
The ESS utilizes an eight-item version of the Center for Epidemiological Studies Depression Scale (CES-D scale) (Radloff, 1977). Referring to the past week, respondents indicated whether they felt depressed, that everything was an effort, restless, happy (reverse-coded), lonely, sad, that they enjoyed life (reverse-coded), and that they could not get going (“none or almost none of the time,” “some of the time,” “most of the time,” or “all or almost all of the time”; alpha=.83). Recent work demonstrates metric equivalence of the CES-D 8 across European countries (Missinne, Vandeviver, Van de Velde, & Bracke, 2014). For ease of interpretation, we calculate the depressive symptomatology score as an average across all item responses and leave the score untransformed, as other treatments of the depressive symptom score (e.g., log transformation, or modeling symptoms as a count) yield the same general results presented here.
Self-Rated Health
Respondents were asked, “How is your health in general? Would you say it is…very good, good, fair, bad or very bad?” We analyze the full range of subjective health in analyses presented here.
Number of health conditions
Respondents indicated whether they have experienced given health conditions in the past twelve months: allergies, bodily pain, breathing problems, cancer, diabetes, high blood pressure, heart or circulation problems, skin conditions, stomach or digestion-related problems, or severe headaches (Eikemo et al., 2016).
Educational attainment
The ESS assesses respondent education according to the International Standard Classification of Education (ISCED) system. The ISCED is structured around basic educational categories developed for cross-national research. Specifically, education is measured as highest credential achieved less than primary education (<P), primary education (P), early or lower secondary qualification (LS), late or upper secondary qualification (US), some college or postsecondary education (SC), four-year university degree (Bachelor’s) or equivalent (C), and postgraduate (G).
Parental education
Parental education likewise was queried according to the ISCED system. Respondents reported the highest level of education obtained by their mother and their father. We take the maximum value of education when both are available and the available value when one is missing. Alternatively, averaging across parents did not change substantive findings.
Childhood household conflict and financial strain
The respondent disclosed how often “there was serious conflict between the people living in your household” or “your family experienced severe financial difficulties” while they were growing up (1=never; 2=hardly ever; 3=sometimes; 4=often; 5=always).
Covariates
All regression analyses adjust for country of residence and for respondent sex and age in years.
Analytic strategy
Here we analyze three general adult health outcomes. Frequency of depressive symptoms is modeled by ordinary least-squares (OLS) regression (Schaan, 2014). Self-rated health is modeled using ordered logistic regression (Bauldry, 2014), and total number of health conditions by negative binomial regression. All models adjust for country of residence using country fixed effects (Schaan, 2014).
These outcomes are modeled using a sequence of regressions in which associations with educational attainment and parental education are examined first. Model 1 regresses the health outcome on parental education and educational attainment, adjusting for age, gender, and country of residence. By focusing on the association between health and education, this model estimates an average association between health and educational attainment net of familial educational origins and basic demographic characteristics (e.g., Ross & Mirowsky, 2011; Schaan, 2014). Then, Model 2 specifies an education interaction term (Education×Parental Education), in order to adjudicate between the resource substitution and resource multiplication perspectives (e.g., Andersson, 2016; Ross & Mirowsky, 2011). Taken together, these first two models establish an average estimated health return for education and how much this estimate varies according parental education (Andersson, 2016, Ross and Mirowsky, 2011, Schaan, 2014).
Childhood financial strain and potential childhood abuse or maltreatment then are analyzed in later models, given how these additional social and economic aspects of childhood are at least partly endogenous to parental education. In Model 3, main effects of childhood household conflict and financial strain are specified. Models 4 and 5 interact these additional childhood indicators with educational attainment sequentially, to test for heterogeneous educational health returns across levels of these indicators. When necessary, an additional model (Model 6) examines all jointly significant interactions between educational attainment and childhood social and economic factors.
Overall, the modeling sequence establishes heterogeneous associations between health and educational attainment across parental education (Models 1–2), across childhood financial strain and maltreatment (Models 3–5), and then across multiple childhood factors if applicable (Model 6). Standard errors are robust, and raw unstandardized coefficients are reported to facilitate the interpretation of interaction terms. Further analyses revealed that findings are substantively identical across genders and when using ESS response weights.
Results
Table 1 overviews means in the 2014 ESS data and associated 95% confidence intervals. On average respondents experienced depressive symptoms between none and some of the time (M=1.67). Self-rated health averages between fair and good (M=3.784) and the average respondent carries 1.5 chronic illnesses. Respondents averaged between an upper-secondary education and some college (M=3.38), while parental education averaged between lower and upper secondary (M=2.54). The average respondent is about 52 years old.
Table 1.
Descriptive statistics (2014 European Social Survey).
| Mean | 95% CI | ||
|---|---|---|---|
| Depressive Symptom Score (1–4)a | 1.673 | 1.667 | 1.678 |
| Self-Rated Health (1–5)b | 3.784 | 3.774 | 3.795 |
| Number of Health Conditions | 1.519 | 1.503 | 1.534 |
| Educational Attainment (ISCED; 0–6)c | 3.377 | 3.360 | 3.394 |
| Parental Education (ISCED; 0–6)c | 2.539 | 2.520 | 2.557 |
| Childhood Household Conflict (1–5)d | 2.178 | 2.167 | 2.190 |
| Childhood Financial Strain (1–5)d | 2.334 | 2.322 | 2.347 |
| Male | 0.466 | 0.461 | 0.472 |
| Age | 52.909 | 52.729 | 53.088 |
Note. N=31544 (20 countries), except for Number of Health Conditions (19 countries, N=29379). ISCED=International Standard Classification of Education
1=(almost) none of time to 4=(almost) all of time.
1=very bad to 5=very good.
0=less than primary school to 6=postgraduate.
1=never to 5=always.
Frequency of depressive symptoms
Table 2 displays regressions of CES-D depression, adjusted for age, sex and country of residence. Model 1 demonstrates that education is negatively related to symptoms (p<.001), with each unit predicting a 0.04 decrease in mean symptom frequency, whereas parental education shows no net relationship (b=−0.006, ns). In Model 2, parental education and educational attainment are statistically interacted, revealing a significant term (Education×Parent Education: b=0.006, p<.001). According to this result, parental education lessens the association between educational attainment and lowered depression. Model 3 enters effects for other childhood socioeconomic indicators, namely household conflict and financial strain; both show relationships with adult depressive symptoms (bs>.05, ps<.001). Model 4 shows that education is more protective against depression among those with higher levels of childhood household conflict (Education×Childhood Household (HH) Conflict: b=−0.008, p<.01). Similarly, in Model 5, education protects against depression increasingly as experience of childhood financial strain increases (Education×Ch. Fin Strain: b=−0.013, p<.001). Finally, Model 6 retains only the jointly significant interaction terms, revealing that parental education and parental financial strain both significantly modify the association between education and adult depressive symptomatology. (An Education×Ch. HH Conflict term is not included in Model 6 because it loses statistical significance when jointly entered; p>.15.).
Table 2.
OLS Regressions of depressive symptom score.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Educational Attainment | -0.040*** | -0.038*** | -0.033*** | -0.034*** | -0.034*** | -0.033*** |
| (0.003) | (0.003) | (0.002) | (0.002) | (0.002) | (0.002) | |
| Parental Education | -0.006 | -0.011* | -0.001 | -0.001 | -0.002 | -0.004 |
| (0.003) | (0.004) | (0.003) | (0.003) | (0.003) | (0.004) | |
| Childhood Household Conflict | 0.076*** | 0.076*** | 0.076*** | 0.076*** | ||
| (0.003) | (0.003) | (0.003) | (0.003) | |||
| Childhood Financial Strain | 0.052*** | 0.052*** | 0.050*** | 0.050*** | ||
| (0.005) | (0.005) | (0.004) | (0.004) | |||
| Education×Parent Education | 0.006*** | 0.004** | ||||
| (0.001) | (0.001) | |||||
| Education×Ch. HH Conflict | -0.008** | |||||
| (0.002) | ||||||
| Education×Ch. Fin Strain | -0.013*** | -0.012*** | ||||
| (0.002) | (0.002) | |||||
| Adjusted R2 | 0.092 | 0.093 | 0.141 | 0.141 | 0.143 | 0.143 |
Note. N=31497. Unstandardized estimates shown. Models adjust for age, sex, and country of residence (not shown). HH=household.
p < .05;
p < .01;
p < .001.
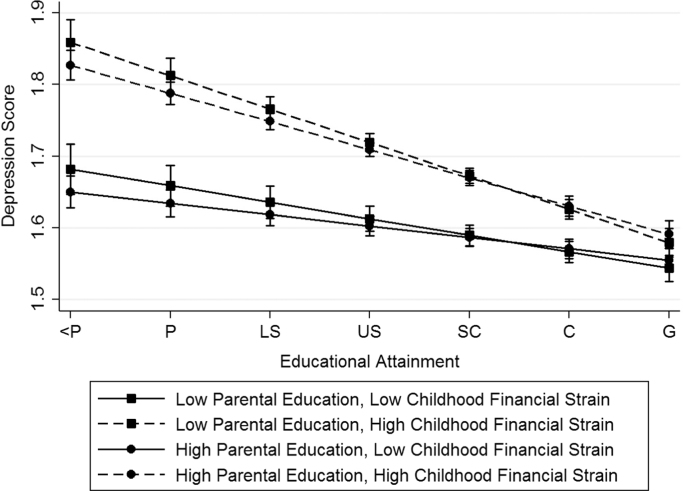
Fig. 1 visualizes results from Model 6. To generate depression predictions, childhood financial strain is defined as low (“never”; 32nd percentile) or high (“sometimes”; 83rd percentile), and parental education similarly is defined as low (primary level; 31st percentile) or high (upper secondary qualification; 75th percentile). As shown by the adjusted predictions (based on average marginal effects), higher educational attainment is linked to lower frequency of symptoms, but this association is much stronger when childhood financial strain is high. Within levels of childhood financial strain, parental education makes a slight difference to the educational slope, but 95% confidence bands do not separate.
Fig. 1.
Adult depression by educational attainment and childhood indicators. Note. Based on final model in Table 2. Educational attainment ranges from less than primary school (<P; level=0) to postgraduate (G; level=6).
Self-rated health
We showcase results from ordered logistic regressions of self-rated health in Table 3. A first model reveals that educational attainment is positively related to self-rated health (unstandardized logit coefficients shown; b=0.194, p<.001). Likewise, parental education shows a positive association with subjective health (b=0.037, p<.001). Model 2 reveals a significant interaction between educational attainment and parental education consistent with resource substitution (Education×Parent Education: b=−0.012, p<.05). Model 3 shows that each additional unit of childhood household conflict or childhood financial strain decreases subjective health in adulthood (ps<.001), and that parental education is not significantly related to health when these resources are controlled (b=0.019, ns). While Model 4 does not reveal significant heterogeneity in educational health returns by childhood household conflict, Model 5 shows that estimated educational health returns increase with higher levels of childhood financial strain (Education×Ch Fin Strain: b=0.019, p<.001). A sixth model (not shown) confirmed that the Education×Ch Fin Strain term maintains statistical significance once an Education×Parent Education term is added to the equation, and that the Education×Parent Education term no longer obtains statistical significance in this joint interaction model.
Table 3.
Ordered logistic regressions of self-rated health.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Educational Attainment | 0.194*** | 0.190*** | 0.178*** | 0.179*** | 0.179*** |
| (0.011) | (0.011) | (0.012) | (0.012) | (0.012) | |
| Parental Education | 0.037*** | 0.046*** | 0.019 | 0.019 | 0.021* |
| (0.011) | (0.011) | (0.010) | (0.010) | (0.010) | |
| Childhood Household Conflict | -0.146*** | -0.147*** | -0.146*** | ||
| (0.013) | (0.014) | (0.013) | |||
| Childhood Financial Strain | -0.175*** | -0.174*** | -0.173*** | ||
| (0.015) | (0.015) | (0.015) | |||
| Education×Parent Education | -0.012* | ||||
| (0.005) | |||||
| Education×Ch. HH Conflict | 0.013 | ||||
| (0.008) | |||||
| Education×Ch. Fin Strain | 0.019*** | ||||
| (0.006) | |||||
| Pseudo R2 | 0.093 | 0.094 | 0.102 | 0.102 | 0.102 |
Note. N=31503. Unstandardized logit estimates shown. Models adjust for age, sex, and country of residence (not shown). HH=household.
** p < .01;
p < .05;
p < .001.
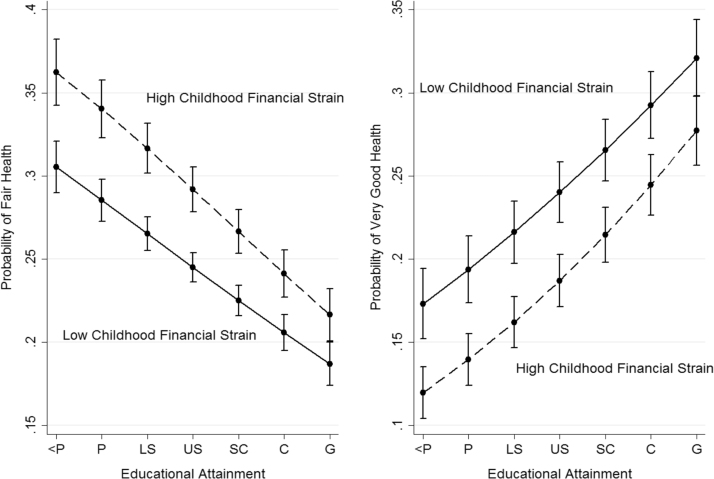
Fig. 2 therefore displays predictions from Model 5, by arraying predicted probabilities of fair health (left panel) and very good health (right panel) in adulthood according to level of educational attainment and either low or high childhood financial strain. Here a resource substitution pattern is visually evident, such that predicted gaps in health by childhood financial strain narrow with increasing respondent education, and no longer significantly differ at the highest level of education (postgraduate). However, differing health returns to education by childhood financial strain are not as dramatic here as observed for depressive symptoms, in that educational health returns are fairly similar across levels of childhood financial strain for self-rated health.
Fig. 2.
Self-rated health by educational attainment and childhood financial strain. Note. Based on final model in Table 3. Educational attainment ranges from less than primary school (<P; level=0) to postgraduate (G; level=6).
Additional models focused on fair, bad, or very bad health did not reveal any significant two-way statistical interactions between respondent education and any of the key childhood social or economic indicators, suggesting that variation across upper levels of subjective health (i.e. fair or above) is important to the heterogeneous returns presented here (e.g., Bauldry, 2014).
Number of health conditions
Negative binomial regressions of number of health conditions are reported in Table 4. In Model 1, each additional unit of educational attainment is linked to a 2.1% decrease in rate of disease (p<.001), while parental education shows no association with disease count (b=0.006, ns). Model 2 finds no significant interaction between parental and respondent education (Education×Parent Education: b=0.004, ns). In Model 3, childhood household conflict and financial strain both demonstrate relationships with adult health conditions, with each additional unit increasing disease rate by about 7 to 9%. While Model 4 shows no interaction between education and childhood household conflict (Education×Ch HH Conflict: b=0.002, ns), Model 5 reveals that experiencing childhood financial strain increases the protective association between education and lower adult disease (Education×Ch Fin Strain: b=−0.007, p<.05).
Table 4.
Negative binomial regressions of number of health conditions.
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Educational Attainment | -0.021*** | -0.019*** | -0.013* | -0.013* | -0.012* |
| (0.005) | (0.005) | (0.005) | (0.005) | (0.005) | |
| Parental Education | 0.006 | 0.003 | 0.014 | 0.014 | 0.013 |
| (0.008) | (0.008) | (0.007) | (0.007) | (0.007) | |
| Childhood Household Conflict | 0.083*** | 0.084*** | 0.084*** | ||
| (0.010) | (0.010) | (0.010) | |||
| Childhood Financial Strain | 0.070*** | 0.070*** | 0.069*** | ||
| (0.008) | (0.008) | (0.008) | |||
| Education× Parent Education | 0.004 | ||||
| (0.003) | |||||
| Education×Ch. HH Conflict | 0.002 | ||||
| (0.004) | |||||
| Education×Ch. Fin Strain | -0.007* | ||||
| (0.003) | |||||
| Pseudo R2 | 0.038 | 0.046 | 0.046 | 0.038 | 0.046 |
Note. N=29364. Unstandardized estimates shown. Models adjust for age, sex, and country of residence (not shown). HH=household.
** p < .01;
p < .05;
p < .001.
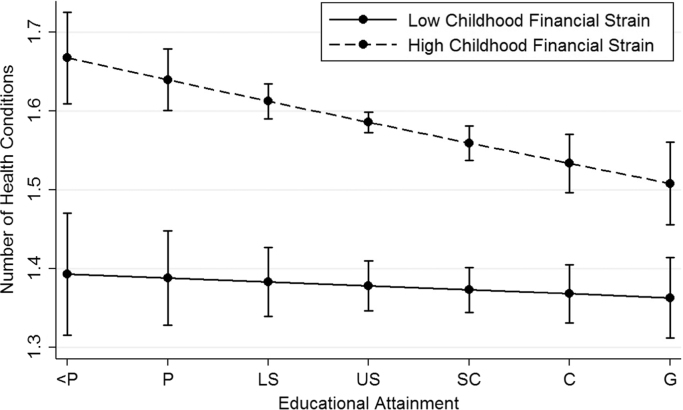
Fig. 3 displays results from Model 5. Here, the association between educational attainment and rate of disease is graphed separately for low and high levels of childhood financial strain. Whereas the educational health gradient at low strain is essentially flat, those who experienced severe financial strain sometimes during childhood show substantial predicted health returns to education. These returns narrow, but do not completely close, the adult disease gap across childhood financial strain, suggesting a powerful and persistent association between early-life adversity and later-life health.
Fig. 3.
Adult disease by educational attainment and childhood financial strain. Note. Based on final model in Table 4. Educational attainment ranges from less than primary school (<P; level=0) to postgraduate (G; level=6).
Discussion
Numerous studies have documented heterogeneous health returns to education by childhood or adolescent factors. Overall, education usually is most predictive of adult health among those from disadvantaged families. However, research has yet to reveal the distinct capacities of multiple childhood conditions to modify educational health returns during adulthood. While parental education is linked to lower levels of household conflict and lower levels of financial strain or hardship during childhood, it also is well-known that these factors exhibit distinct and powerful influences on life-course health. A secondary limitation of existing work is that it has focused almost exclusively on returns in the United States, as the limited work conducted abroad has drawn on non-representative data (e.g., Conti & Heckman, 2010; Schaan, 2014). Finally, empirical evidence to date is unclear as to whether resource substitution or resource multiplication in educational health returns prevails across most health outcomes.
In an effort to help move forward research on heterogeneous returns, this study drew upon recent data from 20 European countries. Estimating average educational health returns across Europe controlling for country of residence allows a strong test of the proposed mechanisms of resource substitution versus resource multiplication, by revealing whether findings hold across diverse geographic, social, cultural and political national contexts within Europe.
We found evidence for resource substitution in the case of adult depressive symptoms, such that individuals from advantaged childhood backgrounds showed the lowest added protection from depressive symptoms with increasing educational attainment. Resource substitution patterns also materialized for self-rated health and for total morbidity or disease count during adulthood. However, our findings suggest the particular importance of childhood financial strain for understanding heterogeneous educational health returns. Namely, across all three general health outcomes examined in this study, higher levels of childhood financial strain increased predicted health returns to educational attainment. For depressive symptoms and total disease count, this shift in estimated educational turns was especially strong. Another childhood resource, parental education, similarly modified estimated educational health returns, but not as robustly or as strongly as did childhood financial strain across the three general health outcomes.
These consistent results across diverse adult health outcomes are remarkable given the different realms of social and physical functioning captured by these adult health indicators. For instance, depressive symptoms reflect ongoing levels of mastery or sense of control. In contrast, self-rated health integrates a diverse set of health processes, ranging from pain, dysphoria or malaise to acute or chronic illness; it also seems to capture one’s sense of vitality or energy above and beyond any major illness (Jylhä, 2009). Finally, given that morbidity count is a total index of general health problems, it may or may not indicate current levels of pain or vitality.
The inclusion of country fixed effects in the present analyses helped to ensure that the obtained patterns are not specific to any nation or set of country-specific mechanisms (e.g., differences in national GDP, health care or health expenditures, educational systems, welfare provisions, or other country-level idiosyncrasies). Further, additional analyses of these adult health outcomes using alternate link functions or outcome specifications (e.g., logit for high depression; OLS for logged depressive symptoms; logit for high number of health conditions) suggested that the general patterns of heterogeneous health returns to education were not model-dependent.
The analyses here carry several limitations that spur areas for future research. First, the ESS utilizes retrospective indicators of childhood conditions. While this is common in population surveys, future life-course data drawing across cohorts would enable the prospective estimation of returns to education (e.g., Bauldry, 2014, Bauldry, 2015). A related issue is that depressive symptoms in adulthood may bias recall of parent-child relationships; however, recent epidemiological research has confirmed that estimates of potential abuse or maltreatment based on retrospective data generally are quite close to estimates obtained from lifetime prevalence data (Kim, Wildeman, Jonson-Reid, & Drake, 2017). This perhaps is due to the more objective nature of harm relative to more subjective parent-child bond measures such as affection or engagement. Relatedly, salient childhood experiences such as residential moves or major loss of resources (e.g., selling a car or valued family possessions, or not having enough food to eat) should fortify the accurate recall of severe financial difficulties growing up. Even if substantial recall error were present in the data, it would need to vary systematically across levels of respondent education in order to influence our findings here that are consistent with resource substitution.
While this study analyzes multiple childhood conditions known to be powerful in shaping life-course health, it is unable to address correlated childhood or adolescent processes, pointing to the need for continued refinement of these factors and their distinct contributions to modifying educational returns. On a related note, because the present study draws exclusively on adult health measures, it leaves unclear whether or to what extent this health variation traces to earlier in the life course, such as to childhood or adolescent precursors to disease such as stress, inflammation, or early illness. Finally, although these analyses adjust for age, some work on heterogeneous returns has adjusted for cohort or period as well. This work finds that age, period and cohort play unique modifying roles in shaping educational health gradients (Andersson, 2016, Masters et al., 2012, Ross et al., 2012). While this work has yet to be applied outside the United States, the presence of repeated cross-sectional data (e.g., ESS) would provide ready grounds for implementing this.
Altogether, this study reveals that heterogeneity in educational health returns across childhood origins indeed seems to exist in non-US contexts, in ways similar to those exhibited in the United States. By isolating processes of heterogeneity across distinct health outcomes and childhood exposures, this study contributes to a more comprehensive understanding of educational health returns (Montez & Friedman, 2015).
Acknowledgements/Funding/COI
A research assistantship at Baylor University facilitated the preparation of this article. The authors declare no conflicts of interest.
References
- Andersson M.A. Health returns to education by family socioeconomic origins, 1980–2008: Testing the importance of gender, cohort, and age. SSM – Population Health. 2016;2:549–560. doi: 10.1016/j.ssmph.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauldry S. Conditional health-related benefits of higher education: An assessment of compensatory versus accumulative mechanisms. Social Science & Medicine. 2014;111:94–100. doi: 10.1016/j.socscimed.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauldry S. Variation in the protective effect of higher education against depression. Society & Mental Health. 2015;5:145–161. doi: 10.1177/2156869314564399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckfield J., Krieger N. Epi+demos+cracy: Linking political systems and priorities to the magnitude of health inequities—evidence, gaps, and a research agenda. Epid Reviews. 2009;31:152–177. doi: 10.1093/epirev/mxp002. [DOI] [PubMed] [Google Scholar]
- Beckfield J., Olafsdottir S., Bakhtiari E. Health inequalities in global context. American Behavioral Scientist. 2013;57:1014–1039. doi: 10.1177/0002764213487343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen R., Jonsson J.O. Inequality of opportunity in comparative perspective: Recent research on educational attainment and mobility. Annual Review of Sociology. 2005;31:223–243. [Google Scholar]
- Carroll J.E., Gruenewald T.L., Taylor S.E., Janicki-Deverts D., Matthews K.A., Seeman T.E. Childhood abuse, parental warmth, and adult multisystem biological risk in the coronary artery risk development in young adults study. PNAS. 2013;110:17149–17153. doi: 10.1073/pnas.1315458110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti G., Heckman J.J. Understanding the early origins of the education-health gradient. Perspectives on Psychological Science. 2010;5:585–605. doi: 10.1177/1745691610383502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D.M., Lleras-Muney A. Understanding differences in health behaviors by education. Journal of Health Economic. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikemo T.A., Bambra C., Huijts T., Fitzgerald R. The first pan-European health inequalities survey of the general population: The European Social Survey rotating module on the social determinants of health. European Sociological Review. 2016:1–17. [Google Scholar]
- Elo I.T. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annual Review of Sociology. 2009;35:553–572. [Google Scholar]
- Ferraro K.F., Schafer M.H., Wilkinson L.R. Childhood disadvantage and health problems in middle and later life: Early imprints on physical health? American Sociological Review. 2016;81:107–133. doi: 10.1177/0003122415619617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzman C., Boyce T. How experience gets under the skin to create gradients in developmental health. Annual Review of Public Health. 2010;31:329–347. doi: 10.1146/annurev.publhealth.012809.103538. [DOI] [PubMed] [Google Scholar]
- Hout M. Social and economic returns to college education in the United States. Annual Review of Sociology. 2012;38:379–400. [Google Scholar]
- Johnson R.C., Schoeni R.F. Early-life origins of adult disease: National longitudinal population-based study of the United States. American Journal of Public Health. 2011;101:2317–2324. doi: 10.2105/AJPH.2011.300252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Social Science and Medicine. 2009;50:344–358. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kim H., Wildeman C., Jonson-Reid M., Drake, B. (2017). Lifetime prevalence of investigating child maltreatment among US children. Am J Public Health, 107: 274–280. [DOI] [PMC free article] [PubMed]
- Masters R.K., Hummer R.A., Powers D.A. Educational differences in US adult mortality: A cohort perspective. American Sociological Review. 2012;77:548–572. doi: 10.1177/0003122412451019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Missinne S., Vandeviver C., Van de Velde S., Bracke P. Measurement equivalence of the CES-D 8 depression-scale among the aging population in eleven European countries. Social Science Research. 2014;46:38–47. doi: 10.1016/j.ssresearch.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Montez Jennifer Karas, Friedman Esther M. Educational attainment and adult health: Under what conditions is the association causal? Social Science & Medicine. 2015;127:1–7. doi: 10.1016/j.socscimed.2014.12.029. [DOI] [PubMed] [Google Scholar]
- Murray C.J.L., Vos T., Lozano R., Naghavi M., Flaxman A.D. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ross C.E., Masters R.K., Hummer R.A. Education and the gender gaps in health and mortality. Demography. 2012;49:1157–1183. doi: 10.1007/s13524-012-0130-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. The interaction of personal and parental education on health. Social Science & Medicine. 2011;72:591–599. doi: 10.1016/j.socscimed.2010.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaan B. The interaction of family background and personal education on depression symptoms in later life. Social Science & Medicine. 2014;102:94–102. doi: 10.1016/j.socscimed.2013.11.049. [DOI] [PubMed] [Google Scholar]
- Schafer M.H., Ferraro K.F. Childhood misfortune as a threat to successful aging: Avoiding disease. Gerontologist. 2012;52:111–120. doi: 10.1093/geront/gnr071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer M.H., Wilkinson L.R., Ferraro K.F. Childhood (mis)fortune, educational attainment, and adult health: Contingent benefits of a college degree? Social Forces. 2013;91:1007–1034. doi: 10.1093/sf/sos192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagmiller R.L., Lennon M.C., Kuang L., Alberti P.M., Aber J.L. The dynamics of economic disadvantage and children’s life chances. American Sociological Review. 2006;71:847–866. [Google Scholar]
- Ziol-Guest K.M., Duncan G.J., Kalil A., Boyce W.T. Early childhood poverty, immune-mediated disease processes, and adult productivity. PNAS. 2012;109:17289–17293. doi: 10.1073/pnas.1203167109. [DOI] [PMC free article] [PubMed] [Google Scholar]